Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Pregnancy loss affects approximately 10% to 30% of all clinically recognized pregnancies, with nearly 80% occurring in the first trimester. The majority of pregnancy losses are sporadic and result from genetic causes that are greatly influenced by maternal age.
Fewer than 5% of women will experience two consecutive pregnancy losses and only 1% experience three or more. Women with two prior losses and no live births experience a loss rate of 25%, which increases to 45% with three consecutive losses.
Evaluation of recurrent pregnancy loss should proceed after two consecutive clinical pregnancy losses and may include screening for genetic factors and antiphospholipid syndrome, assessment of uterine anatomy, and testing for hormonal and metabolic factors.
Treatment of recurrent pregnancy loss should be guided by underlying cause. Women with unexplained recurrent pregnancy loss should be offered psychological support and counseling and reassurance. More than 50% of patients with unexplained recurrent pregnancy loss achieve live birth with no intervention.
Cases in which women are diagnosed with early pregnancy loss can be managed surgically, with medication or expectantly. Studies have noted no difference in subsequent pregnancy rates, and the management choice is typically based on patient preference.
Pregnancy loss is by far the most common complication of pregnancy, affecting more than 20% of clinically recognized pregnancies, and is often physically and emotionally distressing. The terms spontaneous abortion, miscarriage, and pregnancy loss are used interchangeably in the literature ( ). Though used colloquially, for the purposes of this chapter, the term miscarriage will not be used because it imputes a failure on the part of the woman to properly carry the pregnancy. Early pregnancy loss is defined as a nonviable intrauterine pregnancy with either an empty gestational sac (anembryonic gestation, blighted ovum) or with a gestational sac containing an embryo or fetus without fetal heart activity within the first 12 6/7 weeks of gestation. Although the terms embryo and fetus are used synonymously, embryo is the correct term before 10 weeks’ gestation. Biochemical or chemical pregnancy loss refers to a loss that occurs after a positive beta–human chorionic gonadotropin (β-HCG) and before detection on ultrasound. After 20 weeks’ gestation, pregnancy loss is called an intrauterine fetal demise if no delivery or preterm birth or stillbirth if delivery occurred ( ).
In the past the terms threatened abortion, inevitable abortion , and missed abortion were used in reference to the appearance of the patient on presentation. Threatened abortion refers to patients with vaginal bleeding in the setting of a viable intrauterine pregnancy with a closed cervical os; inevitable abortion refers to patients with an open cervical os. The term missed abortion describes patients diagnosed with a loss of pregnancy without the passage of products of conception (POCs). These vague terms are no longer widely used because they often lead to confusion and do not affect the management options for pregnancy loss.
Recurrent pregnancy loss (RPL) traditionally has been defined as three or more consecutive, clinically recognized losses ( ). More recent definitions have recommended including two or more clinically recognized losses ( ). The term habitual abortion has now been almost completely replaced by RPL. In addition, RPL may be further stratified into primary or secondary . Primary RPL refers to pregnancy loss in women who have never carried to viability. In contrast, secondary RPL refers to pregnancy loss in a woman who has had a previous live birth. Nonconsecutive pregnancy loss describes women who have had multiple spontaneous pregnancy losses interspersed with normal pregnancies.
This chapter discusses the epidemiology, etiology, diagnosis, and management of pregnancy loss before 20 weeks’ gestation. Because pregnancy loss may occur spontaneously or as a result of a recurring cause, spontaneous early pregnancy loss and RPL are discussed throughout the chapter.
Pregnancy loss is common, affecting 10% to 30% of clinically recognized pregnancies ( ). Extremes of age increase the risk of pregnancy loss; loss is more common in women younger than 18 years and older than 35 years and rises both with increasing parity and number of prior losses ( Fig. 16.1 ). The loss rate is believed to approach 80% in women age 45 and older ( ).
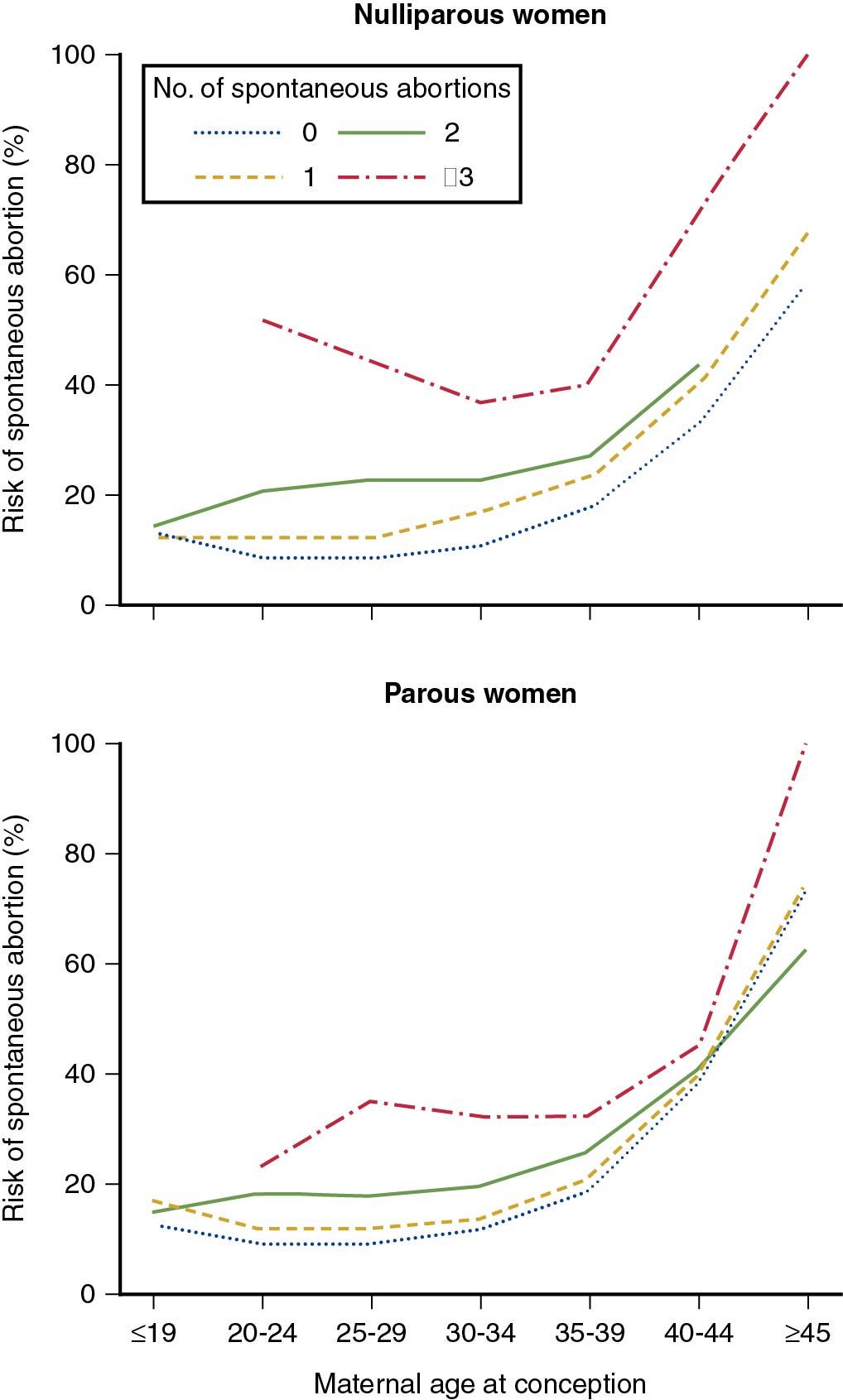
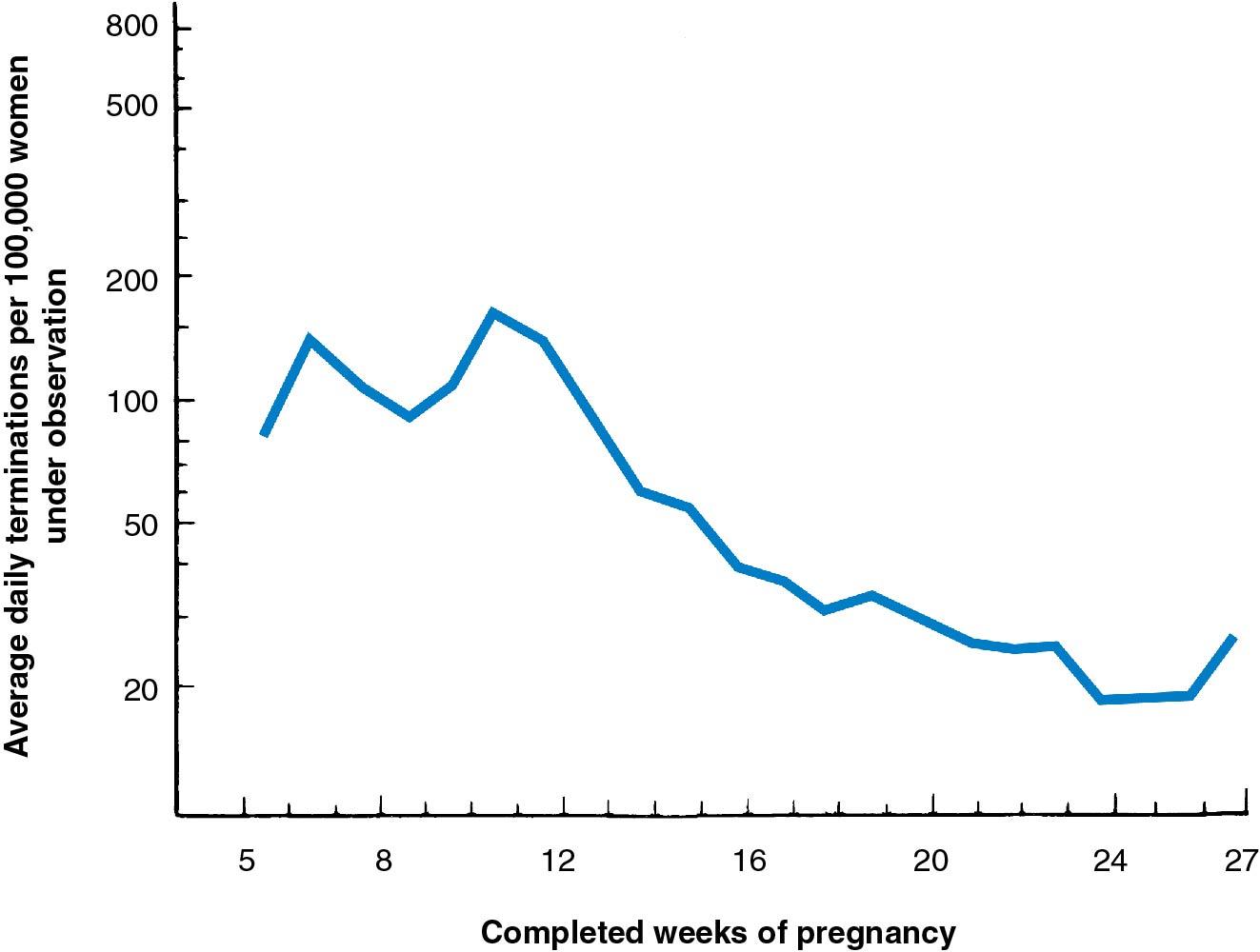
Nearly 80% of all pregnancy losses occur in the first trimester, and the incidence declines with advancing gestational age ( ) ( Fig. 16.2 ). The loss rate when a gestational sac is visualized by ultrasound is 11.5%; it falls to 6% to 8% if embryonic cardiac activity is observed at 6 weeks and falls to 2% to 3% if cardiac activity persists at 8 to 12 weeks. Compared with their younger counterparts, women older than age 34 experience a loss rate twice as high, even after visualization of a fetal heartbeat ( ). Women with bleeding in the first trimester and confirmed presence of fetal cardiac activity have a 15% risk of suffering a pregnancy loss ( ).
Evaluation of the medical literature should take into account that the majority of patients with a prior pregnancy loss will eventually have a successful pregnancy; a study of more than 53,000 parous women reported that 43% experienced one or more prior first trimester pregnancy losses ( ). Remembering that 90% of pregnancy losses are not recurrent, watchful waiting may prove the best, albeit emotionally the hardest thing to do.
Although sporadic pregnancy loss is common, fewer than 5% of women will experience two consecutive pregnancy losses, and only 1% experience three or more ( ). Women with two prior losses and no live births experience a loss rate of 25%, which increases to 45% with three consecutive losses ( ) ( Table 16.1 ).
| Number of Previous Pregnancy Losses | Number of Pregnancies Studied | Pregnancy Loss Risk (%) |
|---|---|---|
| 0 | 18,164 | 10.7 (10.3-11.2) |
| 1 | 21,054 | 15.9 (15.4-16.4) |
| 2 | 2,231 | 25.1 (23.4-27.0) |
| 3 | 353 | 45.0 (39.8-50.4) |
| 4 | 94 | 54.3 (43.7-64.4) |
| Overall | 19,737 | 11.3 (10.9-11.8) |
* The table is calculated from a 6.6% sample of the study pregnancies. Figures in parentheses: 95% confidence limits; χ 2 (trend) = 728; df = 1: P < .001.
Historically, RPL has been defined as three or more consecutive pregnancy losses. The American Society of Reproductive Medicine (ASRM) defines RPL as two or more failed clinical pregnancies, documented by ultrasonography or histopathologic examination, that are not necessarily consecutive ( ). For epidemiologic studies, however, ASRM recommends that ideally three or more losses be used as the threshold for RPL. The European Society of Human Reproduction Embryology (ESHRE) released a consensus statement in 2014 proposing that RPL describes repeated pregnancy loss, including nonvisualized pregnancy losses, but did not recommend a number of losses required to be defined as recurrent loss ( ). The rationale to include nonvisualized pregnancies (biochemical pregnancy losses and/or pregnancies of unknown location) in the definition of RPL comes from a retrospective cohort study of 587 women who had three or more consecutive pregnancy losses before 12 weeks of gestation ( ). Nonvisualized pregnancy losses had the same negative impact on future live birth as clinical pregnancy losses.
It is important to emphasize to patients with RPL that their overall prognosis is good, with more than 80% of women with RPL younger than 30 years and 60% to 70% of women with RPL ages 31 to 40 achieving a successful pregnancy within 5 years of their first visit to a physician ( ).
For a pregnancy to successfully progress to term, a remarkable number of biological processes and events must occur properly both in the embryo/fetus and mother; failure or deficiencies in any of these can result in a pregnancy loss. Thus the evaluation and management of a woman or couple with RPL is based on careful and systematic evaluation for those factors that can contribute to the loss, followed by targeted correction of any deficiencies. Most clinicians begin the diagnostic evaluation for RPL after two failed clinical pregnancies because one early pregnancy loss is relatively common. If a pregnancy loss occurs in the second trimester, the cause is more likely to recur . Thus a diagnostic evaluation should be considered after a woman has had only one second-trimester loss .
The evaluation for women with RPL starts with a history and physical examination, including pertinent questions regarding previous uterine instrumentation, menstrual regularity, exposure to environmental toxins, history of venous or arterial thrombosis, and family history of pregnancy losses or birth defects and open-ended questions that explore the patient’s ideas about causation. The history should include a description of the gestational age of all previous pregnancies because RPL typically occurs at a similar gestational age in consecutive pregnancies and the most common causes of RPL vary by trimester. For example, pregnancy losses related to chromosomal or endocrine defects tend to occur earlier in gestation compared with losses caused by anatomic or immunologic abnormalities. Physical examination should include a general physical assessment with attention to signs of endocrinopathy (e.g., galactorrhea) and uterine abnormalities (e.g., uterine septum, fibroids).
The patient’s history should be used to guide laboratory evaluation. Any history suggestive of thyroid disease may prompt studies for thyroid-stimulating hormone (TSH) level and the presence of antithyroid antibodies. Other studies may include laboratory testing for prolactin, hemoglobin A1C, and antiphospholipid antibodies. Anatomic causes of RPL can be diagnosed using a three-dimensional ultrasound or sonohysterography. POC cytogenetic testing should also be offered if available. If no other cause is identified, a parental karyotype should be performed to determine whether a balanced structural chromosomal abnormality exists. More controversial testing includes testing for ovarian reserve, inherited thrombophilias, autoantibodies, HLA typing, luteal phase progesterone, and sperm DNA fragmentation; routine cervical cultures; screening for diabetes; and endometrial biopsy. Table 16.2 lists the accepted basic diagnostic workup for RPL . A thorough evaluation, including genetic analysis, will reveal a cause of recurrent loss in approximately 90% of couples who seek treatment ( ).
| Investigation | American Society for Reproductive Medicine (ASRM) Recommendations | European Society of Human Reproduction and Embryology (ESHRE) Recommendations | Potential Treatment | Reference |
|---|---|---|---|---|
| Genetic analysis of pregnancy tissue | Recommend | Not routinely recommended; may be performed for explanatory purposes | Guide further investigation | |
| Parental karyotype | Recommend | Not routinely recommended; could be carried out after individual assessment of risk | Genetic counseling and information on preimplantation genetic testing | |
Uterine anatomy
|
Recommend | Recommend | Surgery for selective uterine abnormalities | |
Thyroid screening
|
Recommend | Recommend | Levothyroxine for hypothyroidism | |
| Prolactin screening | Recommend | Not routinely recommended; only if clinical symptoms of hyperprolactinemia (oligo/amenorrhea) | Bromocriptine for hyperprolactinemia | |
Insulin resistance
|
Recommend | Not recommended | Lifestyle and pharmacologic therapy for glycemic control | |
Antiphospholipid antibodies
|
Recommend after 3 unexplained losses before tenth week of gestation | Recommend after two pregnancy losses | Low-dose aspirin and a prophylactic dose heparin | |
Hereditary thrombophilia
|
Not recommended; only if personal history of thromboembolism or first-degree relative with high-risk thrombophilia | Not recommended; only with additional risk factors for thrombophilia | Anticoagulation | |
| Testing not routinely recommended: ovarian reserve, luteal phase insufficiency, alloimmune factors (anti-HY antibodies, natural killer cell testing, anti-HLA antibodies), infectious causes, sperm DNA fragmentation | ||||
Pregnancy loss may be caused by fetal and/or maternal factors. Fetal causes may be related to chromosomal, genetic, or structural abnormalities. Maternal factors include medical conditions such as endocrinopathies and certain thrombophilias, environmental exposures, and structural issues of the uterus. These categories can overlap; for example, maternal diabetes with poor glycemic control may cause a lethal heart defect in the fetus.
Chromosomal abnormalities are the most common cause of early pregnancy loss, accounting for approximately 50% to 60% of all pregnancy losses ( ). Pregnancy loss in the first trimester is more likely to be due to cytogenetic defects compared with losses in the second trimester ( ).
Chromosomal abnormalities can be classified into those caused by an abnormal number of chromosomes and those caused by abnormal chromosome structure. Most chromosomal abnormalities are numeric abnormalities resulting from errors during gametogenesis (chromosomal nondisjunction during meiosis), fertilization (triploidy as a result of digyny or diandry), or division of the fertilized ovum (tetraploidy or mosaicism). In a study using chromosomal microarray analysis, cytogenetic abnormalities were found in 59% of the 2389 post–pregnancy loss POC samples: aneuploidy accounted for 85%, triploidy for 10%, and structural anomalies or tetraploidy for the remaining 4% ( ). Unlike karyotyping, which requires live cells to culture, chromosomal microarray analysis (CMA) using single-nucleotide polymorphism (SNP)–based arrays can be performed on DNA extracted from formalin-fixed and paraffin-embedded (FFPE) tissues . A retrospective study of more than 7000 POC samples successfully analyzed 92% of fresh tissue samples and 86% of FFPE samples using CMA ( ). Clinically significant abnormalities were identified in 53.7% of specimens (3975 of 7396), 94% of which were considered causative of pregnancy loss.
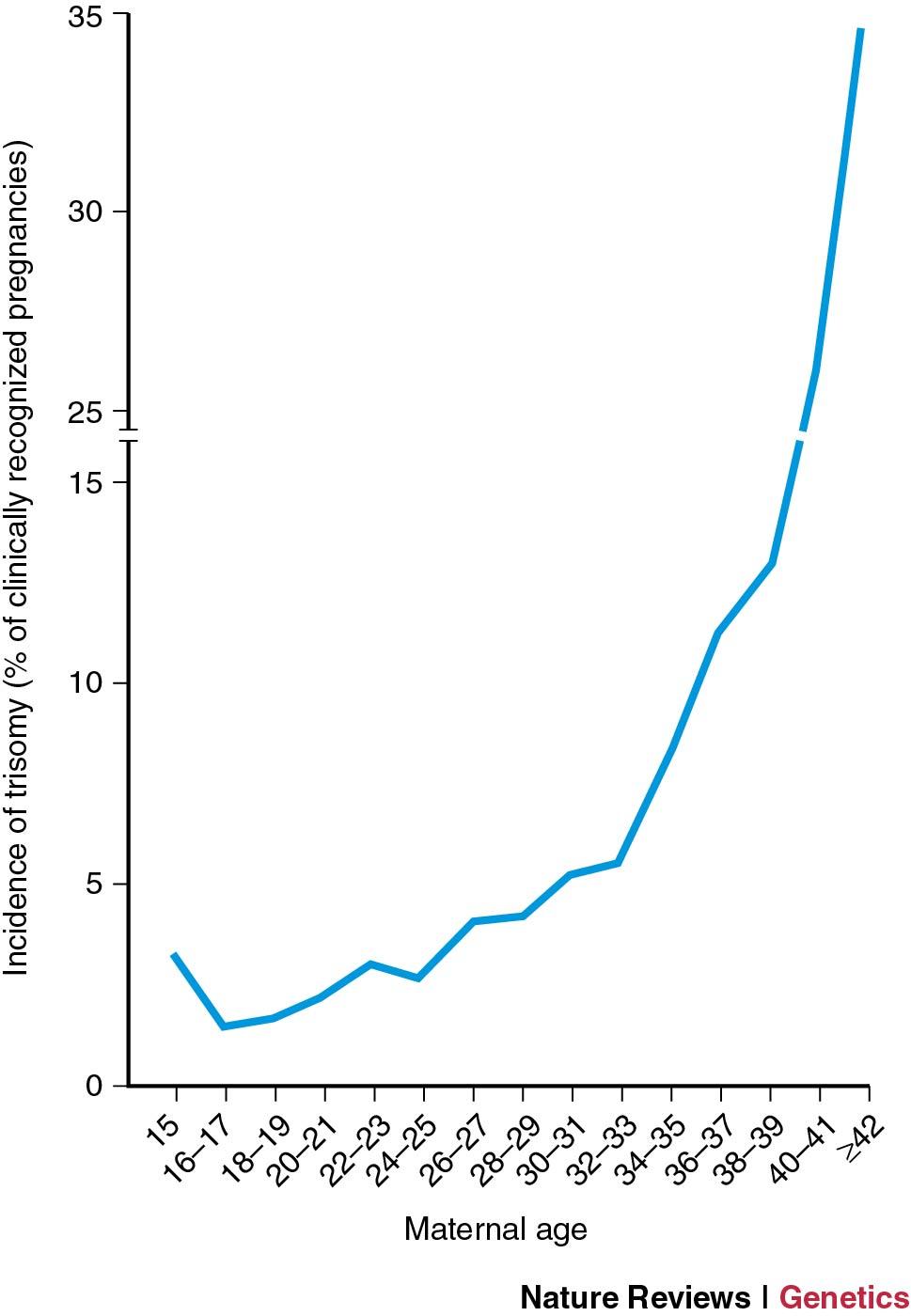
Aneuploidy is usually caused by errors in the first meiotic division of the oocyte, although some trisomies are due to errors in paternal meiotic division. Aneuploidies occur with increasing frequency as maternal age increases, though the rate is not linear, and the rate of increasing frequency of numeric anomalies increases with advanced maternal age ( ; ) ( Fig. 16.3 ). Trisomies represent the largest class of aneuploidies, with trisomy 16 being the most common autosomal trisomy followed by trisomy 22. While monosomy for autosomes is infrequent, monosomy X has been observed in 11.2% of chromosomally abnormal pregnancy losses ( ). However, nearly 1 in 300 monosomy X gestations will survive to viability ( ). Monosomy X is unique in being paternally derived in approximately 75% of cases ( ).
Most chromosomal abnormalities in the embryo arise de novo. Rarely the abnormality is inherited from a parent who may have a balanced chromosomal translocation. Couples with RPL should undergo peripheral karyotyping to detect any balanced structural chromosomal abnormalities. Of couples with RPL, 3% to 5% have a major chromosomal rearrangement (vs. 0.7% of the general population) ( ). About 50% of these rearrangements are balanced translocations, 25% are Robertsonian translocations, and another 12% are female sex chromosome mosaicism. The remainder of major chromosomal rearrangements are either inversions or other types of sporadic abnormalities. Balanced translocations are more common in women and more likely to result in a pregnancy loss if the translocation is of maternal origin . Genetic counseling is recommended when a structural genetic factor is identified. The likelihood of subsequent live birth depends on the chromosome(s) involved and the type of rearrangement. Large studies have shown spontaneous live birth rates of up to 71% in carriers of a structural rearrangement ( ). Preimplantation genetic testing (PGT), amniocentesis, and chorionic villus sampling are options to detect inherited genetic abnormalities in offspring.
In contrast to sporadic pregnancy losses, most RPLs are not caused by chromosomal abnormalities. Stephenson and colleagues analyzed 420 karyotypes of aborted pregnancy samples from 285 couples with RPL and found that 54% of recurrent losses had normal cytogenetic evaluations ( ) ( Table 16.3 ). In women younger than 36, recurrent loss primarily was due to causes other than chromosomal abnormalities. The American College of Obstetricians and Gynecologists (ACOG) and ASRM recommend chromosomal evaluation of POC samples as part of the clinical evaluation of couples with RPL ( ; ). Rescue karyotyping refers to the cytogenetic evaluation of archived POCs that have been formalin fixed and paraffin embedded and may be useful in cases where tissue has been collected but not cytogenetically tested ( ). By identifying the women whose pregnancy loss is due to a gross chromosomal abnormality, cytogenetic testing can prevent patients from undergoing costly and unnecessary evaluations , whereas a negative result warrants further evaluation of a variety of anatomic, endocrinologic, hematologic, and immunologic disorders.
| Diagnosis | Number of Pregnancy Losses | Frequency (%) |
|---|---|---|
| Euploid, female * | 120 | 29 |
| Euploid, male † | 105 | 25 |
| Trisomy 1 | 0 | 0 |
| Trisomy 2 | 4 | 0.95 |
| Trisomy 3 | 0 | 0 |
| Trisomy 4 | 1 | 0.24 |
| Trisomy 5 | 1 | 0.24 |
| Trisomy 6 | 3 | 0.7 |
| Trisomy 7 | 3 | 0.7 |
| Trisomy 8 | 4 | 0.95 |
| Trisomy 9 | 4 | 0.95 |
| Trisomy 10 | 1 | 0.24 |
| Trisomy 11 | 1 | 0.24 |
| Trisomy 12 | 1 | 0.24 |
| Trisomy 13 | 11 | 2.6 |
| Trisomy 14 | 11 | 2.6 |
| Trisomy 15 | 22 | 5.2 |
| Trisomy 16 | 19 | 4.5 |
| Trisomy 17 | 2 | 0.48 |
| Trisomy 18 | 4 | 0.95 |
| Trisomy 19 | 0 | 0 |
| Trisomy 20 | 2 | 0.48 |
| Trisomy 21 | 11 | 2.6 |
| Trisomy 22 | 16 | 3.8 |
| Double trisomy | 9 | 2.1 |
| Sex trisomy (47,XXY) | 1 | 0.24 |
| Monosomy X (45,X) | 18 | 4.3 |
| Monosomy X and trisomy 21 | 1 | 0.24 |
| Triploidy | 27 | 6.4 |
| Tetraploidy | 10 | 2.4 |
| Unbalanced translocations | 8 | 1.9 |
| Total | 420 | 100 |
* Consisting of 118 cases of 46,XX and two cases of balanced translocations.
Uterine abnormalities, either congenital or acquired, may not provide the optimal environment for the developing embryo and thus may result in the loss of a genetically normal embryo.
Women with uterine anomalies have higher rates of first and second-trimester pregnancy losses compared with women with a normal uterus . Uterine anomalies are present in approximately 12.6% of patients (range, 1.8% to 37.6%) with RPL compared with 4.3% of the general population (range, 2.7% to 16.7%) ( ). The wide range reflects the differences in diagnostic and imaging techniques used. Several imaging modalities may be used to evaluate the uterus, including hysterosalpingogram, transvaginal ultrasonography, and sonohysterography. Magnetic resonance imaging (MRI) and three-dimensional transvaginal ultrasonography may help better characterize the anomaly.
The septate uterus is the most common uterine anomaly in the general population and is also associated with poorest reproductive outcomes. Composed of fibromuscular tissue, the septum has a decreased blood supply, which may lead to poor implantation, resulting in early pregnancy loss. Later in gestation, the septum may compromise available space for growth, leading to pregnancy loss, malpresentation, or preterm term birth. Other congenital anomalies associated with pregnancy loss include unicornuate, didelphys, and bicornuate uteruses ( ).
Hysteroscopic septum incision, or metroplasty, is the treatment of choice for women with a septate uterus and a history of pregnancy loss. A large meta-analysis found that hysteroscopic resection of the uterine septum increased live birth rates from 6.1% before surgery to 83.2% after metroplasty. However, many of the retrospective studies included in this meta-analysis used patients as their own controls, which limits the interpretation of these results. The benefits of hysteroscopic metroplasty have not yet been assessed by a prospective randomized trial. In cases of bicornuate uterus, metroplasty may be performed transabdominally or laparoscopically but has not been shown to increase the live birth rate. Thus metroplasty is not recommended for women with bicornuate uterus . Uterine reconstruction is not feasible for the unicornuate uterus.
Fibroids are common benign uterine tumors that are present in more than one-third of women of reproductive age ( ). The size and location of the fibroid is an important factor in determining the risk posed. Submucosal fibroids protrude into and distort the endometrial cavity and can increase the risk of pregnancy loss, possibly as a result of abnormal vascularization, impaired uterine contractility, and rapid distention of the uterus early in pregnancy. An association between pregnancy loss and intramural and subserosal myomas is less clear. Subserosal fibroids with greater than 50% of their mass outside the myometrium are unlikely to cause adverse pregnancy outcomes. The role of intramural fibroids in pregnancy is controversial ( ; ).
A meta-analysis of 23 studies (including 1 randomized trial) found the spontaneous pregnancy loss rate to be higher in women with submucosal or intramural fibroids with an intracavitary component ( ). Studies of women with fibroids that did not distort the uterine cavity have also shown an increased risk of pregnancy loss; however, these studies may have included women with fibroids with intracavitary distortion that was missed on imaging studies such as a hysterosalpingogram or an ultrasound.
Myomectomy is recommended for women with RPL and a fibroid that is submucosal or intramural with an intracavitary portion. Studies have shown a decrease in pregnancy loss rate after a myomectomy. In a large review published in 1981, Buttram and Reiter reported that among 1941 women, an abdominal myomectomy reduced the rate of pregnancy loss from 41% to 19% ( ). A smaller 2004 study by Marchionni and colleagues showed that pregnancy loss rates decreased from 69% to 25% after a myomectomy ( ). Hysteroscopic myomectomy is the procedure of choice for submucosal myomas. With advances in laparoscopic suturing, most myomectomies for intramural fibroids may be performed laparoscopically. An abdominal myomectomy may be performed when there are multiple intramural fibroids or when the uterus is significantly enlarged.
Endometrial polyps are a relatively common acquired anomaly, with an incidence of 7.8% to 34.9% ( ; ). Observational studies have reported improved spontaneous pregnancy rates after hysteroscopic polypectomy ( ; ), possibly because of changes in endometrial receptivity ( ). A 2019 systematic review showed that hysteroscopic resection of endometrial polyps was associated with an increased rate of clinical pregnancy in patients who underwent intrauterine insemination (IUI) ( ). However, clinical pregnancy and miscarriage rates were not improved in patients undergoing in vitro fertilization (IVF) cycles. Thus the effect of hysteroscopic polypectomy on pregnancy outcomes remains unclear . Although there are no adequate studies showing a benefit for polypectomy in RPL, given the underlying premise of restoring anatomy to normal and the low risk associated with polypectomy, removal of polyps may be considered in women with RPL ( ).
Intrauterine adhesions (IUAs), or synechiae, are scar tissue within the uterine cavity and are referred to as Asherman syndrome when associated with symptoms such as amenorrhea, infertility, or pregnancy loss. Pregnancy loss is thought to be a result of insufficient endometrium to support fetoplacental growth.
Adhesions are commonly caused by previous intrauterine surgery ( Table 16.4 ). Any intrauterine surgery may traumatize the basalis layer of the endometrium, which then heals by forming granulation tissue. Granulation tissue on opposing walls of the uterus can fuse, forming filmy adhesions composed of endometrial tissue and dense adhesions consisting entirely of connective tissue. These adhesions may result in partial or complete obliteration of the uterine cavity.
| Condition | Procedure | Incidence | Reference |
|---|---|---|---|
| G ravid | |||
| SAB | Suction D&C | 15% 19% |
|
| First trimester TOP | Suction D&C | 21% | |
| Retained POC | Hysteroscopic resection Suction D&C |
6% 13% 19% 30% |
Smorgick, 2014
|
| G ynecologic | |||
| Septum | Hysteroscopic septum resection (bipolar) | 24% | |
| Fibroids | Hysteroscopic myomectomy (bipolar) Abdominal myomectomy |
8% 22% |
Postpartum complications such as hemorrhage or retained placenta are major risk factors for adhesion formation. A greater number of intrauterine surgical procedures increases the risk of IUA formation. In a meta-analysis of 10 prospective studies, the risk of IUA development was 2.1-fold higher for two or more curettage procedures compared with one curettage procedure ( ). Adhesions can also form in a nongravid uterus as a result of procedures that injure the endometrium such as a myomectomy. In a study by Taskin and coworkers, hysteroscopic resection of multiple submucosal leiomyomas had the highest risk of IUA formation compared with other hysteroscopic procedures ( ).
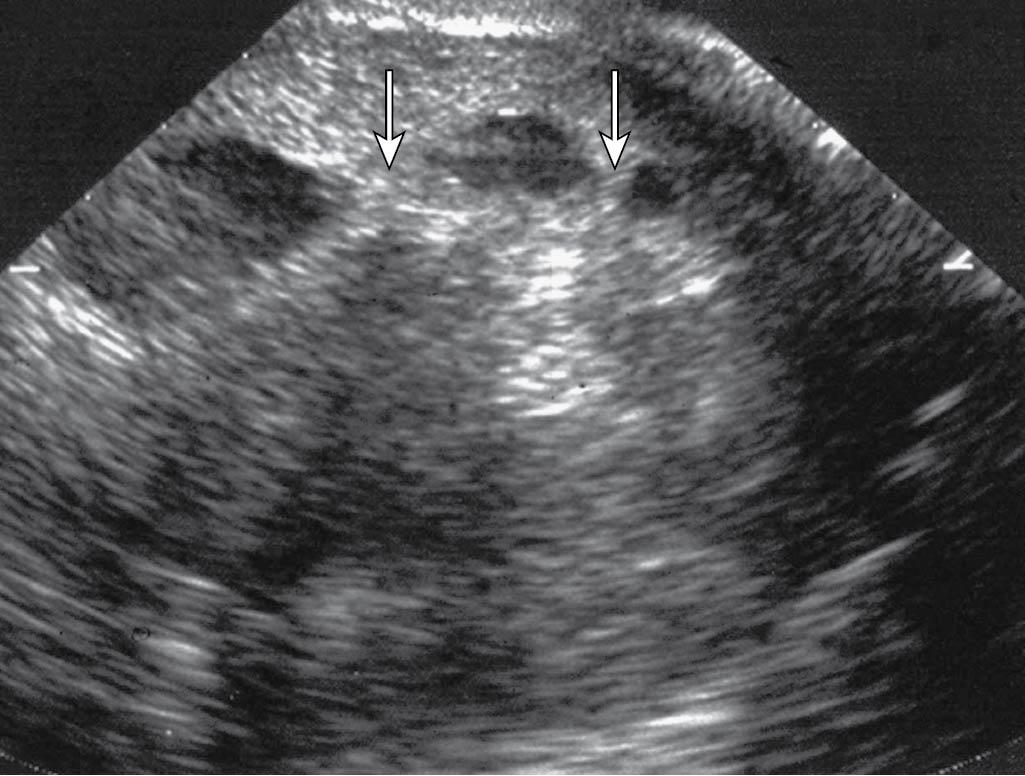
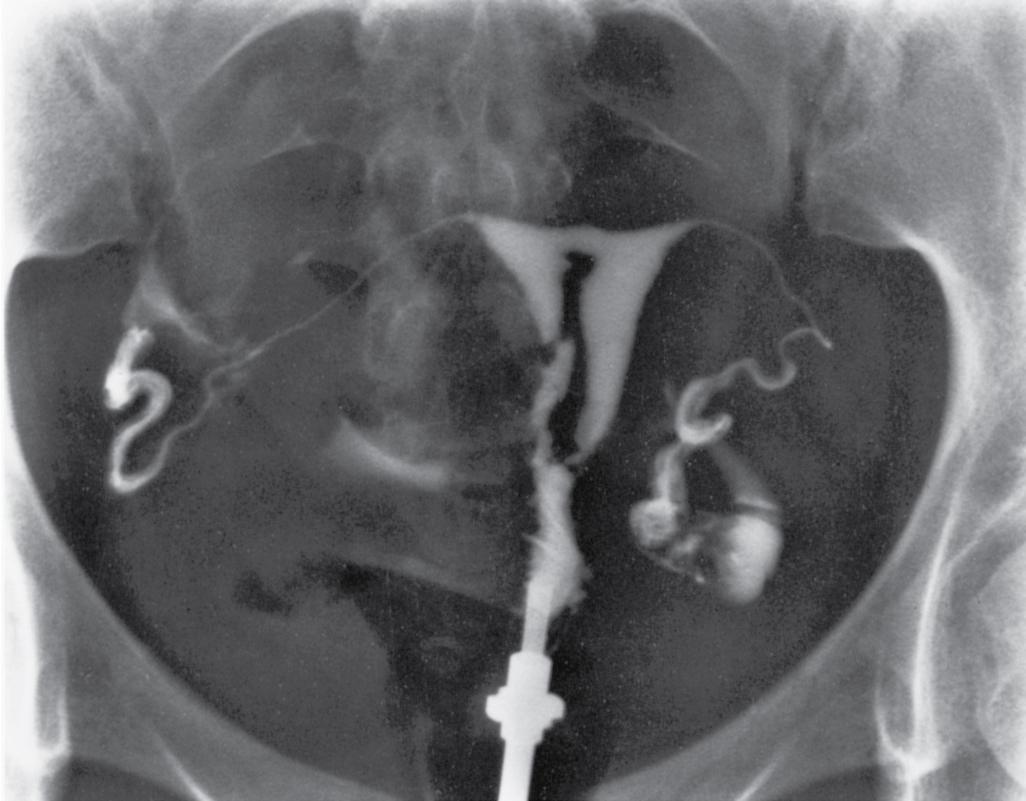
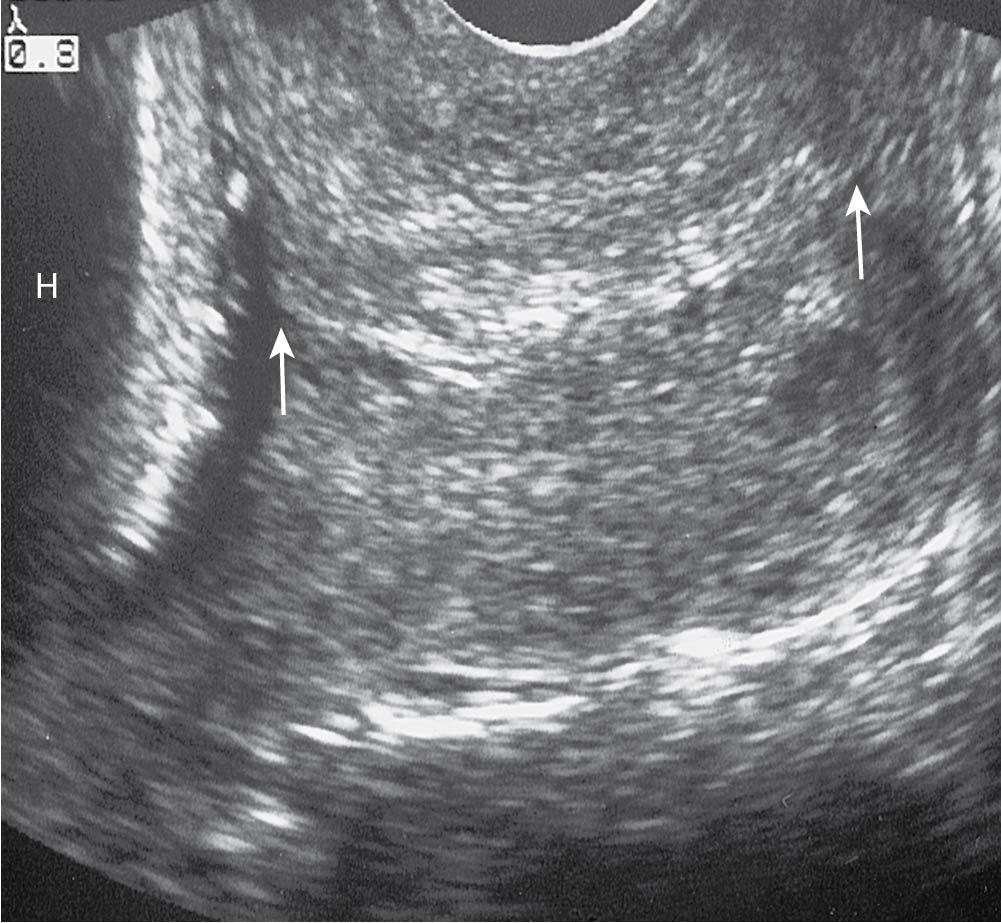
Suspected IUAs may be seen in imaging studies such as ultrasound, saline infusion sonogram ( Fig. 16.4 ), and hysterosalpingogram ( Fig. 16.5 ). On hysterosalpingogram, the defects are typically irregular, with sharp contours and homogeneous opacity that persist in multiple views. The diagnosis is best confirmed and treated by hysteroscopy ( ).
The recommended treatment for symptomatic IUA is hysteroscopic lysis of the adhesions . The goal of surgery is to restore the size and shape of the uterine cavity. Unfortunately, adhesion recurrence rates have been reported to be as high as 30% to 66% after surgical lysis ( ). The prevention of adhesion recurrence is challenging, and no single method has shown superiority ( ). Suggested postlysis management approaches include placement of a mechanical barrier such as a pediatric balloon in the intrauterine cavity, postoperative treatment with estrogen and timed progestin therapy, and a repeat hysteroscopy ( ). In a meta-analysis of trials comparing multiple types of antiadhesion therapies with placebo or no intervention, treatment did not affect the subsequent live birth rate (odds ratio [OR], 0.99; 95% confidence interval [CI], 0.46 to 2.13; 3 studies, 150 women), although antiadhesion therapy was associated with fewer recurrent IUAs at the time of a second-look hysteroscopy (OR, 0.36; 95% CI, 0.20 to 0.64; 7 studies, 528 women) ( ). In women with severe IUAs, we suggest repeating an office hysteroscopy after the initial surgery . At that point, any new adhesions will be filmy and can be gently taken down. This process can then be repeated until the cavity has fully healed from surgery.
Gel barriers and regenerated cellulose adhesions barriers (Interceed) have also been investigated to reduce the recurrence of adhesions. Although studies have suggested that gel barriers (hyaluronic acid gel and polyethylene oxide-sodium carboxymethylcellulose) have a role in preventing IUA reformation ( ; ), a meta-analysis reported no definitive conclusion could be made because of the heterogeneity of study designs and lack of reproducibility of the study results ( ). Because the optimal approach to the prevention of IUAs is not yet known, the discussed treatment options are reasonable alternatives.
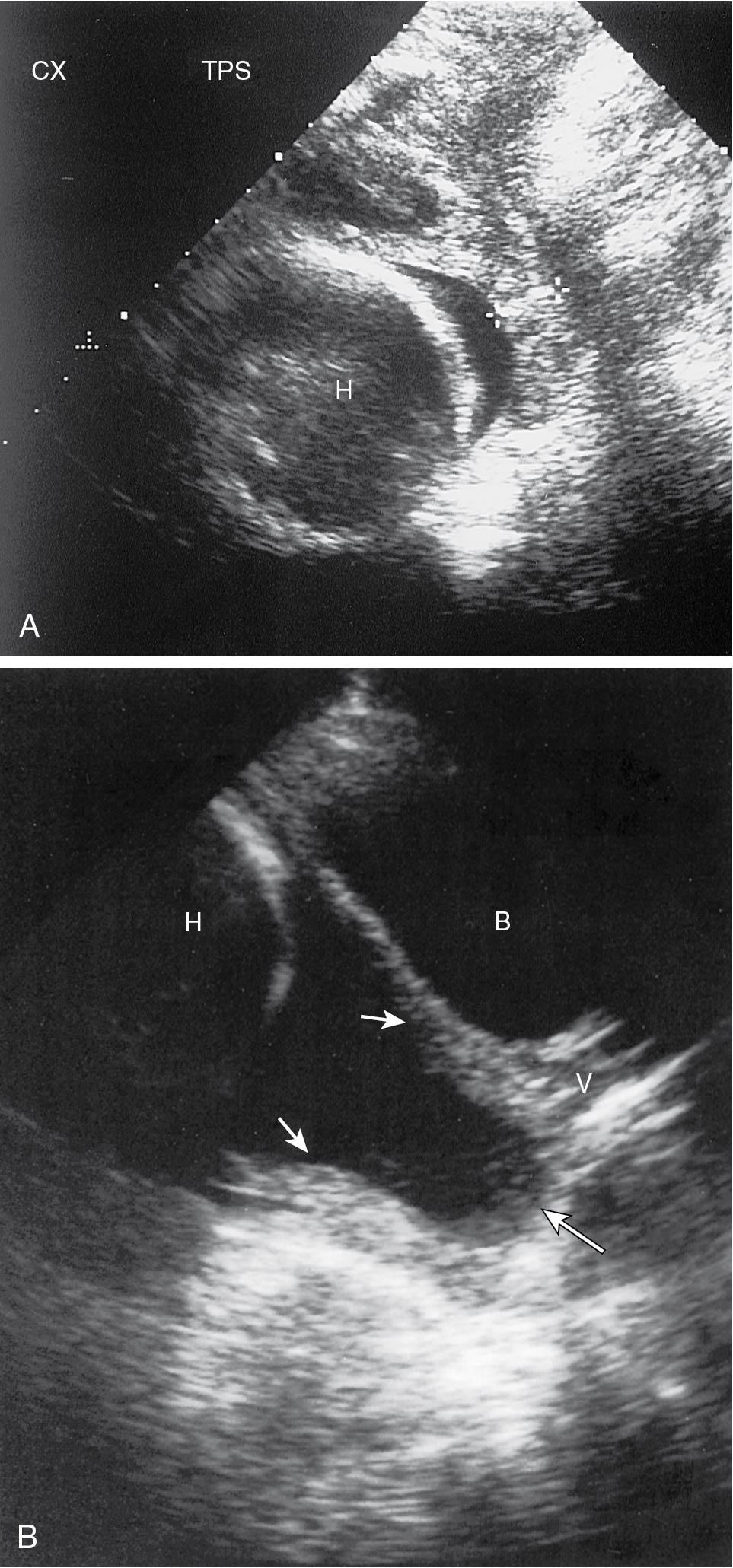
Cervical incompetence is characterized by an asymptomatic dilation of the internal cervical os, leading to dilation of the cervical canal during the second trimester ( Figs. 16.6 and 16.7 ). Cervical abnormalities, either congenital or as a result of trauma, are risk factors for structural cervical weakness.
Cervical trauma may result from treatment of cervical intraepithelial neoplasia such as conization or loop electrosurgical excision procedures, rapid mechanical dilation before a gynecologic procedure, and obstetric lacerations. Congenital abnormalities that have been associated with cervical weakness include uterine anomalies, genetic disorders affecting collagen (e.g., Ehlers-Danlos syndrome), and in utero diethylstilbestrol exposure. Cervical insufficiency may be a cause of recurrent second-trimester loss but is not typically associated with early pregnancy loss.
Progesterone is required for implantation and maintenance of pregnancy; therefore disorders related to impaired progesterone are likely to affect pregnancy success. For the first 7 weeks of gestation, progesterone is produced by the corpus luteum and maintains the endometrium.
After the corpus luteum regresses, progesterone is synthesized by the trophoblast and maintains the decidual tissue. If progesterone secretion from the corpus luteum is low or if the endometrium has inadequate response to normal circulating levels of progesterone, endometrial development may be unable to support the implanted blastocyst, leading to pregnancy loss.
There is no consensus on the best method of diagnosis or treatment for luteal phase deficiency ( ). The diagnosis of luteal insufficiency historically was made by performing a histologic examination of the endometrium; however, histologic dating of the endometrium has proven unreliable and not reproducible ( ). Similarly, the measurement of progesterone levels in the luteal phase is not considered a reliable diagnostic test. There is no standard progesterone value that defines normal luteal function because the corpus luteum varies from cycle to cycle in a normal fertile woman . In a 2015 committee opinion, the ASRM concluded “there is no reproducible, pathophysiologically relevant, and clinically practical standard to diagnose luteal phase deficiency and distinguish fertile from infertile women” ( 2015). Therefore we do not recommend performing luteal phase testing.
Abnormal luteal phase progesterone production may also occur as a result of medical conditions such as elevated prolactin or abnormal thyroid function and treatment of the underlying condition is recommended.
Risk of pregnancy loss is increased in women with poorly controlled thyroid disease, including hypo- and hyperthyroidism. Studies have also shown that subclinical hypothyroidism (SCH), defined as TSH greater than 4 mIU/L, is associated with pregnancy loss and treatment with levothyroxine improves pregnancy rates and decreases the rate of pregnancy loss. A meta-analysis of 18 cohort studies by Maraka and colleagues reported that SCH doubles the risk of pregnancy loss compared with euthyroid women ( ). The normal reference range for TSH changes in pregnancy. The upper limit of normal in most laboratories is 4 mIU/L for nonpregnant women and 2.5 mIU/L during the first trimester of pregnancy. The use of the first trimester pregnancy thresholds to diagnose and treat subclinical hypothyroidism in women attempting pregnancy remains controversial. According to the ASRM, if TSH levels before pregnancy are between 2.5 and 4 mIU/L, management options include either monitoring levels and treating when TSH is 4 mIU/L or greater or treating with levothyroxine to maintain TSH at 2.5 mIU/L or less ( ). The Endocrine Society recommends that patients with RPL be treated to keep a TSH level between 1 and 2.5 mIU/L. Once pregnant, women being treated for hypothyroidism often require an increase in thyroxine during pregnancy, beginning as early as the fifth week of pregnancy.
Studies regarding treating euthyroid patients with positive thyroid antibodies are conflicting. A large randomized controlled trial of 952 euthyroid women with positive antithyroid antibodies showed no benefit when treated with levothyroxine ( ). Routine screening for antithyroid antibodies in women with RPL is not currently recommended but may be considered if repeated TSH values are 2.5 mIU/L or more or when other risk factors for thyroid disease are present.
Hyperprolactinemia has been associated with pregnancy loss. Elevated levels of prolactin can alter the hypothalamic-pituitary axis, resulting in impaired folliculogenesis, decreased oocyte maturation, and a short luteal phase. Normalization of prolactin levels with a dopamine agonist improves pregnancy outcomes in women with RPL . In a randomized controlled trial, 64 hyperprolactinemic women with RPL were randomly assigned bromocriptine therapy or no bromocriptine; treatment resulted in an 85.7% live-born rate compared with 52.4% in the untreated group ( ). Prolactin levels in early pregnancy were significantly greater in women who miscarried.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here