Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Disorders of mineral metabolism (calcium, phosphorus, magnesium) are common, especially in hospitalized patients. The extracellular concentrations of these ions are less than 1% of total body stores, and the principal site of storage is bone. Thus, serum levels may not always reflect underlying pathology. Knowledge of the complex homeostasis of these ions is critical in formulating the differential diagnosis of disorders affecting these ions and in directing appropriate treatment. This regulation occurs in four major target organs (intestine, kidney, parathyroid glands, and bone) via the complex integration of four hormones (parathyroid hormone [PTH], vitamin D and its derivatives, fibroblast growth factor 23 [FGF23], and α-klotho, hereafter called klotho ). An understanding of normal physiology is necessary to accurately diagnose and treat disorders of calcium, phosphorus, and magnesium.
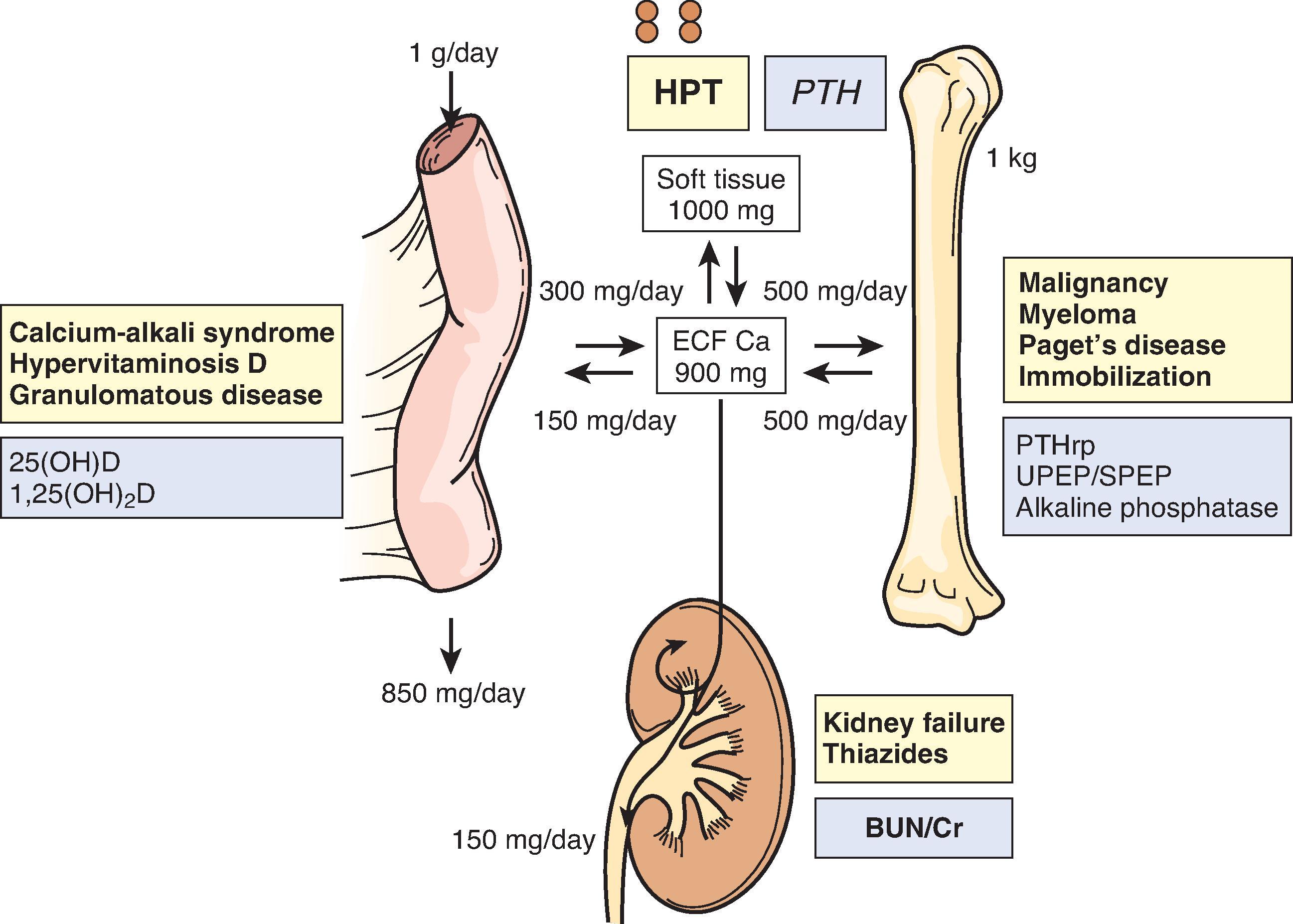
PTH is released in response to hypocalcemia ( Fig. 11.1 ) and maintains calcium homeostasis by three mechanisms: (1) increasing bone mineral dissolution, thus releasing calcium and phosphorus; (2) increasing kidney reabsorption of calcium and excretion of phosphorus; and (3) enhancing the gastrointestinal absorption of both calcium and phosphorus indirectly through its effects on the synthesis of 1,25(OH) 2 -vitamin D. In healthy individuals, the increase in serum PTH level in response to hypocalcemia effectively restores serum calcium levels while maintaining normal serum phosphorus levels.
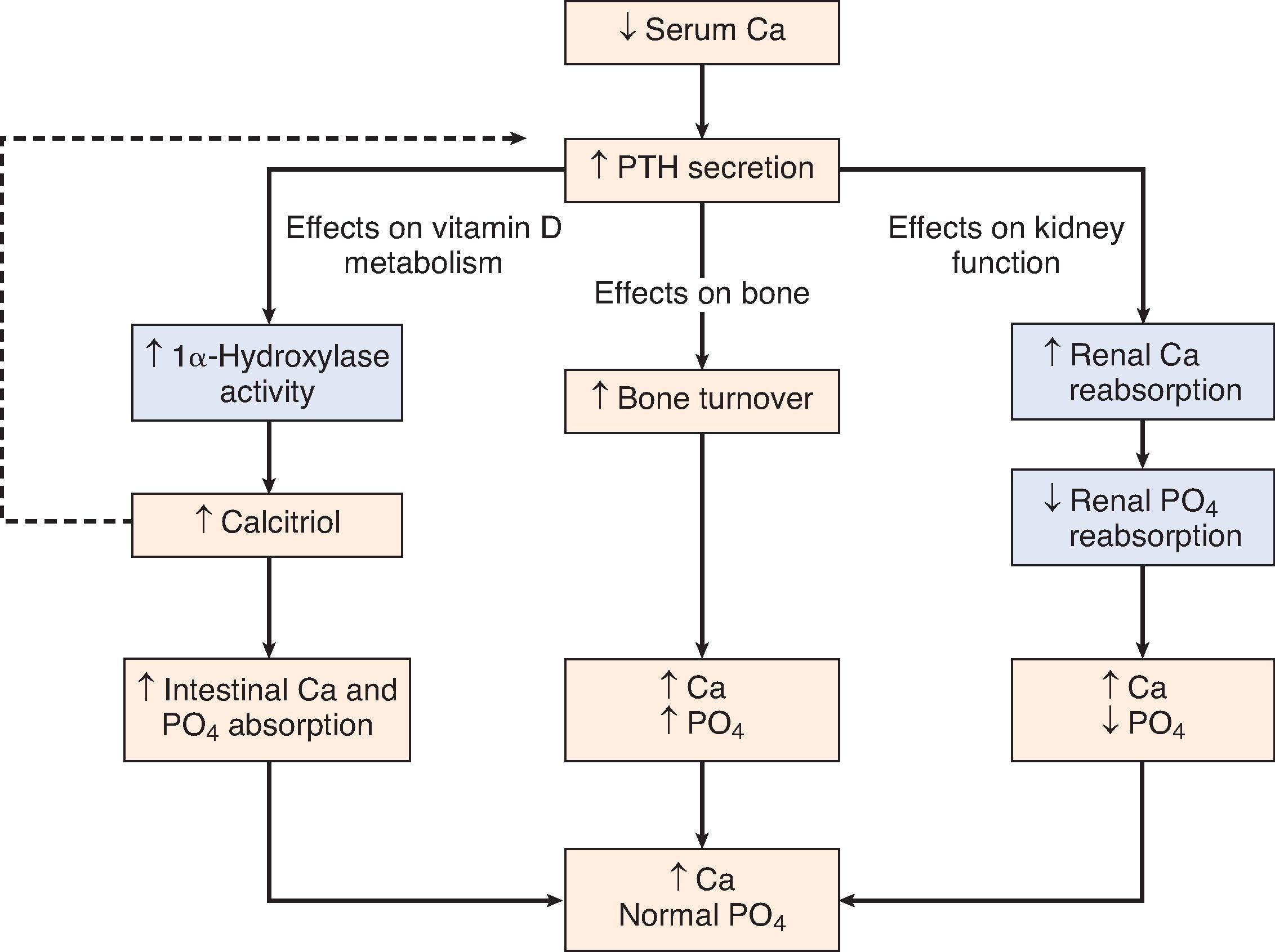
PTH enhances the conversion of 25(OH)-vitamin D [calcidiol] to 1,25(OH) 2 -vitamin D [calcitriol], with the latter decreasing PTH secretion at the level of the parathyroid glands and completing a typical endocrine feedback loop. In primary hyperparathyroidism, PTH is secreted autonomously from adenomatous glands without regard to physiologic stimuli. In contrast, in secondary hyperparathyroidism, the glands initially respond appropriately to low levels of ionized calcium; however, after a prolonged period of chronic kidney disease (CKD) and secondary hyperparathyroidism, the hyperplastic glands become adenomatous and therefore unresponsive to stimuli that would normally suppress PTH secretion (sometimes called tertiary hyperparathyroidism ). After entering the circulation, PTH binds to PTH receptors located throughout the body. Therefore, disorders of PTH excess or insufficiency not only affect serum levels of calcium and phosphorus but also lead to bone, cardiac, skin, and neurologic manifestations.
PTH is cleaved from a precursor preprohormone to an 84-amino-acid protein in the parathyroid gland, where it is stored with other PTH-protein fragments in secretory granules for release. After release, the circulating 84-amino-acid protein has a half-life of 2 to 4 minutes. It is then further cleaved into N-terminal, C-terminal, and mid-region fragments of PTH, which are finally metabolized in the liver and kidneys. PTH secretion can be triggered by hypocalcemia, hyperphosphatemia, or calcitriol deficiency, whereas profound hypomagnesemia can reduce PTH release. The extracellular concentration of ionized calcium is the most important determinant of temporal PTH levels. Active secretion of PTH from stored granules in response to hypocalcemia is controlled by the calcium-sensing receptor (CaSR), and mutations of the CaSR gene can lead to syndromes of hypercalcemia or hypocalcemia through dysregulated PTH release. The CaSR is expressed in thyroid C-cells and in the kidney, where it controls excretion of calcium in the thick ascending limb of the loop of Henle in response to changes in serum calcium concentration.
Through the years, a succession of increasingly sensitive assays has been developed to measure PTH. A major difficulty in measuring PTH accurately with the first-generation assay is the cross-reactivity with inactive, circulating PTH-protein fragments that may accumulate in CKD. These early assays targeted the C-terminus but were inaccurate in patients with kidney disease because of accumulation of these fragments. Subsequent N-terminus assays resulted in similar problems. Accuracy was improved by the development of a second-generation two-site antibody test (commonly called the “INTACT” assay) to detect full-length (1–84, or active) PTH molecules. In this assay, a capture antibody binds to the N-terminus, and a second antibody binds to the C-terminus. However, because the N-terminal antibody is at amino acid 7 instead of amino acid 1, this intact assay still detects some retained C-terminal fragments, albeit less than the older assays. These fragments accumulate in CKD, leading to falsely elevated values in assays of intact PTH such that values above the normal range are associated with complications of hypoparathyroidism at the level of bone. A third-generation assay was developed, which directed antibody binding to the proximal N-terminus portion 1-4 of the PTH molecule thought to be the most “biologically active” while not binding to PTH fragments. It detects 95% of circulating PTH in patients with normal kidney function and 85% in patients with CKD, as compared to 80% and 50%, respectively, with the second-generation assay. However, given the widely available and more robustly evaluated second-generation assay, the 2017 Kidney Diseases Improving Global Outcomes (KDIGO) guidelines continue to suggest using the second-generation assay for PTH monitoring. Additionally, it is recommended to use the same lab for all PTH assays and evaluating trends in PTH levels rather than isolated values.
Vitamin D is called a “vitamin” because it is an essential nutrient that must come from an exogenous source if it cannot be endogenously manufactured in sufficient quantity; however, this is a misnomer, because vitamin D is a hormone that can be synthesized in the skin. Vitamin D 2 (ergocalciferol) from plants and vitamin D 3 (cholecalciferol) primarily from oily fish are the main exogenous sources in a Western diet outside of supplementation in food products. In the skin, 7-dehydrocholesterol is converted to vitamin D 3 in response to sunlight, which is inhibited by sunscreen of skin protection factor (SPF) 8 or greater. After entering the blood, vitamins D 2 and D 3 from diet or skin bind to vitamin D–binding protein and are carried to the liver, where they are hydroxylated to yield 25(OH)D, often called calcidiol ; accordingly, blood calcidiol levels are a direct assessment of the nutritional (dietary) intake and skin conversion of vitamin D. Some clinical assays measure hydroxylated forms of both D 2 and D 3 , whereas others measure the total level of 25(OH)D (D 2 + D 3 ). 25(OH)D (calcidiol) is then converted in the kidney to 1,25(OH) 2 D (calcitriol) by the action of 1α-hydroxylase (the CYP27B1 isoenzyme of the cytochrome P-450 system). In the kidney, CYP27B1 activity is affected by almost every hormone involved in calcium homeostasis. Its activity is stimulated by PTH, estrogen, calcitonin, prolactin, growth hormone, low serum calcium, and low serum phosphorus, and inhibited by calcitriol and FGF23 providing feedback loops of regulation. FGF23 also stimulates CYP24, leading to accelerated degradation of both calcidiol and calcitriol, and thus contributing to the known vitamin D deficiency of CKD.
Calcitriol circulates in the bloodstream bound to vitamin D–binding protein. The free form of 1,25(OH) 2 D enters the target cell, where it interacts with its nuclear vitamin D receptor (VDR). This complex then combines with the retinoic acid X receptor to form a heterodimer, which in turn interacts with the vitamin D response element (VDRE) on the target gene. The major functions of 1,25(OH) 2 D are carried out in three target organs: (1) the small intestine, where it regulates the intestinal absorption of calcium and, to a lesser degree, phosphorus and possibly magnesium; (2) the parathyroid gland, where it inhibits PTH synthesis at the level of messenger RNA transcription; and (3) the osteoblast/osteocytes in bone, where it directly stimulates the secretion of FGF23. Importantly, the kidney CYP27B1 is essential for the feedback loops between calcitriol and both PTH and FGF23.
In addition to the role of vitamin D in mineral metabolism, the VDR is expressed in multiple organs, and 1α-hydroxylase activity can be detected in extrarenal tissues including immune cells, muscle cells, and myocardiocytes. Both 25(OH)D and 1,25(OH) 2 D can be taken up by extrarenal cells, with the former then converted intracellularly to 1,25(OH) 2 D. These features may mediate autocrine or paracrine effects of vitamin D outside its classic target tissues, especially effects on cell differentiation and proliferation and immune function. Recent studies in both normal and CKD patients have demonstrated widespread vitamin D (calcidiol) insufficiency and deficiency. Low levels of this precursor to calcitriol are associated with hyperparathyroidism, falls, fractures, cardiovascular disease, mortality, and cancers in the general population. However, repletion has not yet been shown to improve clinical outcomes in CKD.
FGF23 is a phosphatonin, which is a group of proteins that were identified from the study of genetic disorders characterized by hypophosphatemia from urinary phosphate wasting and cases of FGF23-producing tumor-induced osteomalacia associated with urinary phosphate wasting. FGF23 is made by osteocytes, a subgroup of osteoblasts that are interconnected through a series of canaliculi within cancellous (trabecular) bone. FGF23 directly inhibits the conversion of 25(OH)D to 1,25(OH) 2 D through downregulation of the CP27B1 in the kidney and increases the catabolism of both forms of vitamin D through stimulation of CYP24. FGF23 also inhibits PTH, while 1,25(OH)D and PTH stimulate FGF23, completing a feedback loop ( Fig. 11.2 ). Thus, FGF23 provides the key PTH-bone link and kidney-bone link. Levels of FGF23 are elevated as early as CKD stage 2 and are associated with left ventricular hypertrophy and increased mortality. In the kidney, FGF23 acts through the FGF receptor and its coreceptor klotho; however, in cardiomyocytes, FGF23 acts independently of klotho. In addition to FGF23, there are other phosphatonins, such as matrix extracellular phosphoglycoprotein (MEPE), that may provide an intestine-kidney link.
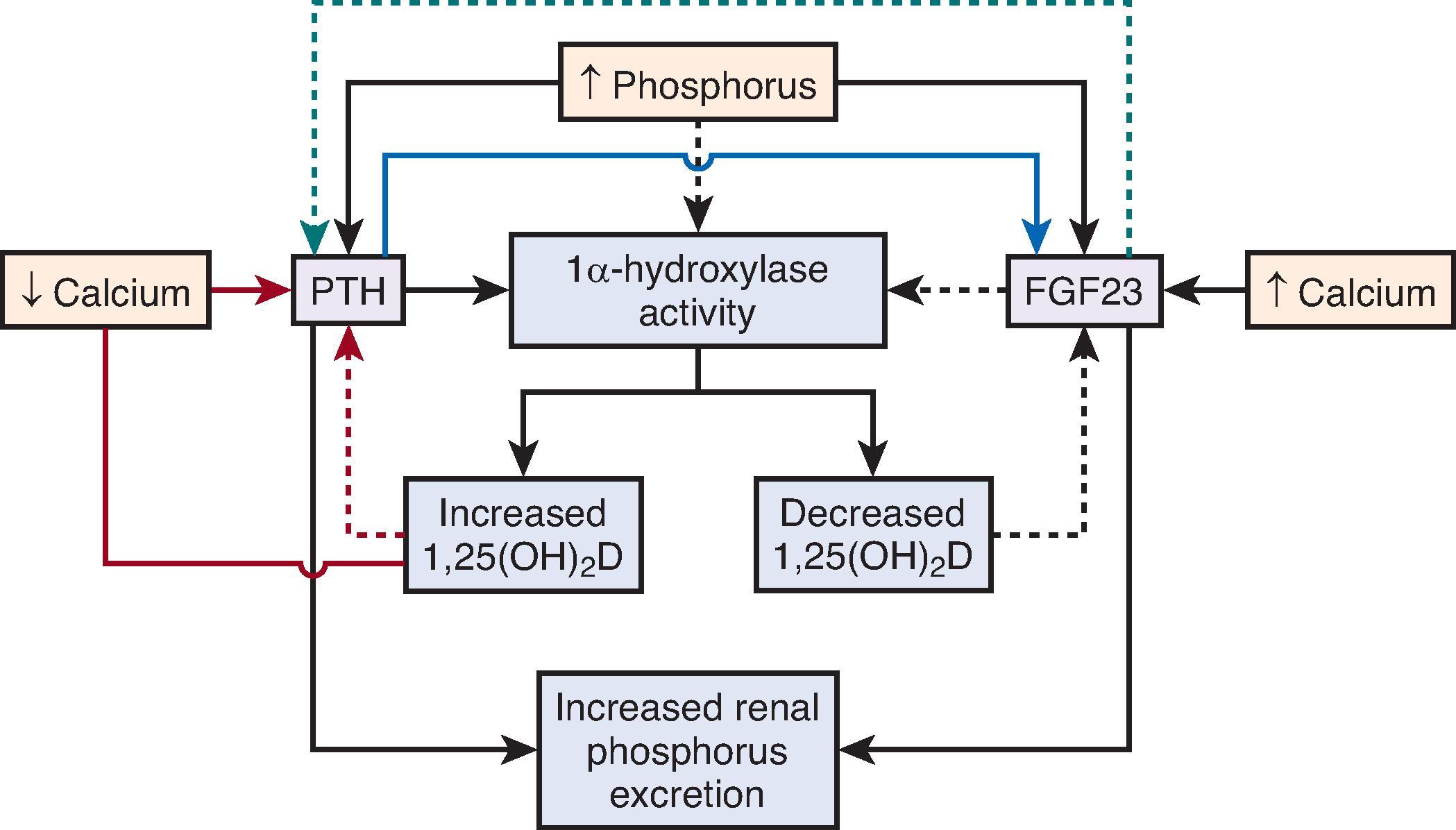
Alpha-klotho null mice have apparent premature aging: early demise, infertility, arteriosclerosis and arterial calcification, osteoporosis, hyperphosphatemia, emphysema, and skin atrophy, paralleling observations of FGF23 null mice. It was thus named klotho after the Greek goddess who spins the thread of life. Alpha-klotho is a 130-kDa transmembrane protein that is predominantly expressed in the distal tubule of the kidney but also in multiple other tissues. The extracellular domain is also cleaved by proteases including a disintegrin and metalloproteinase (ADAM10 and ADAM17) and secreted into the blood, urine, and cerebrospinal fluid where it functions as a hormone. Thus, there is both tissue klotho and secreted (soluble or circulating) klotho. In the kidney, tissue klotho serves as a coreceptor for FGF23, and receptor activation leads to increased urinary excretion of phosphorus. Klotho also stimulates calcium reabsorption in the distal tubule by preventing endocytosis (stabilizing) of the major calcium channels, TRPV5 and TRPV6. Therefore, klotho may work with FGF23 to increase urinary phosphorus content but also ensures that the urine with high phosphorus does not also have high calcium, preventing supersaturation of the urine. Both FGF23 (from bone) and klotho (in the kidney) are stimulated by 1,25(OH) 2 D, and both FGF23 and klotho stimulate kidney 1-alpha hydroxylase (CYP27B1) to complete the endocrine feedback loop. In addition, cleaved/soluble klotho stimulates FGF23 secretion from bone and can affect kidney phosphate homeostasis even in the absence of membrane klotho. Thus, klotho joins FGF23, PTH, and calcitriol in a series of feedback loops that ensure optimal concentrations of calcium and phosphorus in bone and blood.
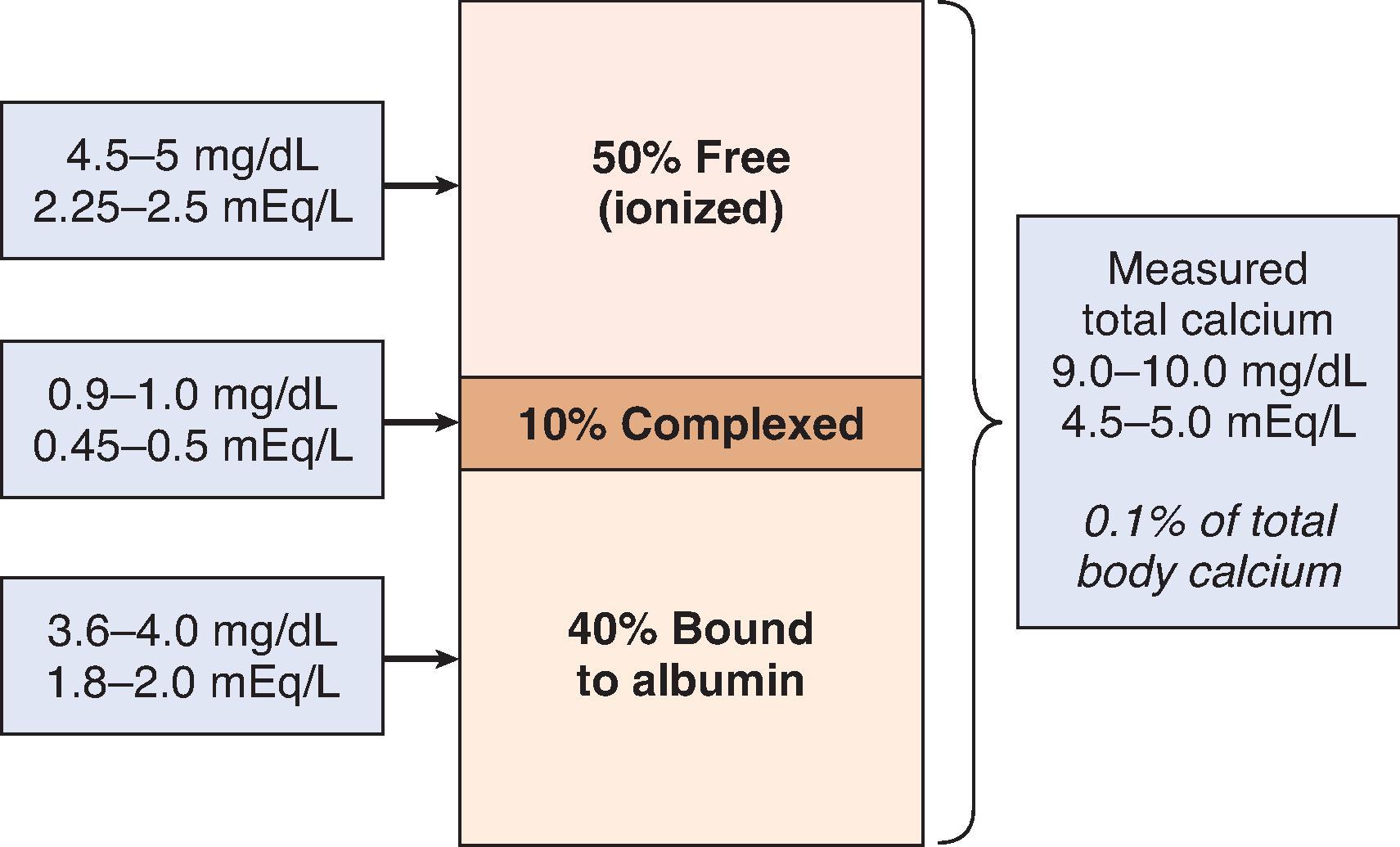
Serum calcium levels are tightly controlled within a narrow range, usually 8.5 to 10.5 mg/dL (2.1 to 2.6 mmol/L). However, the serum calcium level is a poor reflection of overall total body calcium because the intravascular space contains only 0.1% to 0.2% of extracellular calcium, which in turn represents only 1% of total body calcium, with nearly all total body calcium stored in bone. Only ionized calcium, approximately 50% of total serum calcium, is physiologically active, with the remaining 50% of total serum calcium bound to albumin or anions such as citrate, bicarbonate, and phosphorus ( Fig. 11.3 ).
Calcium absorption across the intestinal epithelium occurs via a vitamin D–dependent, saturable (transcellular) and vitamin D–independent, nonsaturable (paracellular) pathway. In states of adequate dietary calcium, the paracellular mechanism prevails, but the vitamin D–dependent pathways are critical in calcium-deficient states. Usually, the dietary intake of calcium is about 600 to 1000 mg/day in healthy adults. Out of every 1 g of ingested calcium, 600 mg is excreted in feces and 200 mg via the urine, thus leading to a net absorption of approximately 200 mg/day. The duodenum is the major site of calcium absorption, although the other segments of the small intestine and the colon also contribute to calcium absorption. In addition, there is secretion of calcium into the lumen of the mid- to distal- small and large intestine via paracellular transport contributing to fecal calcium losses. The heterogeneous distribution of calcium absorption and secretion along the small and large intestines creates a mechanism to respond to changes in physiologic stimulation to manage calcium homeostasis.
In the intestine and in the kidney, transcellular absorption occurs via three steps: (1) the entry of calcium from the lumen into the cells via transient receptor potential vanilloid (TRPV) channels, (2) the intracellular calcium then associates with calbindin to be “ferried” to the basolateral membrane, and (3) calcium is removed from the enterocytes predominantly via the calcium-ATPase, with the Na/Ca exchanger (NCX) playing a minor role. All of the key regulatory components of active calcium transport, TRPV, calbindin, Ca-ATPase, and NCX, are upregulated by calcitriol. At the level of the kidney, vitamin D and PTH work together to control calcium reabsorption and excretion.
In the kidney, the majority (60% to 70%) of calcium is reabsorbed passively in the proximal tubule, driven by a gradient that is generated by reabsorption of sodium and water. In the thick ascending limb, another 20% to 30% of calcium is reabsorbed via paracellular transport driven by the lumen positive net charge. The remaining 10% of calcium reabsorption occurs in the distal convoluted tubule, the connecting tubule, and the initial portion of the cortical collecting duct. The final regulation of urinary calcium excretion is carried out in these distal segments. Patients with CKD are at risk for maladaptive mineral bone metabolism and abnormal calcium homeostasis. Studies have demonstrated that patients suffering from CKD managed with oral calcium replacement or increased dietary calcium intake were shown to have a net positive calcium balance with a hypothetically increased risk for tissues’ deposition and vascular calcification. Therefore, in 2017 KDIGO changed its recommendation of maintaining a normal serum calcium level in CKD to avoiding hypercalcemia and treatment of symptomatic hypocalcemia on an individualized basis, as patients with CKD are at risk for increased morbidity and mortality related to cardiovascular complications in the setting of vascular calcifications.
Inorganic phosphorus is critical for numerous normal physiologic functions, including skeletal development, cell membrane phospholipid content and function, cell signaling, platelet aggregation, and energy transfer through mitochondrial metabolism. Normal homeostasis maintains serum concentrations between 2.5 and 4.5 mg/dL (0.81 to 1.45 mmol/L). The terms phosphorus and phosphate are often used interchangeably, but, strictly speaking, “phosphate” refers to the inorganic form that is in equilibrium (pK 6.8) between HPO 4 2 – and H 2 PO 4 − at physiologic pH in a ratio of about 4:1. For that reason, phosphorus is usually expressed in millimoles (mmol) rather than milliequivalents (mEq) per liter (L); however, as most laboratories report this inorganic component as “phosphorus,” we will use this term in the remainder of this chapter. Levels are highest in infants and decrease with growth, reaching adult levels in the late teenage years.
Total adult body stores of phosphorus are approximately 700 g, of which 85% is contained in bone. Of the remainder, 14% is intracellular and only 1% is extracellular. Of this extracellular phosphorus, 70% is organic and contained within phospholipids and 30% is inorganic. Of the latter, 15% is protein bound and the remaining 85% is either complexed with sodium, magnesium, or calcium or is circulating as the free monohydrogen or dihydrogen forms. Accordingly, only 0.15% of total body phosphorus (15% of extracellular phosphorus) is freely circulating and measured with serum chemistries. Therefore, as with calcium, serum measurements reflect only a small fraction of total body phosphorus and do not accurately indicate total body stores in the setting of abnormal homeostasis (e.g., CKD).
The average American diet contains approximately 1000 to 1400 mg of phosphorus per day, and the recommended daily allowance (RDA) is 800 mg/day. Approximately two-thirds of the ingested phosphorus is excreted in the urine and the remaining one-third in stool. In general, high-protein foods and dairy products contain the most phosphorus, whereas fruits and vegetables contain the least. In addition, grain-based (e.g., soy) protein contains phosphorus bound with phytate, making it less bioavailable. Many prepackaged and fast foods contain extra phosphorus as a preservative, which may not be identified on food labels and vary from lot to lot. An often surreptitious and unquantified source of dietary phosphorus is that which exists in prescription medications. A recent evaluation of commonly prescribed anti-hypertensive medication, multivitamins, and anti-depressants found they have significant quantities of phosphorus, up to 20 to 40 mg per pill, depending on their manufacturer. Therefore, it is difficult to accurately predict the dietary intake based on food type and medications alone.
Between 60% and 70% of dietary phosphorus is absorbed by the gut, in all intestinal segments. Medications that bind dietary phosphorus can decrease the net amount of phosphorus absorbed by decreasing the amount of free phosphorus available for absorption. In patients with CKD, such phosphate binders are used to compensate for the loss of kidney phosphorus excretion.
Passive enteric absorption (which is dependent on the luminal phosphorus concentration) occurs via the epithelial brush border sodium-phosphate cotransporter (NPT2b), driven by the sodium gradient created by the basolateral Na + /K + -ATPase transporter. The NPT2b sits in the terminal web, just below the brush border in “ready-to-use” vesicles that traffic to the brush border in response to acute and chronic changes in phosphorus concentration. Calcitriol can upregulate the NPT2b and thereby actively increase phosphorus absorption.
Most inorganic phosphorus is freely filtered by the glomerulus. Approximately 70% to 80% of the filtered load is reabsorbed in the proximal tubule, the primary site of regulated phosphorus reabsorption in the kidney, with the remaining 20% to 30% reabsorbed in the distal tubule. Hypophosphatemia stimulates CYP27B1, thereby increasing conversion of calcidiol to calcitriol, which in turn increases intestinal phosphorus absorption. Calcitriol also stimulates kidney tubular phosphorus reabsorption, leading to a reduction in urinary phosphorus excretion. In the presence of hyperphosphatemia, there is a rapid increase in urinary excretion of phosphorus, mediated by the levels of serum phosphorus, PTH, and FGF23. Although the effects are more minor, kidney phosphorus excretion is also increased by volume expansion, metabolic acidosis, glucocorticoid exposure, and calcitonin, and is decreased by growth hormone and thyroid hormone. Because of the capacity of the kidney to increase urinary phosphorus excretion, sustained hyperphosphatemia is not seen clinically without impairment of kidney function.
Magnesium plays an important role in neuromuscular function, control of cardiac excitability and vasomotor tone, mitochondrial function and energy metabolism, and DNA and protein synthesis. Magnesium is also a cofactor for many transporters involved in the regulation of sodium, potassium, and calcium. Normal magnesium levels are 0.7 to 1.1 mmol/L (1.4 to 2.2 mEq/L). Magnesium storage is located primarily in the hydroxyapatite mineral component of bone, accounting for 50%-60% of total body stores, while 40%-50% is located in muscle and non-muscular soft tissues. The large bone reserve provides an exchangeable source of magnesium to respond to changes in serum magnesium concentrations.
At this time, there are no known hormones that specifically regulate magnesium homeostasis or balance. Approximately 30% of the dietary magnesium is absorbed, mostly in the small intestine via paracellular pathways with a smaller contribution in the colon. In the colon, absorption from the lumen is predominantly active via transient receptor potential melastatin type 6 channel (TRPM6) and TRPM7, the activity of which is downregulated by increased intracellular magnesium and is independent of vitamin D. Extrusion of magnesium from the basolateral side may be through the Na + /Mg 2+ exchanger CNNM4 based on data from rodent models. However, humans with VNNM4 mutations do not have hypomagnesemia.
About 10% to 20% of filtered magnesium is reabsorbed in the proximal convoluted tubule, and reabsorption decreases with extracellular volume expansion in parallel with that of sodium and calcium. Unlike other divalent ions, most (75%) magnesium is reabsorbed passively through paracellular pathways in the thick ascending limb of the loop of Henle, driven by a lumen-positive voltage in a specific cation-permeable channel formed by the tight junction proteins Claudin-16 (formerly called paracellin ), Claudin-14, and Claudin-19. Mutations of the last proteins have a role in the development of familial hypomagnesemia with hypercalciuria and nephrocalcinosis. About 5% to 10% of magnesium is reabsorbed in the distal convoluted tubule, driven primarily by the luminal membrane potential established by the voltage-gated potassium channel and facilitated by TRMP6, which is located at the luminal membrane of the distal convoluted tubule. Estrogen, insulin, magnesium, and pH may alter expression or function of this transporter.
The majority of the total body stores of calcium and phosphorus are located in bone in the form of hydroxyapatite [Ca 10 (PO 4 ) 6 (OH) 2 ]. Trabecular (cancellous) bone comprises 15% to 20% of bone. Trabecular bone is located predominantly in the epiphyses of the long bones and serves a metabolic function. There is a relatively rapid exchange of calcium between trabecular bone and plasma (days to weeks), as evidenced by a short turnover rate of the radioisotope 45 calcium. In contrast, cortical (compact) bone is located in the shafts of long bones and comprises 80% to 90% of bone. This bone serves primarily a protective and mechanical function and it has a calcium turnover rate of months. The nonmineral component of bone consists principally (90%) of highly organized cross-linked fibers of type I collagen; the remainder consists of proteoglycans and “noncollagen” proteins such as osteopontin, osteocalcin, osteonectin, and alkaline phosphatase. The predominant cell types involved in bone turnover are osteoclasts, the bone-resorbing cells derived from circulating hematopoietic cells, and osteoblasts, the bone-forming cells derived from the marrow. These cells are important in bone remodeling, which occurs in response to hormones, cytokines, and changes in mechanical forces and can in turn affect calcium and phosphorus homeostasis.
Hypercalcemia is defined as elevated serum calcium. Ionized calcium represents the biologically active fraction of total serum calcium. In the presence of hypoalbuminemia, there is a proportionate increase in ionized calcium relative to total calcium, so that measurements of total serum calcium in patients with hypoalbuminemia may underestimate the amount of physiologically active (ionized) calcium. A commonly used formula to estimate ionized calcium from total serum calcium is to add 0.8 mg/dL to the total calcium value for every 1 mg/dL decrease in serum albumin below 4 mg/dL. In certain circumstances, such as the presence of increased concentrations of albumin or molecules capable of binding calcium (e.g., phosphate and citrate), paraproteinemias, or abnormally high or low blood pH, direct measurement of serum-ionized calcium is essential, especially if intravenous (IV) calcium infusion is contemplated. In patients with advanced CKD on dialysis, this estimating formula is not very accurate.
The severity of symptoms caused by hypercalcemia depends on the degree and rate of rise in serum calcium. Gastrointestinal symptoms such as nausea, vomiting, constipation, abdominal pain, and, rarely, peptic ulcer disease may occur. Neuromuscular involvement includes altered mentation, impaired concentration, fatigue, lethargy, and muscle weakness. Hypercalcemia can impair kidney water handling by inducing nephrogenic diabetes insipidus and sodium wasting. The resulting diuresis worsens the hypercalcemia, because volume depletion limits the protective hypercalciuria and exacerbates the volume-dependent proximal tubule reabsorption of calcium. In addition, volume depletion may lead to acute kidney injury, which further limits calcium excretion and favors an additional increase in serum calcium. The hypercalciuria associated with prolonged hypercalcemia can rarely lead to nephrolithiasis and nephrocalcinosis. Cardiovascular effects include hypertension and shortening of the QT interval on the electrocardiogram (ECG). Although cardiac arrhythmias are uncommon, hypercalcemia can trigger digitalis toxicity.
The most common causes of hypercalcemia are malignancy and hyperparathyroidism; in most series, these two diagnoses account for more than 90% of cases. The remaining causes are listed in Box 11.1 , with key causes discussed in more detail in the following paragraphs.
Malignancy
Local osteolytic hypercalcemia
Humoral hypercalcemia of malignancy (PTHrp)
Hematologic malignancies such as lymphoma where there is ectopic calcitriol synthesis
Hyperparathyroidism
Thyrotoxicosis
Granulomatous diseases (sarcoidosis, histoplasmosis, tuberculosis)
Drug-induced
Vitamin D
Thiazide diuretics
Estrogens and antiestrogens
Androgens (breast cancer therapy)
Vitamin A
Lithium
Immobilization
Total parenteral nutrition
Impaired kidney function (AKI or CKD), usually in the setting of medications such as calcium-containing phosphate binders or calcitriol or its analogues
Malignancy is the most common cause of hypercalcemia in hospitalized patients, and the presence of hypercalcemia in cancer patients confers a poor prognosis. Hypercalcemia can result from direct invasion of bone by metastatic disease, referred to as local osteolytic hypercalcemia (LOH). In LOH, tumor cells within the bone marrow space produce a variety of inflammatory cytokines, collectively termed osteoclast-activating factors , which lead to net bone resorption, calcium release, and hypercalcemia. PTH levels are suppressed in response to the hypercalcemia. This mechanism is common with hypercalcemia resulting from breast cancer or multiple myeloma. Hypercalcemia can also result from the production of circulating factors that stimulate osteoclastic resorption of bone. Humoral hypercalcemia of malignancy is caused by secretion of parathyroid hormone–related peptide (PTHrp) by tumor cells. PTHrp bears similarity to PTH only in the initial 8-amino-acid sequence, but this homology permits binding to the PTH receptor, leading to increased bone turnover and hypercalcemia. Specific assays are available to distinguish circulating PTHrp from PTH. Finally, hypercalcemia in malignancy can result from increased production of calcitriol, which stimulates gastrointestinal absorption of calcium. Various lymphoid tumors, most notably Hodgkin lymphoma, have been shown to synthesize large quantities of calcitriol.
The incidence of primary hyperparathyroidism has declined over the past 30 years, but it is still the second most common cause of hypercalcemia. In most cases, primary hyperparathyroidism is caused by a benign adenoma of a single parathyroid gland that autonomously secretes PTH. The disorder may be sporadic, familial, or inherited as a component of the constellation of multiple endocrine neoplasia (MEN). The elevation in PTH results in increased intestinal absorption of calcium through stimulation of calcitriol production, increased osteoclastic bone resorption, and increased kidney tubular reabsorption of calcium. However, because of the elevation in serum calcium, the filtered load of calcium exceeds the ability of the kidney to reabsorb calcium, leading to hypercalciuria and potentially to nephrolithiasis. Secondary hyperparathyroidism is caused by diffuse hyperplasia of all four glands in response to ongoing stimuli such as hypocalcemia or hyperphosphatemia. Iatrogenic hypercalcemia may occur in patients with secondary hyperparathyroidism treated with calcium-based phosphate binders or calcitriol and its derivatives. Secondary hyperparathyroidism can also cause hypercalcemia via increased bone resorption when the glands become adenomatous and no longer respond to the change in calcium—a stage often called tertiary hyperparathyroidism.
Lithium may interfere with the CaSR, leading to a “resetting” of the parathyroid gland sensitivity such that higher levels of calcium are needed to decrease PTH. Clinically, these patients may appear to have hyperparathyroidism, but hypercalcemia resolves when lithium is stopped.
Hypercalcemia from excessive intake of native vitamin D supplements (ergocalciferol and cholecalciferol) is rare, because 1α-hydroxylase (CYP27B1) activity is tightly regulated by calcium levels. In contrast, the excessive administration of calcitriol or of other active vitamin D analogues, such as paricalcitol or doxercalciferol, which bypass this regulatory step at the level of the kidney, can lead to hypercalcemia. These drugs are commonly used in the treatment of secondary hyperparathyroidism in CKD. An endogenous source of excess calcitriol is production by non-kidney tissue like lymphomas and granulomatous diseases, including sarcoidosis, tuberculosis, endemic fungal infections, and berylliosis. Hypercalcemia manifests secondary to pulmonary and lymph node monocyte and macrophage activation and conversion of calcidiol to calcitriol via 1α-hydroxylase activity. Patients with these disorders can often present with asymptomatic or symptomatic hypercalcemia, hypercalciuria, nephrocalcinosis, chronic kidney disease, nephrogenic diabetes insipidus, and nephrolithiasis. Sarcoidosis, being the most common and well evaluated of the granulomatous disorders, hypercalcemia has been reported in up to 63% in a case series of patients. Given the heterogenous nature of granulomatous disorders, special attention must be paid to the patient’s history and risk factors, as management is focused on the treatment of the causative condition.
Inactivating mutations of the CaSR cause familial hypocalciuric hypercalcemia (FHH), a rare hereditary disease with autosomal-dominant transmission. Calcium is unable to activate the mutant receptor in the kidney, leading to increased kidney reabsorption of calcium into the blood from the tubular fluid and hypocalciuria, usually with urine calcium excretion less than 100 mg/day. Because this mutation may also affect the receptor at the level of the parathyroid gland, PTH may be slightly elevated out of proportion to the degree of hypercalcemia. Other clues pointing to this diagnosis include a family history of asymptomatic hypercalcemia. Probands are often discovered after parathyroidectomy fails to correct hypercalcemia.
Clinicians may approach patients with hypercalcemia by considering the diagnoses in Box 11.1 . An alternative approach is to formulate a differential diagnosis based on the physiology of calcium homeostasis ( Fig. 11.4 ) and tailoring diagnostic studies to the suspected pathophysiology.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here