Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Improved and detailed understanding of the molecular basis of many of the diseases in this chapter continues to progress. While Ehlers-Danlos has been well understood for many years, our understanding has further expanded and a new classification scheme systematizes by both clinical presentation and pathogenesis into multiple categories. In other diseases, we have gone from virtually no knowledge or only speculation regarding their molecular determinates to identification of specific genetic mutations that drive their pathogenesis. Although the precise mechanistic details remain a work in progress, this expansion of knowledge has several important implications. The identification of the genetic origin of these diseases:
permits better diagnosis and prognosis, including prenatal evaluation when relevant,
informs our classification schemes,
provides insight into pathogenesis and normal biology,
enables rational, precision medicine for therapeutic interventions.
The earlier Berlin and Villefranche classification systems have been very recently replaced by that of the 2017 international classification of Ehlers-Danlos syndrome (EDS), in which the clinical variants are subtyped by molecular mechanisms ( Table 21.1 ). Thirteen major types are recognized. Most show autosomal dominant inheritance, but autosomal recessive variants are also recognized. This classification is not perfect, but represents the most current and mature consensus understanding of the disease. It classifies the EDS spectrum of diseases in two ways: into 13 clinical entities which correspond in large degree to the prior Berlin and Villefranche systems, with some expansion for additional defined variants (see Table 21.1 ), and also into 6 genetic and pathogenetic groupings that are helpful in understanding the various molecular mechanisms of the disease (see Table 21.2 ). It also removes several conditions from the EDS spectrum that were included in the prior classification schemes.
| 2017 International | Villefranche | Berlin | Inheritance | Clinical features | |
|---|---|---|---|---|---|
| 1 | Classical EDS (cEDS) | Classical type | Types I and II | AD | Soft hyperextensible skin |
| Mesomorphic build | |||||
| Cigarette-paper scarring | |||||
| Molluscoid pseudotumors | |||||
| Spheroids | |||||
| 2 | Classical-like EDS (clEDS) | AR | Velverty hyperextensible skin | ||
| No atrophic scarring | |||||
| Generalized joint hypermobility | |||||
| Easy bruising | |||||
| 3 | Cardiac-valvular EDS (cvEDS) | AR | Cardiac valve dysfunction | ||
| Hyperextensible skin | |||||
| Atrophic scars and bruising | |||||
| 4 | Vascular EDS (vEDS) | Vascular type | Type IV | AD | Bruising |
| Thin translucent skin | |||||
| Aneurysms, vascular rupture, bowel rupture | |||||
| 5 | Hypermobile EDS (hEDS) | Hypermobility type | Type III | AD | Marked joint hypermobility |
| 6 | Arthrochalasia EDS (aEDS) | Arthrochalasia type | Types VIIA and VIIB | AD | Short stature |
| Extreme joint laxity | |||||
| Congenital dislocation of the hip | |||||
| 7 | Dermatosparaxis EDS (dEDS) | Dermatosparaxis type | Type VIIC | AR | Skin fragility |
| Cutis laxa | |||||
| 8 | Kyphoscoliotic EDS (kEDS) | Kyphoscoliosis type | Type VI | AR | Neonatal muscle hypotonia |
| Joint hyperextensibility | |||||
| Kyphoscoliosis | |||||
| Ocular lesions | |||||
| 9 | Brittle Cornea syndrome (BCS) | AR | Thin cornea +/- rupture | ||
| Early progressive ketaoconus / keratoglobus | |||||
| Blue sclerae | |||||
| 10 | Spondylodysplastic EDS (spEDS) | EDS Progerioid type | AR | Short stature from childhood | |
| Muscle hypotonia | |||||
| Limbs bowing | |||||
| 11 | Musculocontractural EDS (mcEDS) | AR | Multiple congenital contractures | ||
| Characteristic congenital facies | |||||
| Skin hyperextensibility, brusing, atrophic scars | |||||
| 12 | Myopathic EDS (mEDS) | AD or AR | Early muscle hypotonia/atrophy, improves with age | ||
| Distal joint hypermobility | |||||
| Proximal joint contractures | |||||
| 13 | Periodontal EDS (pEDS) | EDS periodontis | Type VIII | AD | Hyperextensible skin |
| Mucosal fragility | |||||
| Periodontitis |
| No longer included in EDS spectrum | |||
|---|---|---|---|
| X-linked EDS with muscle hematoma | Other | Type V | X-linked recessive |
| Fibronectin-deficient | Other | Type X | Unknown |
| Occiptal horn syndrome | Type IX | X-linked recessive | |
| Familial articular hypermobility | Other | Type XI | AD |
| 2017 International classification | Locus | Gene | Protein | Inheritance | |
|---|---|---|---|---|---|
| Group A: Disorders of collagen primary structure and processing | |||||
| 1 | Classical EDS (cEDS) | 9q34.3 | COL5A1 | Type V collagen | AD |
| 2q32.2 | COL5A2 | Type V collagen | |||
| 17q21.33 | COL1A1 | Type I collagen | |||
| 4 | Vascular EDS (vEDS) | 2q32.2 | COL3A1 | Type III collagen | AD |
| 17q21.33 | COL1A1 | Type I collagen | |||
| 6 | Arthrochalasia EDS (aEDS) | 17q21.33 | COL1A1 | Type I collagen | AD |
| 7q21.3 | COL1A2 | Type I collagen | |||
| 7 | Dermatospraxis EDS (dEDS) | 5q35.3 | ADAMTS2 | A disintegrin-like and metalloproteinase with thrombospondin type 1 motif 2 | AR |
| 3 | Cardiac-valvular EDS (CVEDS) | 7q21.3 | COL1A2 | Type I collagen | AR |
| Group B: Defects in collagen folding and cross-linking | |||||
| 8 | Kyphoscoliotic EDS (kEDS-PLOD1) | 1p36.22 | PLOD1 | Procollagen-lysin, 2-oxoglutarate 5-dioxygenase 1 (lysylhydroxylase 1) | AR |
| 8 | Kyphoscoliotic EDS (kEDS-FKBP14) | 7p14.3 | FKBP14 | FK506-binding protein 14 | AR |
| Group C: Defects in structure and function of myomatrix (interface of muscle and extracellular matrix) | |||||
| 2 | Classical-like EDS (clEDS) | 6p21.33-p21.32 | TNXB | Tenascin XB | AR |
| 12 | Myopathic EDS (mEDS) | 6q13-q14 | COL12A1 | Collagen XII | AD / AR |
| Group D: Defects in glycosaminoglycan biosynthesis | |||||
| 10 | Spondylodysplastic EDS (spEDS-B4GALT7) | 5q35.3 | B4GALT7 | Galactosyltransferase I β4GalT7 | AR |
| 10 | Spondylodysplastic EDS (spEDS-B3GALT6) | 1p36.33 | B3GALT6 | Galactosyltransferase II β3GalT6 | AR |
| 11 | Musculocontractural EDS (mcEDS-CHST14) | 15q15.1 | CHST14 | Dermatan-4 sulfotransferase-1 | AR |
| 11 | Musculocontractural EDS (mcEDS-DSE) | 6q22.1 | DSE | Dermatan sulfate epimerase-1 | AR |
| Group E: Defects in complement pathway | |||||
| 13 | Periodontal EDS (pEDS) | 12p13.31 | C1R | Complement C1r subcomponent | AD |
| 12p13.31 | C1S | Complement C1s subcomponent | |||
| Group F: Disorders of intracellular processes | |||||
| 10 | Spondylodysplastic EDS (spEDS-SLC39A13) | 11p11.2 | SLC39A13 | Zinc transporter ZIP13 | AR |
| 9 | Brittle Cornea Syndrome (BCS) | 16q24 | ZNF469 | Zinc finger protein 469 | AR |
| 4q27 | PRDM5 | PR domain zinc finger protein 5 | AR | ||
| Unresolved forms of EDS | |||||
| 5 | Hypermobile EDS (hEDS) | ? | ? | ? | AD |
EDS is one of the most common inherited disorders, the incidence estimated being 1 : 5000 individuals. The disease spectrum includes both relatively common and rare types.
The clinical manifestations include :
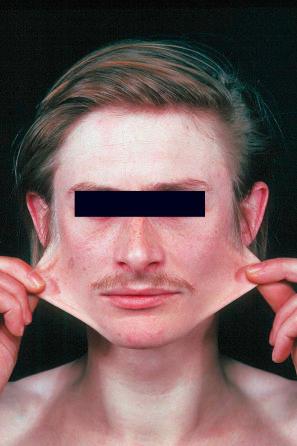
hyperextensible skin ( Figs 21.1 and 21.2 ),

hypermobility of joints ( Figs 21.3 and 21.4 ),


atrophic, paper-thin scars ( Figs 21.5 and 21.6 ),


a tendency to easy bruising,
connective tissue fragility,
variable internal organ involvement.
Trauma, with resultant hematoma formation and scarring, may give rise to so-called molluscoid pseudotumors ( Fig. 21.7 ). Patients also develop hard, discrete, mobile (sometimes calcified) fibrous nodules (spheroids) in the subcutaneous fat of the extremities. Redundant skin (acquired cutis laxa) may develop over the elbows and knees, particularly in elderly patients.

Ocular manifestations include blue sclera, keratoconus, lens subluxation, and retinal detachments; dental involvement may present with severe periodontitis.
Gastrointestinal involvement presents as hematemesis, melena, and colonic rupture, and vascular lesions include arterial rupture and aortic or other major vessel aneurysms. Complications in pregnancy can occur. Underlying coagulopathies, dysphonia, and tongue hypermobility have been described. Mild to moderate neuromuscular symptoms including muscle weakness, myalgia, and decreased vibration sense can also be seen.
The following briefly summarizes the salient clinical features of the 13 EDS disease subtypes of the 2017 international classification where each type is defined with major and minor criteria as well as causative genetics. Table 21.1 also summarizes the nomenclature of the prior Berlin and Villefranche systems and indicates where these overlap with the new system. The new system was created in response to the expanded understanding of the genetics of EDS, leading to new and sometimes rare forms not well addressed under the prior systems. It also responds to the need to strictly define the clinical cohorts to provide appropriate management guidelines as the manifestations and complications of the disease vary between subtypes.
As in the 1997 Villefranche classification ( Table 21.1 ), classic (autosomal dominant) EDS includes types I (gravis) and II (mitis) from the Berlin classification, as their difference is merely one of severity of involvement. Patients suffer from soft hyperextensible skin with a tendency to split over bony eminencies. A broad mesomorphic physique with wide hands and feet is characteristic. Extensive tissue paper scarring (said to resemble a fish's mouth) over the knees and shins is usually present and molluscoid pseudotumors are common, with the cutaneous findings more prominent than in hypermobility types. Additional features may include epicanthic folds, mitral valve prolapse, cutaneous varicosities, myopia, and late-onset osteoarthrosis. Complications in pregnancy include premature rupture of membranes, increasing perineal skin tearing, and prolapsing uterus and bladder. Breast calcification has been reported as a complication from screening mammography. Mutations involve multiple structural collagen genes including COL5A1 , COL5A2 , and COL1A1 .
This subtype explicitly recognizes the autosomal recessive inheritance patterns seen in some cases with symptoms similar to classical EDS. A common feature is skin hyperextensibility with velvety texture, but not atrophic scarring. Generalized joint hypermobility can be seen both in the absence and presence of recurrent dislocations, mostly in the ankle and shoulder. Skin is easily bruised, often with spontaneous ecchymoses. Other features such as foot deformities, leg edema, mild muscle weakness, and rectal and gynecological prolapse can be seen. Defects in TNXB , the gene encoding tenascin X, result in abnormally clumped elastic fibers and are responsible for autosomal recessive forms of EDS that phenotypically mimic the autosomal dominant classical subtype. Tenascin X, an extracellular matrix glycoprotein that binds to and regulates collagen fibril arrangement and possibly remodeling in the dermis can be affected. This and the cardiac-valvular subtype discussed below are newly defined within the 2017 international EDS classification, as are subtypes 9–12.
This autosomal recessive form of EDS is associated with severe and progressive deterioration of cardiac valve integrity and function. Skin is thin and hyperextensible with atrophic scars and ready bruising. Inguinal hernias, joint dislocations, and various foot deformities can be encountered.
Vascular EDS (vEDS), autosomal dominant, is of particular importance because it is associated with the most severe vascular involvement. While vascular phonotypes can be seen in other EDS subtypes, they are particularly prominent here. Patients manifest ecchymotic lesions on the knees, shins, and elbows, and features of acrogeria are often present. The skin is characteristically thin and translucent. Additional cutaneous manifestations include short stature, keloidal or elastotic scars, elastosis perforans serpiginosa, large eyes, lobeless ears, tooth loss, a Madonna-like facies, acro-osteolysis, diffuse scalp alopecia, and orthopedic manifestations including congenital dislocation of the hip. Aneurysms can arise in the aorta or other major vessels, and arteriovenous fistulae and arterial dissection may be complications. Blood vessel walls are notoriously fragile, complicating surgical correction and contributing to the very high mortality associated with this variant. Fistulas of the carotid-cavernous sinus and bowel, pleuroperitoneal, and uterine rupture are also sometimes seen.
Hypermobile (autosomal dominant) patients have minimal cutaneous manifestations, their presentation being limited to symptomatic joint laxity with hypermobility. This is the most common subtype of EDS, representing 80–90% of all cases, and might represent the most common human connective tissue disease with an estimated prevalence of up to 10 million cases in the United States alone. The stricter definitions of hypermobile EDS over prior criteria could reduce these higher prevalence estimates. Muscular pain both with and without activity is common. Additional uncommon findings in one study included dysphonia, Arnold-Chiari type I malformation, and dolichocolon. This type is difficult to diagnose given the more limited spectrum of findings; many authors believe this is identical to the benign joint hypermobility syndrome. The lack of established genetic causes suggests complexities such as polygenic disease, nonpenetrance, sex-linked penetrance, and multifactorial environmental influences.
Arthrochalasia EDS, autosomal dominant, presents with bilateral congenital dislocation of the hips, severe widespread hypermobility and other joint dislocations, muscular hypotonia, and hyperextensible skin with fragility.
Dermatosparaxis EDS, autosomal recessive, named after a condition initially described in cows and sheep, is characterized by skin fragility with tearing and joint hypermobility (Gr. sparagmos , a tearing), is extremely rare, with only a handful of cases reported. Mutations in ADAMTS2 encoding procollagen I amino-peptidase are characteristic. Patients present with marked skin fragility and laxity with redundant skin folds, blue sclerae, increased bruisability, micrognathia, large fontanelles, umbilical hernia, and growth retardation.
Kyphoscoliosis EDS, autosomal recessive, presents with neonatal muscle hypotonia associated with generalized joint laxity, kyphoscoliosis, cystic malformation of the meninges, and cutaneous and ocular fragility with retinal detachment. This type has been further bifurcated into those with deficiency of lysylhydroxylase ( PLOD1 mutations) and a second form which have normal levels of lysyl oxides, but harbor inactivating mutations in FKBP14 .
This autosomal recessive form is evidenced primarily with eye symptoms as the name brittle cornea syndrome implies. Major features include thin cornea that can result in rupture, early onset of progressive keratoconus or keratoglobus, and bluish discoloration of the sclerae. Hypermobility of distal joints can be seen and retinal detachment and deafness are also sometimes seen. Mutations in ZNF469 or PRDM5 are seen.
Short stature, bowing of the limbs, and muscle hypotonia are important criteria. Skin hyperextensibility and osteopenia can be seen. Other features vary based on the which of three genes are involved in this autosomal recessive disorder: SLC39A13 , B3GALT6 , or B4GALT7 .
This autosomal recessive subtype shows multiple flexural contractures that can be accompanied with clubfoot (talipes equinovarus), characteristic craniofacial dysmorphism, and skin with hyperextensibility, easy bruising, fagility with atrophic scars, and distinctly wrinkled palms. Other complications include recurrent dislocations, pneumothorax, colonic diverticula, and spinal deformities.
Both autosomal dominant and autosomal recessive mechanisms of inheritance are described for musculocontractural EDS. Early muscle hypotonia and/or atrophy improves with age. There is hypermobility of distal joint with contractures at the larger proximal joints such as the knees, hips, and elbows. Soft dough skin and atrophic scarring can be seen.
This autosomal dominant subtype features severe periodontitis with early onset, lack of attached gingiva, and pretibial plaques. Because of the strong penetrance, a family history is often documented. The usual EDS spectrum features of skin hyperextensibility, fragility and scarring with easy bruising, and hypermobile distal joints can also be seen.
Berlin type V EDS resembles classic EDS with muscle hematomas, but has an X-linked transmission. Its existence as a separate entity has long been questioned.
Berlin type IX is currently classified in the cutis laxa spectrum (occipital horn syndrome).
Berlin type X EDS is exceedingly rare and associated with fibronectin deficiency and abnormal platelet aggregation. It is uncertain whether this separation as a distinctive variant is justified.
Berlin type XI EDS is now considered to be a separate entity, familial joint laxity syndrome.
EDS represents a heterogeneous group of related genetic disorders characterized not only by abnormal fibrillar collagen synthesis but also by abnormalities in proteins that interreact with collagen. The 2017 international classification also structures the 13 subtypes by pathogenic mechanism into the six groupings below (see Table 21.2 ) :
Group A: disorders of collagen structure and processing
Group B: defects in collagen folding and crosslinking
Group C: defects in structure and function of myomatrix (interface of muscle and extracellular matrix)
Group D: defects in glycosaminoglycan biosynthesis
Group E: defects in complement pathway
Group F: disorders of intracellular processes
The known genetic defects of all 13 types recognized under the 2017 international classification are summarized in Table 21.2 . Only the genetic details of the most common subtype, hypermobile EDS, is completely unknown. For many of the rarer subtypes, molecular testing is considered necessary to firmly establish the diagnosis.
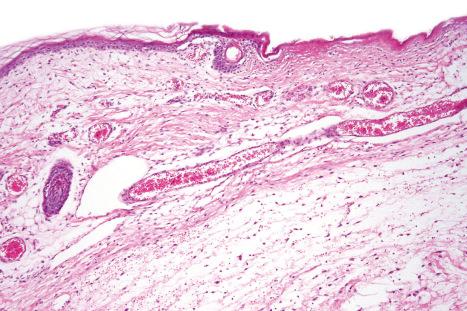
Generally, histologic examination of skin biopsies from patients with EDS is unrewarding. While there may appear to be a diminution in the number and thickness of the collagen fibers, the range is so wide in normal skin that histopathological examination really has little to offer; diagnosis is essentially molecular now that the genetic basis of most EDS subtypes is understood.
Ultrastructural observations are also of limited value. In the classic variant, the resultant abnormal collagen fibrils are 25% greater in diameter, disorganized, and there are characteristic composite fibrils with a cauliflower-like appearance. Tenascin-X deficient fibrils are imperfectly aligned. In the vascular type, collagen fibrils are disorganized, irregular, fragmented, frayed, and show a variable diameter. Hyaluronic acid globules, amorphous matrix, microcalcifications, elastic-like fibers, and microcavities are also present. Similar ultrastructural findings are seen in defects in type I collagen. The fibrils in the arthrochalasia type are angular, whereas in the dermatosparaxis type they have a hieroglyphics-like appearance.
Aplasia cutis congenita (congenital absence of the skin) presents as a focal or widespread loss of skin, subcutaneous fat, and sometimes deeper tissues. The incidence is approximately 3 : 20 000 live births. The vast majority involve the scalp, but the extremities and trunk can be involved. It represents a heterogeneous group of conditions of varied etiologies, which since 1986 has been usefully subdivided into nine groups based on associated features, etiological factors, distribution of lesions, and patterns of inheritance. Usually, localized aplasia cutis is an isolated phenomenon (group 1), but in a significant proportion of patients it may signify a serious underlying congenital systemic disease.
Group 1 patients are prototypic. This can be an autosomal dominant condition or sporadic in nature. Lesions are congenital and present as single or multiple, variably shaped (punched out, round, oval, linear, or stellate), crusted or ulcerated areas measuring 1–2 cm in diameter, usually situated over the posterior aspect of the scalp in close relationship to the parietal hair whorl ( Fig. 21.8 ). Sometimes they are accompanied by conspicuous dilated veins. Bullous lesions are occasionally encountered. Healing is by scarring that is sometimes hypertrophic. In up to 20–30% of cases, these scalp lesions are associated with underlying defects of the skull, meninges, and, less commonly, brain. Some patients have additional congenital defects such as cleft lip and palate. Rare cases with large defects including the underlying bone have been reported. Many of these cases are susceptible to infectious complications and hemorrhage, which rarely can be fatal. Thrombosis can complicate larger lesions. Unlike smaller defects that heal spontaneously, these require surgical intervention.

Group 2 patients have scalp defects associated with transverse terminal limb defects, of which hypoplasia or aplasia of the distal phalanges is the most common. This was initially described to be an autosomal dominant condition (Adams-Oliver syndrome), but autosomal recessive cases are reported. Some other features include syndactyly, eye defects, nail dystrophy, vascular defects including cutis marmorata telangiectatica congenita, cardiac defects, abdominal wall defects, and pulmonary and central nervous system abnormalities. Cases of congenital heart defects and aplasia cutaneous cutis without limb defects have been reported and proposed by some as a form of Adams-Oliver syndrome. Multiple genes have now been reported in classic Adams-Oliver syndrome including: ARHGAP31 , DLL4 , DOCK6 , EOGT , RBPJ , and NOTCH1 . Some of the disease features correlate with particular gene defects. Non-familial probands tend to have higher incidence of additional anomalies relative to familial probands. ARHGAP31 and DOCK6 function in the cdc42/rac1 pathway while the remaining four are involved in the NOTCH signaling pathway. DOCK6 and EOGT are associated with the autosomal recessive form of the disease, while the other four genes show automosomal dominant inheritance.
Group 3 represents the combination of scalp aplasia with organoid (epidermal and sebaceous) nevi. Patients may also have ophthalmological abnormalities including corneal opacities, scleral dermoids, and eyelid colobomata. Occasionally, psychomotor retardation is evident. SCALP syndrome has been described as nevus sebaceous syndrome, central nervous system malformation, aplasia cutis congenita, limbal dermoid, and pigmented nevus (giant congenital melanocytic nevus) with neurocutaneous melanosis and could be related.
Group 4 constitutes the association of aplasia cutis with an underlying maldevelopment of the brain or spinal cord (e.g., porencephaly, meningomyelocele, split cord). Association with faun tail nevus (excessive lumbar hypertrichosis) has been noted. Co-occurrence of both faun tail nevus and fetus papyraceus has been described, suggesting potential overlap with group 5.
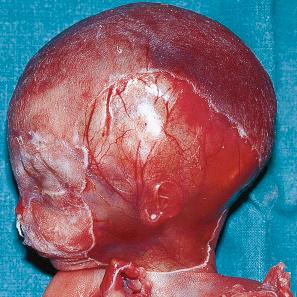
Group 5 represents the association of truncal and limb aplasia cutis with fetus papyraceus or placental infarcts.
Group 6 defines aplasia cutis as a manifestation of epidermolysis bullosa (Bart syndrome). Patients present with skin defects accompanied by blistering on the trunk and extremities ( Figs 21.9 and 21.10 ). This is a heterogeneous group which requires identification and classification of the underlying bullous dermatosis.

Group 7 patients have skin defects of the distal limbs unassociated with blistering. Autosomal dominant and recessive variants have been described.
Group 8 constitutes the development of aplasia cutis as a consequence of intrauterine infection (e.g., herpes simplex/varicella-zoster) or a teratogenic drug (e.g., methimazole, misoprostol).
Group 9 represents aplasia cutis developing against a background of malformation syndromes and ectodermal dysplasias (e.g., trisomy 13, 4p- syndrome, and focal dermal hypoplasia [FDH]).
It is important that aplasia cutis is not mistaken for birth-related trauma with resultant medicolegal considerations. Rare, fatal cases with systemic aplasia cutis congenita have been described.
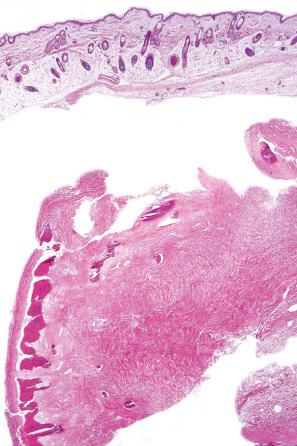
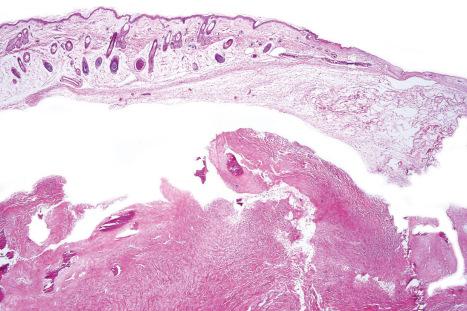
Histologic examination typically reveals an ulcer bed deep to which granulation tissue may be evident ( Figs 21.11–21.13 ). The appendages are absent. If a healed lesion is examined, re-epithelialization of the defect may be seen. There is associated scarring of the dermis.
FDH (Goltz syndrome) is a rare X-link autosomal dominant disorder involving lesions of both ectoderm and mesoderm and is found almost exclusively in females. Sporadic variants are frequently encountered, and a small number of affected males have been reported, possibly from postzygotic mutations; the male homozygous state appears to be lethal. FDH syndrome is associated with cutaneous, skeletal, ocular, oral, dental, aural, and soft tissue defects.
PORCN (Xp11.23) encodes an O -acetyltransferase that facilitates secretion of ligands for the Wnt pathway, and a variety of inactivating mutations including nonsense, missense, splicing, and frameshift (insertions and deletions, including microdeletions) are associated with FDH. Sporadic cases tend to have point mutations and small deletions while familial cases show larger deletions. The Wnt pathway is critical for embryological development of a number of tissues including skin, fibrous, adipose, muscle, bone, teeth, nervous system, and limb patterning. A transgenic mouse model with a conditional PORCN mutant allele can recapitulate various features of the human disease including FDH. The variability in phenotype has been attributed to mosaicism and lyonization. Diagnosis has been proposed to include at least three characteristic skin findings and one or more limb malformations. Using such operational criteria, the vast majority of patients exhibit detectable PORCN mutations. Prenatal diagnosis is an option where appropriate.
Cutaneous lesions, which are almost invariably present from birth, include areas of hypoplastic skin (such as aplasia cutis) which present clinically as depressed and atrophic cribriform and reticulated lesions, linear ( Fig. 21.14 ) or reticular areas of erythema, hyper- or hypopigmentation, fatty tumors (most often on the limbs) ( Fig. 21.15 ), and raspberry-like papillomatous or verrucous growths, particularly around the ostia of the body. Telangiectasia is a frequent manifestation. Linear lesions follow Blaschko lines and are most often seen on the limbs and cheeks. Nail dystrophy, anonychia, and focal alopecia can be present.


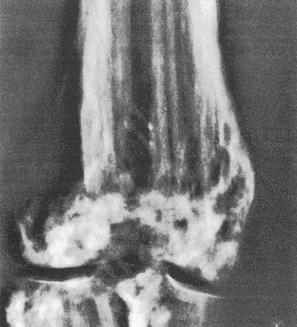
Skeletal manifestations, including hypoplasia or aplasia of the digits, ‘lobster claw hand’, syndactyly, and polydactyly, are seen in 60–70% of patients ( Fig. 21.16 ). Facial, trunk, or limb asymmetry is seen in 30%. Linear, vertically oriented, radiopaque striations in the metaphyses of long bones (osteopathia striata) are characteristic ( Fig. 21.17 ). Bone weakness and early osteoporosis have been reported. Microcrania, sometimes with mental retardation, scoliosis, kyphosis, and spina bifida occulta have also been described.

Ocular findings include hypertelorism, microphthalmia, anophthalmia, aniridia, strabismus, nystagmus, glaucoma, retinal detachment, and colobomata of the iris, retina, choroid, and optic nerve. Oral and dental lesions involving tooth maldevelopment (dysplasia), partial agenesis, anodontia, malocclusion, and poor enamel and papillary gingival hyperplasia may occur in up to 40% of patients. Aural involvement may result in both sensorineural and conduction deafness. A history of tonsillectomy for obstructive sleep apnea was described in almost 90% in a series of 18 patients.
Soft tissue involvement can lead to striking facial asymmetry. The facial characteristics include prominent narrow ears, pointed chin, and nasal changes of a narrow bridge and broadened tip. Cleft lip and palate can occur. Genitourinary, cardiac, abdominal wall defects, and mental retardation have also been reported.
The fatty tumors show a markedly hypoplastic dermis with diminished, thinned collagen bundles and reduced elastic tissue accompanied by fatty replacement. Adipocytes can be clearly seen approaching or even involving the papillary dermis. Identical histologic appearances are seen in nevus lipomatosus superficialis. Adnexa appear to be structurally normal, but may be reduced in number and situated abnormally superficial in the dermis. The conventional view that fatty infiltration of the dermis represents mechanical herniation has been challenged and perhaps represents a heterotopic phenomenon (i.e., an adipocytic nevus). The histologic appearances of the verrucous and papillomatous lesions include hyperkeratosis with epidermal hyperplasia and marked papillomatosis. The dermis is thinned, with fine collagen fibers and increased vascularity, especially in the papillary dermis. The atrophic areas show dermal thinning with sparse attenuated collagen bundles and fatty replacement. Elastic fibers may be increased and thickened. The hyperpigmented foci are characterized by acanthosis with club-shaped rete ridges and increased melanin pigmentation. Melanophages are present in the papillary dermis. By electron microscopy, collagen bundles are found loosely arranged in the extracellular matrix with smaller fibroblasts and irregular thickening of the nuclear lamina.
Tuberous sclerosis (epiloia, Bourneville disease) is a rare inherited systemic illness with an estimated incidence ranging broadly from 1 : 5800 to 1 : 300 000 and may affect up to 2 million people worldwide. Although an autosomal dominant mode of inheritance is sometimes seen, many – if not most cases (up to 80%) – appear to arise by spontaneous mutation. It comprises a constellation of cutaneous lesions as well as cerebral, ocular, cardiac, renal, pulmonary, and skeletal involvement. The sex incidence is equal and there is no racial or ethnic predilection.
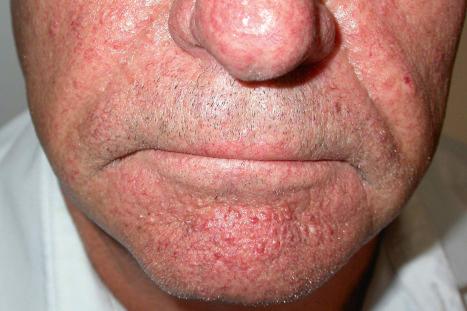
Most characteristic of tuberous sclerosis are facial angiofibromas (adenoma sebaceum), which, while occasionally present at birth, more often appear during early childhood. These were initially thought to be pathognomonic, but can also be seen in multiple endocrine neoplasia type I. They are present in up to 90% of the adults with tuberous sclerosis and consist of smooth, dome-shaped, pink or reddish-brown papules and nodules (sometimes with associated telangiectases), bilaterally and symmetrically distributed, particularly in the butterfly area on the nose and cheeks and often extending to the chin, but sparing the upper lip ( Fig. 21.18 ). Rarely, the lesions can extend to the oral mucosa. Occasionally, the lesions are very extensive and develop into large cauliflower-like masses. Soft fibromas are also found about the face and scalp. Smooth, yellow or red fibrous plaques on the forehead may appear in infancy and be a presenting sign of tuberous sclerosis. Unilateral facial angiofibromas have been noted and could represent segmental expression. Multiple facial angiofibromas without any known genetic disorder have been described.
White macular lesions, which may be single or multiple, are a very frequent initial cutaneous manifestation of tuberous sclerosis. They are best appreciated when the skin is viewed with a Wood's lamp and have been classified into three types :
The most common variant consists of polygonal 0.5–2.0-cm white lesions resembling a thumbprint.
‘Ash leaf’ variegate macules of leukoderma measuring approximately 1–3 cm in diameter are a particular feature of the second variant of tuberous sclerosis ( Fig. 21.19 ).

The third variant consists of guttate scattered 1–3-mm white macules (so-called ‘confetti lesions’).
These macular lesions are said to be present in 70% of patients with tuberous sclerosis. They are evident at birth or develop in the neonatal period. Hypopigmented patches may also affect the hair (poliosis), eyebrows, eyelashes, and occasionally the iris.
Frequently seen is the shagreen patch – peau de chagrin (skin like grainy leather) – mildly yellow lesion found particularly on the lower back (see Fig. 21.19 ). This is a connective tissue nevus, usually presenting in early childhood or around puberty. Large patches in association with spina bifida occulta have been reported. Skin tags are often present, sometimes in large numbers. Other cutaneous lesions include flesh-colored sub- and periungual fibromas ( Fig. 21.20 ). These are found in up to 50% of patients with tuberous sclerosis and usually develop at or around puberty. Café-au-lait macules may sometimes be present. Oral and eyelid angiofibromas with blepharoptosis, enamel teeth pitting, and gingival fibromas can be seen.

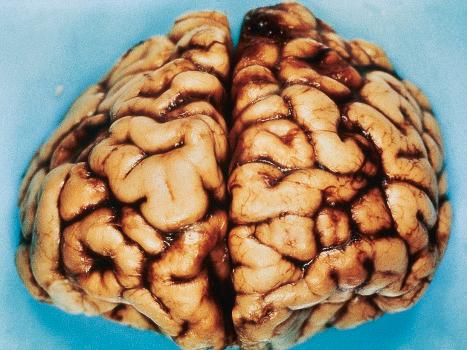
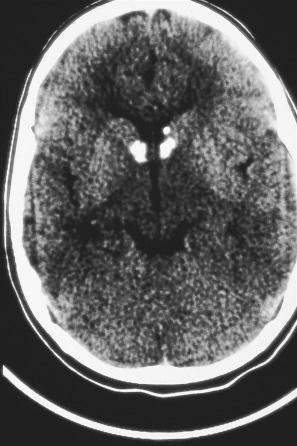
Involvement of the central nervous system usually, but not invariably, results in mental retardation, which is sometimes severe (50–82% of patients). Epilepsy is a common manifestation (80–93% of patients) and often is the presenting symptom. Patients may develop focal or generalized tonic-clonic fits or they can suffer from infantile spasms. The term ‘epiloia’ was coined to define the triad of adenoma sebaceum, mental retardation, and epilepsy. Calcification, particularly of the basal ganglia, is radiologically detected in up to 76% of cases. Ophthalmological investigation reveals the presence of retinal ‘tumors’ or phakomata in up to 53% of cases, although similar lesions can be seen in neurofibromatosis. Occasionally these are calcified. Subependymal nodules and subependymal giant cell astrocytomas are also common.
Cardiac manifestations include murmurs, electrocardiographic abnormalities, heart failure, and sudden death. Pulmonary lesions, although rare, may result in exertional dyspnea, cor pulmonale, and pneumothorax. Affected patients are usually female, often of normal intelligence, and seem less often to suffer from epilepsy. The prognosis is poor.
Radiological examination of the hands and feet often reveals bone cysts, focal sclerosis, and periosteal thickening.
Tuberous sclerosis results from inactivating mutations including deletion, nonsense, missense, and frameshift of two separate genes: TSC1 (9q34) and TSC2 (16p13). These encode the tumor suppressor proteins hamartin and tuberin, respectively. These two proteins heterodimerize and are important regulators of cell proliferation and survival. Loss of TSC1 or TSC2 function in the mTOR (mammalian target of rapamycin) pathway withdraws inhibition with numerous effects in the cells. The ensuing dysregulation of the downstream mTORC1 signaling complex (as opposed to mTORC2) impacts both directly and indirectly on a variety of signaling pathways including Akt in the phosphatidylinositol-3-kinase (PI3K) pathway, extracellular-regulated kinase (ERK), β-catenin, transforming growth factor-β (TGF-β), protein kinase C alpha (PKCα), and p27. mTORC1 impinges on a variety of processes including cell growth, autophagy, cell survival, angiogenesis, lymphangiogenesis, cellular differentiation, and inflammation/immune function. The variety of associated tumors have very low mutational loads relative to carcinomas, but a subset can harbor large chromosomal aberrations.
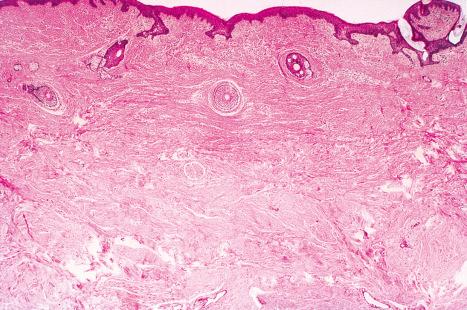
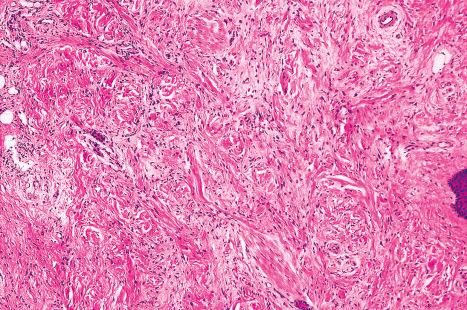
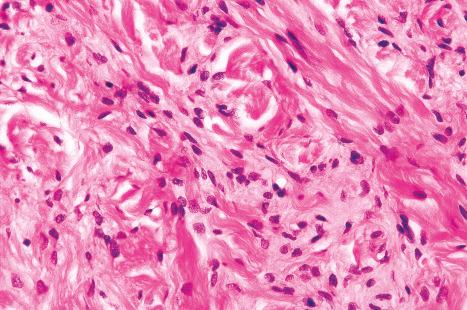
The previously applied term ‘adenoma sebaceum’ is, in fact, a misnomer, the histologic features being those of a fibrovascular hamartomatous proliferation with concomitant atrophy and compression of the skin adnexae. Although often described as an angiofibroma, connective tissue nevus is a more appropriate designation. The lesion consists of an irregular proliferation of fibrous tissue and blood vessels ( Figs 21.21 and 21.22 ). Occasionally, the adnexae become surrounded and compressed by concentric lamellae of collagen ( Fig. 21.23 ).
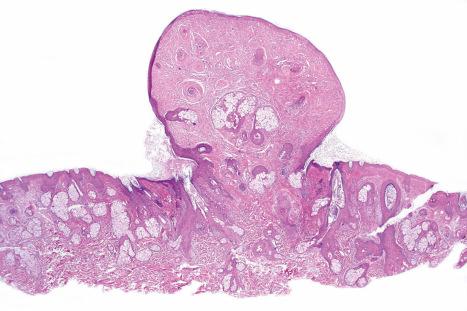
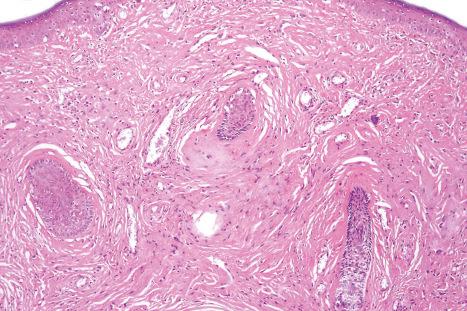
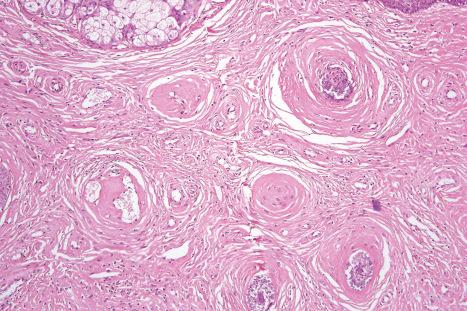
The shagreen patch is a collagenoma, the dermis being replaced by broad bundles of fibrous tissue with diminished or absent elastica ( Figs 21.24 and 21.25 ). Similarly, the sub- and periungual fibromas are fibrous tissue hamartomas.

The hypopigmented macules may show normal or reduced numbers of melanocytes. Ultrastructurally, they show impaired melanogenesis (diminished numbers of small, immature melanosomes). This appears to be due to disrupted melanogenesis and is melanocyte mediated by constitutive activation of mTORC1 that occurs with loss of TSC1 or TCS2 function.
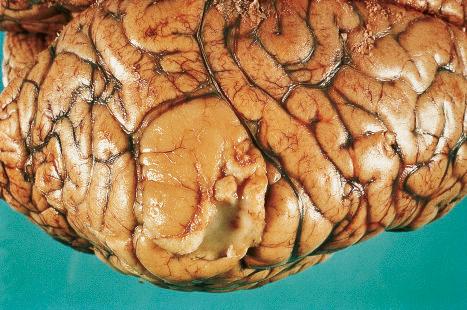
The brain in tuberous sclerosis may be normal or diminished in size ( Fig. 21.26 ). The neuropathology includes cortical tubers, subcortical heterotopic nodules, and subependymal giant cell astrocytomas ( Figs 21.27–19.30 ).


The cardiac manifestations are due to intramyocardial rhabdomyomas, composed of large vacuolated (glycogen-filled) muscle cells. Spontaneous regression is well documented.
The kidneys contain angiomyolipomata (often bilaterally and multiple) in up to 60% of patients and occasionally show infantile polycystic disease. Interestingly, cutaneous angiomyolipomas not associated with tuberous sclerosis are negative for MART-1 and HMB-45. Renal cell carcinoma (which may present in infancy or childhood) is also sometimes encountered. A few patients with tuberous sclerosis complex also have mutations in the nearby PKD1 gene, resulting in autosomal dominant polycystic kidney disease.
Multiple cysts (lymphangiomyomatosis) are the most important pulmonary manifestation. Females are predominantly affected. Angiomyolipoma at this site is exceptional.
There may be an association with neuroendocrine (parathyroid, pituitary, and pancreatic) tumors.
In general, tuberous sclerosis is associated with a poor prognosis, but partial or mosaic expression of the disease is not uncommon and such patients may enjoy a normal life span. Treatment with mTOR inhibitors is transforming the clinical management of some of the more devastating manifestations of this disease.
Nephrogenic systemic fibrosis (formerly known as nephrogenic fibrosing dermopathy) is a multiorgan disease that can have a scleroderma-like dermatosis and is associated with renal failure often combined with exposure to gadolinium.
Although it was initially thought to develop only in individuals undergoing hemodialysis, subsequent publications documenting its occurrence in patients being treated with peritoneal dialysis, or following transplantation, or solely with renal failure, broadened the definition. Most patients have chronic kidney disease with the vast majority having stage 5 disease (estimated glomerular filtration rate [GFR] <15 mL/min/1.73 m 2 ). Disease course can parallel renal function. Some patients with acute renal disease have also been reported to develop this condition. Although the vast majority of documented patients are adults, presentation in children with renal insufficiency has been seen. While several large studies have demonstrated an association with gadolinium exposure and renal failure, clearly not all patients with these conditions develop nephrogenic fibrosis. Some of this variability may be due to the type of gadolinium contrast used. The macrocyclic chelate bonds are more stable than linear bonds and thus considered to confer less risk in patients with compromised kidney function as defined by GFR guidelines. Additional reported risk factors include cumulative exposure to gadolinium, erythropoietin exposure, and elevated ionized calcium and phosphate serum concentrations. A mouse model of the disease suggests that changes in systemic iron mobilization may play a role as well.
Although previously considered primarily a cutaneous disease, it is now known to affect other organs, as documented in several autopsy cases. Extracutaneous findings can be seen, including in the deep soft tissue, blood vessels, thyroid, heart, kidney, dura, and lung. In the skin, the condition is characterized by rapidly growing, symmetrical skin-colored or erythematous papules and nodules that coalesce to form erythematous or hyperpigmented progressive, brawny plaques, sometimes with a peau d'orange appearance ( Figs 21.31 and 21.32 ). These lesions on the breast sometimes mimic inflammatory breast cancer. The plaques have an irregular border and islands of sparing are sometimes described. The limbs and trunk are predominantly affected. The face is usually uninvolved, although there are a number of cases with yellow scleral plaques. The skin is markedly thickened, hard, and has a wooden texture. Lesions may be pruritic, painful, or associated with a burning sensation. Flexion contractures are a common complication, often resulting in considerable immobility. As a consequence, morbidity is high. Occasionally, patients may develop redundant skin similar to cutis laxa and generalized elastolysis. Mortality can occur due to thromboembolism.


The exact mechanism of nephrogenic systemic fibrosis is still being unraveled. The presence of high levels of gadolinium due to renal failure is thought to result in transmetallation, where various serum ions can interact with the gadolinium contrast complex, releasing free gadolinium. Free gadolinium is toxic in animal studies and can be detected in tissue specimens from patients with nephrogenic systemic fibrosis. In vitro studies have shown gadolinium to be profibrotic and proinflammatory, eliciting growth factors from monocytes.
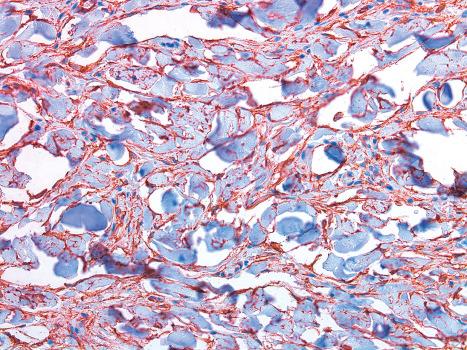
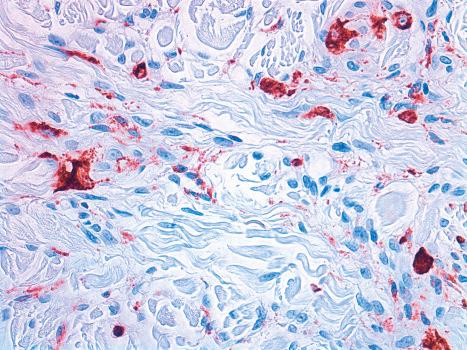
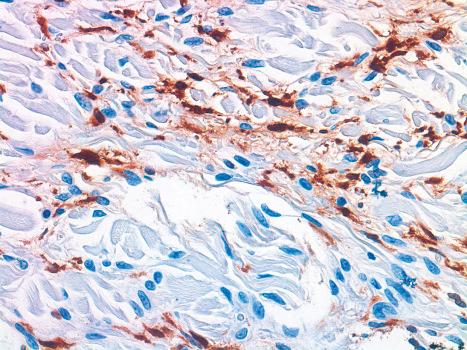
Histologically, early lesions are characterized by a subtle proliferation of fibroblasts and variable numbers of large epithelioid and stellate cells ( Figs 21.33–21.35 ). In an established plaque, there are conspicuous CD34+ dermal dendritic cells with admixed CD68+ macrophages and factor XIIIa-positive cells ( Figs 21.36–21.38 ). Multinucleate forms are present and can show an osteoclast-like morphology. There are numerous fibroblasts associated with irregularly distributed thickened collagen bundles and increased numbers of elastic fibers. Sclerotic bodies or elastocollagenous balls, irregularly shaped paucicellular areas of collagen which can ossify, have been described. Cleftlike spaces are typically present, and there is increased dermal stromal mucin. Progression of the lesion is accompanied by capillary proliferation. During the earlier stages of the illness myofibroblasts have also been identified, but they are typically absent in more chronic lesions. Osseous metaplasia and dystrophic calcification is sometimes evident. Calciphylaxis has been documented in several cases.

Nephrogenic systemic fibrosis is usually devoid of a significant inflammatory cell infiltrate, although occasionally a light superficial and deep perivascular lymphocytic infiltrate may be evident. Granulomatous inflammation has been rarely described.
Nephrogenic systemic fibrosis shows particular histologic overlap with scleromyxedema. Mucin is generally more abundant in the latter condition and inflammatory cells (including plasma cells) are often conspicuous, but these findings are not always reliable to distinguish the two entities. Clinically, the two conditions are quite different: scleromyxedema characteristically affects the face, is commonly associated with systemic involvement, and is accompanied by paraproteinemia in most patients.
Restrictive dermopathy is a very rare predominantly autosomal recessive condition that is classified within the group of lethal congenital contracture syndromes and presents with intrauterine (fetal) akinesia or hypokinesia deformation sequence (FADS). Less than 75 cases have been reported. It is invariably fatal, the average survival time after birth being less than 1 week.
Affected infants are born prematurely at approximately 31 weeks and die from pulmonary hypoplasia and respiratory insufficiency. Spontaneous complete chorioamniotic membrane separation can occur. The clinical manifestations include a rigid, taut, adherent skin with erosions, ulcers, and a tendency to tear easily, generalized contractures, a dysmorphic facies with micrognathia, and a mouth fixed in an ‘O’ shape. Additional features may include blepharophimosis, absent eyelashes, dilatation of the ascending aorta, dextrocardia, dysplasia of the clavicles, and enlarged fontanelles with wide cranial sutures.
The majority of restrictive dermopathy is caused by null autosomal recessive mutations in ZMPSTE24 ( FACE-1 ), encoding a zinc metalloprotease which modifies prelamin A to lamin A, with a minority of patients harboring autosomal dominant mutations in LMNA . Defects in ZMPSTE24 result in accumulation in farensylated prelamin A along the nuclear membrane; the degree of protease dysfunction can correlate with disease severity. Mutations in LMNA are also involved in Hutchinson-Gilford progeria syndrome and result in truncated lamin A precursors. Prelamin A, the precursor to lamin A, plays both a structural role in forming the nuclear lamina and functional roles in nuclear chromatin remodeling and nuclear protein transport. The accumulation of prelamin A results in altering of nuclear contours, is toxic to cells, and can disrupt DNA repair mechanisms. Increased oxidative stress could play a role in cell damage. A transgenic mouse model indicates that disruption of lamin A inhibits normal skin development in the infant. The discovery of these defects has enabled prenatal diagnosis.
Histologically, the epidermis appears normal to slightly thickened, although it is flattened with loss of the rete ridges and a straight lower border. The dermis is thinned and the reticular collagen appears compact and oriented parallel to the surface. Elastic tissue is reduced, and the dermal appendages are poorly developed. The subcutaneous fat may appear increased in thickness.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here