Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
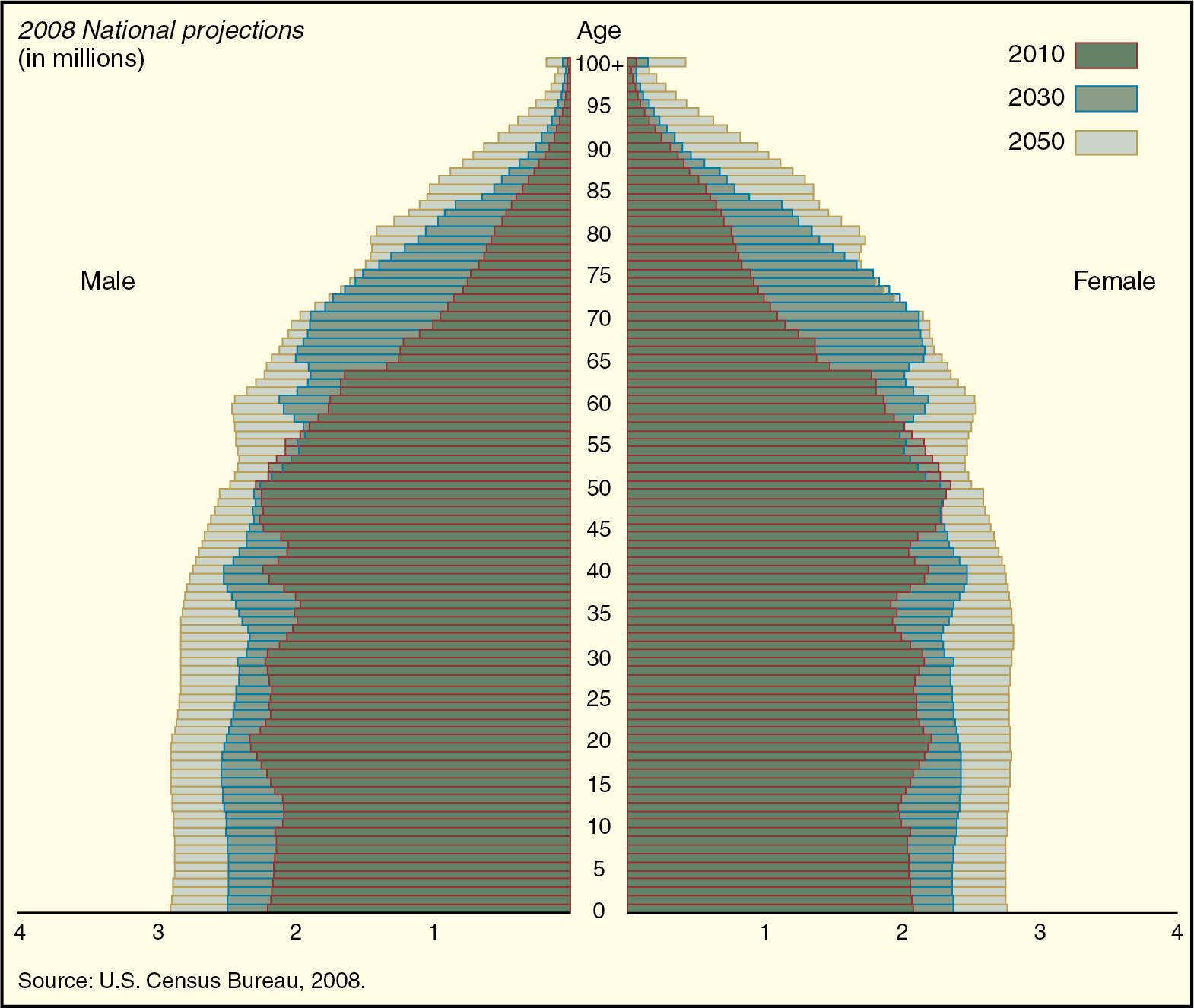
Compared to 100 years ago, people are living much longer. The US life expectancy for men in 1900 was 48 years and for women, 51 years. Currently the average life expectancy in the United States exceeds 75 years. The elderly, defined as those older than 65 years, constitute one of the fastest-growing segments of the population. In 2010, the US elderly population numbered 47 million, representing 17% of the total population. In 2018, there were an estimated 52 million US citizens 65 years and older, and by 2030 there will be approximately 80 million elderly ( Fig. 30.1 ). This growth in the older population is a worldwide phenomenon. In the United States alone, there was a 34% growth in the US population age 65 years and older from 2010 to 2020, and by the year 2025 there are expected to be 15 million individuals aged 85 years. The social, economic, and political costs of these demographic changes are enormous.
Surgeries that were considered prohibitively high risk and rare in octogenarians two decades ago are now being performed routinely. Many elderly patients now undergo complex major cardiac, orthopedic, and other noncardiac surgery. With the changing demographics and advancement in surgical techniques, this trend is likely to grow.
Elderly patients utilize disproportionately more medical care than younger people. By some estimates, 35% of total US medical costs are spent on patients older than 65 years. Per capita healthcare costs are three times higher in patients older than 85 years versus those younger than 65 years. About 40% of all surgery and inpatient procedures are performed on elderly patients.
Though the impact of aging and its associated diseases has been recognized for a long time, optimal care of the elderly continues to evolve. Most anesthesia providers for adults are now involved in the care of geriatric patients and so can be considered “geriatric anesthesiologists.” Thus it is imperative that an anesthesiologist know the impact of aging on physiology and pharmacology, the impact of comorbidities, and the composite effect of all these changes on perioperative outcomes. Elderly patients are not only “old” or “very old”; they are a unique phenotype comprising an aged biological system, multiple comorbid diseases, and a spectrum of geriatric syndromes. Preoperative assessment of the elderly patient must involve assessment of geriatric syndromes, functional status, frailty, cognition, nutritional status, and goals of care.
In the past few decades there has been significant research on the process of aging, the mechanisms that underlie aging, and potential interventions that could delay aging. Aging appears to be driven by progressive accumulation of a variety of random molecular defects that build up in cells and tissues. Aging is thus a continuous process, starting early and developing gradually, instead of being a distinct phase that begins in middle to later life. It is well recognized that all individuals do not age at the same rate. Five key elements seem to contribute to the individuality of the human aging process: genes, nutrition, lifestyle, environment, and chance.
There are two main evolutionary theories for biological aging: the mutation accumulation theory (gene mutations that did not impact reproduction accumulated over time that ultimately resulted in the aging phenotype) and the antagonistic pleiotropy theory of aging (genes that were beneficial in youth and thus favored by natural selection have deleterious effects in late life). Regardless of how aging developed over time, it is clear that aging and longevity are influenced to a degree by our genetic makeup, accounting for about 25% of the variance in the human life span. Multiple genes contribute to the aging phenotype, but there are no specific genes for aging.
There are many mechanisms that can lead to defects and aging, and it is highly likely that no single process is responsible for physiologic aging. The following aging mechanisms are considered the most important and may work synergistically:
Oxidative damage: Free radicals, reactive oxygen species, are by-products of oxygen use and energy metabolism. These free radicals can cause damage to chromosomal deoxyribonucleic acid (DNA) and subsequently impair gene function and damage mitochondrial DNA and telomeres.
DNA damage and repair: Age-related increases in somatic mutations and other forms of DNA damage are well recognized. They can produce permanent alterations of DNA sequences and hence function. A key enzyme involved in the repair of damaged DNA is poly(ADP-ribose) polymerase 1 (PARP-1), and its levels correlate positively with life span. Centenarians who have maintained generally good health have higher levels of PARP-1 than the general population. Telomeres are regions of repetitive nucleotide sequences found at the end of each chromosome. They protect the ends of the chromosome from deterioration and from fusion with nearby chromosomes. A growing body of evidence links telomere length to aging and mortality. With normal aging, telomeres shorten in several tissues, thus limiting the ability of these tissues to regenerate over time, ultimately leading to loss of function and cell death. Premature shortening of telomeres can occur and has been associated with certain diseases such as vascular dementia, psychological and physiologic stress, and others. Telomere shortening is potentially one way by which environmental factors contribute to premature aging.
Mitochondrial senescence: Mitochondria are intricately involved in energy metabolism and generation of oxygen radicals. Just like somatic DNA, mitochondrial DNA also develops point mutations and deletions over time. An increased incidence of mutated mitochondrial DNA has been noted in aging brain tissue, muscle cells, and gut epithelium.
Malfunction of proteins: Damaged, misfolded, or malfunctioning proteins also accumulate over time and are seen in many age-related diseases such as Parkinson disease, Alzheimer disease, and senile cataracts. Though these faulty proteins should be cleared rapidly, their accumulation and aggregation over time become less efficient. Malfunctioning or accumulated proteins lead to loss of particular functions and ultimately to dysfunction of the entire cell.
Environmental factors: Aging is affected by environmental factors that interact with the genome in various ways. It has been recognized that a low-calorie diet leads to a longer life span. This phenomenon is explained by the disposable soma theory, which postulates that natural selection has led to those pathways that optimize utilization of metabolic resources (energy) among competing physiologic demands (growth, maintenance, reproduction). Insulin and insulin-like growth factor gene systems seem to play a crucial role in these processes. Activation of these genes alters the function of a variety of downstream stress response genes, genes encoding for a variety of antimicrobial proteins, and pathways involved in protein turnover.
The boundary between aging and disease pathogenesis is somewhat arbitrary. The same cellular and molecular functions that contribute to improved life span are also responsible for degenerative diseases such as osteoporosis, osteoarthritis, and dementia.
Aging affects the brain, and cognitive decline with aging has been considered an unavoidable consequence of brain senescence. Though there are changes with aging, new evidence suggests that part of these changes is due to aging-related medical conditions. Brain function associated with the normal process of aging should be differentiated from specific changes due to neurodegenerative diseases.
All major cell types in the brain undergo structural changes with aging. These changes include neuronal cell death, dendritic retraction and expansion, synaptic loss and remodeling, and changes in glial cell (astrocyte and microglia) reactivity. There is an overall reduction in neuronal regenerative capacity. The mass of the brain decreases by approximately 15% with aging. This decrease is due to cell loss and shrinkage of cell volume. There is a compensatory increase in cerebrospinal fluid volume. However, all areas of the brain do not shrink at the same rate. The cerebellum, prefrontal cortex, and hippocampus demonstrate increased atrophy after middle age. In addition, white matter is lost at a greater rate than gray matter during the aging process and may contribute to age-related cognitive decline and increase risk for age-related brain disorders.
Changes in brain structure are not limited only to cell volume, but also affect synaptic connections. Neural connections play a critical role in brain function and are responsible for the neural plasticity of the brain. With aging, neural plasticity decreases, yet neuronal connectivity may increase.
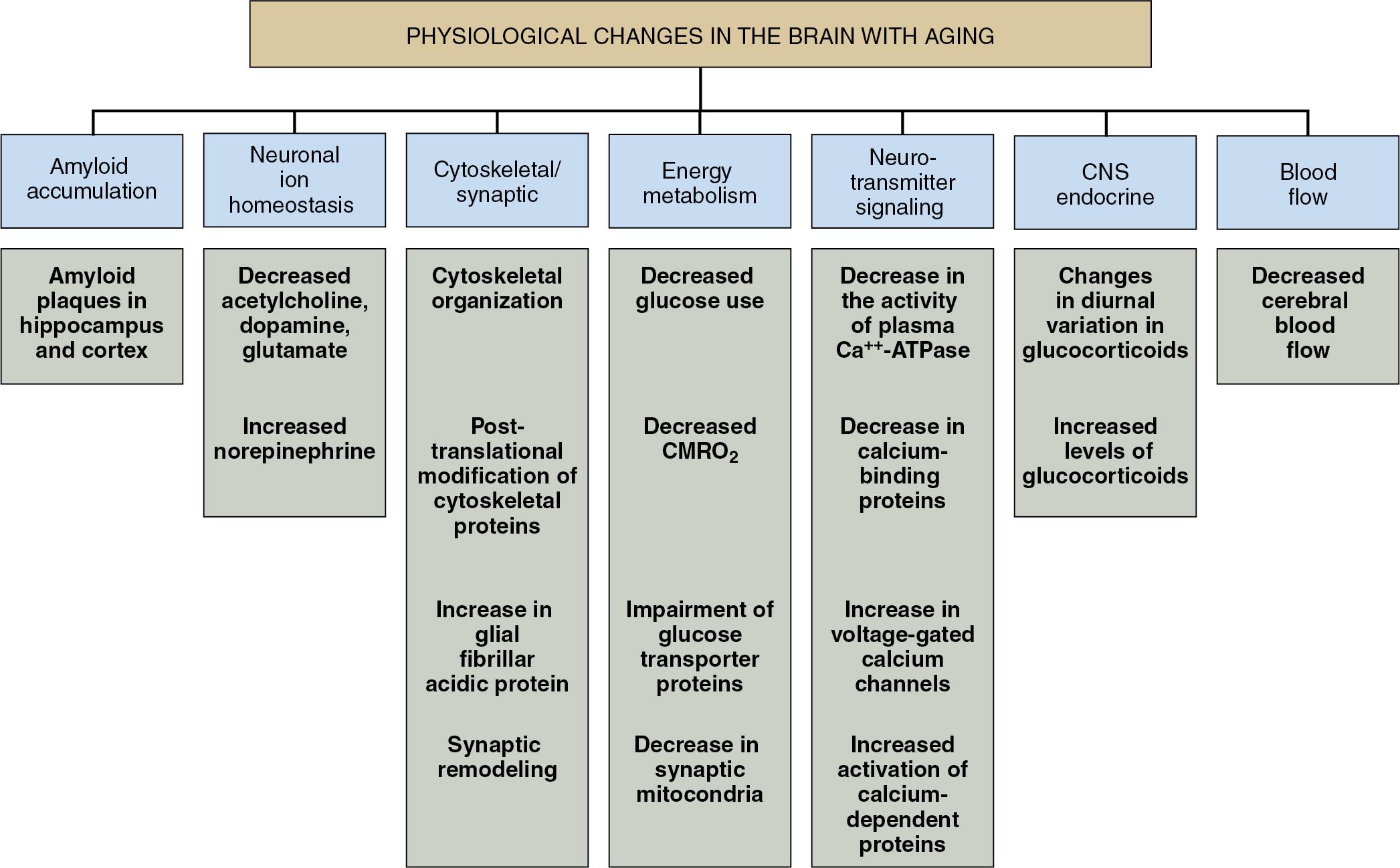
Cellular signaling transduction pathways, cytokines, and growth factors that are involved in neuronal excitability and plasticity are affected by aging. There are significant changes in neurotransmitter signaling. Cholinergic signaling, which plays a crucial role in learning and memory, can be especially impaired in patients with Alzheimer disease. Presynaptic and postsynaptic dopaminergic neurotransmission can also be significantly affected by aging. In conjunction with thalamic contraction, there is impairment of dopamine signal transduction pathways. These pathways play a significant role in age-related deficits in motor control and may explain the susceptibility of the elderly to the extrapyramidal side effects of dopamine receptor antagonist drugs. Norepinephrine levels are increased in some parts of the aging brain, while levels of α 2 -agonist receptors may decrease. Levels of ionic glutamate receptors and γ-aminobutyric acid (GABA) A binding sites decrease with age. Neurovascular, endocrine, and immunologic changes are also noted in the brain with aging ( Fig. 30.2 ). Aging brain has decreased cerebral blood flow due to a reduction in cerebral metabolic rate and is more susceptible to metabolic stress.
Significant cognitive dysfunction is related to aging and age-related diseases. The incidence of many chronic diseases increases proportionally with age, so it can be difficult to differentiate age-related cognitive dysfunction from disease-related cognitive dysfunction in any particular patient. Hypertension, diabetes mellitus, nutritional deficiency, chronic obstructive pulmonary disease, obstructive sleep apnea, thyroid dysfunction, alcoholism, depression, and medications (opioids, benzodiazepines, anticonvulsants, antipsychotics, antidepressants, antihistamines, anticholinergics, and central nervous system stimulants) can affect cognitive function. General intellectual functioning, attention, memory, and psychomotor function decline with age, but language and executive function remain more or less intact.
Tissue elasticity decreases with age, whereas the proportion of collagen increases. Elastin becomes fragmented because of increased activity of matrix metalloproteinases, and collagen becomes increasingly cross linked. These changes produce increased stiffness in tissues, causing significant structural and physiologic changes in the cardiovascular system.
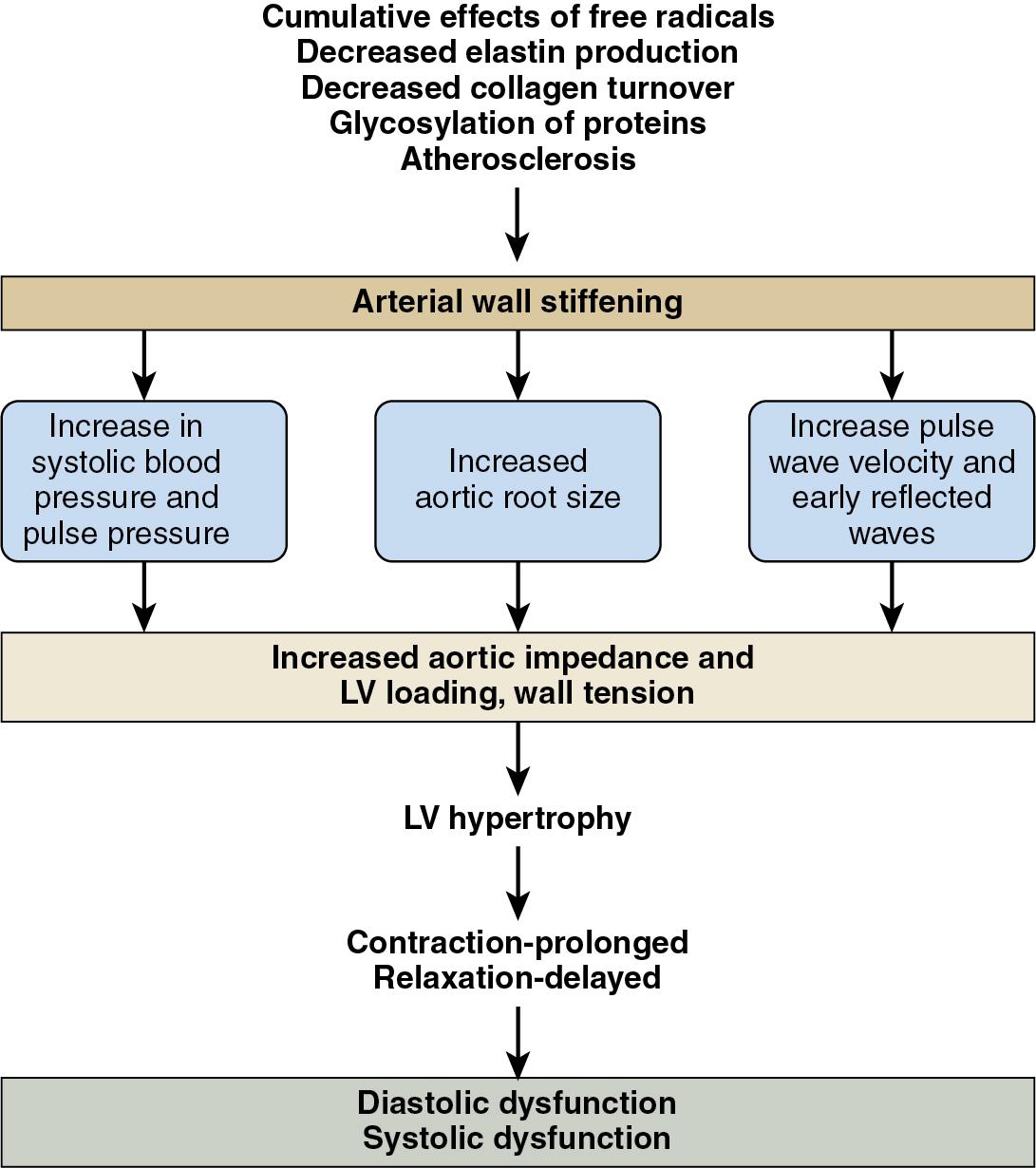
Two major structural effects occur in blood vessels: stiffening and atherosclerosis. The first is a natural change in the composition of blood vessel walls, with decreasing amounts of elastin and increasing amounts of collagen. The cumulative effects of free radicals and glycosylation of proteins add to the progressive stiffness and thickening of arteries, but the aortic lumen actually increases in diameter despite the arterial stiffness/thickening. Atherosclerosis and arterial stiffening due to elastin/collagen changes occur simultaneously, but these processes are quite different. Atherosclerosis is a heterogeneous process that happens quite uniformly throughout the conduit arteries. The severity of blood turbulence and shear stress provide a nidus for the atherosclerotic process. Inflammation is the hallmark of atherosclerosis, with increased cholesterol as a cofactor. Atherosclerosis causes occlusion of arteries, whereas age-related changes typically cause dilatation. Functionally the arteries become less responsive to both vasoconstrictors and vasodilators owing to changes in the endothelium. Though levels of endothelin 1 (a potent vasoconstrictor) are increased, the effect of other vasoconstrictor chemicals such as norepinephrine, ephedrine, and phenylephrine is attenuated.
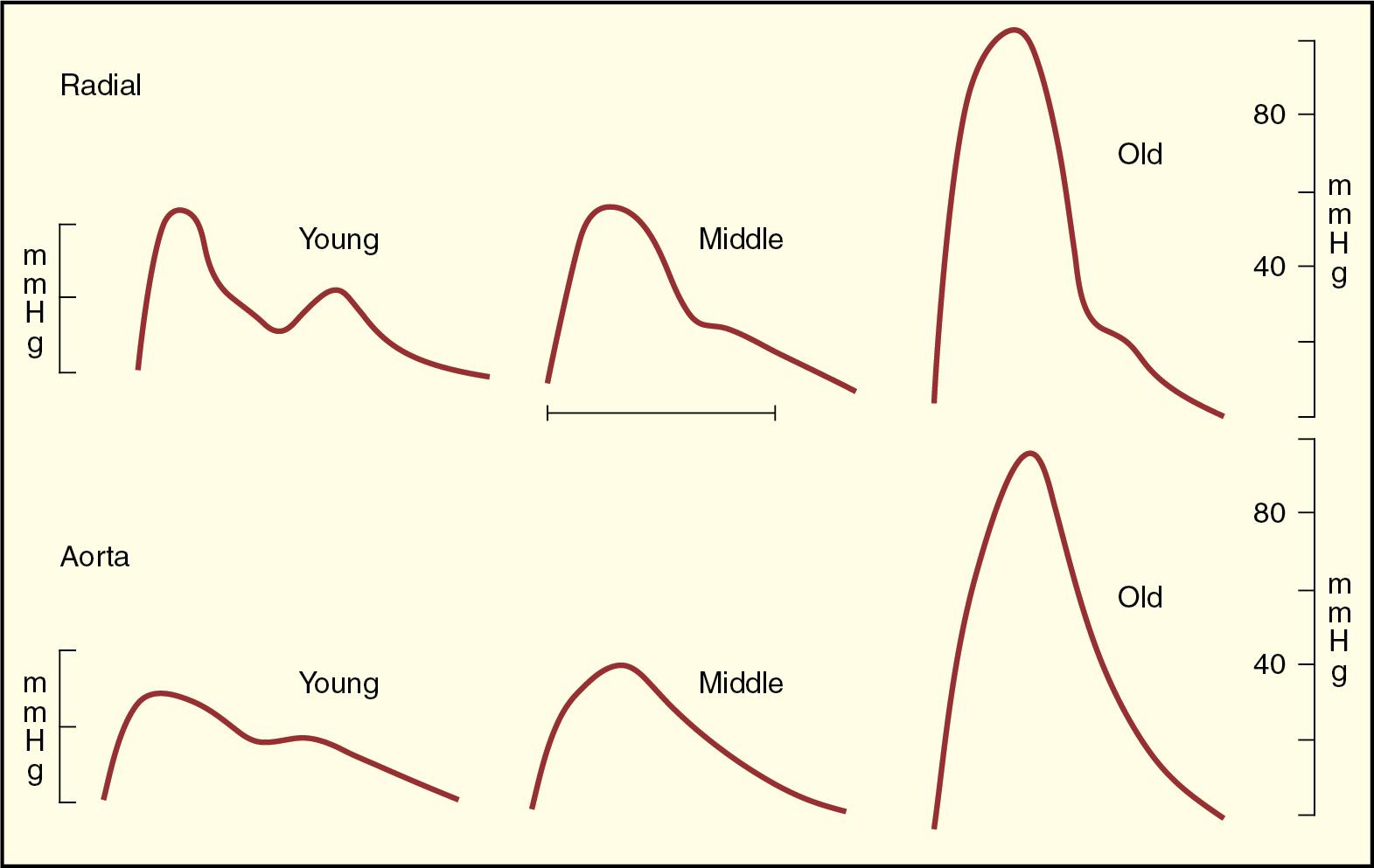
The consequence of stiff arteries is that the pulse wave of the ejected blood travels faster. Velocity increases twofold between the ages of 20 and 80, independent of blood pressure. Stiffer arteries also allow pressure to reflect from the periphery back to the heart quicker while the aortic valve is still open and the heart is ejecting, effectively increasing the afterload on the heart ( Fig. 30.3 ). Thus systolic blood pressure is augmented. Data from the Framingham Heart Study show that systolic blood pressure increases by about 5 mm Hg per decade until the age of 60 and thereafter increases by 10 mm Hg per decade. Diastolic pressure remains unchanged.
These changes lead to alterations in ventricular-vascular coupling. The heart responds to the increased impedance by developing left ventricular hypertrophy. Left ventricular mass increases by 15% between age 30 and 70, with subsequent effects on systolic and diastolic function ( Fig. 30.4 ). These chronic changes make the myocardium more prone to ischemia. Decreased oxygen supply due to an increase in left ventricular end-diastolic pressure and decreased aortic diastolic pressure occurs at the same time as oxygen demand increases owing to ventricular hypertrophy, increased left ventricular end-systolic pressure, increased aortic pressure, and increased duration of systole ( Fig. 30.5 ).
The incidence of diastolic dysfunction increases with age, and this has been proven by detailed echocardiographic studies. Any systolic dysfunction in the elderly should be considered abnormal, especially if it is accompanied by a wall motion abnormality. Though the cardiac myocytes continue to multiply during life, their ability to keep pace with apoptosis decreases. Consequently there is a net loss of about half of cardiac myocytes during life. Older myocytes are stiffer and lack the ability for ischemic preconditioning. The incidence of heart failure increases significantly with age. With heart failure the ratio of β 1 - to β 2 -adrenergic receptors also changes. In persons without heart failure the left ventricle has 80% β 1 -adrenergic receptors and 20% β 2 -adrenergic receptors. In heart failure the ratio changes to 60% β 1 receptors and 40% β 2 receptors. This can have a significant impact on how adrenergic agonists and blockers impact ventricular function.
Ventricular septal thickness increases with age, as does thickness of the aortic and mitral valve leaflets. Annular dilatation is very common, and 90% of healthy octogenarians demonstrate some form of mild multivalvular regurgitation, which is typically central and associated with normal-appearing valve leaflets. Left atrial chamber size also increases. The incidence of aortic sclerosis and stenosis increases with age.
The electrical system of the heart declines with age. The number of pacemaker cells is reduced by about 90% by age 70. Prolongation of the PR interval, QRS duration, and QT interval is noted. The incidence of dysrhythmias, especially atrial fibrillation, increases significantly. The resting heart rate slows, and there is a marked decrease in maximum heart rate in response to exercise. The response to atropine administration is half that of younger individuals. Decreased chronotropic, inotropic, and lusitropic responses to dobutamine have been noted in the elderly. Heart rate variability (i.e., variation in instantaneous heart rate and the R-R interval), which is considered a marker of physiologic reserve, is decreased.
Normal age-related changes in cardiovascular physiology include a decrease in peak heart rate, peak cardiac output, and peak ejection fraction. In addition, there are changes in autonomic tone and baroreceptor reflex activity. There is overall dampening of autonomic and baroreceptor activity with aging. This results in a slower resting heart rate and decreased ability to increase cardiac output via a change in heart rate. Compared to younger individuals, increases in cardiac output in the elderly are achieved by increasing end-diastolic volume rather than by increasing heart rate. This results in an increased reliance on atrial contraction for maintenance of cardiac output. Overall, the ability of the cardiovascular system to withstand stress is significantly decreased.
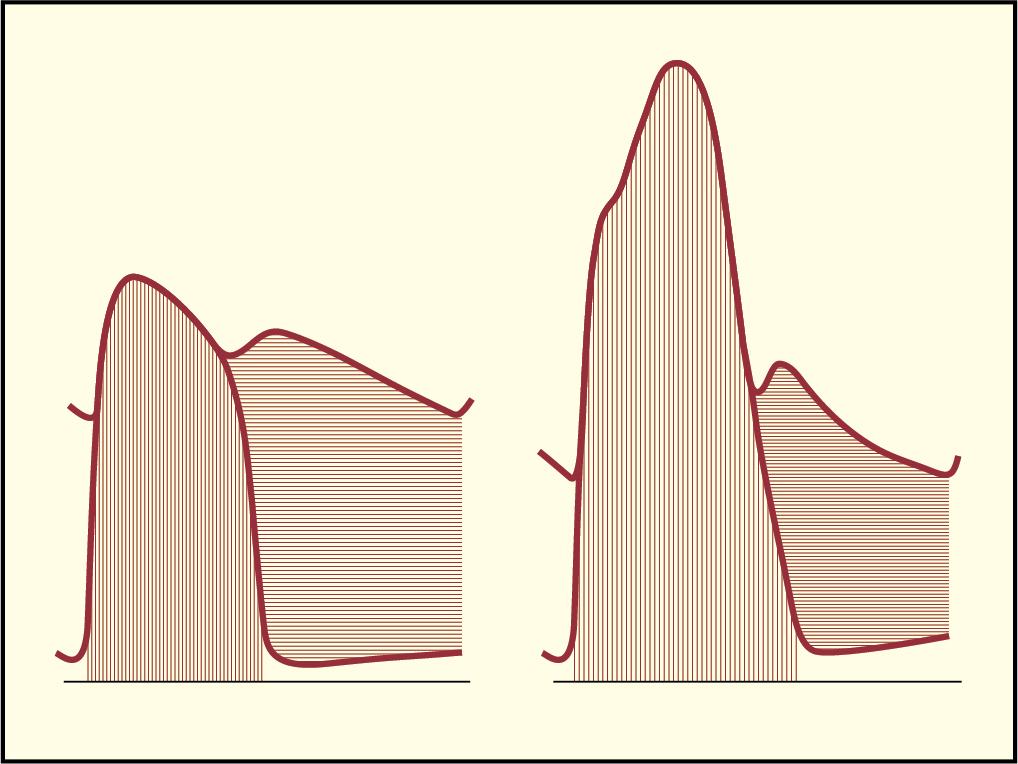
Age-related physiologic changes in the respiratory system can be grouped into three broad categories: (1) mechanical changes, (2) changes in gas exchange, and (3) changes in sensing mechanisms. A progressive decrease in elasticity alters respiratory mechanics and alveolar architecture. The chest wall becomes stiffer as lung tissue loses its intrinsic elastic recoil. Thus chest wall compliance decreases while lung compliance increases. Total lung capacity remains the same, residual volume increases, and vital capacity decreases. Mechanical changes lead to increased work of breathing and make the elderly more prone to respiratory failure. Owing to a progressive decline in diaphragmatic strength and changes in the airway, expiratory flows such as FEV 1 (forced expiratory volume in the first second of expiration) and FEF 75% (forced expiratory flow at 75% of forced vital capacity) decrease ( Fig. 30.6 ).
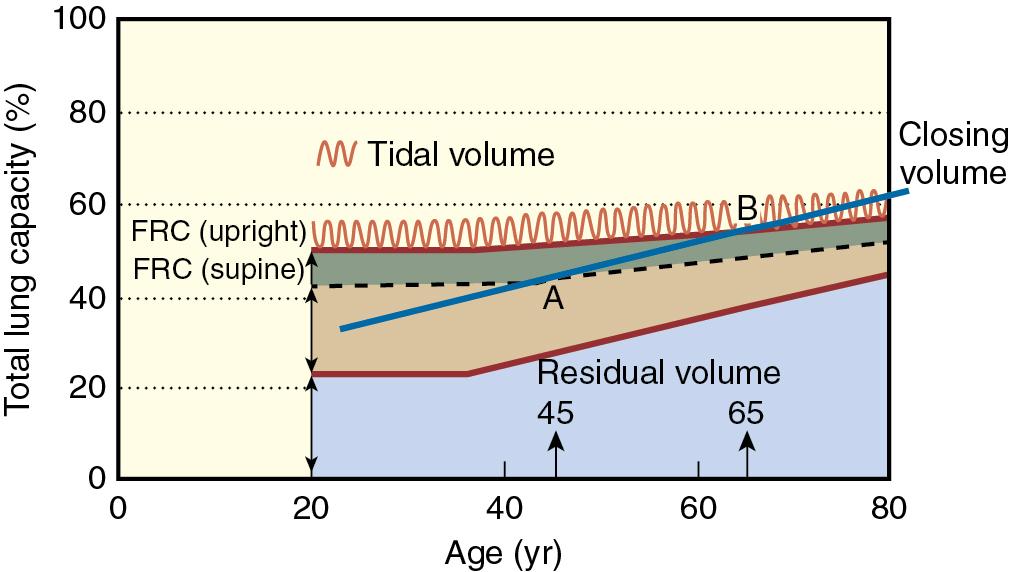
Complex changes at the alveolar level cause a reduction in arterial oxygen tension with age. It is estimated that the arterial partial pressure of oxygen (Pao 2 ) decreases at an average rate of 0.35 mm Hg per year. Mean arterial oxygen tension on room air decreases from 95 mm Hg at age 20 to less than 70 mm Hg at age 80. These changes in arterial oxygenation are caused by an increase in ventilation/perfusion mismatching and to a lesser extent by intrapulmonary shunting. The reduction in elastic tissue in the lung interstitium results in emphysematous changes in lung/airway architecture. Therefore there is an increased tendency of airways to close (i.e., closing volume increases). Closing volume approaches tidal volume, so the elderly are more prone to atelectasis. Residual volume also increases as a proportion of total lung capacity. It is 20% at age 20 and 40% at age 70. Protective cough mechanisms may become attenuated, and both decrease the ability to clear secretions and increase the risk of aspiration. The endurance of the respiratory muscles decreases. Functionally there is reduced respiratory drive in response to hypoxia, hypercarbia, and a resistive load. Increased airway reactivity is also seen.
Various aspects of renal function decline with normal aging. The salient changes in renal function that accompany normal aging are as follows:
Renal vascular dysautonomy: The attenuation of autonomic renal vascular reflexes that are present to protect the kidney from hypotensive and hypertensive states
Senile hypofiltration: The progressive decline in the glomerular filtration rate (GFR) of about 1 mL/year after age 30 that is seen in about two-thirds of the elderly
Tubular dysfunction: Reduction in the maximal tubular capacity to reabsorb and excrete solutes, especially sodium
Medullary hypotonicity: The reduction in tonicity of the renal medulla, which causes a reduced antidiuretic hormone effect and thereby a reduction in water absorption. Elderly patients are unable to maximally concentrate or dilute urine
Tubular frailty: Renal tubular cells being more susceptible to hypoxic or nephrotoxicity injury and take longer to recover from acute tubular necrosis
The clinical consequences of all these changes can be profound. The aging kidney is more susceptible to injury, less able to accommodate hemodynamic changes, and not able to handle water and salt perturbations. A low GFR and diminished tubular function lead to reduced ability to concentrate urine, which means that the obligatory urinary volume to excrete waste products must increase. However, also owing to decreased GFR, the ability to excrete excess free water is diminished, making the elderly more prone to fluid overload, pulmonary edema, and development of hypoosmolar states (e.g., hyponatremia) if large amounts of hypoosmolar fluids are administered.
Aging also causes decreased sensitivity of volume and osmoreceptors, so the thirst response may be diminished and drinking behavior altered. Bladder dysfunction or incontinence can also alter drinking behavior to avoid embarrassing situations. Since many elderly patients have mobility problems or difficulties with the activities of daily living (ADLs), difficult access to fluids further predisposes them to dehydration.
Aging significantly affects the motility of the oropharyngeal/upper esophageal area, colonic function, gastrointestinal immunity, and gastrointestinal drug metabolism. Liver size, blood flow, and perfusion normally decline by 30% to 40% between the 3rd and 10th decades. However, these changes do not have a significant impact on liver function. Liver function has to decrease by 70% to have clinically relevant effects. No significant abnormalities are noted on conventional liver function tests in the elderly.
Significant changes in the immune system include both changes in the innate immune system (macrophages, neutrophils, natural killer cells, etc.) and in the adaptive immune systems. The bactericidal activity of immune cells is decreased. Increased levels of cytokines and chemokines have been noted, which is consistent with a low-grade chronic inflammatory process in the elderly. Age-related functional changes have also been noticed in T-cell and B-cell functions. These changes are thought to impact the ability of the elderly to fight infection and control cancers.
The endocrine glands tend to atrophy in the elderly and reduce hormone production. This frequently leads to impaired endocrine function, such as impaired glucose homeostasis. Deficiencies of insulin, thyroxine, growth hormone, renin, aldosterone, and testosterone are often present. Chronic electrolyte abnormalities, diabetes mellitus, hypothyroidism, impotence, and osteoporosis are common.
The resting metabolic rate declines approximately 1% per year after age 30, and total energy expenditure also goes down, probably secondary to a decline in lean body mass. However, in elderly persons with multiple morbidities and those affected by chronic illness, total energy expenditure increases. Sick individuals often expend most of their energy performing simple ADLs. Longitudinal studies have demonstrated that peak oxygen consumption declines progressively with aging, so the elderly are unable to cope with high oxygen demands.
There is a 10% to 15% decrease in intracellular fluid owing to loss of muscle mass. Total fat content decreases, but the percentage of fat per total body weight increases. Weight tends to decline with aging because of a significant reduction in lean body mass, which is predominantly composed of muscle and visceral organs. Muscle atrophy is greater in fast-twitch than in slow-twitch muscle fibers, presumably secondary to loss of motor neurons. Waist circumference increases throughout one’s life span are due to increasing visceral fat. In some individuals, fat can also accumulate inside muscle tissue, affecting muscle quality and function. Fibroconnective tissue also builds up with aging, and it too can affect muscle quality and function. This loss of muscle mass and quality results in reduced muscle strength that ultimately affects functioning and mobility.
Frailty is defined as a state of reduced physiologic reserve that is associated with increased susceptibility to disability. It is related to normal changes of aging, chronic disease, and inflammation and is characterized by failure of the body to respond to additional stresses such as surgery or infection. Aging, however, does not necessarily guarantee frailty; there are elderly patients who may not become frail just as there are patients under the age of 65 who may meet criteria for being frail. In addition, there is no gold standard for assessing frailty, although there are several well-studied and validated instruments such as the Clinical Frailty Scale, Edmonton Frail Scale, Risk Analysis Index, and Frailty Index. Frailty assessments can be used as a risk stratification tool to provide a more comprehensive informed consent and shared decision making, or they can be used as a more formal assessment to identify areas that may be modified preoperatively to potentially improve outcome. A proposed phenotype definition of frailty is characterized by weight loss, fatigue, impaired grip strength, low physical activity, slow gait speed, and, in some patients, cognitive decline. All these changes lead to a decreased reserve. Compared to their nonfrail counterparts, elderly patients who are frail are likely to decompensate more quickly and recover more slowly from pathologic or physiologic insults such as surgery. Frailty is more prevalent in the perioperative patient compared to the general population, and it is estimated that 25% to 40% of elderly perioperative patients are frail. Current evidence suggests that geriatric surgical patients who are frail have a two- to fourfold increase in mortality and postoperative complications as well as a fivefold increase in hospital discharge to places other than home.
Geriatric syndromes encompass clinical conditions that are frequently encountered in older people. The pathophysiology of geriatric syndromes is multifactorial and can involve multiple unrelated organ systems. These syndromes have deleterious effects on independent functioning and quality of life. The list of geriatric syndromes includes incontinence, delirium, falls, pressure ulcers, sleep disorders, problems with eating or feeding, pain, and depressed mood. In addition, dementia and physical disability can also be considered geriatric syndromes. Geriatric syndromes are the phenotypic consequences of frailty. Virtually all geriatric syndromes are characterized by changes in four domains: (1) alteration in body composition, (2) gaps in energy supply and demand, (3) signaling disequilibrium, and (4) neurodegeneration. Only dementia and falls will be discussed here.
The population of patients with dementia is growing. In 2020, the World Health Organization (WHO) reported dementia to affect an estimated 50 million people, 5% to 8% of the global population age 60 and over. They further project that this number will rise to 82 million in 2030 and 152 million in 2050. Thus a significant proportion of elderly perioperative patients are likely to have preexisting dementia. Intellectual decline is one of the early hallmarks of dementia. Major differences are seen in the elderly in terms of intellectual function compared to themselves in early adulthood. In any patient with a slowly progressive dementia, sudden changes in cognitive, behavioral, or health status may occur. Mental status is often a barometer of health in these patients, and abrupt changes necessitate a search for any additional problem that may be occurring ( Table 30.1 ). Numerous population-based studies report decreased longevity in elderly individuals who experience cognitive decline. In fact, the WHO listed dementia as the seventh leading cause of death worldwide and the third leading cause of death in both Europe and the United States in 2019. Diminishing cognitive performance over any time interval is predictive of an earlier death. In addition, preexisting dementia in the surgical patient is a strong predictor of postoperative complications and greater hospital costs and is an independent predictor of 30-day mortality. Perhaps the most important challenge in treating dementia is identifying causes of reversible dementia, such as chronic drug intoxication, vitamin deficiencies, subdural hematoma, major depression, normal-pressure hydrocephalus, and hypothyroidism.
| Diagnosis | Distinguishing Features | Symptoms | Course |
|---|---|---|---|
| Dementia | Memory impairment | Disorientation, agitation | Slow onset, progressive, chronic |
| Delirium | Fluctuating level of consciousness, decreased attention | Disorientation, visual hallucinations, agitation, apathy, withdrawal, memory and attention impairment | Acute; most cases remit with correction of underlying medical condition |
| Psychotic disorders | Deficit in reality testing | Social withdrawal, apathy | Slow onset with prodromal syndrome; chronic with exacerbations |
| Depression | Sadness, loss of interest and pleasure in usual activities | Disturbances of sleep, appetite, concentration; low energy; feelings of hopelessness and worthlessness; suicidal ideation | Single episode or recurrent episodes; may be chronic |
Unfortunately, most causes of dementia, including degenerative brain diseases such as Alzheimer disease and other common multi-infarct states, are incurable. This does not mean, however, that symptoms cannot be treated and ameliorated. Pharmacotherapy for dementia is tailored to control behavioral problems such as agitation, depression, and sleep disorders that may be present and to prevent further intellectual decline and neurodegeneration. These treatments may include vitamin E, N-methyl-D-aspartate (NMDA) antagonists, selective serotonin reuptake inhibitors (SSRIs), melatonin, and centrally acting acetylcholinesterase inhibitors.
For the anesthesiologist the challenges in caring for elderly patients with declining mental capacity are many. Perioperative interactions with the patient and family must take into account the patient’s compromised ability to process general and medical information and capability to provide truly informed consent. Care for individuals with dementia typically requires multidisciplinary collaboration, including family and caregivers with written identification of healthcare power of attorney and advanced directives preoperatively. Documentation of baseline cognitive and neurologic function may become significant if postoperative alterations in mental function are encountered. If acute deterioration is suspected, a neurologic consultation is advised. While more research is needed to elucidate the best perioperative care for elderly patients with dementia, perioperative care should focus on evaluating and managing delirium, treating postoperative pain, and minimizing sleep disturbances.
Unstable gait and falls are a serious concern in older patients. Problems with balance and falls tend to be multifactorial. Poor muscle strength, neural damage in the basal ganglia and cerebellum, and peripheral neuropathy are all recognized risk factors for falls. The American Geriatric Society recommends asking all older adults about falls and gait instability. Patients with a history of multiple falls should undergo an evaluation of gait and balance to determine the precipitating factors.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here