Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Radiographs form the cornerstone of diagnostic imaging of the hand and wrist, and are usually the first imaging modalities performed following clinical evaluation.
The keys to obtaining the most information from radiographs are ordering the correct radiographs for the situation, and ensuring the radiograph is appropriately taken.
A systematic and careful examination of the radiograph is necessary to glean the often subtle findings in the hand and wrist.
Clinical evaluation with plain radiographs often provides sufficient information for clinical decision-making.
Computed tomography (CT) scans, ultrasound, magnetic resonance imaging (MRI), and other advanced imaging modalities can supplement information from plain radiographs in selected situations. On occasion, they may be the primary imaging study performed.
These advanced imaging modalities allow today's clinician to visualize disorders that would previously have required open surgery or biopsy.
![]() Access video content for this chapter online at Elsevier eBooks+
Access video content for this chapter online at Elsevier eBooks+
A proper and directed history-taking followed by a careful examination of both hands and wrists forms the foundation of making a clinical differential diagnosis in hand conditions.
Appropriate investigations are then ordered to help confirm the clinical diagnosis.
Diagnostic imaging modalities are often the first-line investigations ordered, as many clinical conditions in the hand and wrist can be seen visually.
Technological advances in many advanced imaging modalities like ultrasound, computed tomography (CT), and magnetic resonance imaging (MRI), have led to them being applied for use in the hand and wrist. This increases clinician choices for diagnostic imaging of a suspected clinical condition.
The radiograph, despite its simplicity and age, still forms the foundation of imaging of hand and wrist conditions. In many clinical situations, an appropriately chosen and well-taken set of radiographs may be all the diagnostic imaging required.
The key to obtaining the most information from a radiograph is to understand which radiographs are appropriate for each clinical situation, and how to obtain good-quality radiographs for evaluation.
Advanced imaging modalities may then be ordered to provide additional information for decision-making.
This chapter will equip the reader with practical information about the different imaging modalities available for the hand and wrist.
It will start from the foundation of radiographs, covering the appropriate views, how they are taken, and how best to evaluate them. Following which, the advanced imaging techniques will be described in turn, emphasizing their applications in the hand and wrist.
Radiography is the cornerstone in diagnostic imaging of the hand and wrist. It should be the first imaging modality for the diagnosis of most hand and wrist disorders. The plain radiograph is inexpensive in relation to other imaging modalities, technically easy to perform, and widely available. The correct radiograph taken in an appropriate manner provides much imaging information to the attending clinician. In many hand and wrist conditions, radiography may also be the only imaging modality required for definitive diagnosis and assessment.
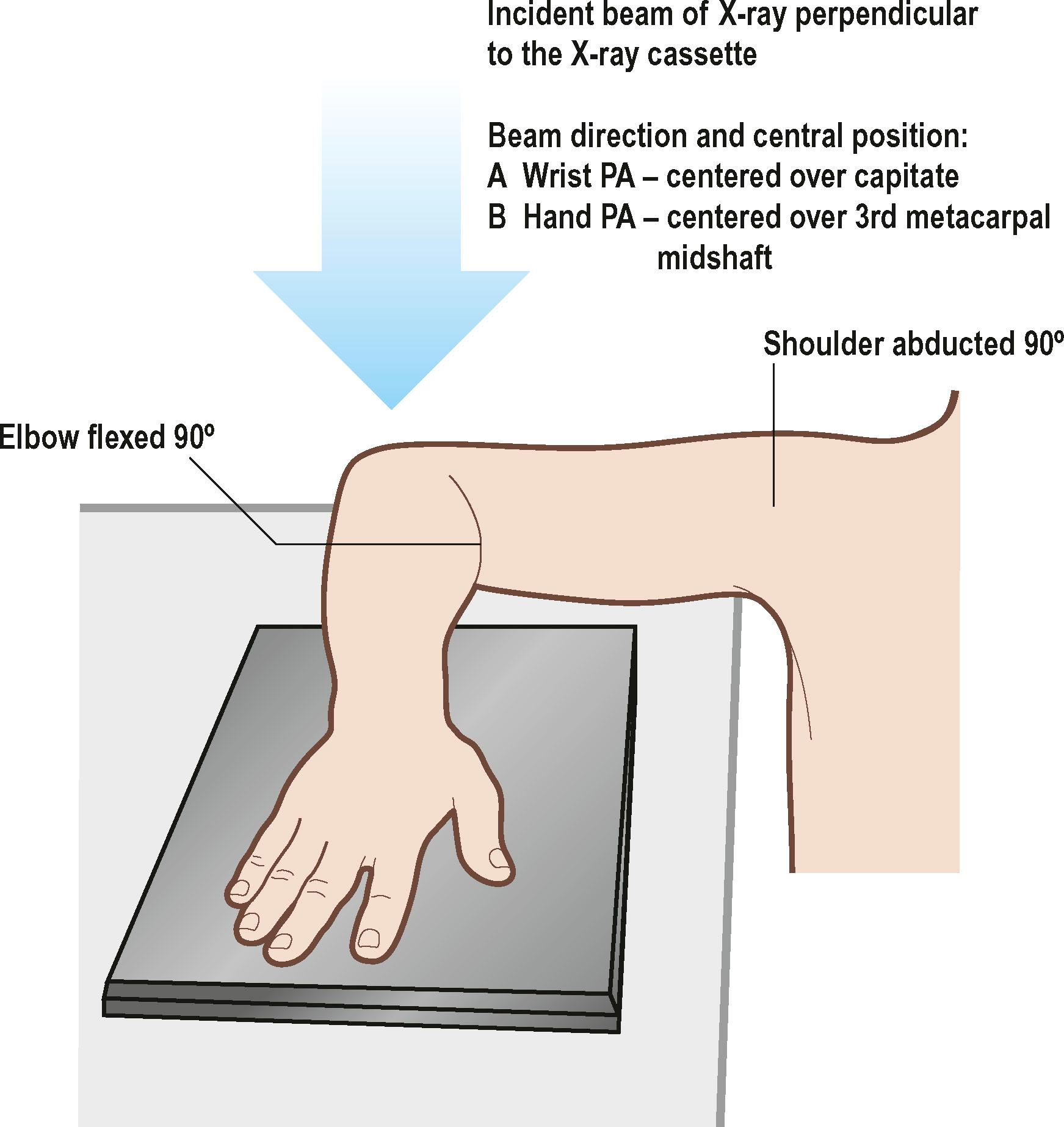
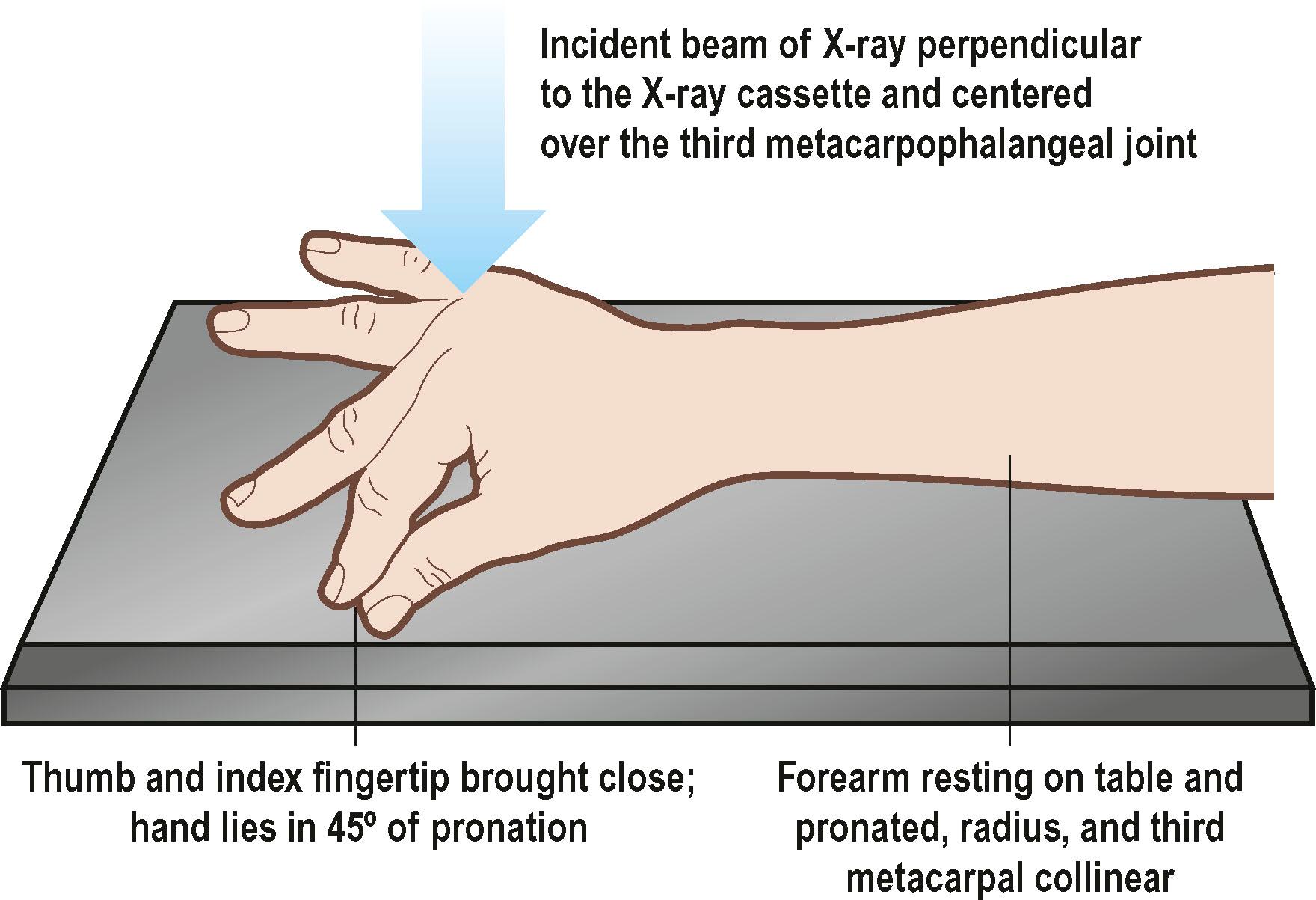
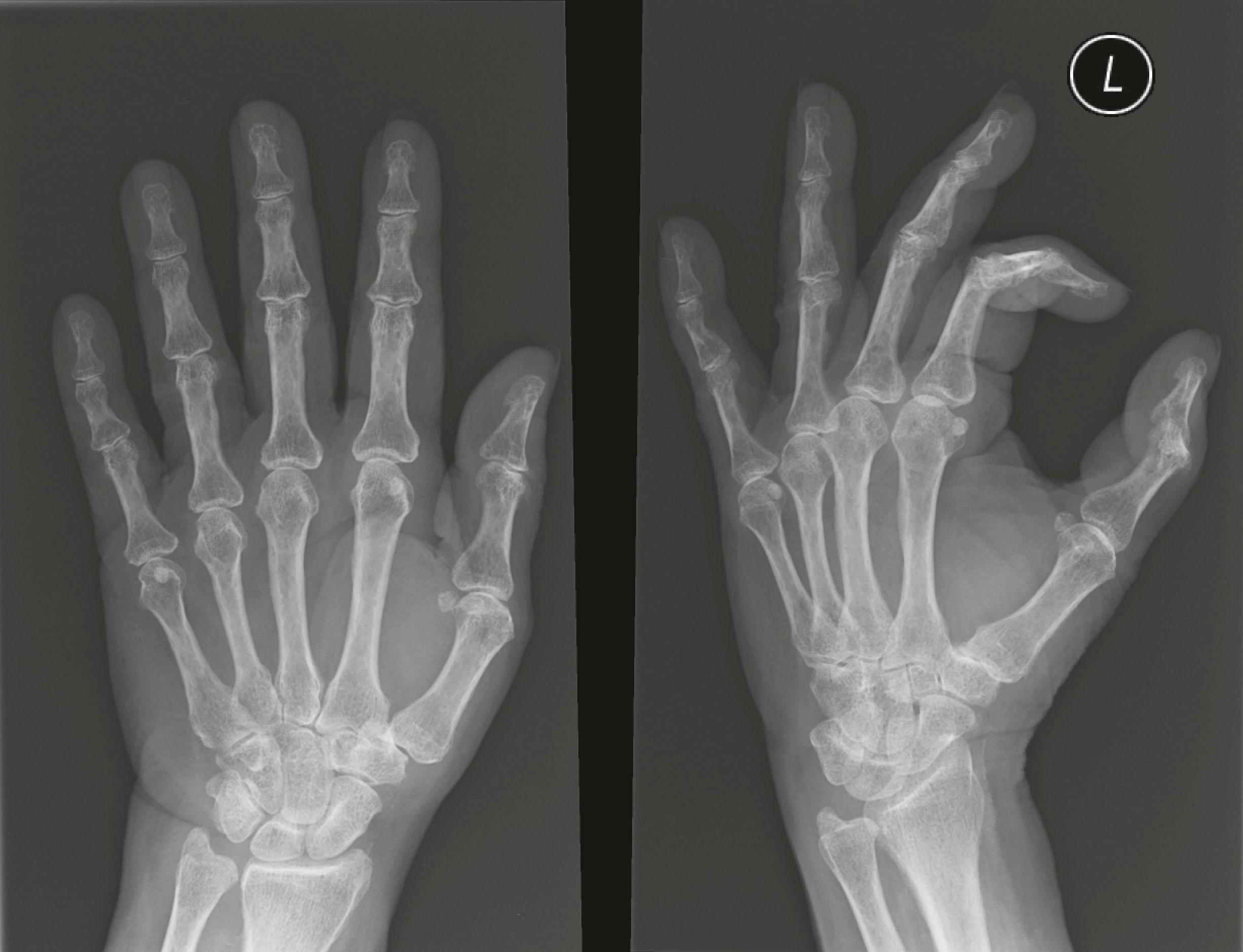
The three basic radiographs to evaluate the hand are: posteroanterior (PA), oblique, and true lateral views. The radiographs should be performed in a standardized fashion to allow proper evaluation ( Figs. 3.1 & 3.2 ). Specialized views are required to assess specific areas not well seen in the above views. The PA hand view provides a useful overview of the skeletal structure of the hand. Fractures, osseous tumors, and even soft-tissue masses ( Fig. 3.3 ) can be seen on this view. The oblique view of the hand is useful to assess the metacarpals, as a true lateral view of the hand will lead to an overlapping of the second to fifth metacarpals. In the common boxer's or fifth metacarpal neck fracture, this view allows an assessment of the amount of angulation of the fracture.

In hand radiographs, begin by assessing the overall alignment of the metacarpals and phalanges. The individual bones should then be evaluated in terms of cortical shape and integrity, as well as bony quality. Fractures are usually easy to detect, although a careful review is necessary in the case of undisplaced or minimally displaced fractures. Osseous tumors are identified by an area of different lucency in the bone. There may be changes in the outline of the bone. Enchondromas are common benign bony tumors in the hand. They can result in pathological fractures, so an assessment of the bone for such pathology should be done, particularly if the trauma resulting in the injury is trivial ( Fig. 3.4 ). Osteomyelitis typically occurs in the hand following open injuries ( Fig. 3.5 ).


The joints should then be assessed, starting from the carpometacarpal joints (CMCJs) and working distally. The CMCJs may be dislocated following injury. These injuries are uncommon but are difficult to diagnose. In a normal hand X-ray the second to fifth CMCJs should be clearly visible on the PA view ( Fig. 3.6 ). The loss of these features in the second to fifth CMCJs is usually due to a fracture dislocation of one or more of the CMCJs. However, an improperly performed hand radiograph can also give this impression. Fisher et al . described a systematic approach to evaluating the PA view of the hand for dislocations of the fourth and fifth CMCJs. In subluxation of the fifth CMCJ, the base of the fifth metacarpal is usually offset ulnarly compared to the hamate ( Fig. 3.7 ). Several views have been suggested to confirm this diagnosis. The true lateral of the hand provides a useful way to assess the CMCJ for any signs of dislocation and oblique views may also be helpful ; if the diagnosis is still uncertain, a CT scan of the hand including the CMCJs will confirm the diagnosis. The more distal joints are then evaluated, from the metacarpophalangeal joints to the proximal interphalangeal joints and distal interphalangeal joints. A normal joint should be completely congruent with a visible joint space.


Osteoarthritis commonly affects the interphalangeal joints and thumb CMCJs. It is often demonstrable on radiographs by narrowing of the joint space, subchondral sclerosis, osteophytes, and deformity ( Fig. 3.8 ).

The origins of diagnostic radiology are of particular significance to hand surgery. The first radiograph of human anatomy after the discovery of X-rays by Wilhelm Conrad Roentgen was that of his wife's hand in 1895. The medical community was quick to see the potential applications of this technology, and radiographs were rapidly adopted for clinical use. As a result, Roentgen is considered the father of diagnostic radiology, and his discovery led him to win the first Nobel Prize in Physics in 1901.
Plain X-ray radiographs are still the first-line imaging modality for the diagnosis of most hand and wrist disorders. Plain film radiography has progressed from a tedious process using an acetate-based film to one that applies digital technology. In newer facilities, widespread adoption of digital technology has led to radiographs that are not printed on film, but viewed on the computer screen. Beyond technology, the development of special views through positioning of the patient or machine, and stress application, has enabled improvements in imaging of specific disorders. The development of water-soluble contrast dyes allowed the use of X-rays to perform arthrography.
CT, MRI, and ultrasound are advanced imaging technologies that have become widely adopted for musculoskeletal imaging, including the hand and wrist. Improvements in hardware technology, software, and imaging protocols have resulted in improved imaging of bone, joints, and soft tissue. These technologies have enabled detailed visualization and assessment of the musculoskeletal system and its disorders in a noninvasive manner. Prior to these technologies, many of these disorders would have required open surgery or biopsy for diagnosis.
Improvements in imaging modalities and technology are only part of the equation for the advances made in musculoskeletal imaging. Equally important has been the parallel development of musculoskeletal radiology as a distinct subspecialty. The dedication of musculoskeletal radiologists has been instrumental in developing their field, and subspecialty training of future musculoskeletal radiologists. These radiologists can better appreciate the often subtle findings on imaging, leading to improved diagnosis. This has translated to earlier and more effective clinical care and improved outcomes.
Musculoskeletal radiology continues to progress at a rapid pace as both a clinical specialty and in technological advances. Building on its strong foundations, musculoskeletal imaging will continue to be a crucial pillar in the diagnosis and assessment of hand and wrist disorders.
( Box 3.1 )A true lateral radiograph of the finger is needed to complete an assessment of the digit. Hand radiographs alone are insufficient for assessment. This is because the oblique view of the hand does not provide an adequate lateral profile of the digit and interphalangeal joint spaces to supplement the PA view. With only a PA view, subtle fractures, fracture displacement, or joint subluxation of the fingers may not be apparent. Metacarpal head fractures may also be difficult to assess and the Brewerton view will give additional information to the standard hand radiographs.
Purpose : To obtain tangential views of the metacarpal heads – for evaluation of metacarpal head fractures and erosive changes in rheumatoid arthritis
Positioning : With the palm facing up, the MCPJs are flexed 65° with the posterior aspect of the fingers in contact with the cassette, and beam angled at 15° from the ulnar side of the hand
Purpose : To obtain a true lateral view of the TMCJ, and see the trapezium in profile
Positioning : Palm of the hand must be placed flat on the cassette with the hand and forearm pronated, with the beam is then directed 5–10° distal to proximal
Purpose : To obtain a true AP view of the TMCJ
Positioning : The hand and forearm is hyperpronated such that the dorsum of the thumb lies on the cassette, with the beam angled 15° from the vertical
To assess the thumb, specialized views are also necessary as the thumb lies in an oblique plane relative to the other digits in the usual hand radiograph. A true PA and lateral view of the thumb is obtained to allow proper radiographic assessment of the thumb. One common condition in the thumb for which radiographs are performed is that of basal joint or trapeziometacarpal joint (TMCJ) arthritis ( Fig. 3.9 ). This condition is graded radiologically using the Eaton classification. The irregular saddle shape of the trapezium makes visualization of the bone difficult, and the Betts view will allow all four articulations of the trapezium to be visible without overlap ( Fig. 3.10 ).

The ulnar collateral ligament of the thumb metacarpophalangeal joint is commonly injured in forceful thumb abduction. Less commonly the radial collateral ligament may also be injured. Lateral stress application during the posteroanterior thumb radiograph can be helpful to assess if the ligament injuries are complete or partial. Ultrasonography and MRI are alternatives to assess this injury.
Evaluation of the pediatric hand, especially after injury, is often more difficult than in adults. All carpal bones and epiphyses in the hand lack ossification in the newborn. The ossification centers then appear in a well-recognized sequence, as detailed in Table 3.1 . The staggered ossification of the various carpal bones ( Fig. 3.11 ) and the presence of the growth plate may confuse the examiner as to whether a fracture is present or not.
| Females | Males | |
|---|---|---|
| Appearance of capitate and hamate | 3 months | 3 months |
| Appearance of distal radius ossification center | 10 months | 1 year 3 months |
| Appearance of phalanges and metacarpal ossification center | 10 months to 2 years | 14 months to 3 years |
| Fusion of phalangeal and metacarpal epiphyses | 13–15 years | 14–16 years |
| Fusion of distal radius and ulna epiphyses | 15–17 years | 17–19 years |
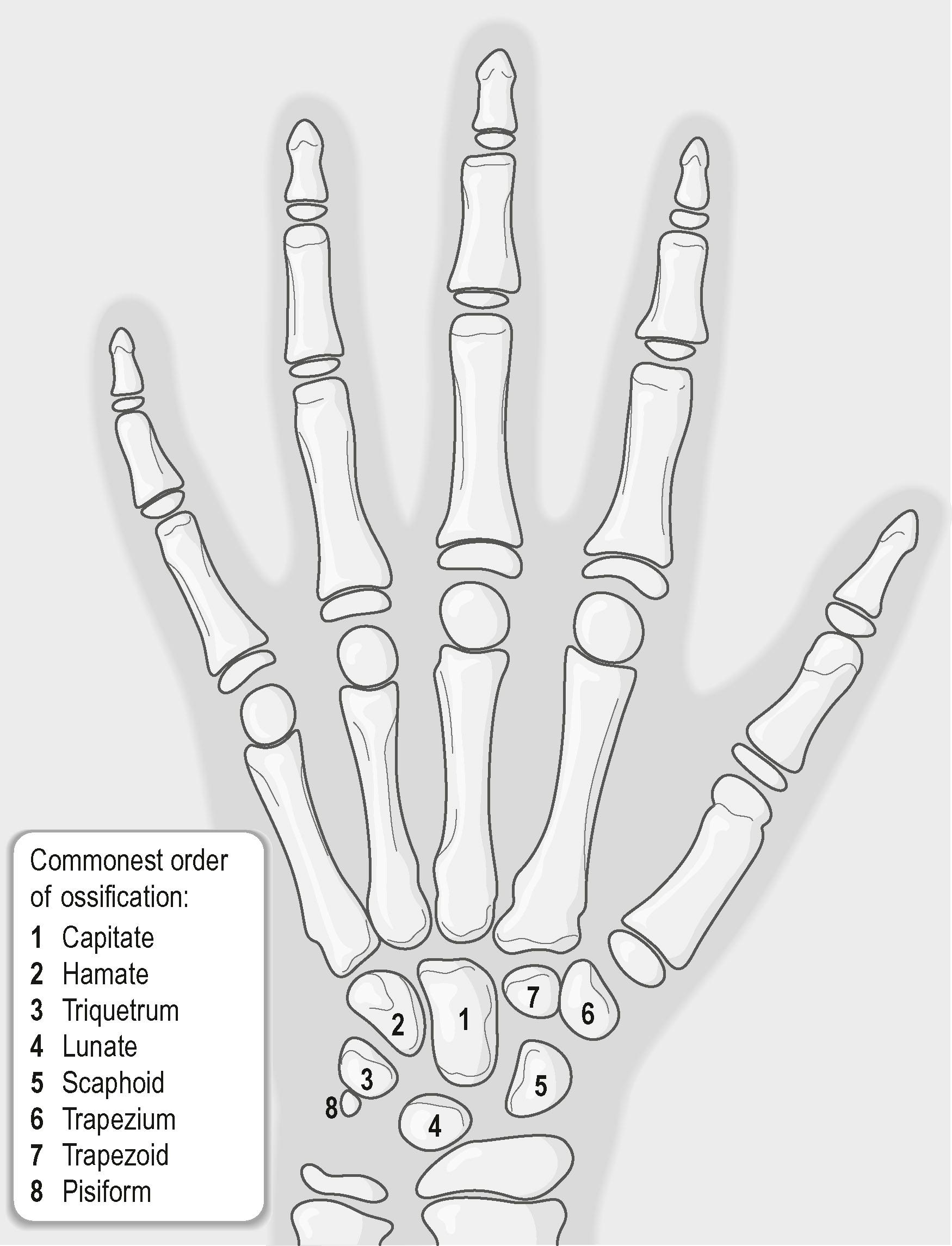
A misdiagnosis rate of 8% for pediatric hand fractures was found in one study. There are several reasons for this. Clinical evaluation in children is more difficult, the more so the younger the child. It may not be possible to localize the site of the problem clearly, e.g., the site of injury following trauma. Proper standardized views may also be difficult to obtain. Other reasons for misdiagnosis include missing additional fractures and using an X-ray that was obscured by dressings. When the clinical suspicion remains high and the films obtained are inadequate, the radiograph should be repeated, either the same day or at another time when the patient is more cooperative. Similar views taken of the opposite uninjured limb are also helpful for evaluation.
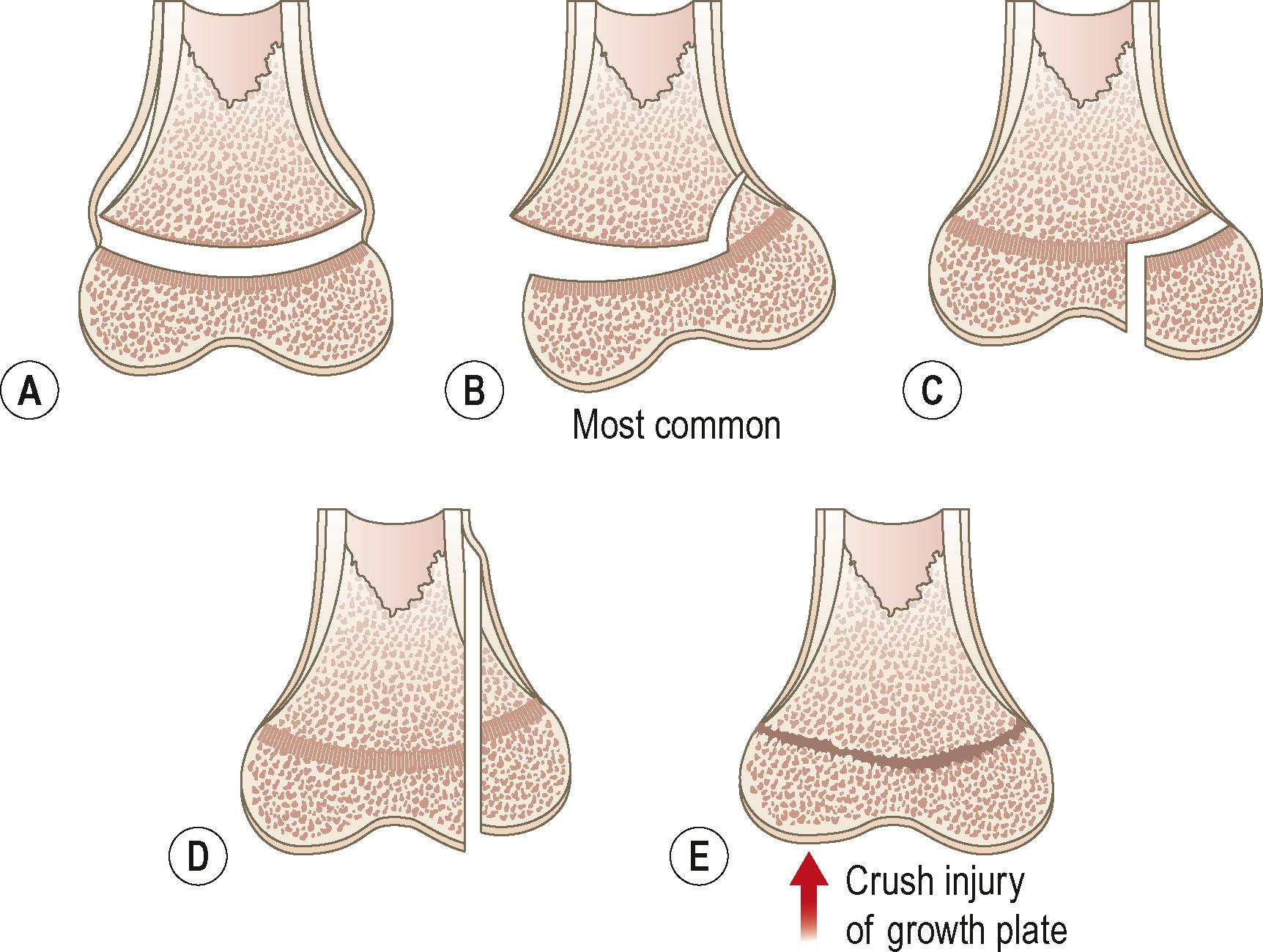
Growth plate-related injuries are common in children. These injuries can be classified according to the system described by Salter and Harris ( Fig. 3.12 ). The Salter–Harris type II fracture injury is the most common type of growth plate injury seen in the hand.
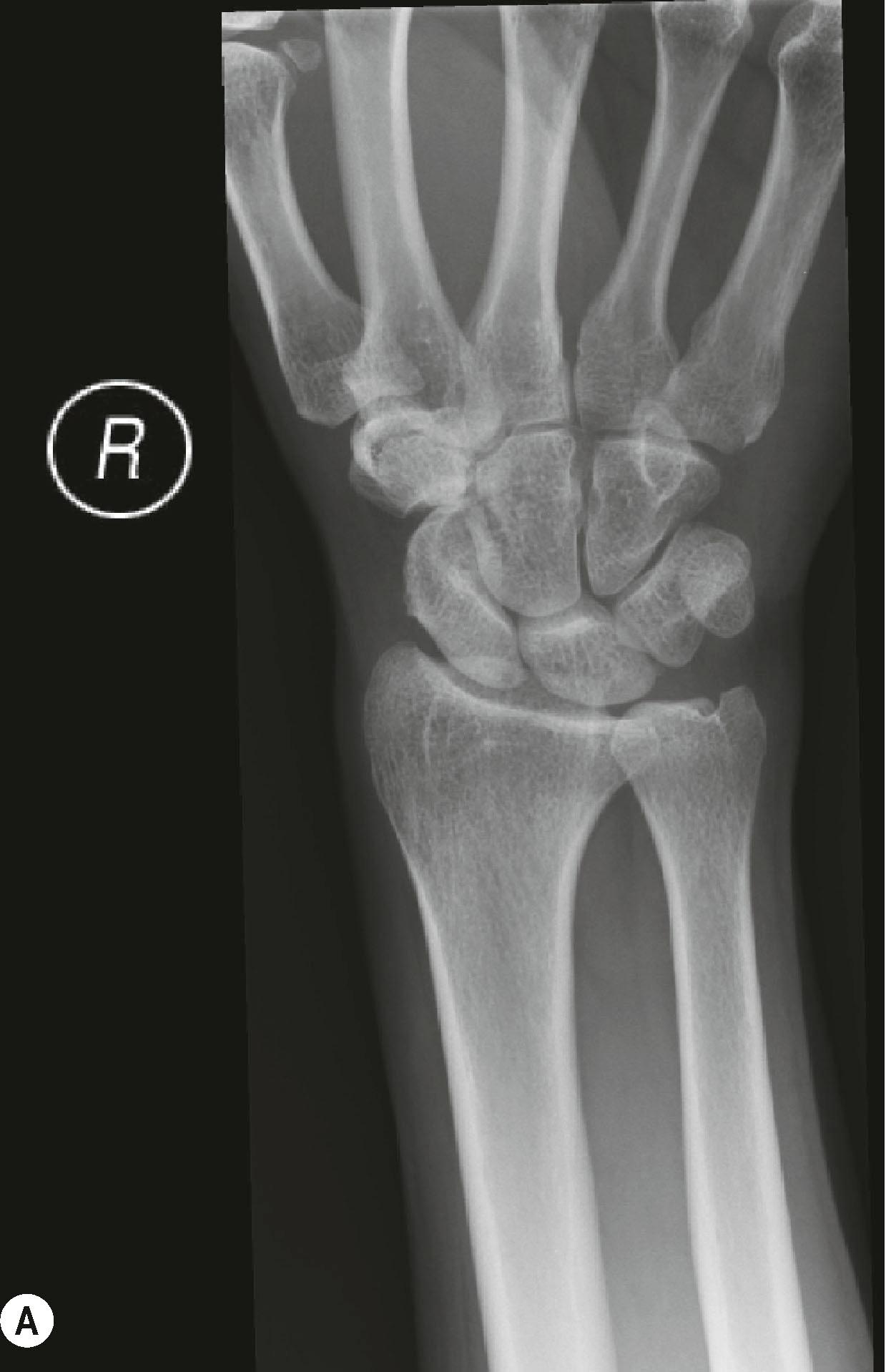
A properly performed set of orthogonal wrist radiographs forms the basis of an effective evaluation of the wrist. This is especially important when indices are being measured. The wrist has numerous asymmetrically arranged bones, so a methodical assessment of the bones, joints, and overall alignment of the wrist is necessary.
Obtaining proper views for wrist radiographs (see Fig. 3.1 ; Fig. 3.13 ; see Fig. 3.18 ) requires careful positioning which may be difficult to achieve in patients with pain or limitations in motion of the affected upper limb ( Box 3.2 ).
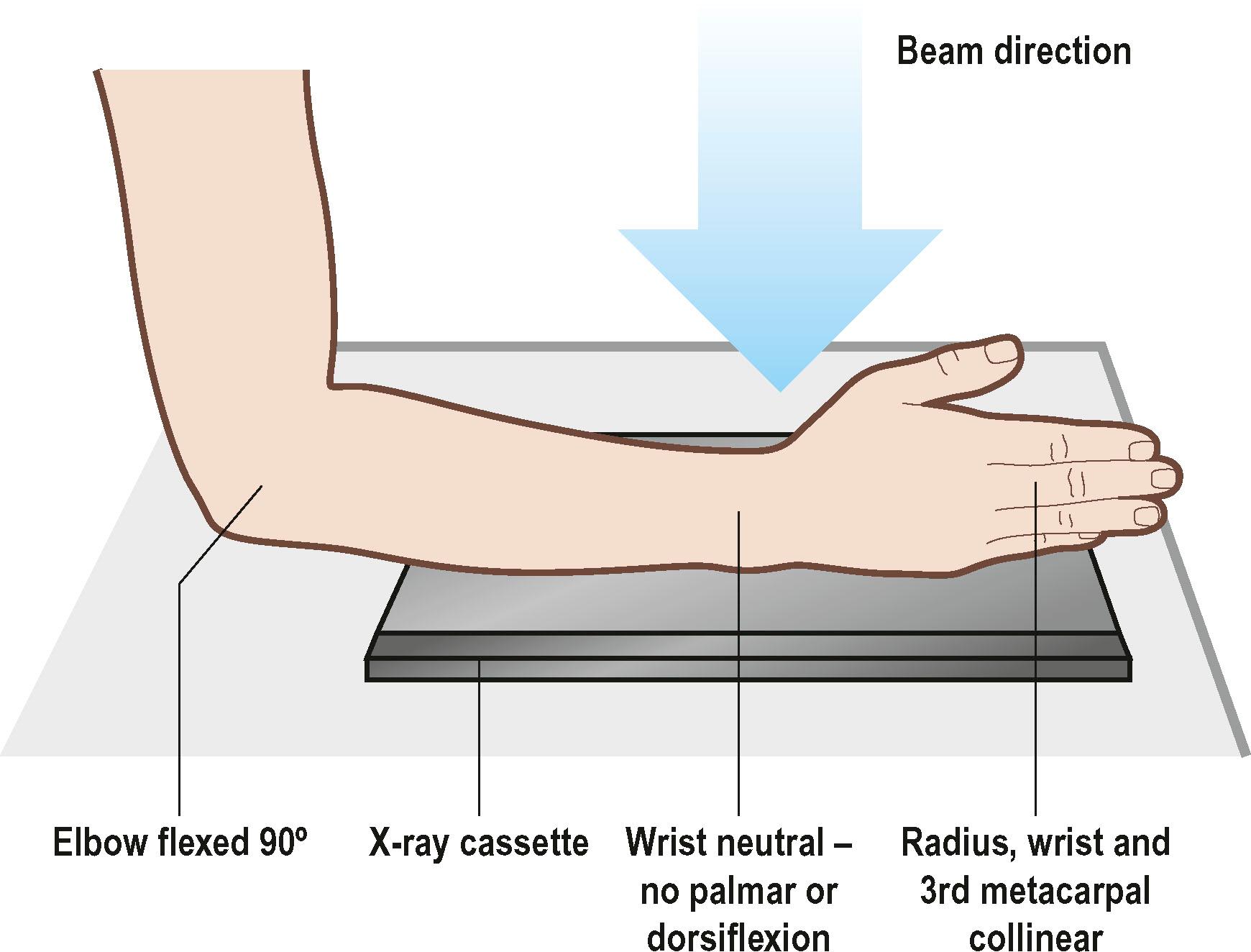
There are criteria for acceptable wrist views. The posteranterior (PA) view is assessed using the position of the ulnar styloid and extensor carpi ulnaris tendon groove. The lateral view is assessed using the radioulnar overlap and scaphopisocapitate relationships.
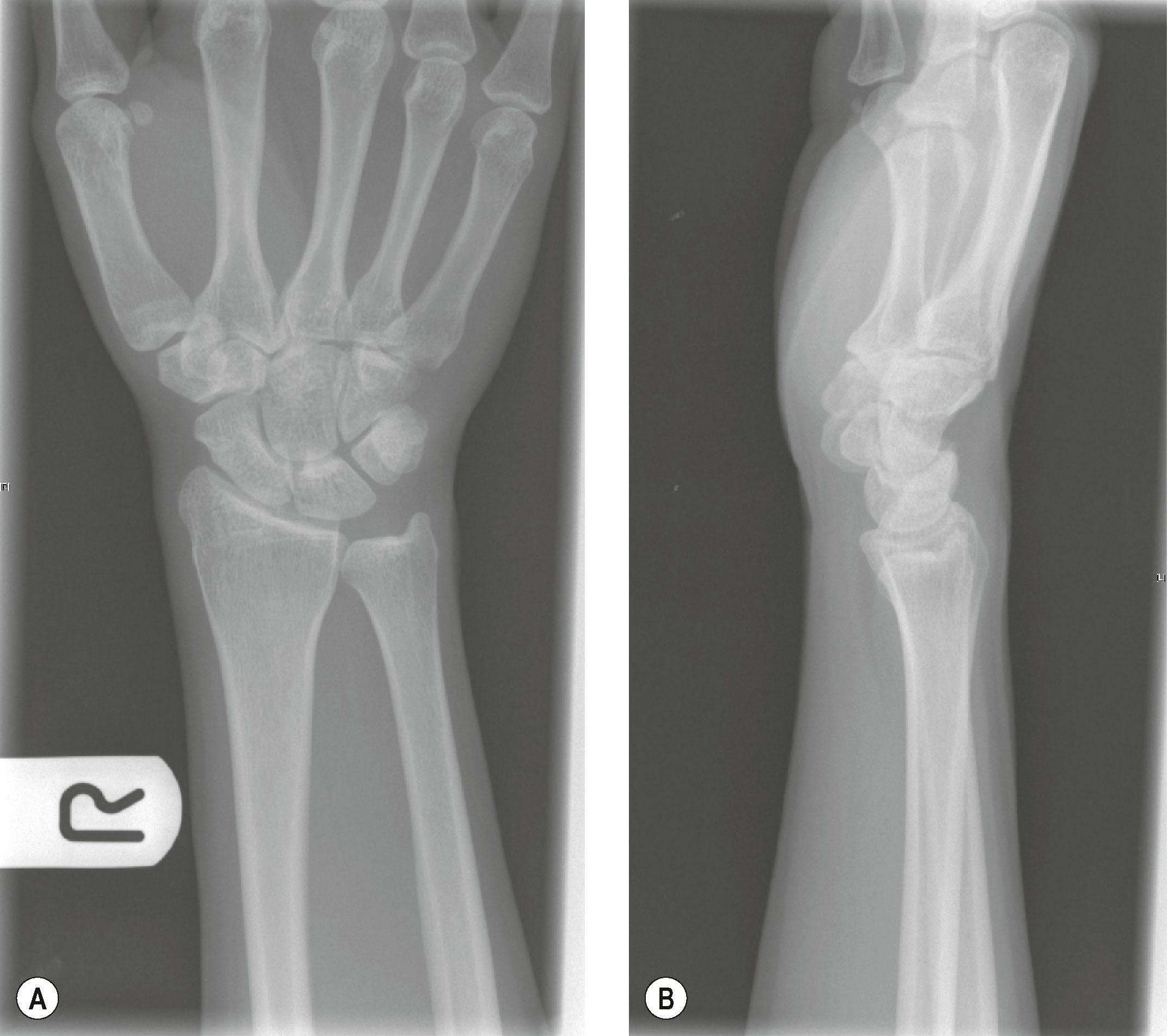
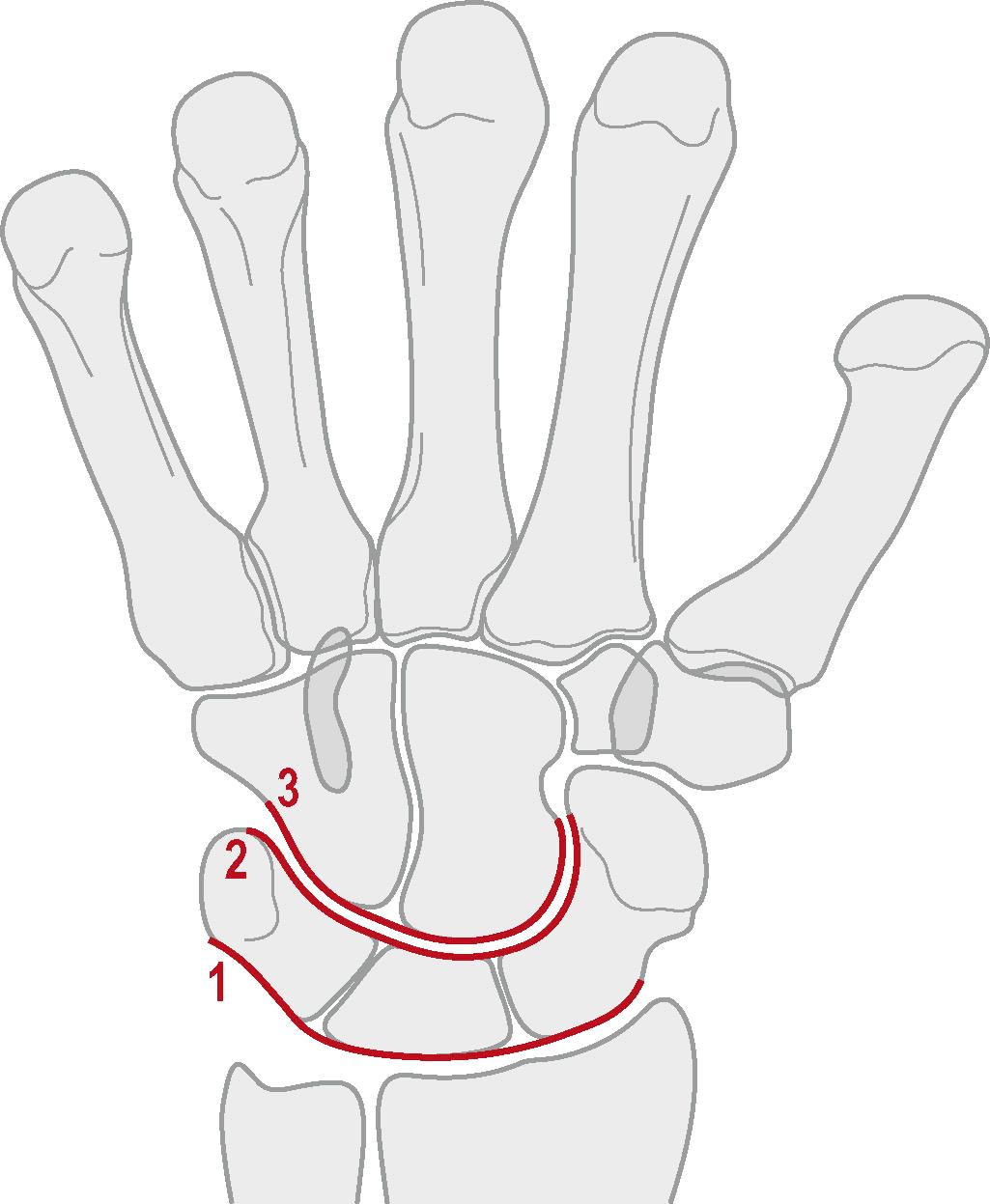
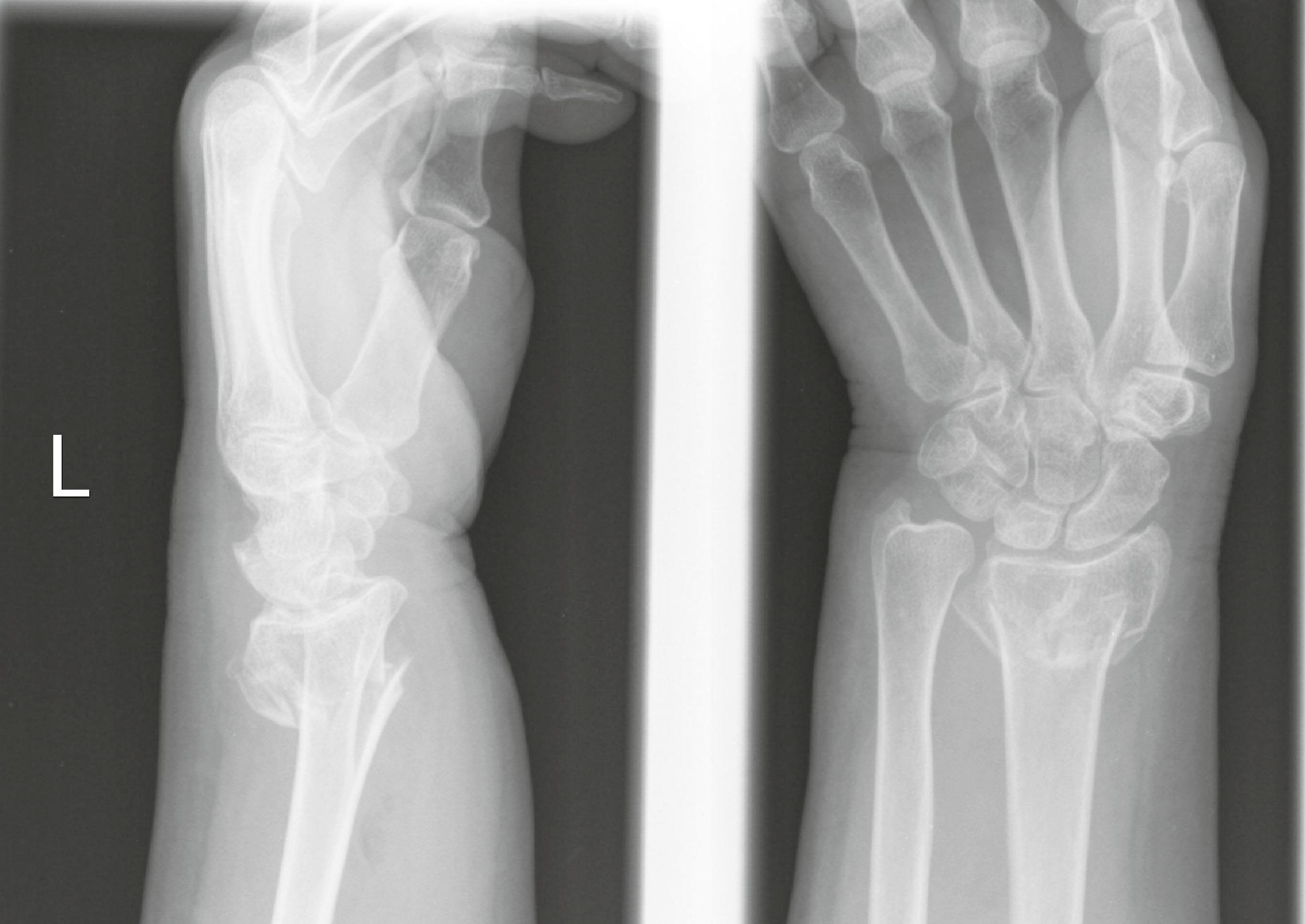
The wrist radiograph is first evaluated by checking the overall alignment of the bones of the wrist, starting with the distal radius and ulna, progressing to the carpal bones and metacarpal bases. Gilula described three smooth arcs made by the articular surfaces of the proximal and distal carpal row bones in a normal wrist PA radiograph ( Fig. 3.14 ). A loss of the normal contour usually indicates a disruption in the normal arrangement of these carpal bones. A common cause of this is a perilunate dislocation ( Fig. 3.15 ). Lunotriquetral (LT) dissociation is another cause of the loss of the normal Gilula's lines. Care must be taken when interpreting these findings in an asymptomatic patient as radial or ulnar deviation of the wrist can introduce a break in the arcs.

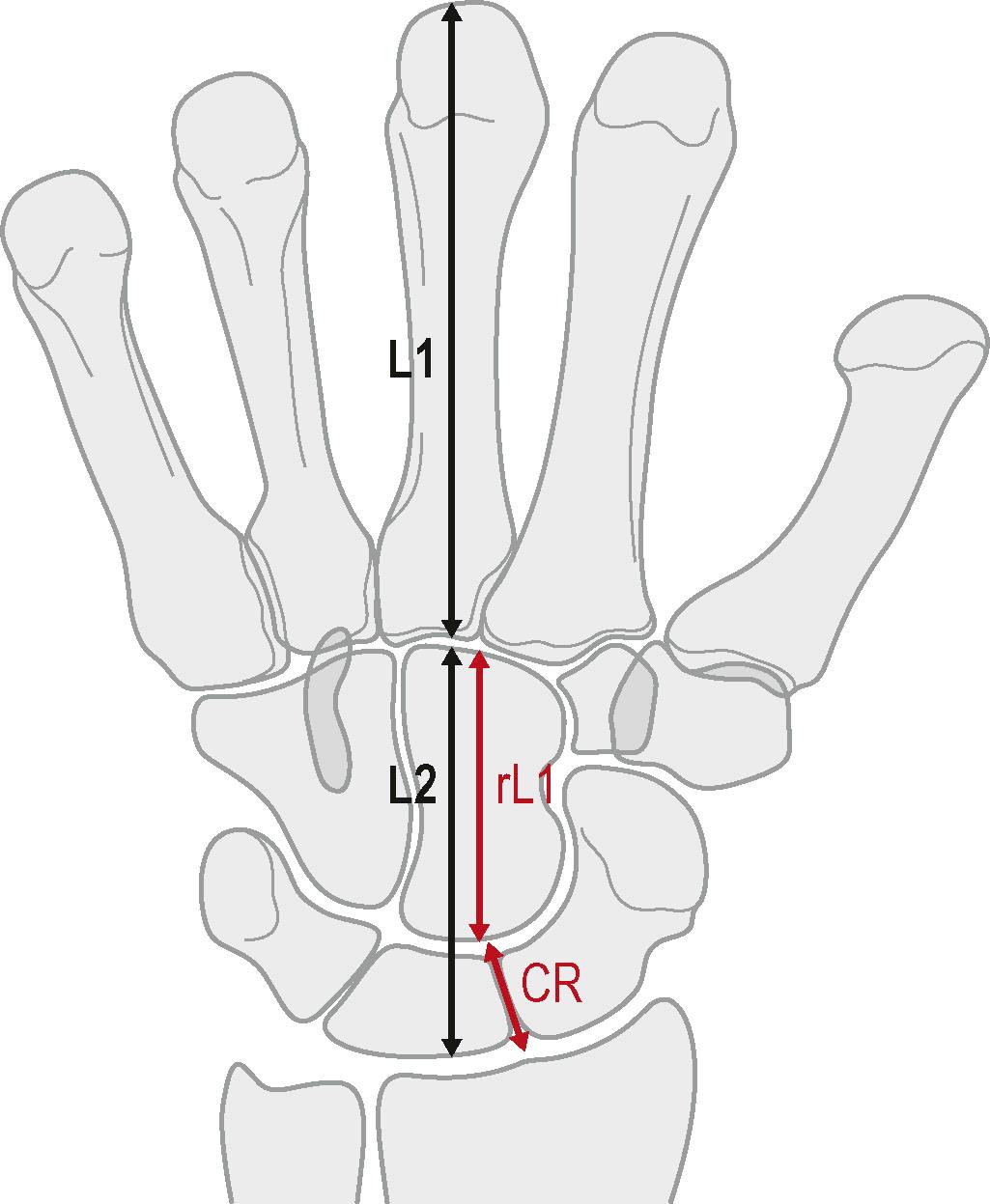
The overall relationship between the different bones can also be assessed using two common parameters: the carpal height ratio and ulnar variance. These provide a quantitative assessment of the structural integrity of the carpal rows, and the relationship of the distal radius and ulna articular surfaces, respectively.
The carpal height ratio ( Fig. 3.16 ) gives a measure of the distance between the distal articular surface of the radius to the proximal articular surface of the third metacarpal base. A loss of this distance is seen in collapse of a carpal bone, for example Kienbock's disease (avascular necrosis [AVN] of the lunate) or in malrotation of the carpal bones, for example in rheumatoid arthritis or scapholunate (SL) dissociation. A ratio is used instead of actual dimensions to correct for variability in carpal bone sizes.
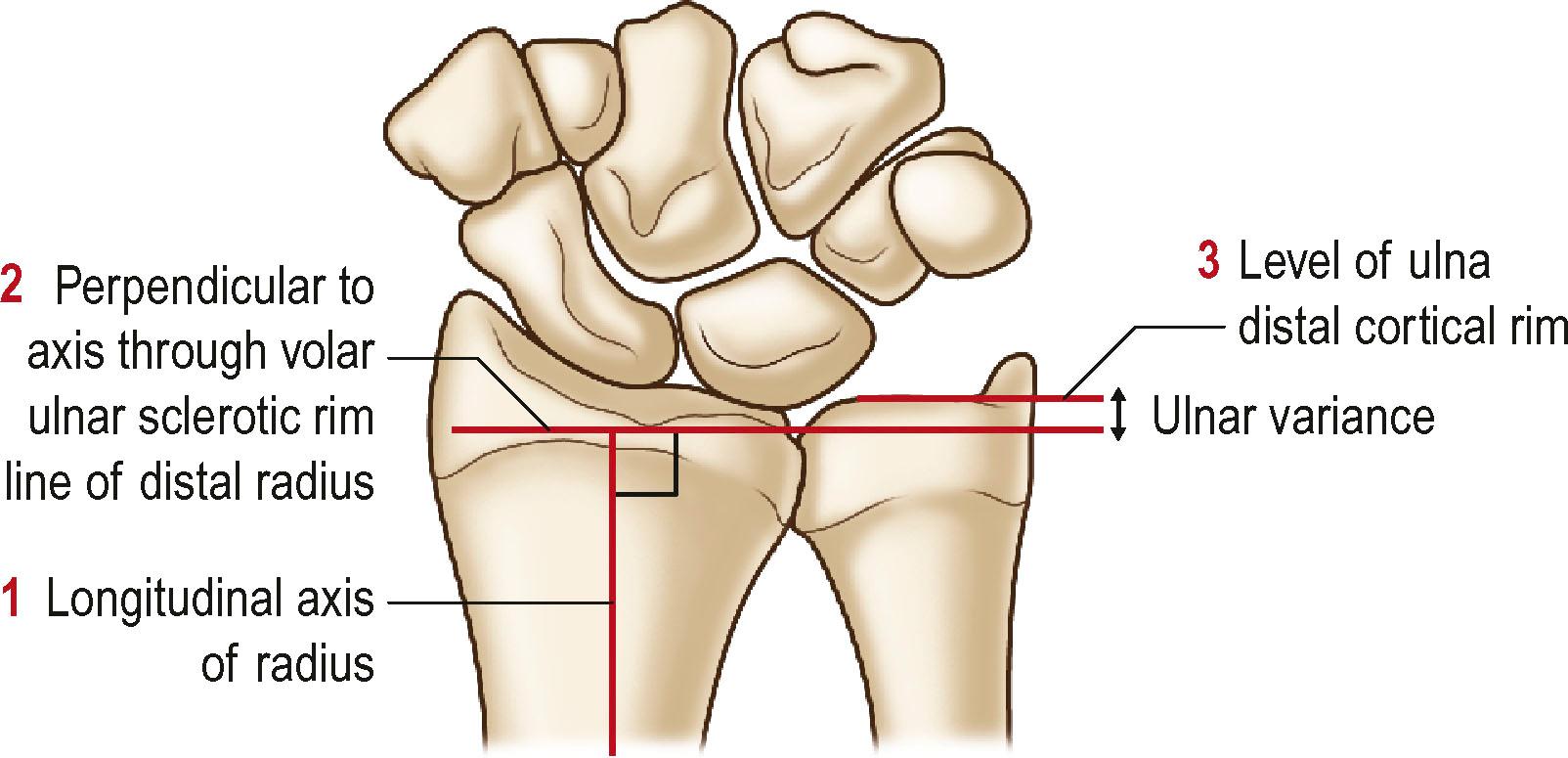
The ulnar variance provides a measure of the height difference between distal radius and ulnar articular surfaces. There are several ways to measure the ulnar variance. We prefer the technique of the perpendiculars ( Fig. 3.17 ). It is easy to perform and has been shown to have higher intra- and interobserver reliability.
A proper PA and lateral radiograph of the wrist ( Fig. 3.18 ; see Fig. 3.13 ) is the first necessary imaging for the evaluation of a suspected distal radioulnar joint (DRUJ) instability. Radiographic findings associated with this injury include widening of the DRUJ, a fracture of the ulnar styloid base, or a displaced fracture from the ulnar fovea. On the lateral view, there is loss of the normal radioulnar overlap. A comparison radiograph of the contralateral normal wrist is helpful if the findings are unclear. The application of volar or dorsal-directed stress is also helpful in cases of suspected DRUJ instability ( Fig. 3.19 ).

Scaphoid fractures are the commonest carpal fracture. The shape of the scaphoid bone does not lend itself well to evaluation by just two orthogonal views, so a “scaphoid series” of X-rays is usually done ( Fig. 3.20 and Box 3.3 ).

The scaphoid view of the wrist addresses the normal foreshortening of the scaphoid seen on the conventional posteroanterior (PA) wrist radiograph. The view is taken with the wrist ulnarly deviated and the X-ray tube angled 20–30°. Several other views are helpful for assessment of the scaphoid: a pronated oblique view (to view the distal third and tubercle of the scaphoid better), a supinated view (to assess the dorsoradial ridge of scaphoid and pisiotriquetral articulation), and a lateral view to help assess a humpback deformity.
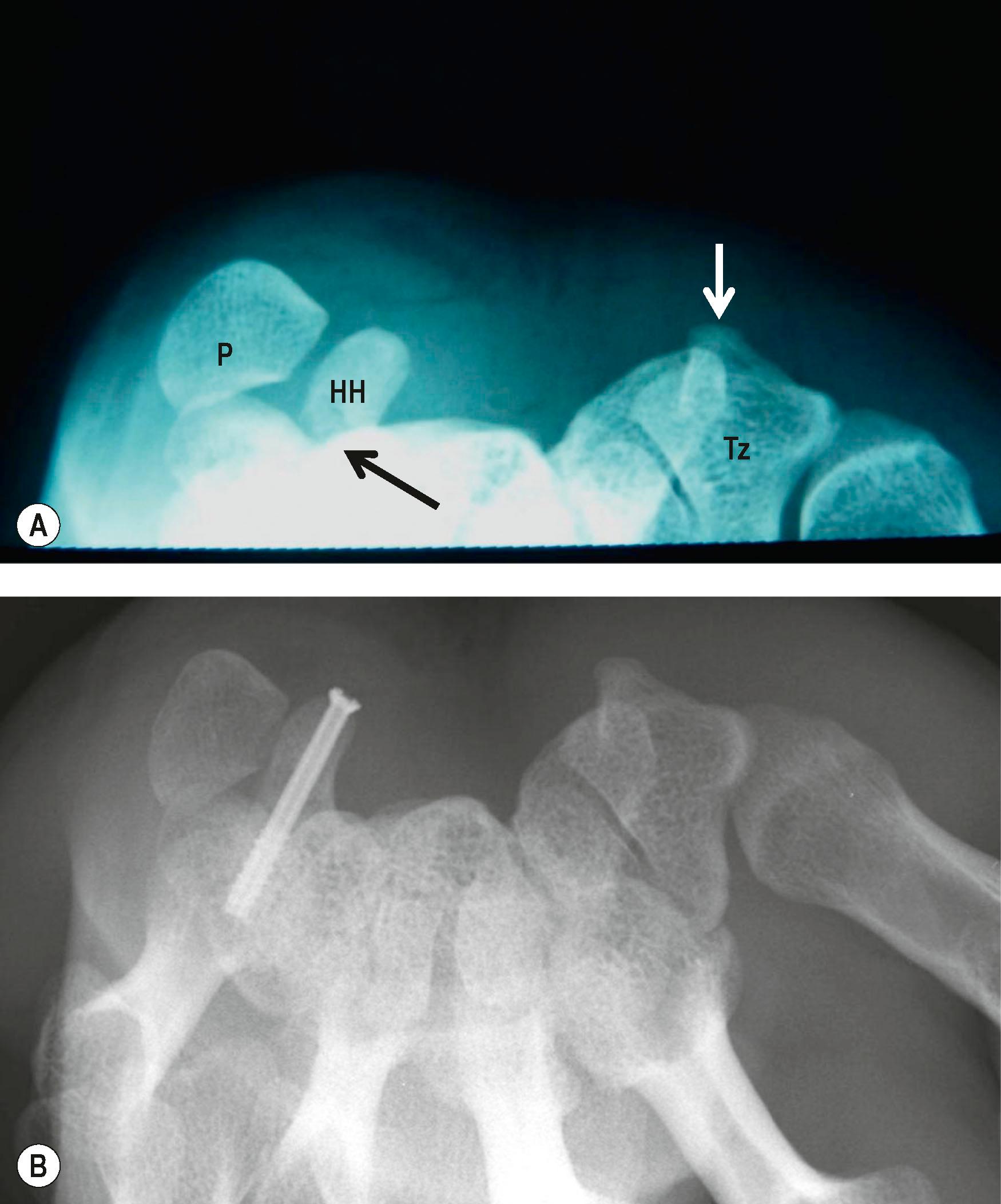
Fractures of the hook of the hamate are uncommon but disabling. A carpal tunnel view is helpful to diagnose this injury ( Fig. 3.21 ), although a CT scan can also provide the definitive diagnosis.
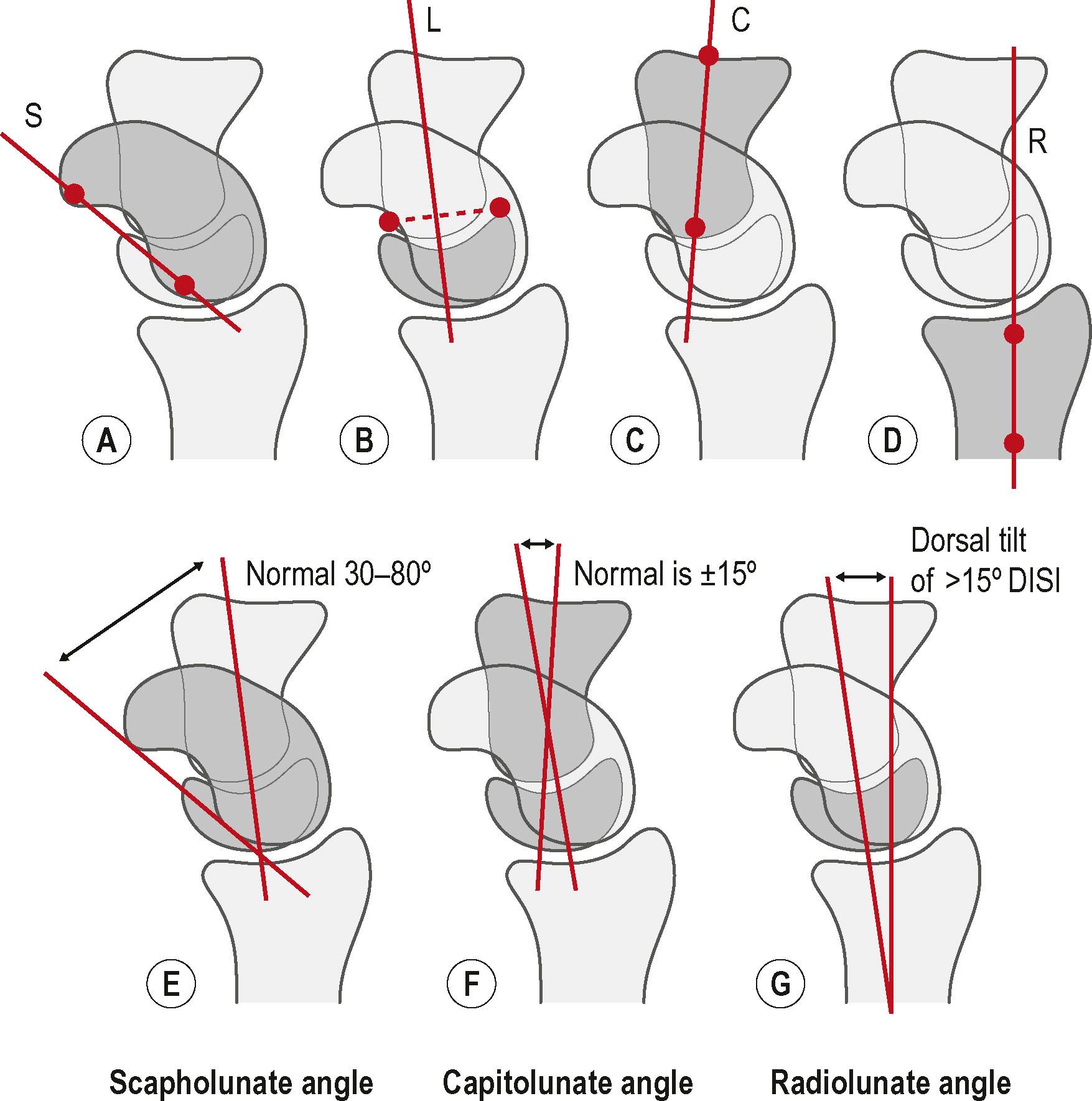
Injuries to the wrist ligaments, for example the SL ligament, can lead to carpal instability. In severe cases, this can be seen on the usual wrist views as loss of the normal relationships between the carpal bones. In SL instability, this is typically seen as a dorsal intercalated segmental instability deformity ( Fig. 3.22 ) with an increase in the SL angle, and dorsal tilt in the radiolunate angles ( Fig. 3.23 ). However, in milder forms of instability, application of loads and/or positioning of the wrist are necessary to bring out these dynamic changes in carpal relationships. The clenched-fist PA series of the wrist is one technique used to diagnose dynamic carpal instability ( Fig. 3.24 ).

Ulnar abutment syndrome is a common cause of ulnar-sided wrist pain. The use of a clenched-fist pronated view of the wrist enhances the ulnar variance and may demonstrate the abutment ( Fig. 3.25 ).

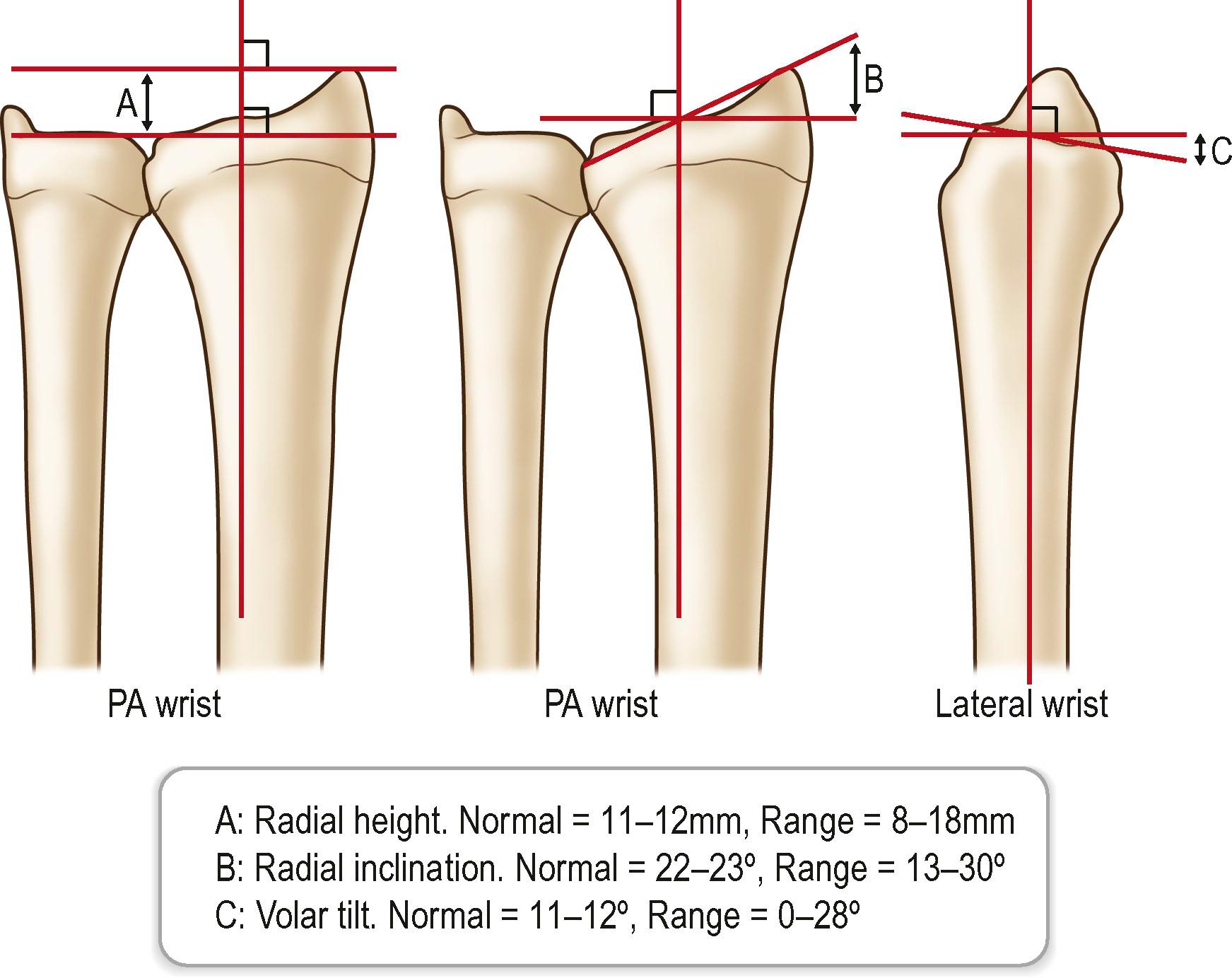
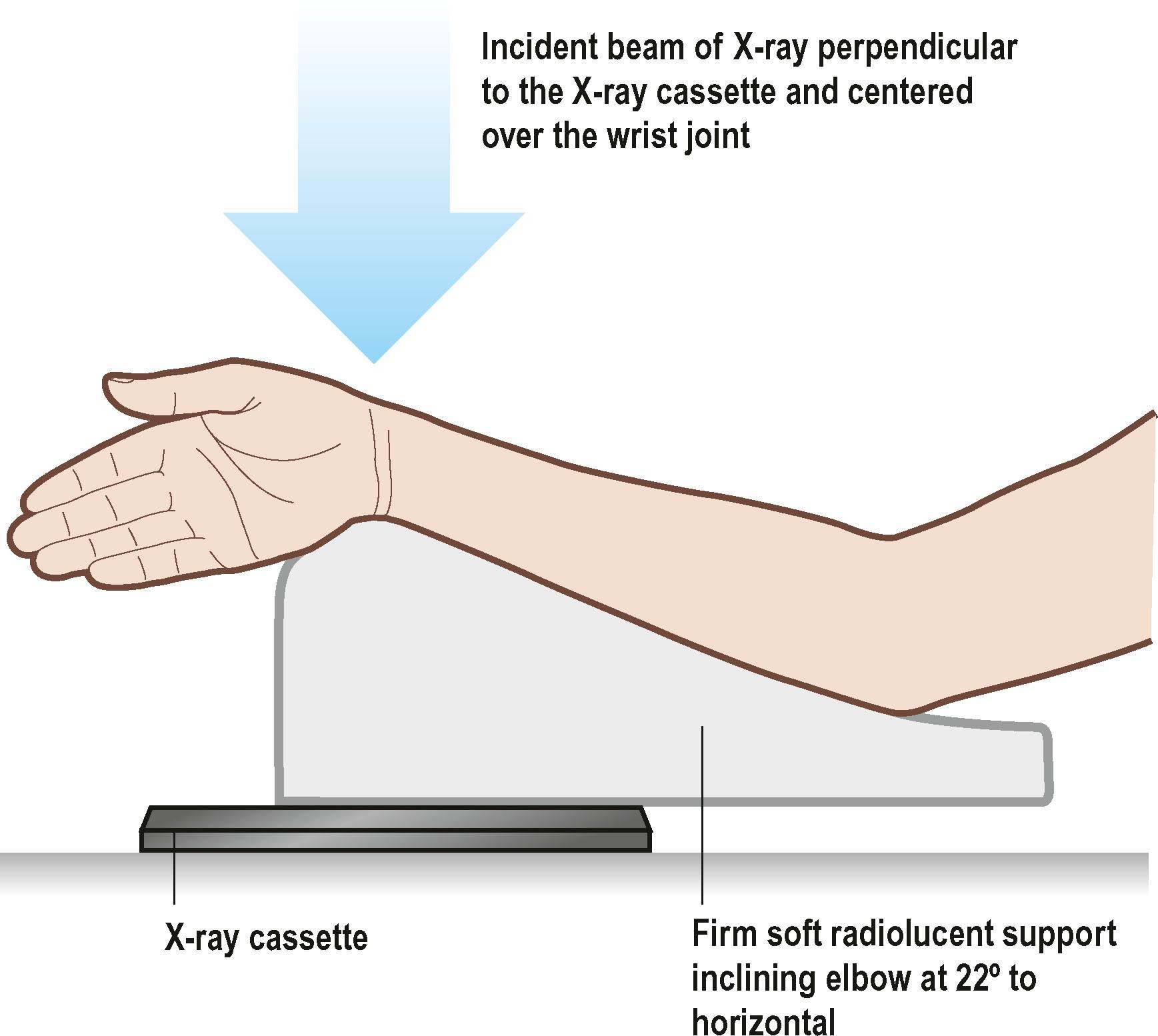
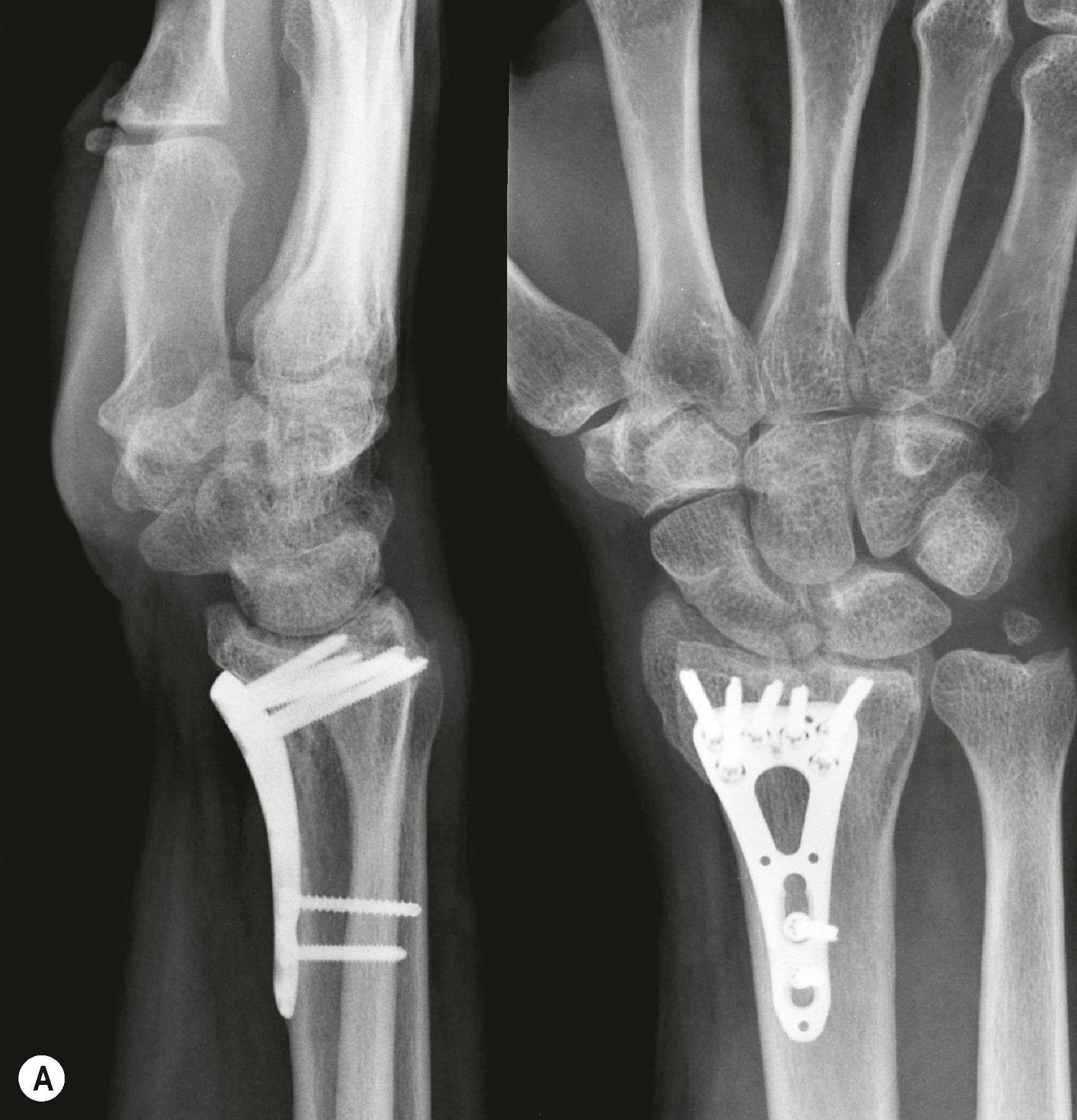
Distal radius fractures are the commonest fractures encountered in the emergency room. Loss of the normal distal radius indices ( Figs. 3.26 & 3.27 ) due to fracture displacement can affect final outcome. Unstable and displaced fractures are commonly treated with plates and screws. Screws placed subchondrally offer the greatest rigidity in fixation. However, conventional wrist views do not allow accurate assessment of screw position, especially when a distal fracture line compels the surgeon to place the screws in close proximity to the radiocarpal joint. This is because standard views do not compensate for the normal anatomic tilt of the radius. Radiographs angled 22° lateral and 11° posteroanterior ( Fig. 3.28 ) enable tangential X-ray exposure to the articular surface and facilitate this assessment after fixation. With increasing using of volar plates for treatment of distal radius fractures, extensor tendon rupture from screw protrusion dorsally is a concern. Detection of dorsal screw protrusion from a lateral X-ray has a sensitivity of only 56%, and on average, protrusion of the radial-most screw can only be detected at a minimum of 6.5 mm of protrusion. Special X-ray views can be done to improve detection of screw protrusion ( Box 3.4 and Fig. 3.29 ).
This view aligns the X-ray beam to the radial side of the dorsal cortex, allowing easier detection of prominent screws in the first and second dorsal compartment.
This view aligns the X-ray beam to the dorsal-ulnar corner of the distal radius and allow easier detection of prominent screws in the fourth extensor compartment.
This view is done with the wrist hyperflexed and the X-ray beam aimed along the longitudinal axis of the radius.
The availability of fluoroscopy in many clinics and operating rooms allows the dynamic assessment of many hand and wrist conditions. Smaller, lower cost, and lower radiation mini C-arms have also lowered the barrier to acquiring such facilities. The clinician can operate the C-arm to obtain the best view and view changes in the relationships of the bones “live” with motion, loading, or application of stress. Fluoroscopy is helpful for assessing carpal instability, including SL injuries ( ![]() ) and midcarpal instability (
) and midcarpal instability ( ![]() ), guiding percutaneous insertion of implants, and assessing the position of implants.
), guiding percutaneous insertion of implants, and assessing the position of implants.
Ultrasound is widely used in hand surgery. The ultra-high frequency probes and smaller probe sizes allow higher-quality images of the hand and wrist ( ![]() ). Ultrasound's safety, portability, and relatively low cost have supported wider adoption.
). Ultrasound's safety, portability, and relatively low cost have supported wider adoption.
Beyond its accessibility and lack of radiation exposure, one additional advantage of ultrasound over other forms of advanced imaging, like CT scanning or MRI, is that it allows dynamic and real-time assessment. The addition of Doppler imaging enhances the information provided by the ultrasound study.
Ultrasound uses the acoustic properties of generated sound waves to form images. An ultrasound transducer generates the sound waves in pulses. When the transducer is applied over the surface of the part to be examined, the sound waves pass through tissues. At the junction of two tissues, an acoustic interface occurs. When the sound waves meet an acoustic interface, some of the sound wave energy is reflected, while the rest continues to be transmitted deeper. The greater the differences in material properties of the adjacent tissues, the more energy is reflected. The reflected sound wave is received in the transducer. This is then converted to an electrical signal for processing. The greater the sound reflected, the larger the amplitude of the reflected wave, and consequently, the brighter the image. The primary mode used in hand surgery is the B-mode where two dimensional images are created by simultaneous scanning the area of interest with a linear array of transducers. This provides a cross-sectional image with the horizonal and vertical directions corresponding to the real distances in tissue and the grayscale corresponding to the echo strength.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here