Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Keywords: Diagnosis; lung cancer; mind mapping; molecular; staging
Mind maps are used as a tool to illustrate the principles involved in the diagnostic evaluation of a patient with known or suspected lung cancer.
Addressed are factors important in establishing the diagnosis and defining the extent of disease; the histologic and molecular classifications of lung cancer; and the potential role for repeat biopsy in patients with acquired resistance to targeted therapies.
Reviewed are diagnostic platforms for tumor profiling in the clinical setting and the use of these technologies in the noninvasive evaluation of surrogate tissues for both disease monitoring and early diagnosis.
The personalized treatment of lung cancer begins with an accurate diagnosis and assessment of both the extent of disease and other clinically relevant prognostic and predictive factors that are necessary to define the optimal treatment approach. Treatment decision making relies on a number of both patient- and tumor-specific factors. Lung cancer is a heterogeneous disease, and recent advances in molecular analysis and the development of targeted therapy approaches have added to the complexity of the diagnostic evaluation. In addition, revisions in the staging system, changes in the pathologic classification, and the addition of minimally invasive diagnostic modalities have increased the importance of a coordinated multidisciplinary team approach to establish both the diagnosis and the tumor stage as efficiently as possible.
Mind mapping was developed as a technique to visually represent ideas and their nonlinear relationships. Mind maps have been used as teaching tools in a number of different fields, including medical education, to present complex information and improve recall. Originally developed by Tony Buzan, a mind map starts with a central idea or key concept, which is then linked by branches to related ideas. Mind maps include color and pictures to illustrate the intra- and inter-relationship between ideas. Unlike a linear algorithm or a concept map, a mind map begins with a central idea, and its relationships are depicted radially (i.e., radial or spider map). The information is organized hierarchically, with the most general information at the center and more detailed information depicted at the extremes of each relationship branch.
In this appendix, we use mind maps as a tool to illustrate the principles involved in the diagnostic evaluation of a patient with known or suspected lung cancer. The initial mind maps address the factors that are important in establishing the diagnosis and defining the extent of disease. Because of the growing importance of targeted therapies, we use this technique to illustrate both the histologic and molecular classifications of lung cancer. In addition, we address the potential role for repeat biopsy in patients with acquired resistance to targeted therapies. Lastly, we use mind maps to review diagnostic platforms for tumor profiling in the clinical setting and to assess the potential to use these technologies in the noninvasive evaluation of surrogate tissues for both disease monitoring and early diagnosis.
Fig. A.1 includes a mind map that outlines the factors that are important to address during the initial history and physical examination of a patient suspected of having lung cancer. The objectives of the initial evaluation are to estimate the probability that lung cancer is present and to assess for evidence of distant metastatic disease. In addition, the initial evaluation should clarify patient-specific factors that may affect treatment decision making if cancer is confirmed, including comorbidities, performance status, underlying lung function, and the patient’s values and goals.
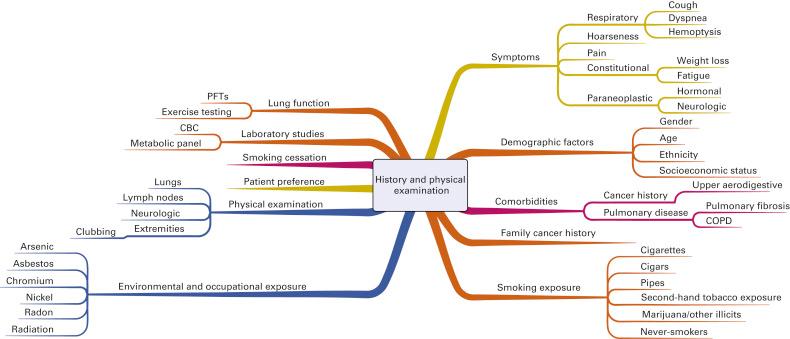
The initial risk assessment for lung cancer includes an evaluation of symptoms. Most patients with lung cancer will have symptoms at presentation. Symptoms may be due to the primary tumor or due to regional or distant spread of disease. Constitutional symptoms, including weight loss or fatigue, are important to consider because they may reflect an advanced stage of lung cancer. Several paraneoplastic syndromes have also been described, each with potentially unique clinical manifestations. Early recognition of a paraneoplastic process is important to minimize the risk for long-term morbidity and mortality.
The most common risk factor for lung cancer remains tobacco smoking. Lung cancer is 10 to 20 times more likely to develop in individuals with a history of smoking than in persons who have never smoked. The individual risk is affected by age as well as the duration and intensity of smoking. Lung cancer develops in only a minority of smokers, however, so inherited factors may also play a role in lung cancer risk. Other environmental and occupational exposures are also important to consider (see Fig. A.1 ). For example, pollution is increasingly being recognized as a risk factor for lung cancer. Important personal risk factors include age, gender, ethnicity, socioeconomic status, and comorbidities, including acquired lung disease. Although more men than women will die of lung cancer, the gender gap is narrowing, and lung cancer is the leading cause of cancer-related mortality among women in the United States. Although the rates of lung cancer are similar for black and white women, the incidence of lung cancer is higher among black men than among white men. Both the incidence of and mortality from lung cancer are higher in populations of lower socioeconomic status.
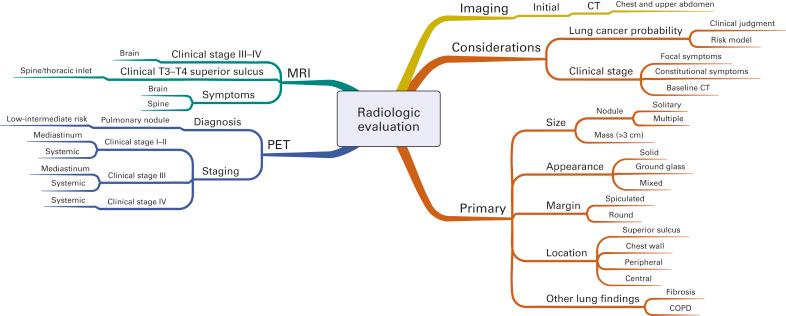
Fig. A.2 is a mind map that illustrates the radiologic evaluation. All patients should have initial computed tomography (CT) of the chest and upper abdomen that extends through the adrenal glands. The decision to pursue additional imaging for diagnosis and staging depends on both the estimated risk of lung cancer and the initial clinical stage. When patients have focal symptoms suggestive of metastatic disease, directed imaging (e.g., magnetic resonance imaging of the spine or brain) is recommended for confirmation. The radiographic characteristics of the primary abnormality in the lung that affect the risk assessment include the size, radiographic appearance, margin, and location of this lesion, as well as any underlying lung disease or additional lesions. Positron emission tomography (PET) is used in the diagnostic evaluation to characterize pulmonary nodules considered to be at low to intermediate risk for lung cancer. PET is not recommended to characterize abnormalities considered to be at high risk for lung cancer. However, PET is frequently recommended for mediastinal and systemic staging in most patients, including patients with early (stage I–II), locally advanced (stage IIIA–IIIB), and metastatic (stage IV) disease. In addition to PET, magnetic resonance imaging of the brain is frequently recommended for staging of patients with clinical stage III or IV disease.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here