Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
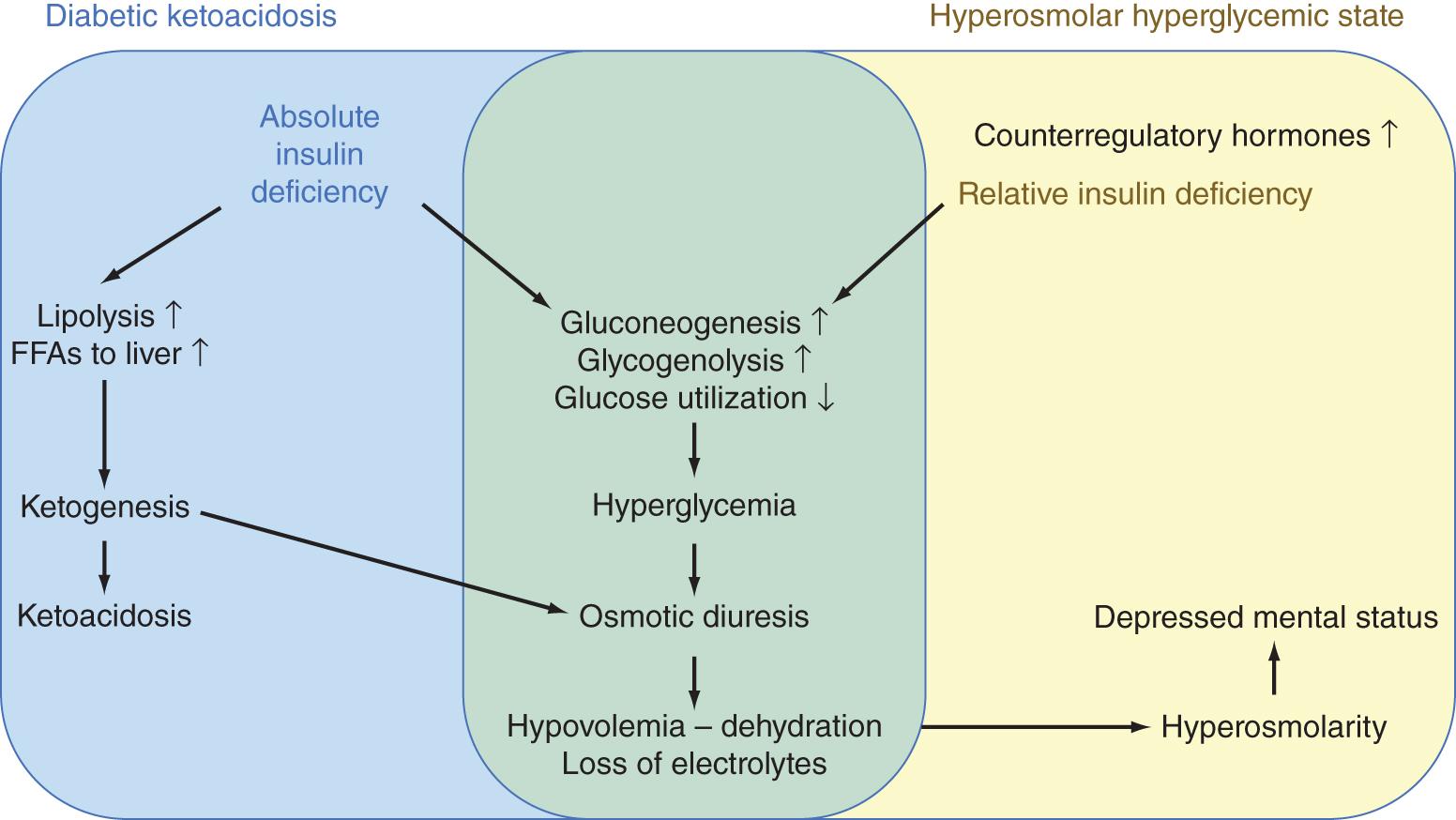
Diabetic ketoacidosis (DKA) and hyperosmolar hyperglycemic state (HHS) are endocrine emergencies occurring in diabetes patients. Both conditions require prompt, adequate treatment to avoid mortality. In patients with known diabetes mellitus, both conditions are most commonly triggered by noncompliance with diabetes treatment or infection. Nevertheless, any condition that induces severe insulin resistance and elevated counterregulatory hormones may trigger DKA or HHS, including severe trauma, myocardial infarction, and stroke. DKA and HHS may be the presenting syndrome of previously unknown or new-onset diabetes. ,
DKA and HHS are caused by an absolute or relative, respectively, insulin deficiency in the presence of elevated counterregulatory hormones (glucagon, cortisol, growth hormone, and catecholamines) ( Fig. 135.1 ). This constellation leads to increased hepatic gluconeogenesis and glycogenolysis and reduced peripheral glucose utilization in insulin-dependent tissues. The resultant hyperglycemia induces glycosuria once above the renal threshold, leading to osmotic diuresis and significant losses of water and electrolytes, in particular potassium and phosphate. In cases of (nearly) absolute insulin deficiency or very severe insulin resistance with substantially elevated counterregulatory hormones, lipolysis is activated, and free fatty acids are oxidized to ketone bodies in the liver. Ketones by themselves may aggravate osmotic diuresis, and accumulation of ketone bodies induces ketoacidosis. In patients with residual insulin effect, hepatic ketogenesis is suppressed. As a result, hyperglycemia and associated fluid and electrolyte losses further aggravate, eventually leading to a hyperosmolar hyperglycemic state, characterized by severe dehydration and alterations in mental state. As DKA can only develop in cases of minimal insulin effect, it mainly occurs in patients with type 1 diabetes, whereas HHS develops in patients with type 2 diabetes. DKA usually develops rapidly (within 24 hours), whereas HHS develops more insidiously over days.
In the vast majority of cases, DKA patients present with severe hyperglycemia (>200–250 mg/dL [11.1–13.9 mmol/L]). However, some diabetes patients at risk—taking sodium-glucose co-transporter 2 (SGLT2) inhibitors, pregnancy, excessive alcohol intake, prolonged fasting, chronic liver disease—may develop ketoacidosis in the absence of elevated blood glucose concentrations. Several pathophysiologic mechanisms may contribute to the so-called “euglycemic DKA” or “DKA with lower-than-anticipated glucose levels,” including increased urinary glucose losses, glucose uptake by the fetus, and insufficient gluconeogenesis because of lack of substrate or liver disease.
In most cases, the diagnosis of a hyperglycemic emergency is obvious after taking a history and performing a clinical examination and is confirmed by laboratory examination ( Table 135.1 ). Apart from diagnosing DKA/HHS, the precipitating event also should be sought, which often needs additional diagnostic tests.
| Diabetic Ketoacidosis | Hyperosmolar Hyperglycemic State |
|---|---|
| Precipitant Factors | |
| Noncompliance with insulin treatment | Noncompliance with treatment |
| Infection | Infection |
| New-onset (type 1) diabetes | New-onset (type 2) diabetes |
| Other | Other (corticosteroids, excess diuretics, etc.) |
| Course of Illness | |
| Rapid (in general <24 hours) | Insidious (days) |
| Clinical Findings | |
| Polyuria, polydipsia, dehydration, hypovolemia | Polyuria, dehydration, hypovolemia |
| Nausea, vomiting, abdominal pain | Depressed mental status up to coma |
| Fruity odor of breath, Kussmaul respiration | |
| Diagnostic Laboratory Criteria | |
| Blood glucose >200–250 mg/dL * | Blood glucose >540–600 mg/dL * |
| AND elevated ketones in blood or urine | AND serum osmolality >320 mmol/kg |
|
|
| Concomitant Laboratory Abnormalities | |
| Elevated anion gap | Variable anion gap |
| Low C-peptide | Normal C-peptide |
| Acute kidney injury | |
* For conversion of blood glucose concentrations in mg/dL to mmol/L, divide by 18. American Diabetes Association guidelines recommend the highest reported blood glucose cutoff for both diabetic ketoacidosis and hyperosmolar hyperglycemic state, UK guidelines the lowest. , , In patients at risk—taking sodium-glucose co-transporter 2 (SGLT2) inhibitors, pregnancy, excessive alcohol use, decreased caloric intake, chronic liver disease—ketoacidosis may develop in the absence of elevated blood glucose concentrations (euglycemic diabetic ketoacidosis).
Patients with DKA/HHS present with polyuria and clinical signs of volume depletion and weight loss, which are accompanied by polydipsia in alert patients. Nausea, vomiting, and abdominal pain frequently occur in DKA patients but not in HHS patients. , DKA patients usually present with Kussmaul respiration because of metabolic acidosis, with a fruity breath scent resulting from exhaled acetone. Patients with HHS and severe DKA typically have decreased consciousness secondary to the pronounced metabolic alterations and volume depletion. Focal neurologic deficits and seizures may also occur in HHS.
DKA patients usually present with the classic triad of severe hyperglycemia (the “D” in DKA), ketosis (“K”), and metabolic acidosis (“A”). The key diagnostic criterion in DKA is a significant elevation in circulating ketone concentrations.
Three ketones are produced in DKA: acetoacetate, a ketoacid produced by the liver; beta-hydroxybutyrate, a hydroxyacid formed by reduction of acetoacetate; and acetone, a true ketone that is formed by decarboxylation of acetoacetate and that is exhaled. Increased ketogenesis can be confirmed by measuring increased circulating ketone concentrations or by detecting ketonuria. The preferred diagnostic test is the direct measurement of blood beta-hydroxybutyrate, however, for several reasons. First, beta-hydroxybutyrate is the most abundant circulating ketone in DKA, exceeding values of 3 mmol/L (31 mg/dL). Second, the alternative test, the nitroprusside test, which semiquantitatively detects acetoacetate in blood or urine, may yield false-positive and false-negative results. Finally, acetoacetate testing may not be reliable to monitor therapy during DKA. Indeed, because beta-hydroxybutyrate is converted into acetoacetate during treatment to be excreted in the urine, rise in acetoacetate concentrations may falsely give the impression of insufficient treatment response.
The traditional blood glucose cutoff of DKA is 200–250 mg/dL (11.1–13.9 mmol/L), and in most cases, admission blood glucose is even considerably higher. , However, in patients with additional risk factors—SGLT2 inhibitors, pregnancy, excessive alcohol intake, prolonged fasting, chronic liver disease—DKA may develop without severe hyperglycemia. Moreover, pseudonormoglycemia may develop in cases of severe hyperlipidemia.
The third diagnostic criterion of DKA is metabolic acidosis (pH <7.3 and HCO 3 − <18 mmol/L) with elevated anion gap, explained by the accumulation of ketones. Metabolic acidosis can be classified as mild (pH 7.25–7.3 and HCO 3 − 15–18 mmol/L), moderate (pH 7.0–7.24 and HCO 3 − 10–14.9 mmol/L), or severe (pH <7.0 and HCO 3 − <10 mmol/L).
HHS is characterized by more severe hyperglycemia (>540–600 mg/dL [30–33.3 mmol/L] and often >1000 mg/dL [55.6 mmol/L]) and hyperosmolarity (serum osmolality >320 mmol/kg) in the absence of significantly elevated ketone concentrations and metabolic acidosis. , However, mild ketonemia may develop. The laboratory alterations in HHS are typically accompanied by severely impaired mental status (stupor, coma).
DKA and HHS patients may have secondary organ damage because of volume depletion, including acute kidney injury. Acute kidney injury is usually more pronounced in HHS patients, because of a more protracted time course before admission and more severe volume depletion. Although patients have a potassium and phosphate deficit, admission serum potassium and phosphate are often normal or elevated as a result of insulin deficiency, hypertonicity, and acidemia. Severe hyperlipidemia caused by lipolysis may lead to pseudohyponatremia and pseudonormoglycemia in DKA. Because infection is a common trigger for DKA and HHS, patients often have increased inflammatory parameters upon admission. C-peptide is low in DKA patients because of absolute insulin deficiency, whereas C-peptide is usually in the normal range in HHS patients.
Initial treatment consists of fluid resuscitation, insulin therapy, potassium supplementation, and treatment of the precipitating cause ( Box 135.1 ). Other treatments, including bicarbonate and phosphate substitution, are controversial. After resolution of ketoacidosis and HHS, insulin therapy should be switched to maintenance therapy. , ,
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here