Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Type 1 and type 2 diabetes are associated with a variety of symptoms at all levels of the gastrointestinal tract, a phenomenon documented by Rundles as early as 1945 . Probably the best known gastrointestinal complication of diabetes is gastroparesis, and diabetes is the underlying cause in about one-third of patients attending specialist centers with a diagnosis of gastroparesis .
The first detailed description of diabetic gastroparesis was by Kassander in 1958, who used the term “gastroparesis diabeticorum” to describe abnormal retention of barium contrast in the stomach – similar to that following vagotomy – in a series of six patients who had typically been diagnosed with diabetes from a young age and had a high prevalence of other complications including neuropathy . The retention of gastric contents in these cases was asymptomatic, so Kassander assumed that it was “more often overlooked than diagnosed”, and surmised that this would likely contribute to erratic glycemic control, since (referring to insulin-treated patients) “the retention of stomach contents in a diabetic obviously may cause confusion as far as food intake and utilization are concerned”.
In this chapter, the definition and epidemiology of diabetic gastroparesis will be reviewed, along with its clinical manifestations, etiology and pathophysiology, investigation, and management, with an emphasis on the inter-dependent relationship between the rate of gastric emptying and control of blood glucose concentrations.
Diabetic gastroparesis is broadly defined by abnormally slow emptying of solids and/or nutrient liquids from the stomach, in the absence of mechanical obstruction, in a person with diabetes . What is not universally agreed is whether upper gastrointestinal symptoms are required to make the diagnosis. Symptoms are known to have only a weak association with the presence of delayed gastric emptying and, as noted, Kassander recognized that patients with gastric retention may be asymptomatic, even if potentially troubled by other sequelae, particularly impaired glycemic control . Moreover, in many patients with diabetes who have prominent upper gastrointestinal symptoms, gastric emptying is well within the normal range, or occasionally abnormally rapid , so the diagnosis of gastroparesis cannot be made on the basis of symptoms alone. There is recent recognition that small intestinal dysfunction can also contribute to symptoms, so that a broader label of “diabetic gastro-enteropathy” may be a more appropriate term to encompass symptomatic patients with diabetes .
Estimates of the prevalence of diabetic gastroparesis vary widely depending on whether the focus is on a community-based or a tertiary referral population, and the definition of gastroparesis that is employed. The issue is of major relevance to the utilization of healthcare resources, given evidence from the US Nationwide Emergency Department Sample that Emergency Department visits for diabetic gastroparesis more than doubled between 2006 and 2013 (from 4.7 to 10.5 per 100,000 visits) with an escalation in associated costs from $84 million to $182 million . Moreover, symptomatic diabetic gastroparesis is a risk factor for prolonged hospitalization amongst patients with diabetes . The implication for healthcare costs is already profound, but the global prevalence of diabetes amongst adults is predicated to rise further, from 8.4% in 2017 to 9.9% by 2045 .
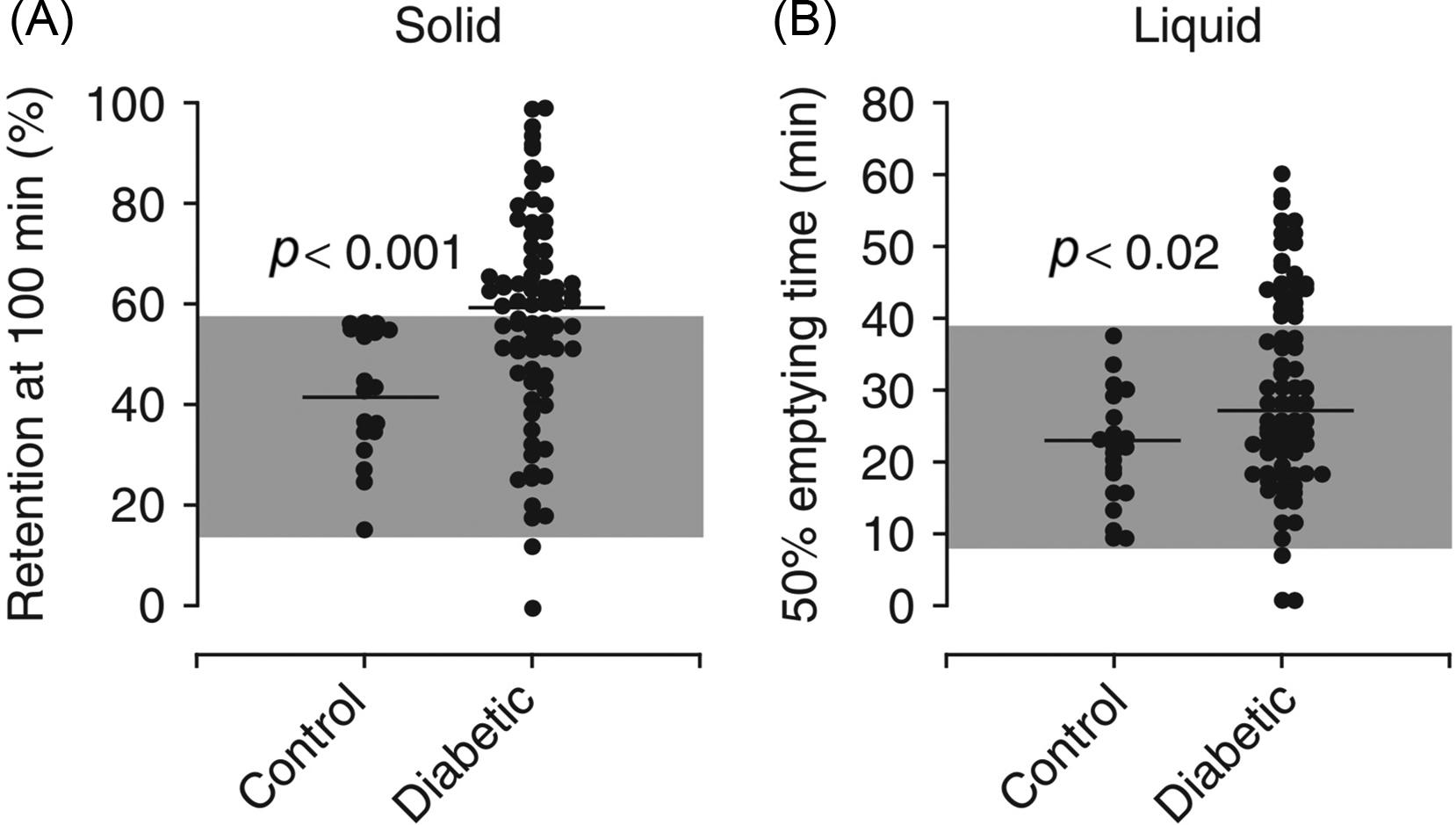
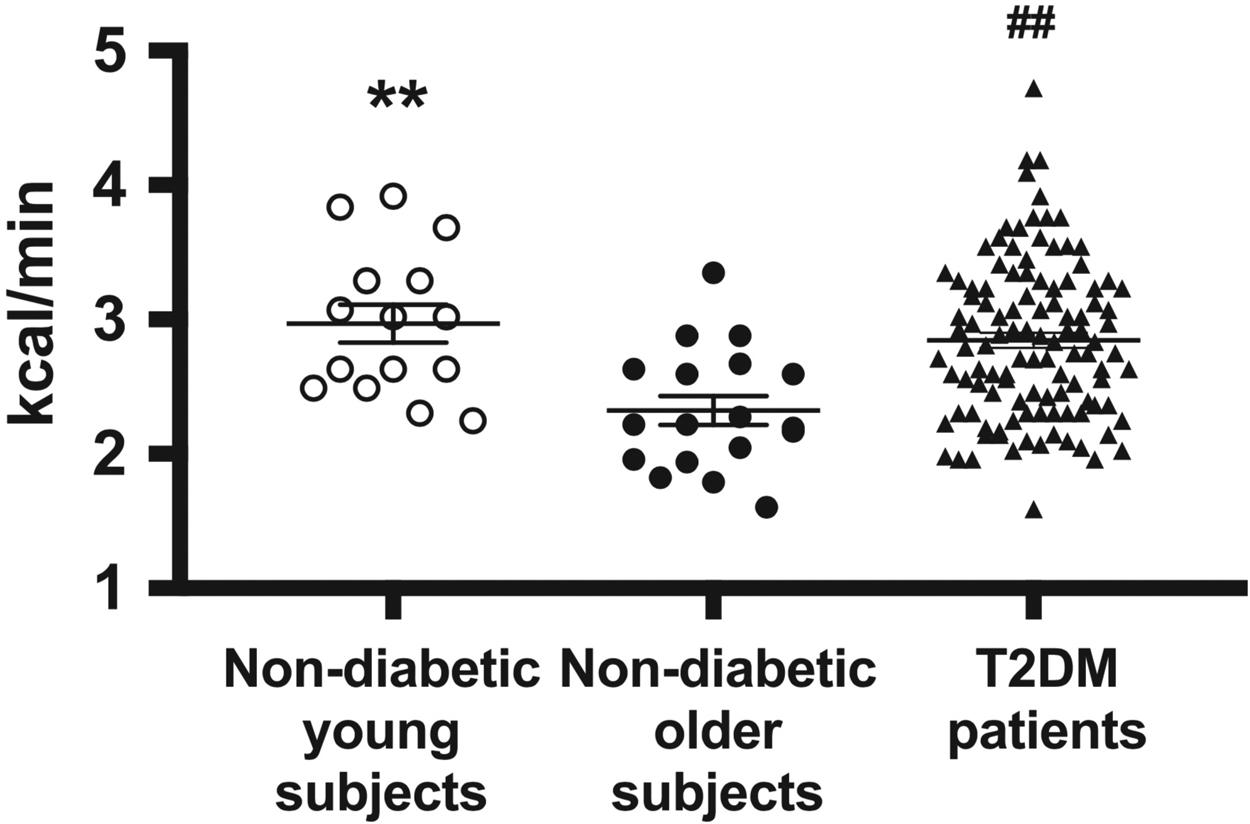
A cross-sectional study from our own tertiary referral center over 25 years ago indicated that between 30–50% of patients with longstanding, mostly type 1 diabetes, not selected on the basis of gastrointestinal symptoms, had abnormally slow emptying of solids, nutrient liquids, or both ( Fig. 18.1 ). A recent assessment of 78 patients with type 1 diabetes at the 20 year point in the Epidemiology of Diabetes Interventions and Complications (EDIC) extension of the Diabetes Control and Complications Trial (DCCT) yielded remarkably similar outcomes, with 47% having delayed gastric emptying of a solid meal . There is less information about gastric emptying early in the course of type 1 diabetes, but we showed that emptying of a solid meal was, if anything, more rapid in children and adolescents with type 1 diabetes when compared to age-matched controls . Until recently, there was less information about patterns of gastric emptying in type 2 diabetes, but recent studies from our group and others indicate that patients with uncomplicated type 2 diabetes and good glycemic control have gastric emptying within the normal range, or even slightly more rapid than age-matched controls ( Fig. 18.2 ), consistent with some earlier reports in recently diagnosed type 2 patients . In patients with complicated type 2 diabetes and less than optimal glycemic control, the prevalence of gastroparesis is likely to be similar to type 1 diabetes , and a majority of cases of diabetic gastroparesis is likely to occur in type 2 patients, simply because they greatly outnumber type 1. The picture is confounded by the observation that longstanding diabetes, including type 2, is associated with a loss of capacity to secrete islet amyloid polypeptide – which itself slows gastric emptying .
The best available information on the prevalence – or rather, cumulative incidence – of gastroparesis in a community-based sample comes from Minnesota . Over the course of a decade, 5% with people with type 1%, and 1% of those with type 2 diabetes, developed gastroparesis, defined by either a scintigraphic study or the presence of “typical” symptoms. However, it is likely that this is a substantial underestimate, since only a minority of those with symptoms, and almost none who are asymptomatic, are likely to have had gastric emptying measured. However, a multi-center US study analyzing over 7000 patients from the T1D Exchange Clinic Registry Database also indicated that about 5% of type 1 patients have gastroparesis, with risk factors including older age and longer duration of diabetes, female sex, higher glycated hemoglobin (HbA1c), lower socio-economic status, and greater prevalence of microvascular complications, especially neuropathy .
When simply considering gastrointestinal symptoms, a number of studies have reported that upper gut symptoms such as nausea, vomiting, fullness, and early satiation are substantially more prevalent in diabetes patients attending specialist clinics when compared to controls . In community-based surveys (which relate for the main part to type 2 diabetes), by contrast, the increase in symptom prevalence over non-diabetic controls is more modest , but as with gastroparesis, there is a female predominance, and an association with poor glycemic control as assessed by HbA1c . Specific symptoms that are increased over the general population include nausea, vomiting, bloating, early satiation, abdominal pain, and heartburn . It should be noted that in some cases, these symptoms could be associated with diabetic medications, including metformin and acarbose. As in functional dyspepsia, there is a “turnover” of symptoms when observed over several years, i.e. as some symptoms resolve, new ones emerge, with a relatively stable net symptom burden . Upper gut symptoms in diabetes, as in functional dyspepsia, are strongly associated with anxiety and depression, and impaired quality of life . Gastroparesis specifically is associated with lower quality of life than the general population, in proportion to symptom severity .
Normal gastric emptying relies on the close coordination of contractile activity in different regions of the stomach and proximal small intestine . The proximal stomach initially relaxes to accommodate the volume of an ingested meal with minimum rise in intragastric pressure, followed by a progressive increase in tone that generates pressure to drive the gastric emptying of liquids. The antrum grinds solids into particles no more than 1–2 mm in diameter before pumping the resulting chyme across the pylorus, which acts as a brake to gastric outflow by generating phasic and tonic pressures. Coordination between antral and duodenal contractions is an important contributor to efficient transpyloric flow. Interaction between nutrients and the small intestinal mucosa initiates neural and hormonal feedback (including cholecystokinin, glucagon-like peptide-1, and peptide YY) to slow further gastric emptying; this feedback is critical in optimizing the transit and mixing of luminal content with the mucosal surface for digestion and absorption.
Digestible solids empty from the stomach in an overall linear fashion, following an initial lag phase. Low-nutrient liquids empty in a mono-exponential fashion, with this curve becoming more linear as the nutrient content of ingested liquid increases. In this way, nutrients exit the stomach at a caloric rate that is relatively constant within individuals, but with substantial inter-individual variation, in the range of 1–4 kcal/min , influenced amongst other factors by age and ethnicity .
Postprandial patterns of antro-duodenal contractions ultimately revert to a fasting pattern, usually with a burst of activity (“phase III”) during which indigestible solids are emptied from the stomach and swept along the small intestine. While fasting persists, the upper gastrointestinal tract undergoes a cyclical pattern of activity known as the migrating motor complex (MMC), characterized by motor quiescence for about 40 min (phase I), irregular contractions of increasing frequency for about 50 min (phase II), and 5–10 min of regular contractions at the maximum rate in the stomach (3/min) and small intestine (10–12/min) . The waves of electrical depolarization that underly each contraction are controlled by specialized “pacemaker cells”, the interstitial cells of Cajal, with the gastric pacemaker being situated about two-thirds up the length of the greater curvature from the pylorus.
Motor abnormalities in patients with diabetic gastroparesis are heterogeneous, and include a reduction in fasting tone of the proximal stomach, but also impaired meal-induced accommodation , hypomotility of the antrum , disordered duodenal motility and flow patterns , and reduced coordination between antrum and duodenum . Some patients with gastroparesis demonstrate pylorospasm , and/or a poorly compliant pyloric sphincter . Abnormalities of the gastric electrical rhythm are also evident, with abnormal initiation and conduction of the slow wave . The variable contribution of these underlying abnormalities in different patients suggests that, ideally, management should be personalized based on individual pathophysiology.
Patients with longstanding type 1 diabetes and those with refractory diabetic gastroparesis display increased sensitivity to proximal gastric distension compared to healthy controls, further suggesting that the etiology of upper gastrointestinal symptoms is likely to be multi-factorial and not simply related to delayed gastric emptying.
Gastroparesis had, until recently, widely been assumed to represent a manifestation of autonomic neuropathy arising as a complication of longstanding diabetes, particularly sub-optimally controlled type 1 diabetes . In both patients with diabetes, and in rodent models, there is a reduction in cells in the vagal motor and sensory sympathetic ganglia, with structural abnormalities of vagal nerve fibers both intrinsic and extrinsic to the gut wall that include axonal degeneration and segmental demyelination . Evaluation of gastrointestinal autonomic function in humans is, unfortunately, imprecise, as it is reliant on a range of indirect tests, including assessment of cardiac autonomic function , evaluation of adrenergic and sudomotor responses, and the pancreatic polypeptide response to sham feeding; the latter has good specificity but limited sensitivity . Some studies have reported a relationship between delayed gastric emptying and markers of autonomic neuropathy and others not , but generally any relationship is found to be weak , suggesting that additional mechanisms are likely to be involved.
In the last decade, full thickness gastric biopsies, particularly from patients enrolled in the Gastroparesis Clinical Research Consortium (GpCRC; a multi-center collaboration of US institutions), have revealed a much more heterogenous picture, with loss of ICC, an immune infiltrate, and small muscle atrophy, in addition to abnormalities of the enteric and extrinsic nervous systems . These patients from specialized referral centers largely represent longstanding, symptomatic gastroparesis that has been resistant to multiple therapies, so whether the findings generalize to a broader spectrum of patients remains uncertain. However, the concept that ICC loss is driven by macrophages, immune dysregulation, and oxidative stress now has widespread support . Murine models reveal a switch from alternately activated CD206+ M2 macrophages which express heme oxygenase-1 (HO-1) and are cytoprotective, to classically activated M1 macrophages that produce damaging cytokines resulting in ICC loss . The latter can be reversed in mice using antioxidant therapies such as hemin or carbon monoxide . In patients with diabetic (but not idiopathic) gastroparesis, the degree of slowing of gastric emptying is related to the loss of ICC in biopsies and, as in mouse models, the latter is associated with loss of CD206+ macrophages . ICC loss is even more marked in the pylorus than the antrum, and associated with fibrosis . However, a randomized controlled trial of hemin infusions – used in clinical practice to treat the porphyrias – in 20 patients with diabetic gastroparesis failed to improve gastric emptying or symptoms, and the increase in HO-1 was not sustained after the first week ; the authors suggested that either the dose may have been inadequate (limited in part by the high cost of hemin) or the disease process had reached an irreversible stage.
Other abnormalities supported by animal models include a preferential loss of inhibitory neurons expressing nitric oxide synthase (nNOS) , and accumulation of advanced glycation end products which could lead to structural remodeling and resultant motor and sensory abnormalities . Altered expression of the Ano-1 gene, which encodes a calcium-activated chloride channel that mediates electrical conduction in the ICC, has been reported , and patients with diabetic gastroparesis have been shown to manifest long alleles of the HMOX1 gene, which is associated with nausea . Proteomic studies indicate differential protein expression in diabetic gastroparesis that correlates with specific symptoms (e.g. properdin with bloating), or with gastric emptying (e.g. prostaglandin G/H synthase) .
It has long been established that variations in the blood glucose concentration influence gastric motor function in both healthy volunteers and patients with type 1 diabetes. For example the induction of acute hyperglycemia (~15 mmol/L) slows gastric emptying , associated with a reduction in antral motility and proximal gastric tone , stimulation of pyloric contractions , and disturbance of the gastric electrical rhythm , potentially mediated by endogenous prostaglandins or nitric oxide . Even modest changes in glycemia, within the normal postprandial range (8 mmol/L), can slow gastric emptying , while insulin-induced hypoglycemia (~2.5 mmol/L) accelerates emptying substantially, even in patients with longstanding type 1 diabetes and gastroparesis ; this represents a counter-regulatory mechanism to hasten the absorption of ingested carbohydrate .
The influence of chronic variations in glycemia on gastric motility is less clear. As discussed, cross-sectional data show an association between higher HbA1c and an increased prevalence of gastrointestinal symptoms , but in itself this does not provide direct evidence for an association with gastric emptying. An evaluation of a subset of the DCCT/EDIC cohort did not reveal any relationship between current HbA1c and the rate of gastric emptying ; however, emptying did relate weakly to both HbA1c at the time of entry into DCCT and the mean HbA1c over the intervening 27 years. This suggests that early, intensive treatment to control glycemia can reduce the incidence of gastroparesis, as has been shown for other complications of diabetes, including autonomic neuropathy .
It is controversial whether intensive therapy to control, and even normalize, blood glucose can reverse delayed gastric emptying once the latter is manifest. Observations in patients receiving combined kidney/pancreas transplants suggested this may be the case . However, intensifying therapy in poorly controlled patients with type 2 diabetes, either overnight using insulin infusions, or over 6 months, did not accelerate gastric emptying , although the improvement in HbA1c was relatively modest (reduction in mean HbA1c from 10.6% to 9.0%), so that in the majority of patients, diabetes was still poorly controlled. In another study where there was early restoration of euglycemia in women with newly diagnosed type 2 diabetes, gastric emptying was reported to improve markedly , although this study was uncontrolled.
Changes in the blood glucose concentration can alter the rate of gastric emptying, but conversely, the rate of emptying of a carbohydrate-containing meal is now appreciated to be a major determinant of the postprandial glycemic excursion ( Fig. 18.3 ). For example, the blood glucose concentration 30 min after a 75 g glucose drink is directly related to the rate of emptying of the drink from the stomach in individuals with either normal or impaired glucose tolerance, or type 2 diabetes . Some ethnicities, such as Hispanic Americans or Han Chinese appear particularly prone to postprandial hyperglycemia related to rapid gastric emptying. It is apparent, therefore, that type 2 patients who do not require insulin therapy are likely to benefit from dietary or pharmacological treatments that slow gastric emptying, as long as this does not induce symptoms or other adverse effects .
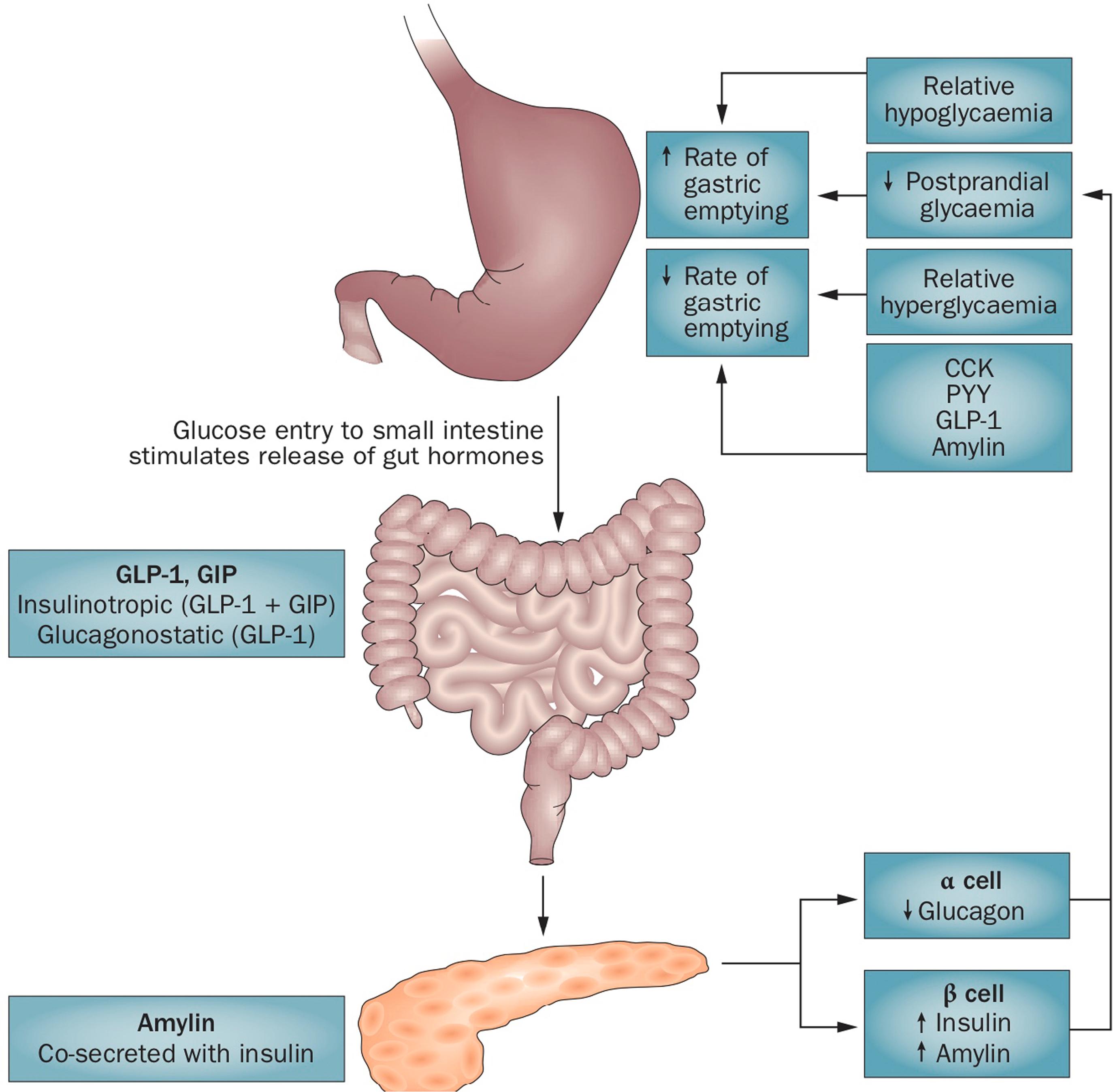
One class of antidiabetic medication that slows gastric emptying is the GLP-1 receptor agonists (GLP-1RAs). Some members of this class have a short plasma half-life (exenatide BD and lixisenatide) while others are longer-acting and suited to less frequent injection (e.g. daily for liraglutide or weekly for exenatide QW, dulaglutide, or semaglutide). While these medications reduce fasting hyperglycemia by their insulinotropic effect, with minimal risk of hypoglycemia since insulin stimulation is glucose-dependent (requiring blood glucose >7–8 mmol/L), and also suppress glucagon, their dominant mechanism of action to target postprandial glycemia is by slowing gastric emptying . The degree of slowing of emptying is related to the rate of gastric emptying at baseline, i.e. more marked in those with normal and especially rapid emptying, and minimal in those whose gastric emptying is already slow. Sustained stimulation of the GLP-1 receptor, however, results in tachyphylaxis for the effect to slow gastric emptying , suggesting that the short-acting GLP-1RAs are likely to maintain their effects on gastric emptying more strongly than the longer-acting members of the class. This appears to be the case in comparisons of exenatide BD with exenatide QW , and lixisenatide with liraglutide , albeit using suboptimal methodology to quantify gastric emptying. Recent evidence indicates, nonetheless, that exenatide QW maintains a substantial effect to slow gastric emptying after 8 weeks exposure in healthy volunteers . A highly effective treatment paradigm for longstanding type 2 diabetes is to use a long-acting insulin to control fasting glycemia, in combination with a GLP-1RA to diminish postprandial glucose excursions ; here again, it appears likely that a short- rather than long-acting GLP-1RA would be the ideal choice. An alternative medication that slows gastric emptying to control postprandial glycemia is the amylin analog, pramlintide , which is licensed in the US, but not in other markets, for the management of both type 1 and type 2 diabetes.
In patients with gastroparesis who have type 1 or insulin-treated type 2 diabetes, the delay in emptying of meals from the stomach increases the propensity for a mismatch between absorption of carbohydrates and the action of exogenous insulin therapy . For example, these patients require less insulin in the first 120 min after a meal, and more in the following 120 min, when compared to patients without gastroparesis . It is now recognized that “unexplained” episodes of hypoglycemia, particularly when they occur early in the postprandial period, may be the only presenting feature of diabetic gastroparesis, and should prompt measurement of gastric emptying . In such patients, glycemic control may best be improved by the use of a prokinetic drug to accelerate gastric emptying, in order to provide a more predictable match between carbohydrate absorption and insulin delivery. A recent meta-analysis of 5 clinical trials involving a variety of prokinetic drugs used over 4–24 weeks indicated a reduction in HbA1c (by ~1%) compared to placebo , although the frequency of hypoglycemic episodes was not specifically evaluated.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here