Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
A neuromodulation system may consist of two or more components, including the implantable pulse generator (IPG) and a therapy lead which delivers stimulation to the underlying neural tissue. The leads direct energy from the pulse generator to the target and provide key differentiation between device manufacturers. Some device variations include an external power source and a battery-free implantable pulse generator. It is important to understand both the therapies as well as the technology and engineering trade-offs when designing implantable neurostimulator systems (INS). This chapter will focus on device design and materials, as well as device safety considerations, with specific focus on deep brain stimulation (DBS) and spinal cord stimulation (SCS) systems.
Recent SCS and DBS advances have focused on new waveform frequencies, stimulation using more contacts to provide directional stimulation volume fields and closed-loop functionality. High-frequency (ex. kHz), subthreshold, and burst pulse patterns have been shown to provide paresthesia-free pain relief for some groups of patients [ ]. Similarly, directional DBS leads have recently been shown to outperform omnidirectional leads in providing a wider therapeutic window [ ]. New paradigms are beginning to use physiological signals (ex. evoked spinal cord potentials or respiration patterns) to synchronize device stimulation or to perform dosing of therapy to reduce habituation. Finally, devices seek to provide greater selectivity and more therapy coverage using a greater number of electrodes have employed active-Lead technology. Active-leads significantly increase the number of therapy electrodes with no increase in pulse generator size or lead tail complexity, breaking a decades-old neuromodulation limitation.
Emerging implanted devices are increasingly adopting technologies which have been matured by the commercial smartphones and tablet market. Clinical programmers are migrating to tablet applications and patient programmers are migrating to smartphone apps. New devices are also adopting commercial smartphone charging and communication chipsets for wireless charging and Bluetooth Low-Energy (BLE). These communication standards make it simpler to connect and upgrade implanted devices in the future.
Most manufacturers provide some level of magnetic resonance imaging (MRI) labeling for their neuromodulation systems. The chapter covers upgradeable implanted devices whereby new upgrades can be wirelessly uploaded to the device without the need for a surgery to replace the device.
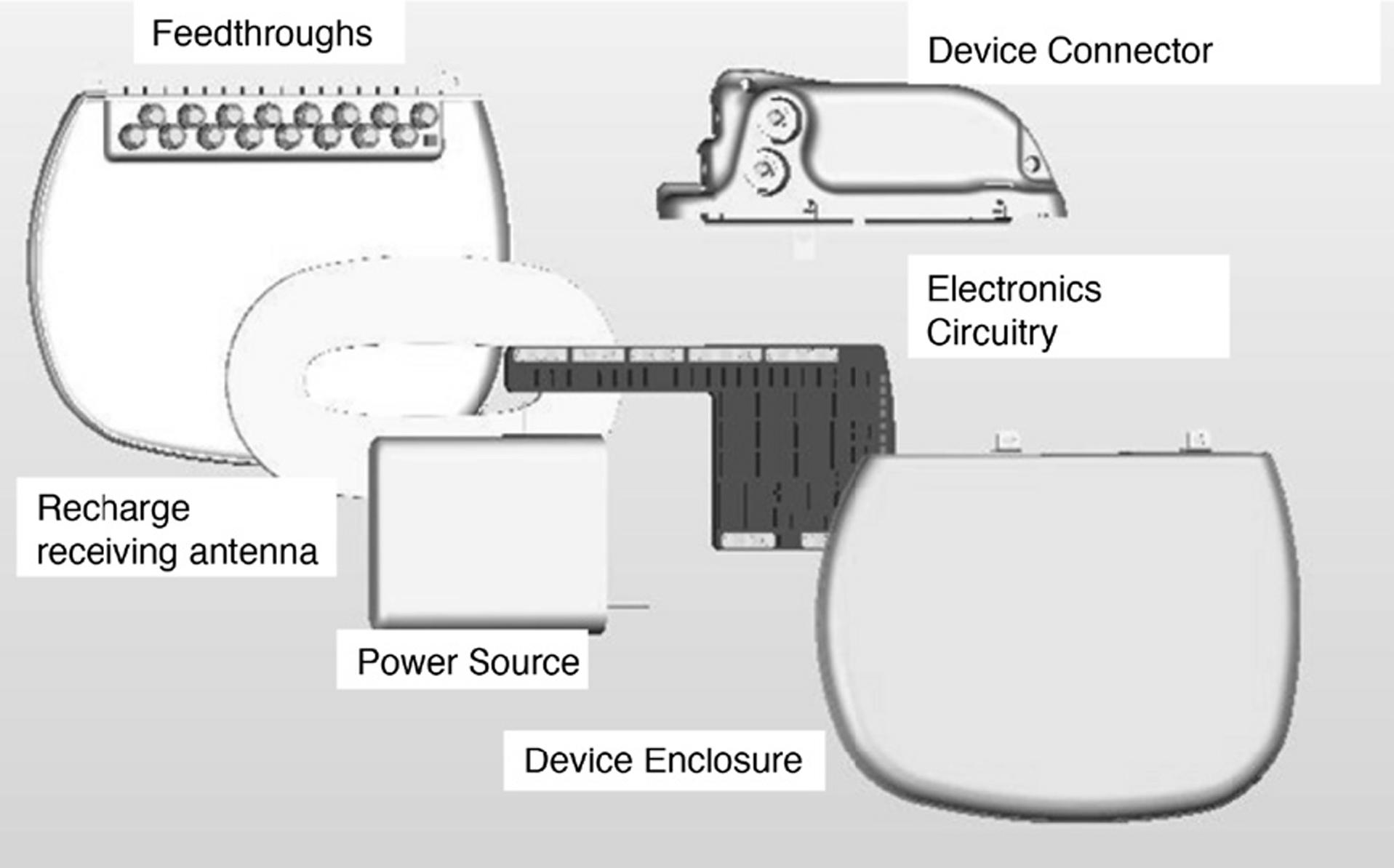
An implantable pulse generator consists of several components: the device enclosure, electronics pulse-generation circuitry and chipsets, communication and/or recharge antenna, hermetic feedthroughs, and a header with one or more ports ( Fig. 8.1 ). These systems may be classified into three types based on their power source: rechargeable, primary power source, and transcutaneous inductively powered devices. Most of the systems implanted today for DBS and SCS are rechargeable or primary power source devices. Recent devices for spinal cord, sacral nerve, and peripheral nerve stimulation have utilized wearable external power sources to wirelessly charge the implanted device.
Device enclosures are constructed from a titanium hermetic package. The power source and electronic circuitry are contained within this hermetic enclosure to ensure safe containment and prevention moisture ingress from contacting these components. Conversely, the packaging prevents potentially harmful substances present in the internal components from reaching the body. In rechargeable devices, typically a magnetic or radiofrequency (RF) energy is transferred from an external wearable charger with a transmitting antenna/coil to a receiving antenna/coil located on or inside the IPG. Many devices such as those from Medtronic and Boston Scientific are inductively charged, while some examples of radio frequency powering included the Medtronic Mattrix, Xtrel, and ANS Renew. Recent efforts by Stimwave have utilized the 510(k) pathway to develop new renditions of these types of radio frequency SCS devices.
Communication to the electronic circuitry is done with wireless telemetry between a clinician programmer and the patient programmer and the implanted IPG. Conventional devices utilized the Medical Implant Communication Standard (MICS) and 402–405 MHz antennas, whereas companies are migrating to the 2.4 GHz Industrial, Scientific, and Medical (ISM) band. The widespread availability of smartphones and tablets equipped with BLE provide an attractive means to program implanted device settings. An external patient programmer app or a clinician programmer app running on a tablet or smartphone may be used to establish communication with the device and to program stimulation therapy parameters. Tablets have begun to simplify the intraoperative programming sessions. Similarly, many IPGs have provided a smartphone with a software application that enables the patients to toggle between stimulation settings. The clinical programmer provides a greater range of adjustment than a patient programmer, as the patient may be restricted to certain ranges of use by the clinician, depending on the specific therapy and system.
The device header houses the electrical contacts that mate with the proximal extension or lead connectors. The number of canted-coil spring contacts typically matches the number of independently programmable therapy electrodes on the distal end of the lead. The lead or lead extension is inserted, positioned, and secured inside the device header with a torque wrench. Each electrical contact in the device header connects to a feedthrough conductor. For spinal cord and deep-brain stimulation, headers have 2–4 ports with typically 8–16 contacts per port. The total number of therapy electrodes on a lead has ranged between 16 and 32 contacts requiring 2–4 ports. The feedthroughs are electrical conductors that carry the stimulation current from the electronic circuitry through the hermetic enclosure. These feedthroughs are made of an insulative material, such as glass or ceramic, to maintain the electrical isolation between each other and from the device conductive enclosure material. The material of the device header electrically insulates the connection of each feedthrough conductor. The header configuration determines how many different leads can be utilized by the device. The header typically mates with single, dual triple, or quad lead systems. These systems support multiple cylindrical leads, 16–32 contact paddle leads, or a combination of leads.
The physical form factor and volume of the pulse generator is derived by balancing the clinical therapy stimulation requirements with the technology and engineering size, weight, and power constraints of the implanted device. The form factor is governed by a number of attributes including the number of therapy electrodes, power source type and energy capacity, and the stimulation output amplitude, duty cycle, and frequency.
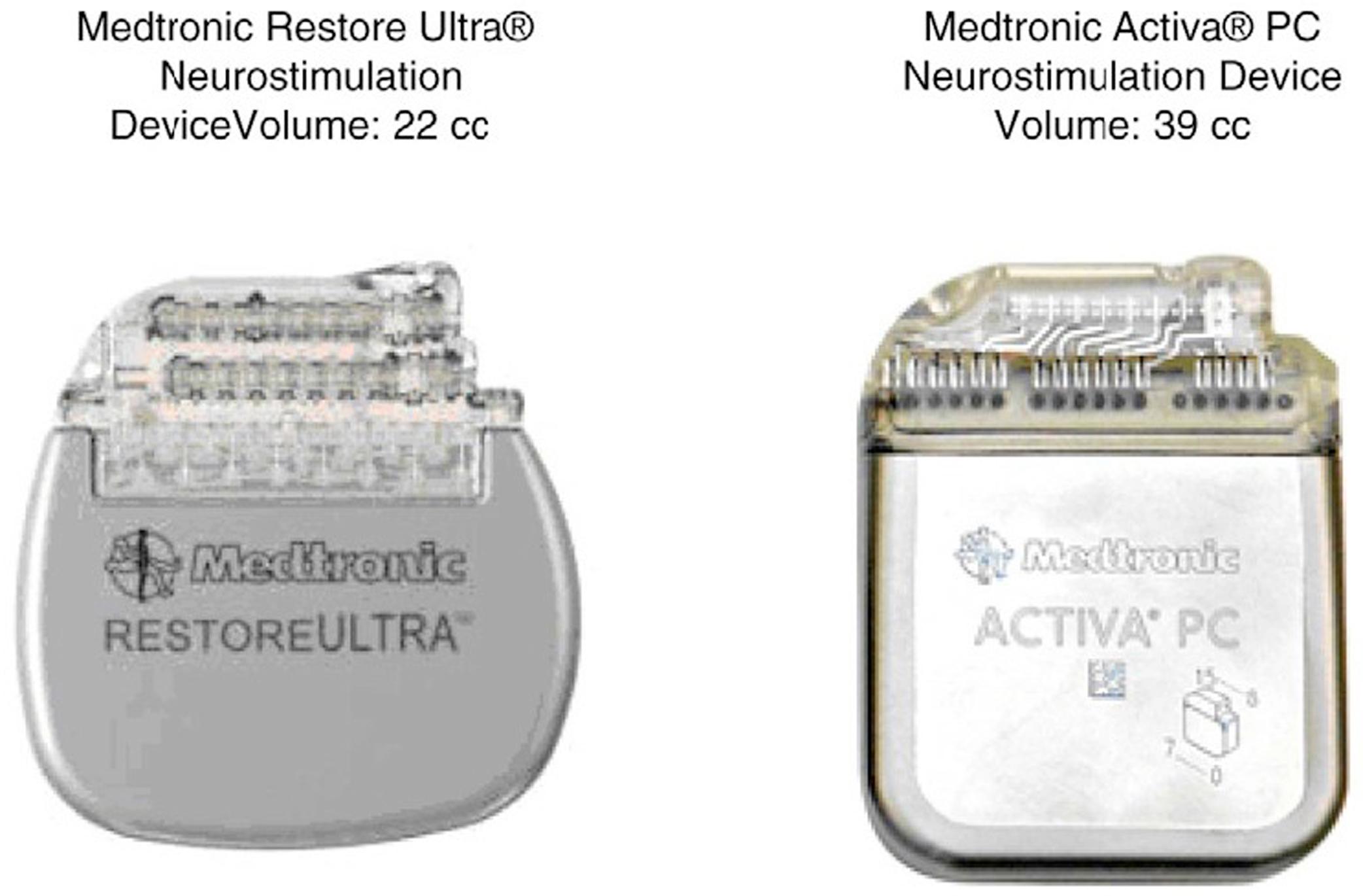
Significant technological advances in battery energy density, electronic circuitry miniaturization, and connector density have enabled IPG sizes to be reduced. Most IPGs for DBS and SCS are between 10 and 20 cm 3 in total volume which is dominated by the battery volume. While integrated circuits have miniaturized according to Moore's law, battery energy density has not [ ]. Some manufacturers have adopted a no-battery and no hermetic package approach such as the StimWave Freedom to reduce implanted volume, at the expense of requiring an externalized belt or patch on the overlying skin nearby to be worn during therapy delivery.
The IPG is typically implanted in a subcutaneous or submuscular pocket located below the subclavicular region, lower abdomen or upper buttocks ( Fig. 8.2 ). The size of the implanted device is primarily driven by the battery capacity and the number of header ports. More therapy electrodes require additional header ports which increase the device volume. In general, rechargeable devices or transcutaneous inductively coupled devices are smaller than nonrechargeable IPGs. Neuromodulation therapies that require less stimulation amplitude and fewer electrodes such as Dorsal Root Ganglia stimulation for chronic pain enable a smaller IPG to be realized. These smaller devices are implanted in different areas of the body and typically are implanted closer to the target therapy site. For example, StimWave Freedom promises that it can be implanted near the DRG, adjacent to the dorsal columns, or near peripheral nerves for any type of neuromodulation. Similarly, inductively powered cochlear implants are small enough for implantation in the mastoid process in the skull. Implanting the device closer to the target therapy site also has advantages in minimizing lead length. Recent RF “mid-field” charging methods provide slightly improved penetration depth for delivering energy to smaller-sized miniature implanted devices. By using 800 MHz–1.2 GHz RF antennas, the implanted receiver is reduced to an inefficient antenna which is smaller in volume than conventional inductive coils designed to operate at MHz frequencies. The dielectric constant and loss tangent of physiological saline, fat, bone, blood, and other tissues attenuate RF fields by approximately 30 dB/cm at 1 GHz. Therefore, RF powering methods have inherently poor coupling efficiency to the implanted device and require significant external transmit power levels and optimization methods such as beamforming to reduce energy losses and prevent tissue heating by exceeding the specific absorption rate (SAR) limits. Though touted as superior power transfer, mid-field powering lacks superiority for most applications—especially those requiring larger stimulation current such as DBS and SCS.
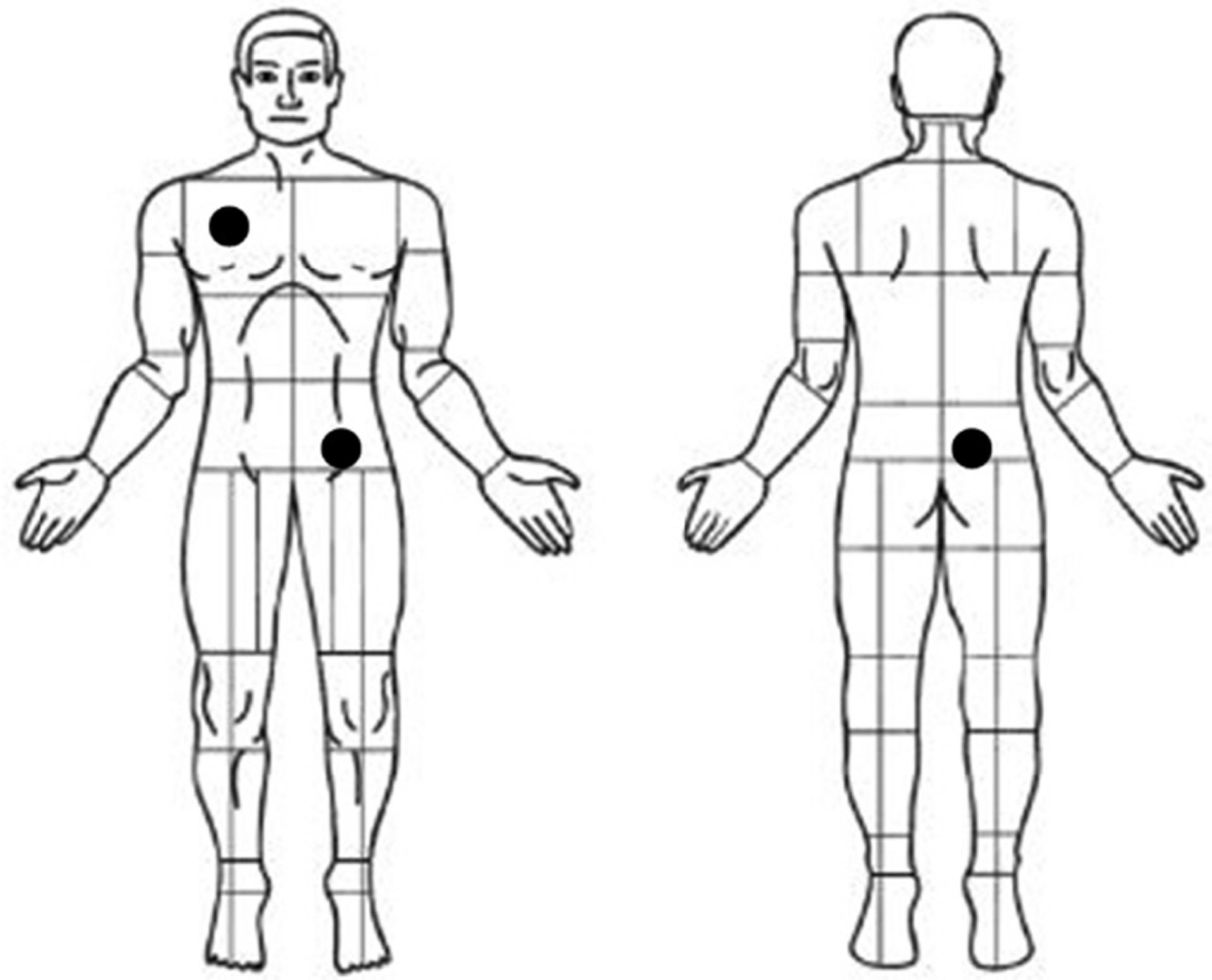
A small number of device complications around the IPG continue to occur in patients. The device shapes and form factor are designed to minimize tissue reaction and skin erosion by incorporating large-radii edges and header smoothness. The IPG thickness is especially important to minimize surgical pocket complications. Lower abdomen implant locations can tolerate approximately 12 mm thick and larger devices. In contrast, the subclavicular region requires thinner and smaller devices to prevent skin erosion. Smaller devices also provide an improved cosmesis effect for the patient to better conceal the system within subcutaneous tissues. Device form factors for SCS are shown in Fig. 8.3 [ ].
Implanting depth is an important consideration for recharge and telemetry. Implanting the device too shallow can result in skin erosion, while implanting the device too deep can result in poor recharge coupling or loss of inductive telemetry. Typical recharging depths range may be performed from 1 to 3 cm deep using conventional inductive coils placed within the titanium enclosure. Improvements in recharging have been achieved by incorporating inductive loops outside of the hermetic package (e.g., Neuros Medical Altius) to prevent the eddy current losses associated with charging through titanium. The receiving recharge coil is typically located external to the hermetic titanium package in the implanted device header to improve the efficiency of the power transmission. When the receiving coil is located external to the hermetic titanium enclosure, it is packaged in magnetically transparent materials such as polyurethane, silicone rubber, polysulfone, ceramic, glass, or biocompatible epoxy. IPG charging coils outside of the titanium enable faster charging at potentially greater depths. For midfield chargers, an RF antenna is positioned outside the titanium enclosure as well.
Other improvements have included battery chemistries which support charging at a faster C-rate without reducing the long-term battery performance or lifetime. In general, battery energy density and charge capacity has not increased every year in the same way semiconductor technology has miniaturized according to Moore's law. Looking forward, IPGs for SCS are unlikely to undergo significant miniaturization from rapid improvements in battery capacity [ ]. The header connection port volume is one potential area for size reduction, similar to pacemakers, which have adopted the newer 0.9 mm canted coil springs.
The transition to 2.4 GHz communication from the MICS band has also improved communication telemetry distance due to the higher regulated power levels in the 2.4 MHz ISM bands. Previous MICS devices required relatively close proximity due a 25 μW (−16 dbm) maximum transmit power, while 2.4 GHz connections can be performed from greater distances with transmit power as high as 0 dbm. Forward error correction methods can further improve range by 5 dB with reduced data rates. While the MICS radios previously provided the lowest energy communication available, numerous 2.4 GHz radios can be duty cycled to have a similar telemetry current consumption of approximately 1 μA quiescent current.
IPG recharge efficiency reduces and charging time increases significantly for deeper implant depths. The efficiency of recharging is impacted by whether the recharging coil is positioned in the header or inside the Titanium enclosure. Charging times can range from 0.5 to 3 h depending, with the fastest being from devices with charging coils on the outside of the hermetic enclosure. Recharging can be a significant burden for patient compliance, especially as high-frequency waveforms (1–50 kHz) consume significantly more battery life and require recharging every 1–2 days. Burst devices and tonic waveforms require far less energy and have a reduced patient recharging burden.
Materials that are implanted in the human body must be biocompatible and biostable for delivering stimulation for a duration of 5–10 years. Device manufacturers ensure that materials implanted in the body meet all required standards for implantable medical devices. International standards for biological evaluations of medical device materials include ISO 10993-1:2018 which outlines a set of comprehensive tests and protocols required for medical devices. The materials are categorized based on the duration of body contact and the type of body tissue that contact that the medical device. The standard outlines four types of body contact: noncontacting medical devices, surface-contacting devices, external communicating devices, and implanted devices.
Implanted medical devices are further defined based on the specific implantation locations of the device. These sites are categorized into two different groups: direct tissue/bone or blood contact. In addition to the site of the implant, the required tests also vary depending on the duration of the implant or contact. The standard also specifies tissue contact duration such as limited (less than 24 h), prolonged (24 h–30 days), or permanent (more than 30 days). Implanted neurostimulation devices have been evaluated by these biological tests including cytotoxicity, sensitization, irritation or intracutaneous reactivity, systemic toxicity, subacute and subchronic toxicity, genotoxicity, and hemocompatibility to ensure biocompatibility.
In addition to biocompatibility, the biostability of the materials and designs that are implanted is evaluated using other mechanical, environmental, and electrical safety standards. Biostability evaluation includes detailed mechanical, electrical, and chemical characterization of the material properties after being subjected to the human body for the defined exposure. Materials that are resistant to degradation and corrosion are key characteristics that the device manufacturers consider when selecting materials for chronic, implantable systems such as neurostimulation devices.
The materials of the implanted device that have direct tissue contact for permanent exposure periods include the device enclosure, device header and, with some designs, the recharge receiving antenna. Titanium is the most common material used for the hermetic package. It exhibits high levels of corrosion resistance, is nonmagnetic, lightweight, nontoxic and biologically compatible with human tissue and bone. Titanium also has excellent mechanical strength and durability characteristics. It is often formed into thin-walled halves that are seam-welded together to create the hermetic enclosure or by deep-drawn methods with a welded lid. Titanium has several implantable grades. Commercially pure titanium, such as Grade 1 or 2, is most commonly used. Commercially pure titanium has excellent formability and elongation which allows cold working and forming of custom device shapes and a relatively tight bend radius. Other titanium alloys, such as Grade 9 or 23, include other alloys such as aluminum or vanadium which increase the electrical resistivity of the material. This increase in electrical resistivity results in lower magnetic eddy current loss during inductive power transfer used with rechargeable systems. These alloys do not have the formability or elongation properties of commercially pure titanium which translates into larger bend radius constraints for the device form factor. However, the improved recharge performance allows the device to be implanted deeper.
Biocompatibility is considered a large risk where new materials are used. However, biocompatibility testing remains important to assess residuals associated with the manufacturing process even if all materials have known biocompatibility. Risk analysis should be performed according to ISO 10993-1:2018 to determine the risk of a particular device material or manufacturing process.
Multi-contact electrode systems provide the ability to steer current between multiple cathodes and returns using one or more electrodes on the lead. Modern IPGs can provide monopolar stimulation with the titanium hermetic package as a return common electrode. The titanium may also be connected as a low-impedance source to provide anodal intensification up to approximately 5% of the stimulation amplitude.
The electrical contacts in the device header are typically made from titanium, SS316L platinum, or platinum iridium alloy materials. Commonly used insulating materials include polyurethane, silicone rubber, tecothane, polysulfone, and biocompatible epoxy.
The implantable lead is the most important component of a therapy delivery system, as it directs stimulation energy into the neural tissue (e.g., brain, peripheral nerve, or spinal cord). The lead provides an electrical conduction pathway from the IPG to the therapy electrodes that are isolated from the environment of the body. Leads must be designed to conform to the surrounding anatomy to maximize electrical stimulation coupling to enable adequate modulation of neural tissue. Leads must also focus therapy to maximize the therapeutic window without causing off-target side effects from misplaced fields. In DBS for example, side effects can include impaired speech or motor function. In SCS, side effects include patient discomfort and reduction in the therapy window. Leads are also subject to the material biocompatibility and biostability requirements previously discussed. Additionally, the lead design should minimize the invasiveness of the procedure and should consider the potential of lead removal from the body without damage or disruption of neural tissue.
The lead may be connected directly to the neurostimulator and, in some cases, may be connected to an extension which bridges the connections between the neurostimulator and the lead. The lead or extension is secured to the neurostimulator connector using set screws or spring-lock mechanisms. It is important to establish a secure electrical connection between the lead and device header as improper connections may lead to increases in system impedance that may affect the therapy delivered. In addition, nonionic fluids should be used for wiping the lead, and connections should be dried since fluid in the connection may result in short circuit. A short circuit may cause stimulation at the connection site, intermittent, or loss of stimulation. Extensions are typically used between a DBS lead and the neurostimulator but may in turn affect MRI compatibility of the system. If the neurostimulator needs to be replaced due to infection, battery replacement, or other reasons, the extension may be disconnected from the neurostimulator without having to handle the previously implanted leads.
Implanted SCS for stimulating the dorsal columns have used 2–4 header ports and 16–32 therapy contacts to improve the spinal cord surface area covered by the electrodes. Devices such as the Medtronic Intellis employ 16 contacts, and the Boston Scientific Wavewriter provides 32 stimulation contacts using a variety of leads. Multiple types of lead extensions, splitters, and bifurcations exist for connecting different types of leads. For example, the Boston Scientific Infineon is a 16-conductor lead with 16 in-line contacts on the proximal end. To connect to an 8-contact IPG port, a splitter is used to convert to two 8-contact plugs.
Lead insulators are typically made out of a robust, biocompatible, and flexible material such as polyurethane, silicone, or silicone-urethane copolymers. The insulators can be multilumen with conductors in each lumen, or single lumen with coiled wires down the length of the lead. Coiled leads provide a stretchable lead which may provide greater long-term flex reliability.
Percutaneous SCS leads and DBS leads have cylindrical contacts to enable the lead to be inserted through a 4–5 french (1.5 mm) inner diameter needle and advanced in a nondamaging fashion. Stylets may be inserted into the bore of the lead to help steer it into position. The requirements for contact spacing and surface area vary between SCS and DBS with most leads providing between 8 and 16 cylindrical contacts for circumferential stimulation. The contacts of a percutaneous SCS lead may span from 25 to 78 mm to provide stimulation points over one to three vertebral levels. DBS leads normally have smaller contacts more tightly spaced to target small anatomical structures of the brain with finer granularity. The development of directional leads now reduces negative off-target stimulation of DBS leads.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here