Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
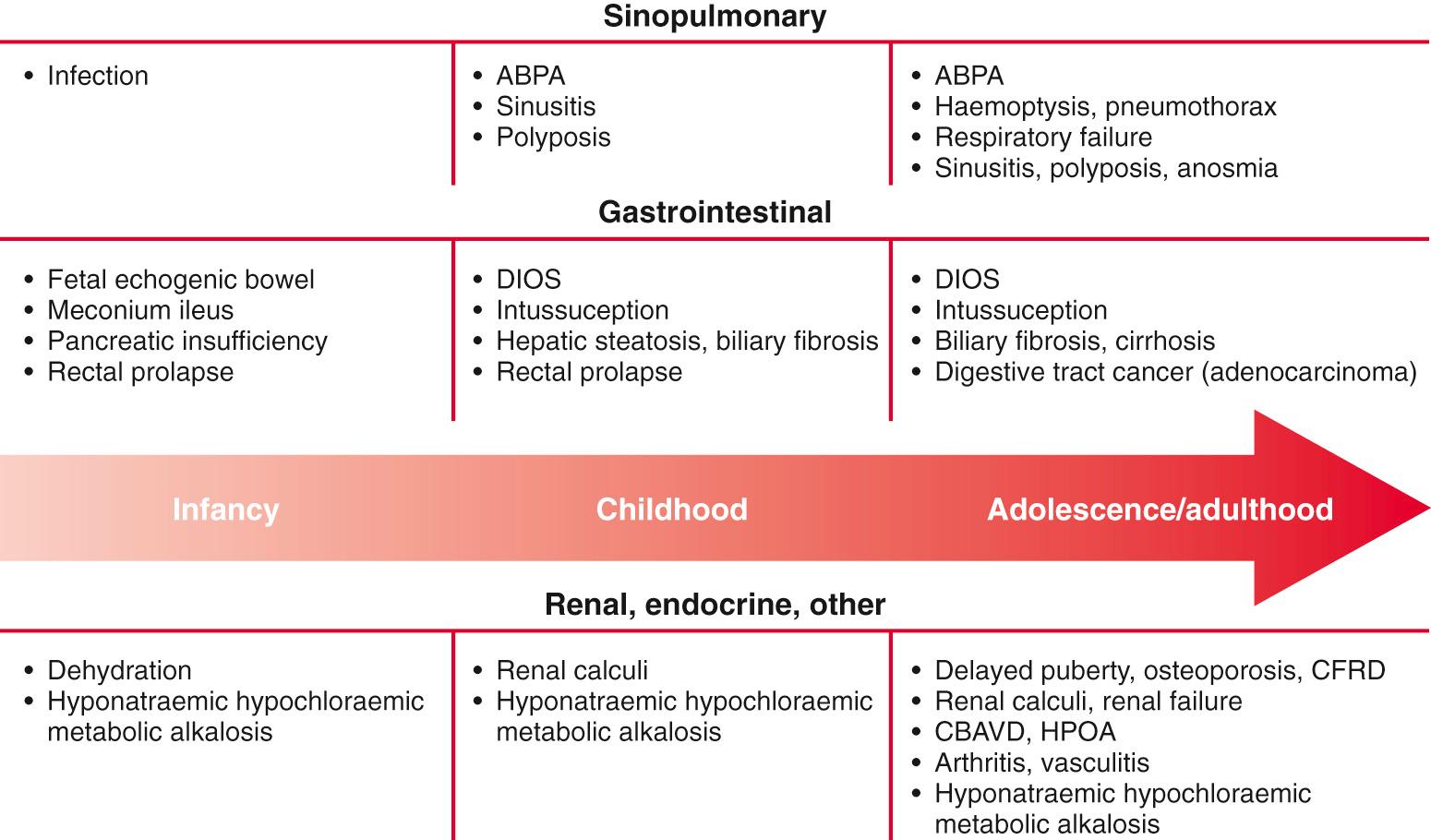
Cystic fibrosis (CF) is an inherited multisystem disorder of children and adults; it is the most common life-limiting recessive genetic trait among whites. Dysfunction of the cystic fibrosis transmembrane conductance regulator (CFTR) protein, the primary defect, leads to a wide and variable array of presenting manifestations and complications.
CF is responsible for most cases of exocrine pancreatic insufficiency in early life and is the major cause of severe chronic lung disease in children. It is also responsible for many cases of hyponatremic salt depletion, nasal polyposis, pansinusitis, rectal prolapse, pancreatitis, cholelithiasis, and nonautoimmune insulin-dependent hyperglycemia. Because CF may manifest as failure to thrive and hepatic dysfunction, including cirrhosis, this disorder enters into the differential diagnosis of many pediatric conditions ( Table 432.1 ).
RESPIRATORY
GASTROINTESTINAL
OTHER
|
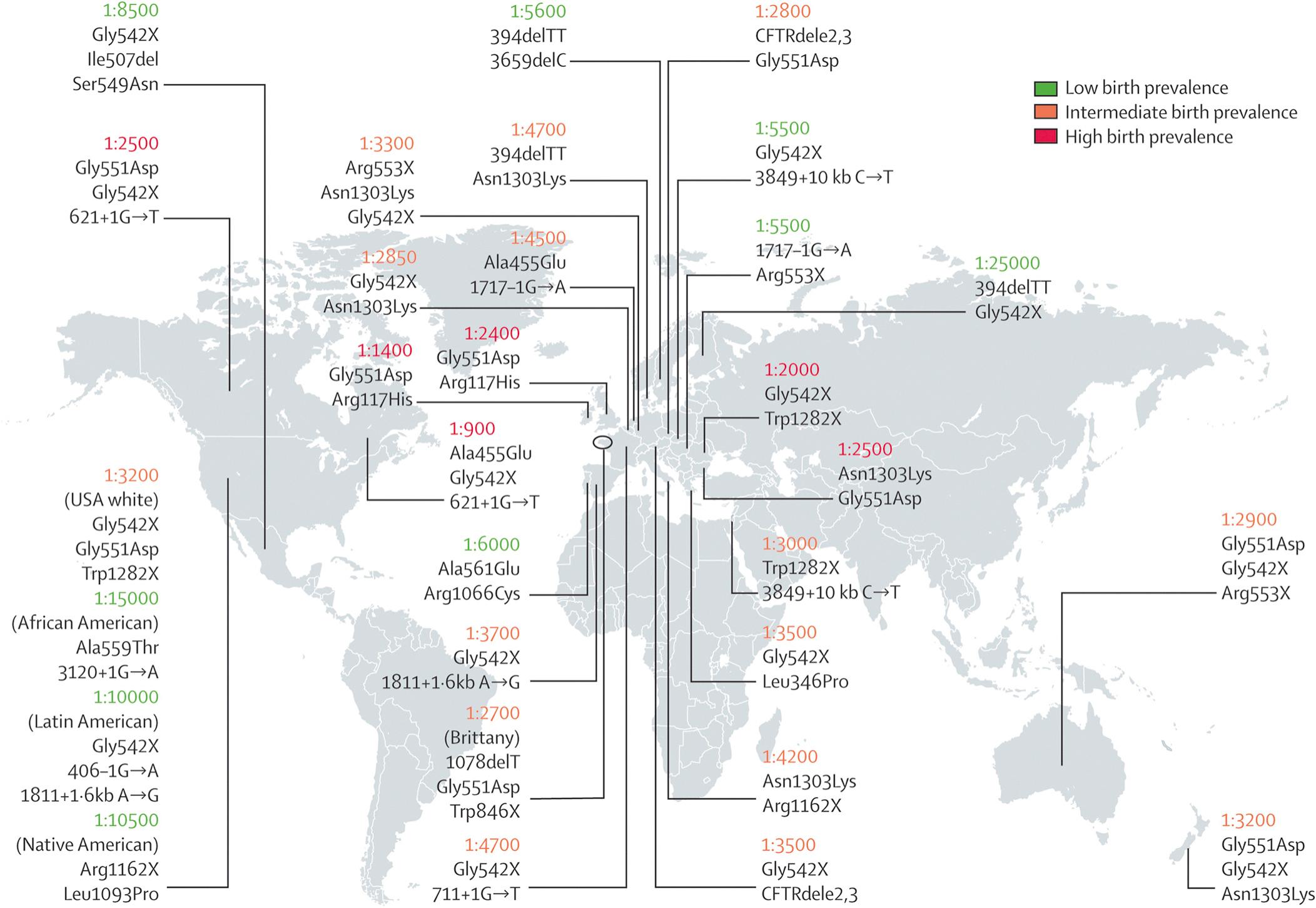
CF occurs most frequently in white populations of northern Europe, North America, and Australia/New Zealand. The prevalence in these populations varies but approximates 1 in 3,500 live births (1 in 9,200 individuals of Hispanic descent and 1 in 15,000 African Americans). Although less frequent in African, Hispanic, Middle Eastern, South Asian, and eastern Asian populations, the disorder does exist in these populations as well ( Fig. 432.1 ).
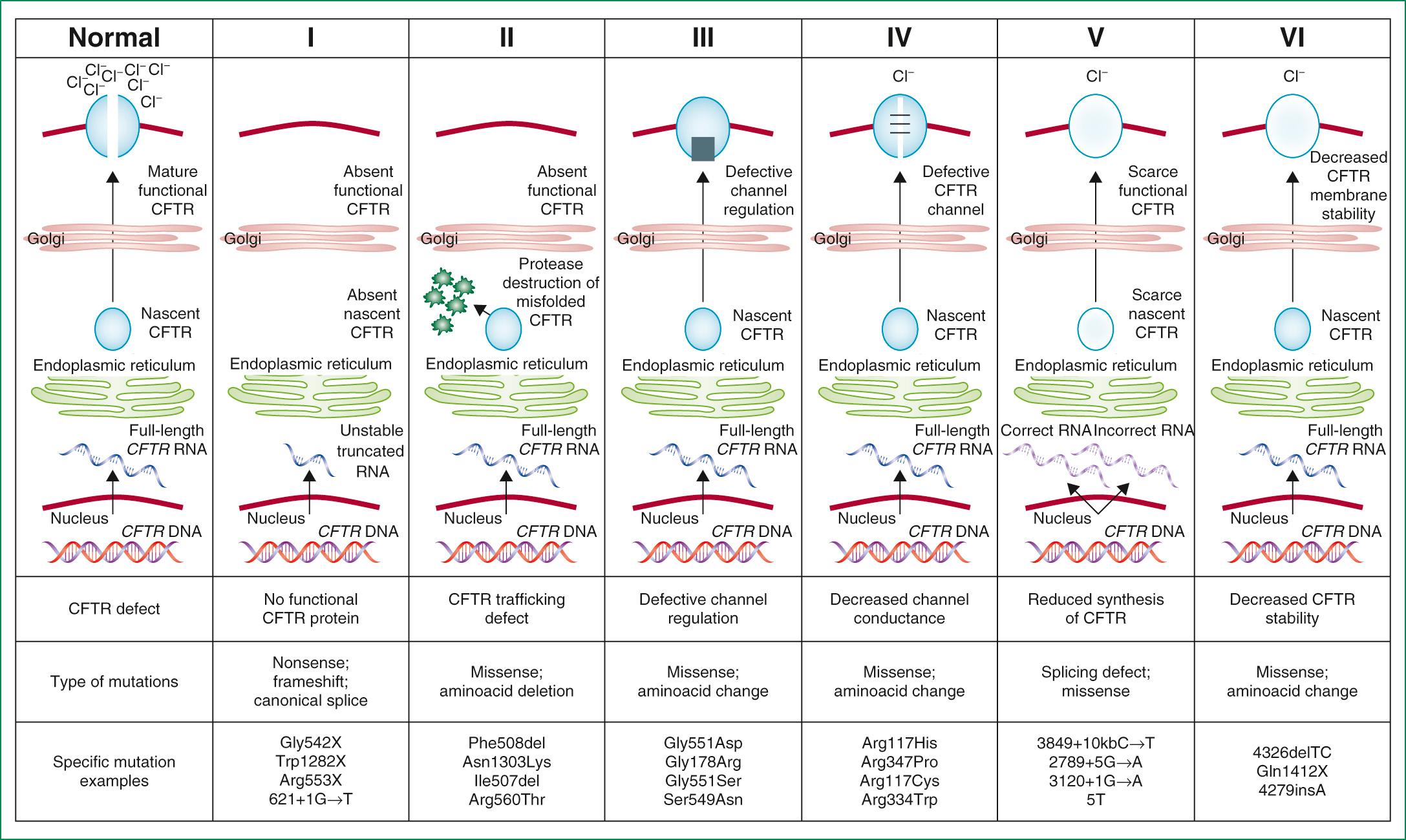
CF is inherited as an autosomal recessive trait. The CF gene codes for the CFTR protein, which is 1,480 amino acids . CFTR is expressed largely in epithelial cells of airways, the gastrointestinal tract (including the pancreas and biliary system), the sweat glands, and the genitourinary system. CFTR is a member of the adenosine triphosphate–binding cassette superfamily of proteins. It functions as a chloride channel and has other regulatory functions that are perturbed variably by the different mutations. More than 1,900 CFTR polymorphisms have been described, many of which are not clearly of clinical significance. Those that are associated with clinical manifestations may be grouped into 6 main classes based upon how they impact upon protein structure and function ( Table 432.2 ; Fig. 432.2 ). Mutation class I-III are generally considered to be severe mutations in that they lead to a complete or nearly complete absence of CFTR function, whereas class IV-VI mutations are associated with some residual functional protein. The most prevalent mutation of CFTR is the deletion of a single phenylalanine residue at amino acid 508 (F508del). This mutation is responsible for the high incidence of CF in northern European populations and is considerably less frequent in other populations, such as those of southern Europe and Israel. Nearly 50% of individuals with CF in the United States Cystic Fibrosis Foundation (CFF) Patient Registry are homozygous for F508del, and approximately 87% carry at least 1 F508del gene. Remaining patients have an extensive array of mutations, none of which has a prevalence of more than several percentage points, except in certain populations; for example, the W1282X mutation occurs in 60% of Ashkenazi Jews with CF. Through the use of probes for 40 of the most common mutations, the genotype of 80–90% of Americans with CF can be ascertained. Genotyping using a discreet panel of mutation probes is quick and less costly than more comprehensive sequencing and is the approach typically used in state newborn screening programs. In remaining patients, sequencing the entire CFTR gene and looking for deletions and duplications are necessary to establish the genotype. As sequencing technologies evolve and costs decrease, sequencing the entire CFTR gene may become mainstream for all patients.
| CLASS | EFFECT ON CFTR | FUNCTIONAL CFTR PRESENT? | SAMPLE MUTATIONS |
|---|---|---|---|
| I | Lack of protein production | No | Stop codons (designation in X; e.g., Trp1282X, Gly542X); splicing defects with no protein production (e.g., 711+1G→T, 1717-1G→A) |
| II | Defect in protein trafficking with ubiquitination and degradation in endoplasmic reticulum/Golgi body | No/substantially reduced | Phe508del, Asn1303Lys, Gly85Gly, leu1065Pro, Asp507, Ser549Arg |
| III | Defective regulation; CFTR not activated by adenosine triphosphate or cyclic adenosine monophosphate | No (nonfunction CFTR present in apical membrane) | Gly551Asp, Ser492Phe, Val520Phe, Arg553Gly, Arg560Thr, Arg560Ser |
| IV | Reduced chloride transport through CFTR at the apical membrane | Yes | Ala455Glu, Arg117Cys, Asp1152His, Leu227Arg, Arg334Trp, Arg117His * |
| V | Splicing defect with reduced production of CFTR | Yes | 3849+10kbC→T, 1811+16kbA→G, IVS8-5T, 2789+5G→A |
* Function of Arg117His depends on the length of the polythymidine track on the same chromosome in intron 8 (IVS8): 5T, 7T, or 9T. There is more normal CFTR function with a longer polythymidine track.
The relationship between CFTR genotype and clinical phenotype is highly complex. CFTR mutation class is strongly associated with pancreatic dysfunction and will usually predict this manifestation in any given patient. Respiratory complications and lung function decline are also correlated with mutation class severity but with greater variation due to the influence of non-CFTR modifier gene polymorphisms and environmental influences on the manifestations of lung disease in any one individual. Studies have identified specific non-CFTR modifier genes of importance; genome-wide association studies identified a polymorphism on chromosome 11 in the intergenic region between EHF (an epithelial transcription factor) and APIP (an inhibitor of apoptosis) that is associated with lung disease severity and may influence the expression of EHF and APIP, as well as other genes in the region, including PDHX , CD44 , and ELF5 . A region on chromosome 20 may also be found to relate to lung disease severity. This region encompasses several genes (MC3R, CASS4, AURKA) that may play a role in lung host defense involving neutrophil function, apoptosis, and phagocytosis. Genome-wide association studies analysis also identified genetic regions that predispose to risk for liver disease, CF-related diabetes, and meconium ileus.
The high-frequency of CFTR mutations has been ascribed to resistance to the morbidity and mortality associated with infectious dysenteries through the ages. Cultured CF intestinal epithelial cells homozygous for the F508del mutation are unresponsive to the secretory effects of cholera toxin. CFTR heterozygous mice experience less mortality when treated with cholera toxin than their unaffected wild-type littermates.
A number of long-standing observations of CF are of fundamental pathophysiologic importance; they include failure to clear mucous secretions, a paucity of water in mucous secretions, an elevated salt content of sweat and other serous secretions, and chronic infection limited to the respiratory tract. In addition, there is a greater negative potential difference across the respiratory epithelia of patients with CF than across the respiratory epithelia of control subjects. Aberrant electrical properties are also demonstrated for CF sweat gland duct and rectal epithelia. The membranes of CF epithelial cells are unable to secrete chloride or bicarbonate in response to cyclic adenosine monophosphate–mediated signals, and at least in the respiratory epithelial cells, excessive amounts of sodium are absorbed through these membranes. These defects can be traced to a dysfunction of CFTR. CFTR function is highly regulated and energy dependent; it requires both cyclic adenosine monophosphate–stimulated protein kinase A phosphorylation of the regulatory domain and ATP binding and hydrolysis at the nucleotide binding domains. CFTR also interacts with other ion channels, signal transduction proteins, and the cytoskeleton ( Fig. 432.3 and see Fig. 432.2 ).
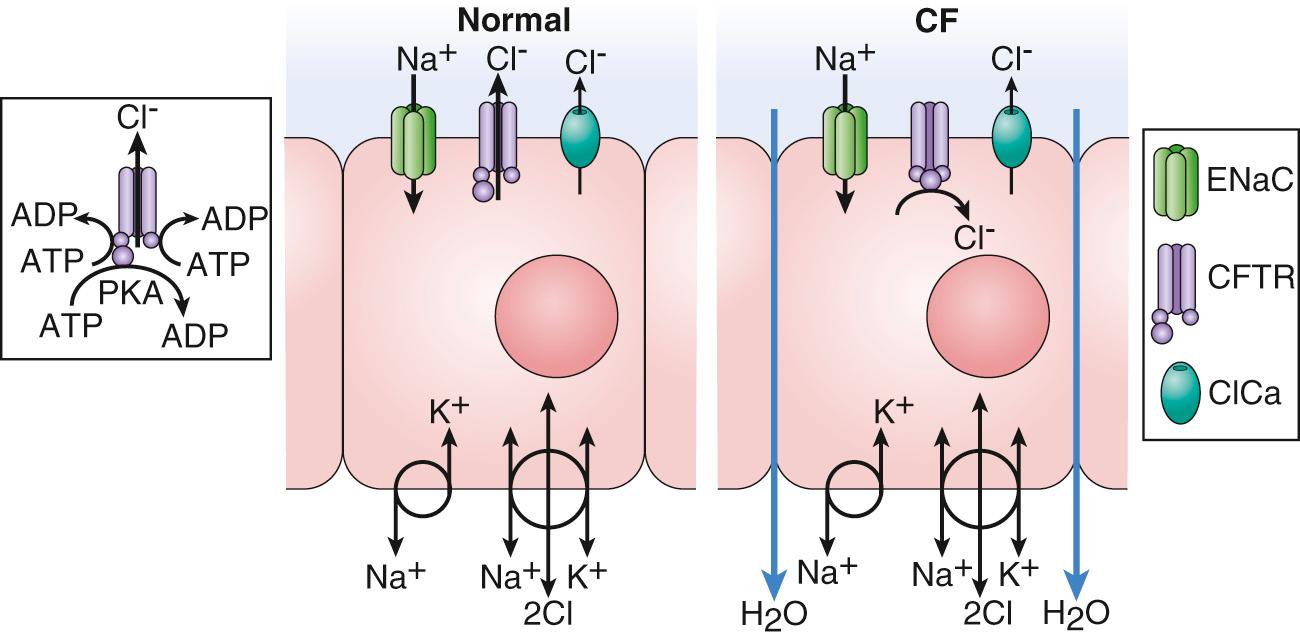
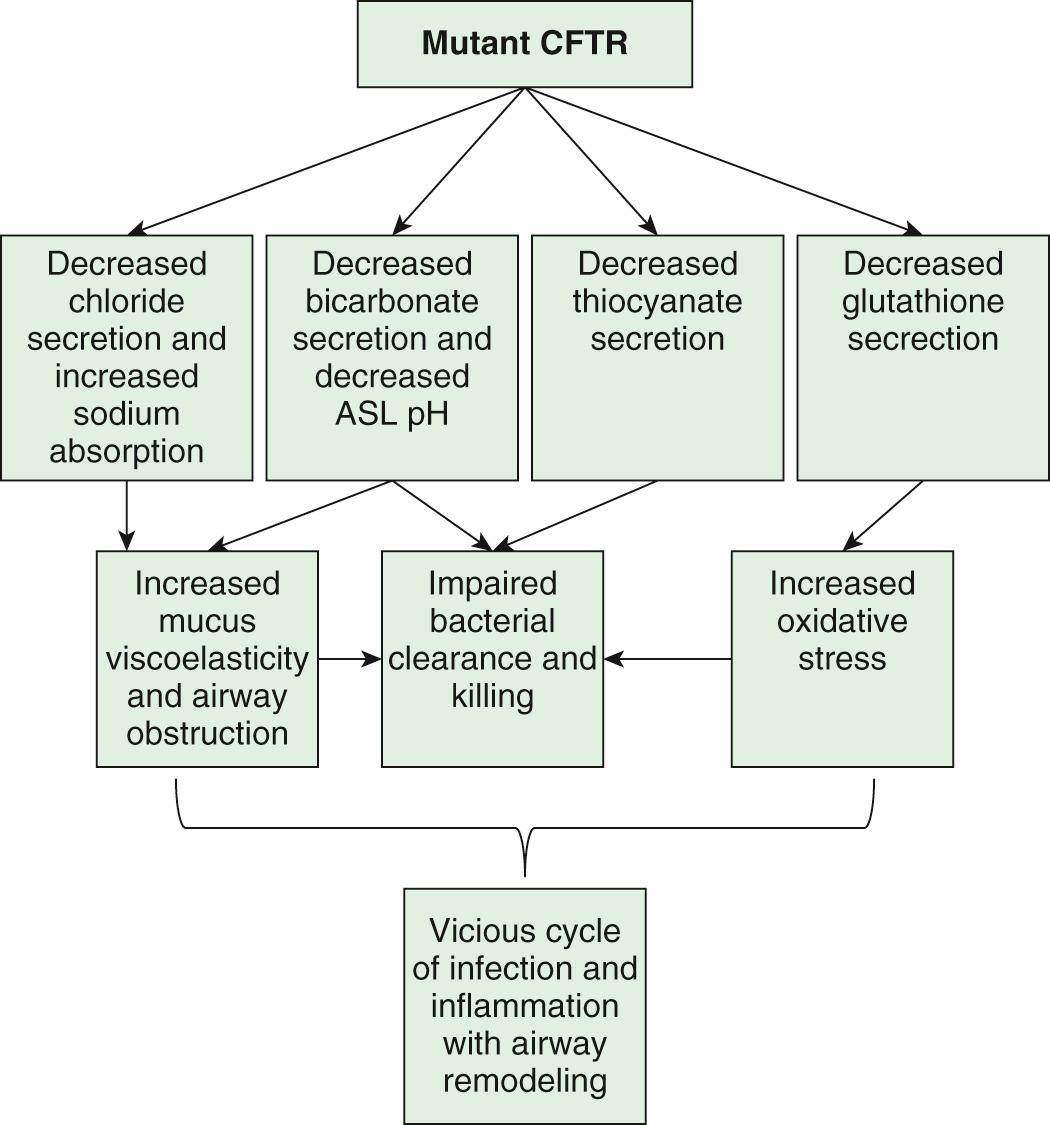
Many hypotheses have been postulated to explain how CFTR dysfunction results in the clinical phenotype ( Fig. 432.4 ). It is likely that no one hypothesis explains the full spectrum of disease. One model is that airway hydration homeostasis requires both CFTR and P2Y 2 -regulated calcium-activated chloride secretion. When extracellular ATP is depleted such as after viral infections, calcium-activated chloride secretion is not activated and the failure of mutant CFTR chloride secretion results in dehydrated airway secretions, increased concentration of mucin solids, and more viscoelastic mucus that is not cleared by normal mucociliary transport. Another mechanism that is supported by both primary human airway studies and investigations in the CF pig is that mutant CFTR causes failure of HCO 3 − secretion and a more acidic airway surface liquid, which increases mucous viscoelasticity resulting in poor mucociliary clearance. Mucous secretions are tethered to submucosal gland ducts and are retained and obstruct airways, starting with those of the smallest caliber, the bronchioles. Airflow obstruction at the level of small airways is the earliest observable physiologic abnormality of the respiratory system. CFTR dysfunction in airway smooth muscle has been implicated in tracheal and airway abnormalities in humans and in animal models of the disease (pig and mice). These data suggest that CFTR expression in this nonepithelial tissue contributes to airway constriction.
It is plausible that similar pathophysiologic events take place in the pancreatic and biliary ducts (and in the vas deferens), leading to desiccation of proteinaceous secretions and obstruction. Because the function of sweat gland duct cells is to absorb rather than secrete chloride, salt is not retrieved from the isotonic primary sweat as it is transported to the skin surface; chloride and sodium levels are consequently elevated.
Chronic infection in CF is limited to the airways. One explanation for infection is a sequence of events starting with failure to clear inhaled bacteria promptly and then proceeding to persistent infection and an inflammatory response in airway walls. Another explanation for early infection is the failure of innate immune proteins to kill bacteria in an abnormally acidic airway milieu. In addition, it has been proposed that abnormal CFTR creates a proinflammatory state or amplifies the inflammatory response to initial infections (viral or bacterial). Some investigators have identified primary differences in CF-affected immune cells (including macrophage, neutrophils, lymphocytes, and dendritic cells) and have suggested that these alterations contribute to this proinflammatory state as well as a dysregulated immune response. It appears that inflammatory events occur first in small airways, perhaps because it is more difficult to clear altered secretions and microorganisms from these regions. The agents of airway injury include neutrophil products, such as oxidative radicals and proteases, and immune reaction products. These inflammatory products further aggravate airway obstruction by increasing mucin secretion and altering mucin structure to promote both intramolecular and intermolecular interactions. Excessive inflammatory cell polymers in CF sputum, including DNA, filamentous actin, and glycosaminoglycans, further contribute to abnormal mucous viscoelastic properties and airway obstruction. Chronic bronchiolitis and bronchitis are the initial lung manifestations (see Chapter 418 ), but after months to years, structural changes in airway walls produce bronchiolectasis and bronchiectasis . With advanced lung disease, infection may extend to peribronchial lung parenchyma.
A central feature of lung disease in patients with CF is the high prevalence of airway infection with Staphylococcus aureus (see Chapter 208.1 ), Pseudomonas aeruginosa (see Chapter 232.1 ), and Burkholderia cepacia complex (see Chapter 232.2 ), organisms that rarely infect the lungs of other individuals. It has been postulated that the CF airway epithelial cells or surface liquids may provide a favorable environment for harboring these organisms. CF airway epithelium may be compromised in its innate defenses against these organisms, through either acquired or genetic alterations. Antimicrobial activity is diminished in CF secretions; this diminution may be related to hyperacidic surface liquids or other effects on innate immunity. Another puzzle is the propensity for P. aeruginosa to undergo mucoid transformation in the CF airways. The complex polysaccharide produced by these organisms generates a biofilm that provides a hypoxic environment and thereby protects Pseudomonas against antimicrobial agents.
Altered lipid homeostasis has been implicated as a predisposing factor for respiratory tract infection and inflammation. Concentrations of lipoxins—molecules that suppress neutrophilic inflammation—are suppressed in CF airways. There is an imbalance of lipids with increased arachidonic acid and decreased docosahexaenoic acid, which promotes inflammation. There is also an imbalance of ceramide in the CF airway that is proinflammatory. Supporting the idea that altered lipid uptake affects infection and inflammation is the observation that the 10–15% of individuals with CF who retain substantial exocrine pancreatic function have delayed acquisition of P. aeruginosa and slower deterioration of lung function. However, it appears that nutritional factors are contributory only because preservation of pancreatic function does not preclude development of typical lung disease.
The variation in progression of lung disease seen in patients with CF is largely influenced by social and physical environment factors, whose impact matches that of CFTR genotype. Exposure to environmental tobacco smoke and outdoor air pollutants, and early acquisition of respiratory virus infections, as well as pathogenic organisms like P. aeruginosa and methicillin-resistant S. aureus, have been implicated as causes of worsening disease. Sex/gender disparities also seem to exist, with females having a poorer prognosis. Although studies have suggested that estrogen may influence disease exacerbations, the gap seems to be narrowing in the past decade.
Although most CF care is delivered at specialty centers and is broadly influenced by current clinical guidelines, there is enough variability in treatment approaches to cause large variation in respiratory and nutritional outcomes across the care networks in both North America and Europe. Social determinants of health are associated with significant disparities in outcome; socioeconomic status has been shown to be a strong predictor of mortality, as well as both nutritional status and lung function on both sides of the Atlantic. The specific mechanism of effect is unclear, but evidence suggests a role for socioeconomic status–related differences in health behaviors and disease self-management practices, stress and mental health issues, and environmental tobacco smoke exposure. Differential access to specialty care and medications is not a major factor in North American children (lack of insurance in some adults is a problem); however, differences in disease outcomes across European countries of varying wealth are quite clear.
The earliest pathologic lesion in the lung is that of bronchiolitis (mucous plugging and an inflammatory response in the walls of the small airways); with time, mucous accumulation and inflammation extend to the larger airways ( bronchitis ) (see Chapter 418.2 ). Goblet cell hyperplasia and submucosal gland hypertrophy become prominent pathologic findings, which is most likely a response to chronic airway infection. Organisms appear to be confined to the endobronchial space; invasive bacterial infection is not characteristic. With long-standing disease, evidence of airway destruction such as bronchiolar obliteration, bronchiolectasis, and bronchiectasis (see Chapter 430 ) becomes prominent. Imaging modalities demonstrate both increased airway wall thickness and luminal cross-sectional area relatively early in lung disease evaluation. Bronchiectatic cysts and emphysematous bullae or subpleural blebs are frequent with advanced lung disease, the upper lobes being most commonly involved. These enlarged air spaces may rupture and cause pneumothorax. Interstitial disease is not a prominent feature, although areas of fibrosis appear eventually. Bronchial arteries are enlarged and tortuous, contributing to a propensity for hemoptysis in bronchiectatic airways. Small pulmonary arteries eventually display medial hypertrophy, which would be expected in secondary pulmonary hypertension.
The paranasal sinuses are uniformly filled with secretions containing inflammatory products, and the epithelial lining displays hyperplastic and hypertrophied secretory elements (see Chapter 408 ). Polypoid lesions within the sinuses and erosion of bone have been reported. The nasal mucosa may form large or multiple polyps , usually from a base surrounding the ostia of the maxillary and ethmoidal sinuses.
The pancreas is usually small, occasionally cystic, and often difficult to find at postmortem examination. The extent of involvement varies at birth. In infants, the acini and ducts are often distended and filled with eosinophilic material. In 85–90% of patients, the lesion progresses to complete or almost complete disruption of acini and replacement with fibrous tissue and fat. Infrequently, foci of calcification may be seen on radiographs of the abdomen. The islets of Langerhans contain normal-appearing β cells, although they may begin to show architectural disruption by fibrous tissue in the 2nd decade of life.
The intestinal tract shows only minimal changes. Esophageal and duodenal glands are often distended with mucous secretions. Concretions may form in the appendiceal lumen or cecum. Crypts of the appendix and rectum may be dilated and filled with secretions.
Focal biliary cirrhosis secondary to blockage of intrahepatic bile ducts is uncommon in early life, although it is responsible for occasional cases of prolonged neonatal jaundice. This lesion becomes much more prevalent and extensive with age and is found in 70% of patients at postmortem examination. This process can proceed to symptomatic multilobular biliary cirrhosis that has a distinctive pattern of large irregular parenchymal nodules and interspersed bands of fibrous tissue. Approximately 30–70% of patients have fatty infiltration of the liver, in some cases despite apparently adequate nutrition. At autopsy, hepatic congestion secondary to cor pulmonale is frequently observed. The gallbladder may be hypoplastic and filled with mucoid material and often contains stones. The epithelial lining often displays extensive mucous metaplasia. Atresia of the cystic duct and stenosis of the distal common bile duct have been observed.
Glands of the uterine cervix are distended with mucus, copious amounts of which collect in the cervical canal. In >95% of males, the body and tail of the epididymis, the vas deferens, and the seminal vesicles are obliterated or atretic, resulting in male infertility.
Since the universal adoption of CF newborn screening in the United States and overseas, as well as the evolution of aggressive and proactive treatment approaches, the clinical face of CF is very different from what it was in earlier decades. Diagnosis is typically accomplished before 1 mo of age, prior to any obvious clinical symptoms or signs, and treatment is targeted on immediately correcting nutritional deficiencies and delaying the respiratory complications of the disease. The interaction of mutational heterogeneity and environmental factors leads to highly variable involvement of the lungs, pancreas, and other organs. A summary of the time course of potential development of clinical manifestations is shown in Fig. 432.5 .
Infants diagnosed by CF newborn screening are generally asymptomatic from a respiratory standpoint. Nonetheless, the majority are infected with S. aureus , Haemophilus influenza , or even P. aeruginosa within the 1st mo of life, and chest CT scans show characteristic heterogeneous air trapping in ![]() of infants by their first birthday, and bronchiectasis is found in more than 10% of 1 yr olds and ∼60% of 5 yr olds. The earliest symptom is usually cough that may begin with a viral respiratory tract infection but then persists unless treated with antibiotics. With treatment, the generally realized goal is for patients to remain asymptomatic throughout childhood, except for the periodic development of cough, chest congestion, sputum production, and/or wheezing that define a pulmonary exacerbation .
of infants by their first birthday, and bronchiectasis is found in more than 10% of 1 yr olds and ∼60% of 5 yr olds. The earliest symptom is usually cough that may begin with a viral respiratory tract infection but then persists unless treated with antibiotics. With treatment, the generally realized goal is for patients to remain asymptomatic throughout childhood, except for the periodic development of cough, chest congestion, sputum production, and/or wheezing that define a pulmonary exacerbation .
The rate of progression of lung disease is the chief determinant of morbidity and mortality. As lung disease slowly progresses, chronic cough, sputum production, exercise intolerance, shortness of breath, and failure to thrive are noted. Cor pulmonale, respiratory failure, and death eventually supervene unless lung transplantation is accomplished; this has become increasingly uncommon in childhood. Infection with certain strains of B. cepacia and other multidrug-resistant organisms may be associated with particularly rapid pulmonary deterioration and death.
Eventual physical findings include increased anteroposterior diameter of the chest, generalized hyperresonance, scattered or localized coarse crackles, and digital clubbing. Expiratory wheezes may be heard, a manifestation of airway inflammation and edema that may or may not be associated with bronchodilator responsiveness. Cyanosis is a late sign. Common pulmonary complications include atelectasis, hemoptysis, pneumothorax, and cor pulmonale; these usually appear in late adolescence or beyond.
Even though the paranasal sinuses are virtually always opacified radiographically, acute sinusitis is infrequent. Nasal obstruction and rhinorrhea are common, caused by inflamed, swollen mucous membranes or, in some cases, nasal polyposis. Nasal polyps are most troublesome between 5 and 20 yr of age.
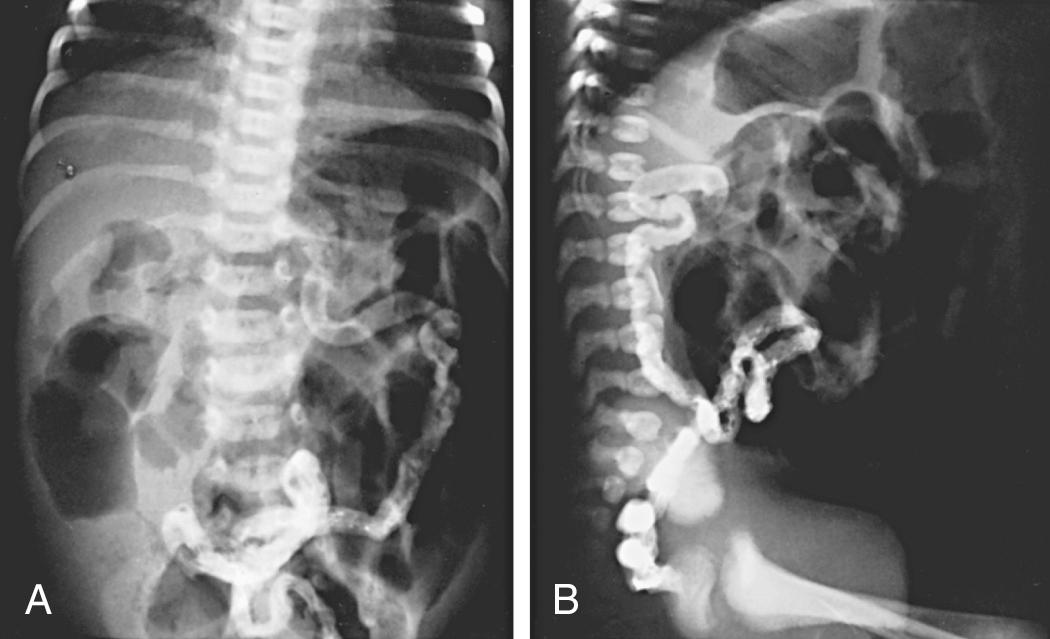
In 15–20% of newborn infants with CF, the ileum is completely obstructed by meconium ( meconium ileus ). The frequency is greater among siblings born subsequent to a child with meconium ileus and is particularly striking in monozygotic twins, reflecting a genetic contribution from one or more unknown modifying genes. Abdominal distention, emesis, and failure to pass meconium appear in the first 24-48 hr of life (see Chapters 123.1 and 356.2 ) and often requires surgical intervention. Abdominal radiographs ( Fig. 432.6 ) show dilated loops of bowel with air-fluid levels and, frequently, a collection of granular, “ground-glass” material in the lower central abdomen. Rarely, meconium peritonitis results from intrauterine rupture of the bowel wall and can be detected radiographically as the presence of peritoneal or scrotal calcifications.
Ileal obstruction with fecal material ( distal intestinal obstruction syndrome [DIOS] ) occurs in older children, causing cramping abdominal pain, abdominal distention, and obstruction that can be treated with medical approaches to bowel evacuation.
More than 85% of children with CF have exocrine pancreatic insufficiency, causing protein and fat malabsorption. Symptoms, if untreated, include frequent, bulky, greasy stools and failure to gain weight even when food intake appears to be large. Weight gain can be challenging, but attainment of normal growth and development is an expectation of treatment. A protuberant abdomen, decreased muscle mass, poor growth, and delayed maturation are classic and rarely seen physical signs. Excessive flatus may be a problem. Supplementation with fat-soluble vitamin preparations has made deficiencies of vitamin A, E, and K unusual, but vitamin D deficiency continues to be prevalent and, although rickets is rare, osteoporosis is common, especially in older patients and those with more severe lung disease. Class IV-VI mutations are associated with pancreatic sufficiency, but patients with these mutations are prone to pancreatitis when they reach adolescence.
Historically a relatively common event, rectal prolapse occurs much less frequently as the result of earlier diagnosis and initiation of pancreatic enzyme replacement therapy.
Infants may occasionally present with neonatal jaundice suggestive of biliary obstruction. Evidence for liver dysfunction is most often detected in the first 15 yr of life and can be found in up to 30% of individuals. Biliary cirrhosis becomes symptomatic in only 5–7% of patients. Manifestations can include icterus, ascites, hematemesis from esophageal varices, and evidence of hypersplenism. Biliary colic secondary to cholelithiasis may occur in the 2nd decade or later. Liver disease occurs independent of genotype but is associated with meconium ileus and pancreatic insufficiency.
Endocrine pancreatic insufficiency tends to develop in the 2nd decade and beyond and is more common in patients with a family history of type II diabetes mellitus. It most commonly begins with postprandial hyperglycemia and may or may not be accompanied by weight loss or flattening weight gain. Fasting hyperglycemia and elevated hemoglobin A 1c are later manifestations. Ketoacidosis usually does not occur, but eye, kidney, and other vascular complications have been noted in patients living ≥10 yr after the onset of hyperglycemia. Recurrent, acute pancreatitis occurs occasionally in individuals who have residual exocrine pancreatic function and may be the sole manifestation of homozygotic CFTR mutations.
Virtually all males are azoospermic because of failure of development of wolffian duct structures, but sexual function is generally unimpaired. The female fertility rate is diminished, especially in women who have poor nutrition or advanced lung disease. Pregnancy is generally tolerated well by women with good pulmonary function but may accelerate pulmonary progression in those with advanced lung problems and may lead to glucose intolerance. Urinary incontinence associated with cough occurs in 18–47% of female children and adolescents.
Excessive loss of salt in the sweat predisposes young children to salt depletion episodes, especially during episodes of gastroenteritis and during warm weather. These children may present with hypochloremic alkalosis. Hyponatremia is a risk particularly in warm climates. Frequently, parents notice salt frosting of the skin or a salty taste when they kiss the child. A few genotypes are associated with normal sweat chloride values.
The diagnosis of CF has been based on a positive quantitative sweat test (Cl − ≥ 60 mEq/L) in conjunction with one or more of the following features: identification of 2 CFTR mutations, typical chronic obstructive pulmonary disease, documented exocrine pancreatic insufficiency, and a positive family history. With newborn screening, diagnosis is often made prior to obvious clinical manifestations such as failure to thrive and chronic cough. Diagnostic criteria have been recommended to include additional testing procedures ( Table 432.3 ).
| Presence of typical clinical features (respiratory, gastrointestinal, or genitourinary) |
| or |
| A history of CF in a sibling |
| or |
| A positive newborn screening test |
| plus |
| Laboratory evidence for CFTR (CF transmembrane regulator) dysfunction: |
| Two elevated sweat chloride concentrations obtained on separate days |
| or |
| Identification of two CF mutations |
| or |
| An abnormal nasal potential difference measurement |
The sweat test, which involves using pilocarpine iontophoresis to collect sweat and performing chemical analysis of its chloride content, is the standard approach to diagnosis of CF. The procedure requires care and accuracy. An electric current is used to carry pilocarpine into the skin of the forearm and locally stimulate the sweat glands. If an adequate amount of sweat is collected, the specimens are analyzed for chloride concentration. Infants with a positive newborn screen for CF should have the sweat chloride testing performed after 36-wk corrected gestational age and at a weight greater than 2 kg and at age greater than 10 days to increase the likelihood of sufficient sweat collection for an accurate study. Positive results should be confirmed; for a negative result, the test should be repeated if suspicion of the diagnosis remains.
More than 60 mmol/L of chloride in sweat is diagnostic of CF when one or more other criteria are present. In individuals with a positive newborn screen, a sweat chloride level less than 30 mmol/L indicates that CF is unlikely. Borderline (or intermediate) values of 30-59 mmol/L have been reported in patients of all ages who have CF with atypical involvement and require further testing. Table 432.4 lists the conditions associated with false-negative and false-positive sweat test results.
WITH FALSE-POSITIVE RESULTS
WITH FALSE-NEGATIVE RESULTS
|
Several commercial laboratories test for 30-96 of the most common CFTR mutations. This testing identifies ≥90% of individuals who carry 2 CF mutations. Some children with typical CF manifestations are found to have 1 or no detectable mutations by this methodology. Some laboratories perform comprehensive mutation analysis screening for all the >1,900 identified mutations.
The finding of increased potential differences across nasal epithelium (nasal potential difference) that is the increased voltage response to topical amiloride application, followed by the absence of a voltage response to a β-adrenergic agonist, has been used to confirm the diagnosis of CF in patients with equivocal or frankly normal sweat chloride values. This testing is primarily used in research applications and has never undergone extensive validation as a clinical tool.
The diagnosis of pancreatic malabsorption can be made by the quantification of elastase-1 activity in a fresh stool sample by an enzyme-linked immunosorbent assay specific for human elastase. The quantification of fat malabsorption with a 72-hr stool collection is rarely necessary in the clinical setting. CF-related diabetes affects approximately 20% of adolescents and 40–50% of adults, and clinical guidelines recommend yearly oral glucose tolerance testing (OGTT) after age 10. OGTT may sometimes be clinically indicated at an earlier age. Spot testing of blood and urine glucose levels and glycosylated hemoglobin levels are not sufficiently sensitive.
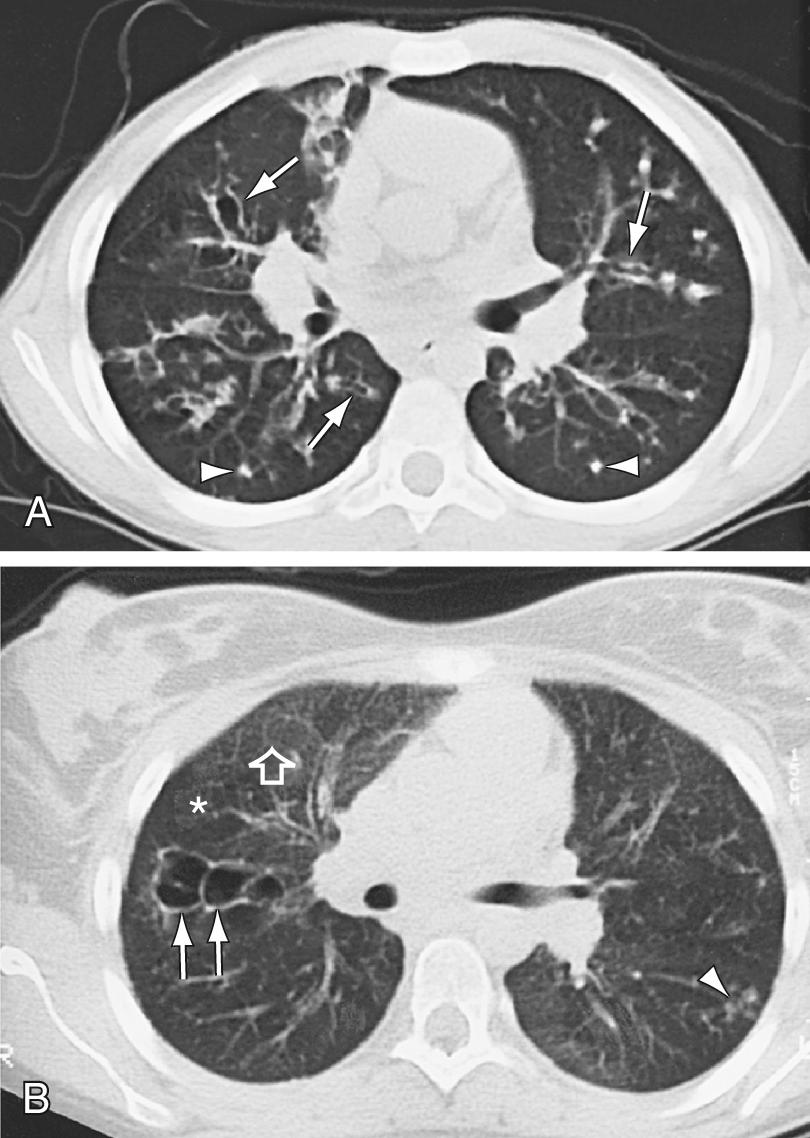
Hyperinflation of lungs occurs early and is often accompanied by nonspecific peribronchial thickening ( Fig. 432.7 ). Bronchial thickening and plugging and ring shadows suggesting bronchiectasis usually appear first in the upper lobes. Nodular densities, patchy atelectasis, and confluent infiltrate follow. Hilar lymph nodes may be prominent. With advanced disease, impressive hyperinflation with markedly depressed diaphragms, anterior bowing of the sternum, and a narrow cardiac shadow are noted. Cyst formation, extensive bronchiectasis, dilated pulmonary artery segments, and segmental or lobar atelectasis is often apparent with advanced disease. Most CF centers obtain chest radiographs (posteroanterior [PA] and lateral) at least annually. Standardized scoring of radiologic changes has been used to follow progression of lung disease. CT of the chest can detect heterogeneous hyperinflation and localized thickening of bronchial airway walls, mucous plugging, focal hyperinflation, and early bronchiectasis ( Fig. 432.8 ). CT abnormalities are commonly seen at a young age, even in asymptomatic children with normal lung function.

Radiographs of paranasal sinuses reveal panopacification and, often, failure of frontal sinus development. CT provides better resolution of sinus changes if this information is required clinically. Fetal ultrasonography may show pancreatic changes indicative of CF and suggest ileal obstruction with meconium early in the second trimester, but this finding is not predictive of meconium ileus at birth.
Infant pulmonary function testing is done routinely for clinical evaluation at a few CF centers but, given its complexity and the need for sedation, for the most part it is reserved for research protocols. Lung clearance index (LCI) measured by multiple breath washout can be done in infants and young children and is a sensitive measure of ventilation inhomogeneity caused by small airways disease. Currently it is primarily used for research, but given its ease and applicability it may be adopted as a standard monitoring tool in the future as CF care centers become more accustomed to its use.
Standard pulmonary function studies are usually obtained starting at about 4 yr of age and are routinely done by age 6. Forced expiratory volume in 1 sec (FEV 1 ) is the measurement that has been shown to correlate most closely with mortality and shows a gradual decline averaging 2–3% per year throughout childhood. Although a small number of children may already show evidence of airway obstruction by age 6, trends over the past several decades, as reported by the CFF patient registry, show a steady improvement in average FEV1 of the CF population, and as of 2015 ∼75% had normal or near-normal lung function at age 18 yr. Residual volume and functional residual capacity are increased early in the course of lung disease and are the cause of decreasing forced vital capacity (FVC) measurement. Restrictive changes, characterized by declining total lung capacity and vital capacity, correlate with extensive lung injury and fibrosis and are a late finding. Testing at each clinic visit is recommended to evaluate the course of the pulmonary involvement and allow for early intervention when clinically significant decrements are documented—this is probably the most sensitive indicator of a pulmonary exacerbation that should be treated with systemic antibiotics.
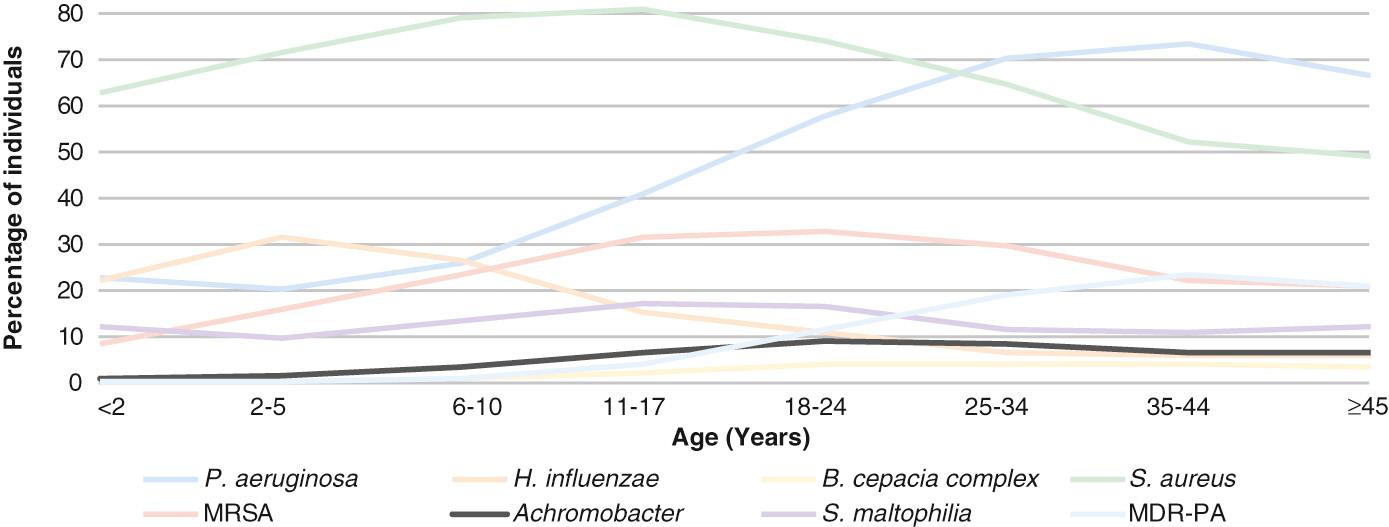
H. influenza and S. aureus are the most common organisms recovered in young children ( Fig. 432.9 ). Pseudomonas may be acquired early and is eventually an organism of key significance. P. aeruginosa appears to have a special propensity for the CF airway and over time characteristically develops a biofilm associated with a mucoid appearance in the microbiology lab and which correlates with more rapid progression of lung disease. Once P. aeruginosa develops a mucoid phenotype, it is extremely difficult to eradicate from the airway. A wide range of other organisms are frequently recovered, particularly in advanced lung disease; they include a variety of Gram-negative rods including the Burkholderia cepacia complex, which may be associated with a fulminant downhill course (the cepacia syndrome); Stenotrophomonas maltophilia , and Achromobacter xylosoxidans; assorted fungi, especially Aspergillus fumigatus , which is most important due to the relatively common development of allergic bronchopulmonary aspergillosis ; and nontuberculous mycobacterial species, especially Mycobacterium avium complex and Mycobacterium abscessus . Airway cultures are obtained regularly, most typically using oropharyngeal swabs in young children, and then sputum (which may be induced) in older children capable of expectoration. Oropharyngeal swabs typically give a good indication of the lower airway flora, but fiberoptic bronchoscopy may be used to gather lower respiratory tract secretions of infants and young children who do not expectorate if there is a concern for false-negative cultures, especially regarding the presence of P. aeruginosa .
The CF airway microbiome consists of a large number of additional organisms, especially anaerobes that are identified through antigen detection but not culture methods. The significance of this finding and its therapeutic implications remain somewhat unclear, but it has long been appreciated that response to antibiotic treatment of pulmonary exacerbations is not always predictable based upon culture and sensitivity of airway cultures.
Newborn screening for CF is mandated in all 50 states and is the most common way that CF is diagnosed. A variety of newborn screening algorithms are in place to identify infants with CF. Most algorithms use a combination of immunoreactive trypsinogen (IRT) results and limited DNA testing on blood spots; because not all mutations can be found using this approach, babies with an elevated IRT and a single detected mutation are considered a positive screen, and all positive screens are followed by a confirmatory sweat analysis. Depending upon race and ethnicity, about 10–15% of infants with a positive screen based on the finding of only 1 CF mutation will be found to have CF. This screening test is ≈95% sensitive and should result in a median age at diagnosis of less than 1 mo. Newborn diagnoses can prevent early nutritional deficiencies and improve long-term growth and may improve cognitive function. Importantly, good nutritional status (50 percentile weight for length or 50 percentile body mass index) is associated with better lung function at 6 yr of age.
An occasional patient may be missed by newborn screening, and those caring for adolescents and adults need to be aware that most of those older patients were not screened at birth and may present at later ages, into late adulthood. Prior to the advent of newborn screening, infants and children commonly presented with malabsorption and failure to thrive, in addition to respiratory symptoms. Most older patients whose diagnosis was missed early in life will have unusual class IV, V, or VI mutations and therefore normal pancreatic function. They will more typically present with chronic productive cough due to either bronchitis or chronic sinusitis and may have nasal polyps or allergic bronchopulmonary aspergillosis or unexplained bronchiectasis. The most common nonrespiratory manifestations will be congenital bilateral absence of the vas deferens (CBAVD) (in males) or recurrent pancreatitis. It is important to recognize that sweat testing at an adept lab (typically limited to CF Foundation accredited care centers) is the most accurate way to diagnose CF in this group. CFTR mutation testing with standard panels is never as sensitive as sweat testing and will frequently miss the unusual mutations that are seen more commonly in people who present late in this manner.
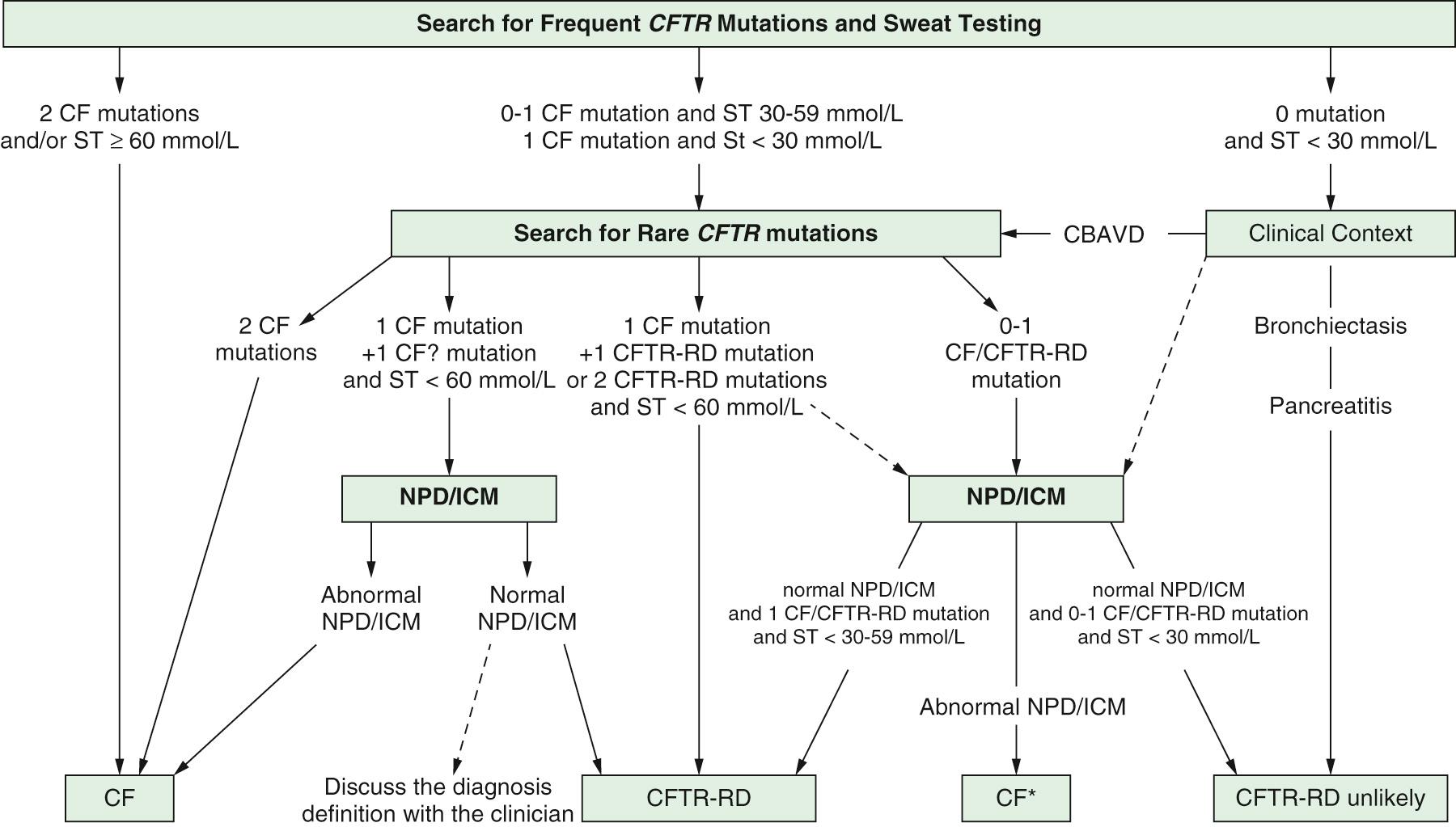
There is a subset of infants with a positive newborn screen for CF who have a nondiagnostic sweat chloride (30-59 mmol/L) and/or 1 or 2 CFTR mutations that is not clearly disease causing. These infants have CFTR - related metabolic syndrome (CRMS) (also called CFTR-related disease) and should be followed in a CF center closely through the 1st yr and then annually to evaluate them for the development of CF symptoms. Indeed, in some (∼10%) patients, the sweat test becomes clearly abnormal over time and they can be diagnosed as having CF. Because CRMS is a condition defined by asymptomatic detection in the context of newborn screening and CF newborn screening has been commonly performed only in the past decade or so, it is not clear whether some children in this group will eventually develop manifestations of CFTR-related disorder, such as CBAVD, chronic sinusitis, recurrent pancreatitis, or even bronchiectasis. An approach to the evaluation of patients with CRMS is seen in Fig. 432.10 .
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here