Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Surgical treatment of high-grade gliomas has been a challenge for neurosurgeons since the early days of our specialty with Harvey Cushing and Walter Dandy. Dandy developed the hemispherectomy to treat patients with invasive high-grade gliomas and observed they still succumbed to their disease. Despite his failure to find a cure, one patient did live an astounding 3.5 years after surgery. Unfortunately, almost 90 years after Dandy’s development of the hemispherectomy, the impact of surgery on survival for high-grade glioma patients remains limited.
With more than 23,000 new malignant gliomas diagnosed in the United States a year, and more than half of them glioblastoma, development of effective treatments remains a priority due to the devastation this disease confers on patients and their families.
Over the past decade there have been advancements in the molecular classification of central nervous system tumors. The World Health Organization (WHO) has recently published an update to the grading and classification of brain tumors that for the first time included molecular characteristics. In this update the WHO has included the characterization of isocitrate dehydrogenase (IDH) mutational status as a criterion for classifying high-grade gliomas. WHO grade III and IV diffuse astrocytic and oligodendroglial high-grade tumors now include: anaplastic astrocytoma, IDH-mutant (grade III); anaplastic oligodendroglioma, IDH-mutant and 1p/19q-codeleted (grade III); anaplastic pleomorphic xanthoastrocytoma (grade III); glioblastoma, IDH-wildtype (grade IV); glioblastoma, IDH-mutant (grade IV); and diffuse midline glioma, H3 K27M-mutant (grade IV). Yan and colleagues reported longer median survival in patients with anaplastic astrocytoma or glioblastoma when the tumor harbored either an IDH1 or IDH2 mutation. In the anaplastic astrocytoma patient population, the median survival for IDH mutant patients was 65 months versus 20 months in the wild-type group. In the glioblastoma patient population, the median survival for IDH mutant patients was 31 months versus 15 months for the wild-type group. In addition to age, duration of symptoms, and neurological status at presentation, molecular characterizations of high-grade gliomas and their impact on patient prognosis are considered when evaluating treatment options.
Standard treatment for high-grade gliomas currently consists of surgery, radiation, and medical therapy. Here, we focus on the role of surgery in the treatment of high-grade gliomas at initial diagnosis and at the time of recurrence.
Patients with high-grade gliomas present with a variety of symptoms, including headaches, seizures, cognitive/psychiatric dysfunction, sensorimotor dysfunction, language impairments, visual changes, and gait disturbances. Many of these symptoms may be associated with a variety of etiologies other than a brain tumor. In a systematic review and meta-analysis where magnetic resonance imaging (MRI) of the brain was done for headaches, only 0.7% of 19,559 patients had brain tumors. In patients that have brain tumors, headaches are the presenting symptom in about 25%. , Seizures are also a common presenting symptom, particularly for tumors near the motor cortex or temporal lobes. About 29% to 49% of all of those with glioblastomas have seizures at some point during the course of their disease. , Cognitive dysfunction is another significant finding, present in up to 90% of patients with preoperative cognitive testing. Overall symptoms of high-grade gliomas are varied, some requiring medical treatment preoperatively while others are best relieved by tumor resection.
Preoperative management of cerebral edema and seizures are important for high-grade gliomas. Dexamethasone has been the primary treatment of cerebral edema since the early 1960s. How much and how long to use steroids is varied. Recently it has been shown that independent of common side effects of steroids, patients with glioblastomas had a worse overall survival if they were on dexamethasone at the initiation of radiotherapy. This data was complemented by genetic data that showed down-regulation of 19 genes by dexamethasone, all cell-cycle related. We do not initiate steroids on a routine basis in newly diagnosed tumor patients unless they are symptomatic from their cerebral edema. If symptomatic, they will be started on dexamethasone 4 mg four times daily. Intraoperatively, patients are usually given dexamethasone 10 mg intravenously prior to the start of surgery. Postoperatively the goal is for a dexamethasone taper over 1 week if the patient’s symptoms can tolerate it.
Preoperative treatment of high-grade gliomas and other brain tumors with prophylactic antiepileptic medications has been studied in many randomized controlled clinical trials. In the literature, the frequency of seizures in brain tumor patients varies widely. Some report 20% to 45% in all brain tumors, 15% to 50% in patients undergoing surgery for brain tumors, 60% to 100% in low-grade gliomas, and 40% to 60% in high-grade gliomas. The chronology of seizures in patients with brain tumors postoperatively is usually divided into immediate (24 hours), early (1 week), and late (>1 week). A majority of seizures in patients undergoing craniotomy occurs within the first 72 hours postsurgery; however, this was not specific to brain tumor patients only.
The most classically used AEDs have been phenytoin, valproic acid, phenobarbital, and other older-generation medications. Over the years they have fallen out of favor for first-line prophylactic treatment due to their cytochrome P450 induction capability, which may interfere with levels of antacids and dexamethasone. In a study comparing patients with glioblastoma treated with P450-inducing AEDs compared to non-P450-inducing AEDs, the patients treated with non-P450-inducing AEDs had a longer survival:13.9 months compared to 10.8 months. Efficacy of these AEDs has also been called into question. Multiple meta-analyses have been done in patients with brain tumors receiving phenobarbital, phenytoin, or valproic acid that showed no efficacy in reducing overall seizure risk or seizures in the early or late period. Two of these meta-analyses found rates of mostly minor adverse events to be 24% and 15%. ,
Today newer AEDs, such as levetiracetam, are preferred due to their favorable side-effect profiles, limited impact on protein binding, lack of P450 enzymatic activity, renal metabolism, and no therapeutic level monitoring. In one study looking at the use of levetiracetam in newly diagnosed glioma patients with epilepsy (88% were high-grade), 45% of the high-grade tumor patients had seizures and were treated with levetiracetam starting at a dose of 1500 to 3000 mg/day. Eighty-eight percent of the high-grade glioma patients with seizures were seizure-free on levetiracetam with follow-up of 10 to 35 months. With the limited literature available on the prophylaxis or treatment of seizures related to brain tumors, levetiracetam may prove efficacious with minimal side effects or interactions with chemotherapeutics.
The most important questions to ask are: How effective are current AED treatments for preventing seizures, what side-effects do they have, and, if efficacious at preventing seizures, what duration of treatment should be employed? Current data suggest that prophylactic or therapeutic treatment of brain tumor patients with older-generation AEDs is not recommended due to their potential adverse effects on outcome and side-effect profiles. , , , The most promising prophylaxis and treatment of tumor-related seizures are newer-generation AEDs including levetiracetam, although their efficacy has yet to be determined in rigorous randomized controlled trials. The practice at our institution is prophylactic treatment of high-grade gliomas with levetiracetam and cessation of therapy by 4 weeks after surgery. It is also our first-line therapy in patient with brain tumors who present with seizures.
Preoperative imaging in patients with high-grade gliomas is a must for establishing a proper differential diagnosis and surgical planning with the ultimate goal of safe surgical treatment. Since its introduction, MRI has been the main imaging tool for brain tumor evaluation. Consensus recommendations agree that a standard brain tumor MRI protocol include the following sequences on a 1.5 tesla imaging system: 3D T1 weighted precontrast, axial 2D fluid-attenuated inversion recovery (FLAIR), axial 2D diffusion-weight imaging (DWI), axial 2D T2 weight noncontrast, and 3D T1 weighted postcontrast. Each imaging sequence has its own utility in making a differential diagnosis and in operative planning ( Fig. 7.1 ).
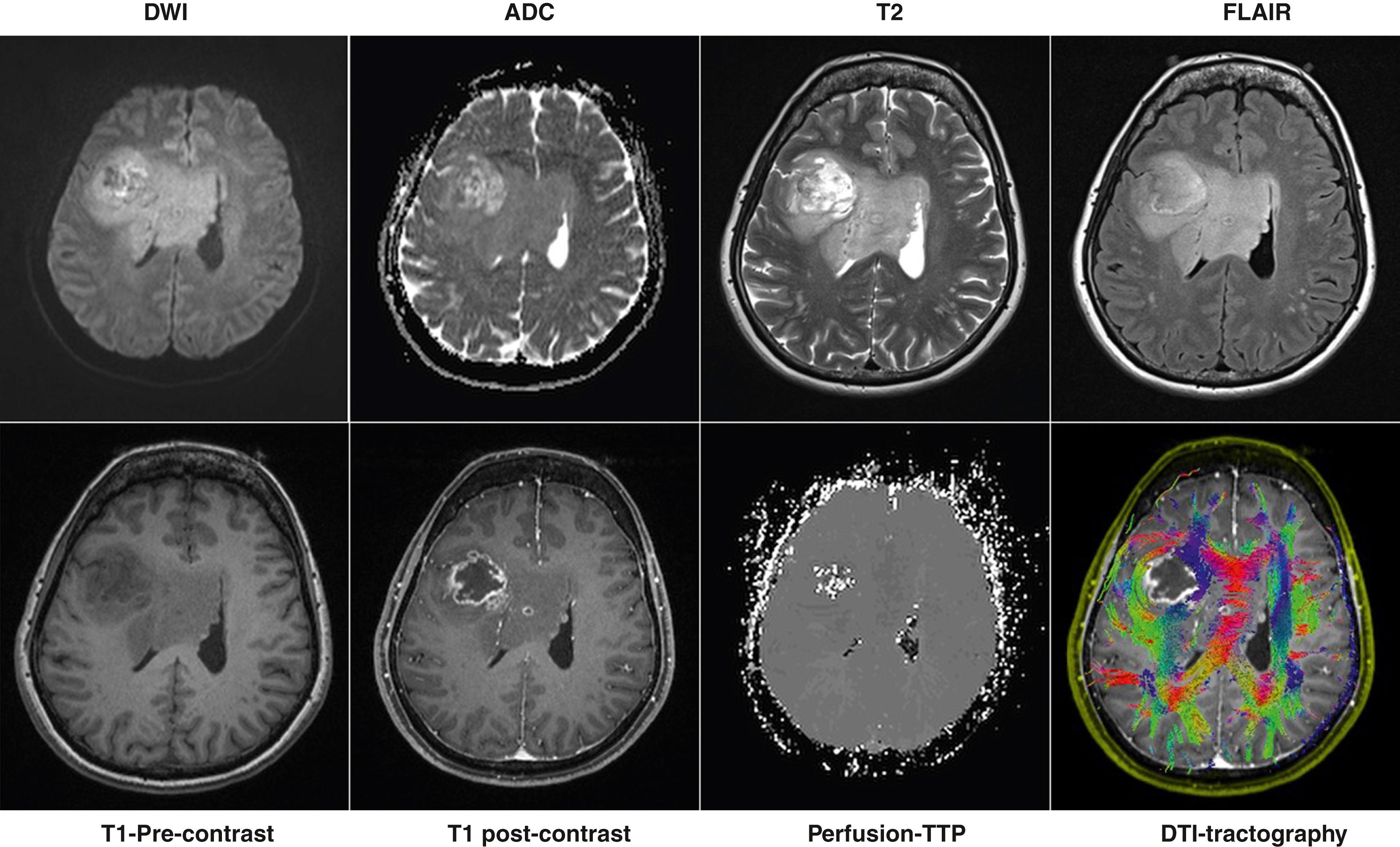
Normal and abnormal anatomical tissue architecture is best delineated by T1 weighted precontrast and postcontrast with gadolinium and T2 weighted imaging sequences. Gadolinium-enhancing tissue is indicative of breakdown in the normal blood-brain barrier (BBB), which is seen in most high-grade gliomas. , T1 weighted postcontrast and T2 weighted images are very useful in operative decision-making, as extent of safe resection can be estimated, which has implications for morbidity and survival outcomes. T2 weighted FLAIR sequence is mostly important for evaluating peritumoral vasogenic or infiltrative edema. FLAIR sequences have gained significant attention recently as a surrogate for assessment of tumor infiltration, recurrence, and extent of resection. Diffusion weighted imaging identifies areas of random motion of water molecules, which is then quantified in the apparent diffusion coefficient map (ADC). Restricted diffusion, DWI hyperintensity and ADC hypointensity is most often used for identifying acute stroke but may also be used to identify tumors with high cellularity. Although not commonly used in the clinical realm, low ADC values have been shown to correlate with high-grade tumors.
Newer MRI techniques employed recently for aid in surgical planning include perfusion, diffusion tensor imaging (DTI), and functional MRI (fMRI). MR perfusion has multiple different techniques most commonly used is dynamic susceptibility contrast (DSC). Relative cerebral blood volume (rCBV) maps in perfusion imaging shows elevations in tumors related to angiogenesis distinguishing it from low rCBV in other pathologies.
DTI is being heavily evaluated for its utility in determining important white matter tracts (tractography) for planning a surgical approach (see Fig. 7.1 ). It has been investigated as a tool to determine whether a tumor is invading important fiber tracts or displacing them, allowing for a safer gross total resection (GTR). There are limitations to DTI imaging which have prevented its widespread clinical application. Currently, it is only able to determine unidirectional fiber tracts within a single voxel. Since most fiber tracts are multidirectional within a voxel, the accuracy of tractography is limited. Overall, DTI has two potentially very important implications for surgery of high-grade gliomas. It allows for better delineation of tumor borders, leading to superior extent of resection, and illumination of important white matter tracts, possibly improving safety of surgical resections.
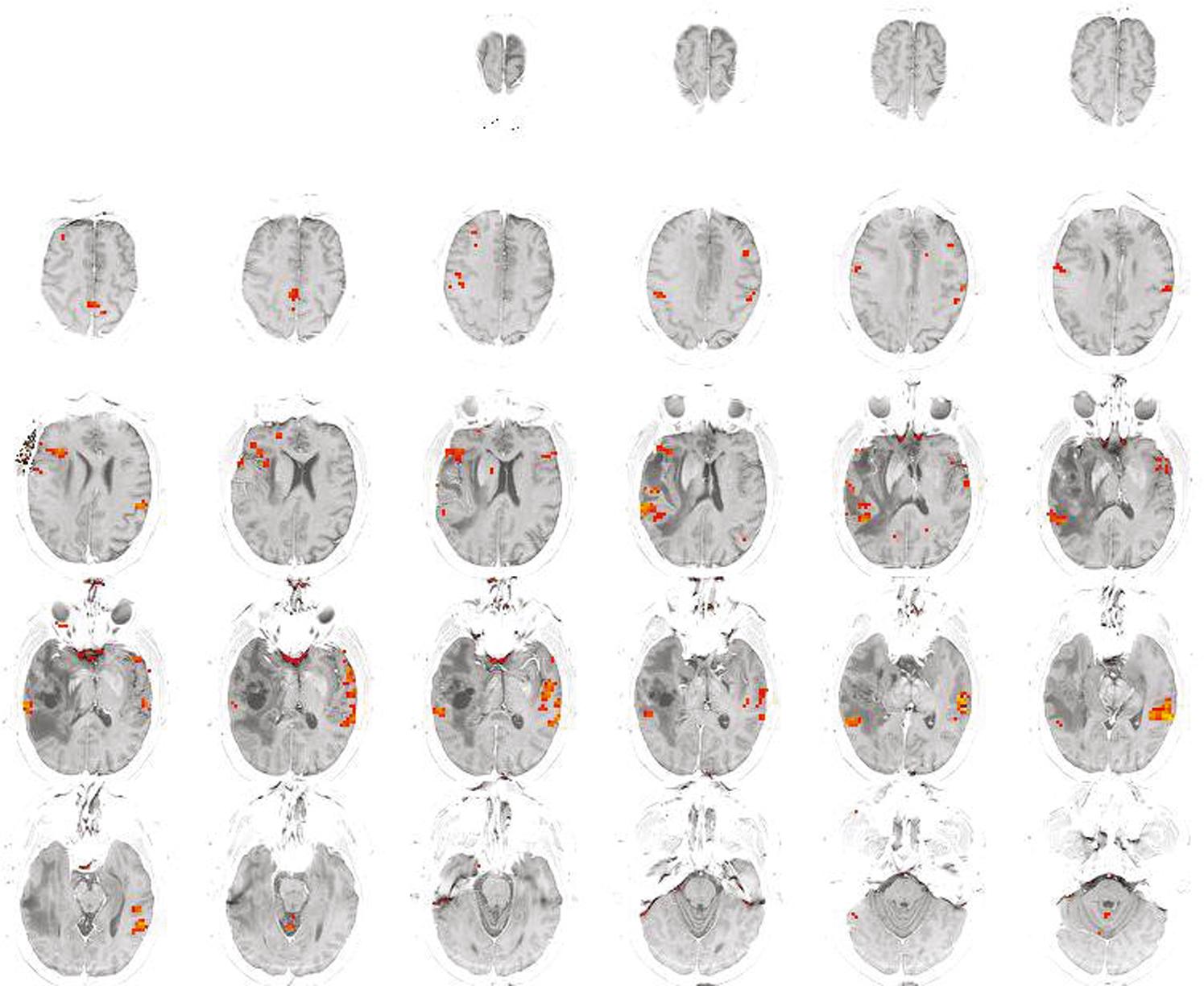
fMRI has been used as an adjunct to preoperative planning for certain tumors including high-grade gliomas in eloquent areas ( Fig. 7.2 ). Task-based fMRI is an indirect measure of cortical function by looking at changes in blood oxygen level dependent signal while performing certain motor and language tasks. Unfortunately, the correlation of task-based fMRI has been variably correlated with the gold standard of intraoperative direct cortical stimulation (DCS). When using fMRI for motor cortex mapping there is better correlation with DCS than with its use for language mapping, likely due to the complexity of language-related tasks and variability in techniques. , More recently, a technique called resting state fMRI (rs-fMRI) has been developed that does not rely on a patient to perform tasks, can be done under sedation, and therefore can be used in pediatric patients as well as other patients that are unable to complete task-based fMRI. Another advantage is that multiple functional networks can be assessed from the same MR acquisition, as opposed to the multiple acquisitions necessary for task-based fMRI. fMRI has been used extensively, with most benefit likely in preoperative motor cortex localization.
Postoperative serial MR imaging for patients undergoing resection of high-grade gliomas is necessary for multiple reasons. It is important to understand the extent of resection, assess for postoperative ischemic strokes, postoperative hemorrhage, and have a baseline measurement to compare at serial time points in response to medical and radiation treatment effects. In this section we will focus on serial MRI imaging characteristics as they relate to tumor treatment effects and tumor progression.
Assessing for tumor recurrence is the main objective of serial MR imaging in high-grade gliomas. Classically, high-grade glioma response to treatment has been evaluated by the McDonald criteria. In order to address the issues of pseudoprogression and pseudoresponse, the Response Assessment in Neuro-oncology (RANO) working group developed new guidelines for determining tumor progression termed the “modified RANO criteria.” They included assessment of T2 FLAIR when determining tumor progression. Separate iRANO criteria were made for assessing pseudoprogression in the context of immunotherapy treatments and NANO criteria for assessing neurological function. These criteria have helped standardize treatment responses and enrollment in clinical trials, but they are not without limitations.
Pseudoprogression —a temporary increase in gadolinium enhancement and edema after chemoradiation—has been observed in 10% to 36% of patients. , Interestingly, pseudoprogression has been observed in patients due to recently introduced immunotherapies.
Pseudoresponse is a phenomenon that has come to light with development of angiogenesis augmenting therapies such as bevacizumab. Gadolinium enhancement of high-grade gliomas relies on increased vascular permeability in the tumor. Anti-angiogenic treatments can significantly reduce vascular permeability and MRI enhancement as soon as 1 to 2 days after initiation, leading to the false assumption of tumor regression.
The goals of surgical resection of high-grade gliomas are symptom relief, tissue histopathological and genetic diagnosis, and maximally safe extent of resection. It is important to emphasize the safety of surgical resection, as causing postoperative deficits in patients may lead to worse survival. In this section we will focus on the extent of surgical resection (EOR) as it applies to patient outcomes and consideration of tumor location.
Throughout the literature there is debate as to the extent of resection of high-grade gliomas and their associated outcomes. Surgical options include biopsy, subtotal resection (STR), GTR or image complete resection, and the newly described supratotal resection (SuTR). These options are all related to the EOR on the T1 weighted contrast enhancing portion of the tumor, except for SuTR. When discussing SuTR, this describes complete resection of the contrast-enhancing portion of the tumor, including as much of the T2 weight FLAIR hyperintensity that is surgically safe.
Multiple prospective studies and even meta-analyses of these studies have been performed, and still there is no consensus on the EOR and their associated survival comparisons. One major reason is that studies do not have a consensus on the definition of STR. It may mean that 20% or 80% of the enhancing part of a tumor was resected. Lacroix and colleagues published a series of 416 patients with glioblastoma that determined that 98% tumor resection was necessary in order to confer a survival benefit of surgery. This effectively meant that only GTR was an acceptable outcome of surgical resection. Sanai and colleagues, published on 500 consecutive patients with newly diagnosed glioblastoma, showing graded survival benefit to STR as minimal as 78%. Median survival for EOR ≥ 78% was 12.5 months, EOR ≥ 80% was 12.8 months, EOR ≥ 90% was 13.8 months, and GTR was 16 months, whereas the overall median survival for the 500 patients, which included all STRs, was 12.2 months. A recent meta-analysis comparing biopsy, STR, and GTR showed that patients undergoing GTR were 61% more likely to survive at 1 year, 19% more likely to survive at 2 years, and 51% more likely to be progression-free at 12 months when compared to patients having STR. When analyzing the survival benefit of STR compared to biopsy there was a significant survival benefit at 1 year in the STR; however, this did not translate to 2-year survival benefits.
Recently a new philosophy of brain tumor resection has emerged, supratotal resection. This has mostly been assessed for low-grade gliomas but has recently been looked at for a series of glioblastoma patients. , In this study they looked retrospectively at the use of selective cortical mapping and subpial resection broader than the contrast enhancing regions in noneloquent regions. In the subpial technique they would continue resection in noneloquent areas until the pia was reached, instead of stopping at the edge of contrast enhancement and normal tissue. If the contrast-enhancing portion was adjacent to eloquent cortex, then they would only remove visible tumor. This subpial technique resulted in GTR resections of greater than 95% in 29% of patients for an overall survival of 54 months. When the patients were divided by 100% EOR compared to 90% to 99% EOR, there was a statistically better overall survival in the patients experiencing 100% EOR. In another retrospective study of over 1200 glioblastomas, patients who had 100% resection of the enhancing portion of the tumor and had greater than 53% resection of T2 weighted FLAIR imaging demonstrated increased median survival of 23.2 months over those who had less than 53% FLAIR resection, who had a median survival of 18.7 months. Overall, the extent of tumor resection is very important when planning surgery. If the surgeon feels that they are able to resect 78% or more without causing harm, then surgery should be attempted. Ultimately the goal should be 100% resection of the enhancing portion of the tumor and possibly, in noneloquent areas, extending that to include areas of FLAIR hyperintensity using a subpial surgical technique. However, this must be balanced with causing neurological deficits, which has been demonstrated to lead to worse overall survival.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here