Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Perinatal palliative care (PPC) programs are increasing across the U.S. These services exist in a wide variety of settings from health care institutions to community- or faith-based organizations, have varying levels of ability and comfort in providing PPC for different clinical scenarios and levels of diagnostic certainty, and varying access to multi-disciplinary specialists and variable missions and visions of the program.
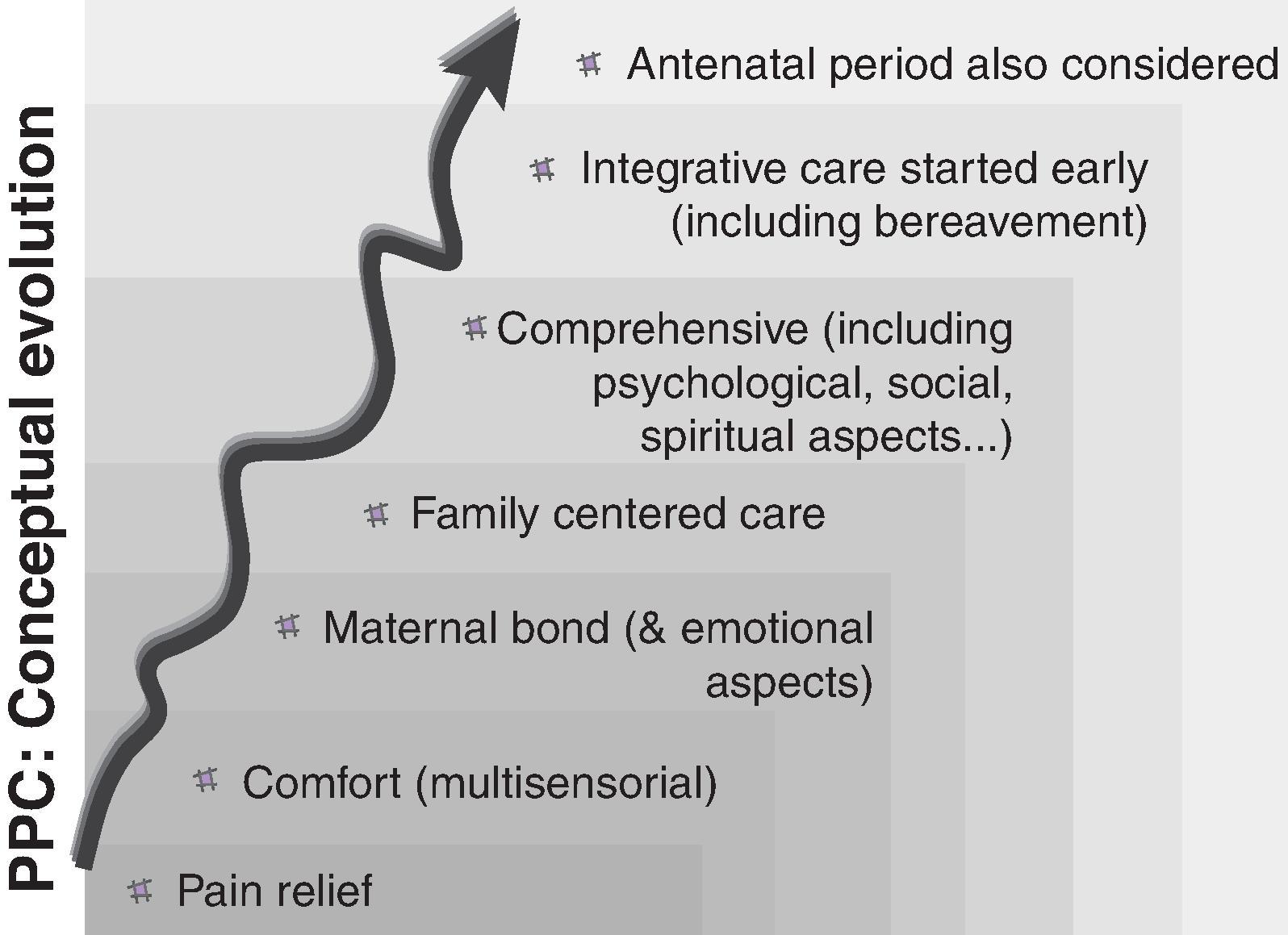
PPC is evolving beyond providing supportive end of life care only, and can provide an extra layer of support to infants, families and clinicians while medical treatments are attempted for serious diagnoses that may not necessarily pose a high risk of death.
In comparison to the evidence for palliative care for older children and adults, there remain basic and unanswered questions related to palliative care for infants.
A growing body of research is dedicated to symptom control for the actively dying infant, ranging from optimal medication titration to the ethical complexity of double effect where medications for symptom management could shorten life.
A challenging limitation of PPC research is the difficulty in accurately and adequately defining the outcomes that matter to infants, families, staff, and health systems.
Palliative care is specialized medical care targeting quality of life for patients with serious illness and their families. The practice grew out of the hospice movement and became a board-certified medical subspecialty in 2006. Although hospice focuses on end-of-life care, palliative care can begin at the time of a serious diagnosis. In 2000 the American Academy of Pediatrics recommended “clinical policies and minimum standards that promote the welfare of infants and children living with life-threatening or terminal conditions, with the goal of providing equitable and effective support for curative, life-prolonging and palliative care.”
Palliative care for neonates may be termed perinatal palliative care (PPC), encompassing prenatal/ postnatal care by inpatient and outpatient palliative care providers; perinatal hospice , referring to prenatal/postnatal care from hospice providers; or neonatal palliative care , or simply pediatric palliative care. Here we use the phrases “perinatal palliative care” and “perinatal hospice” to include prenatal and postnatal services.
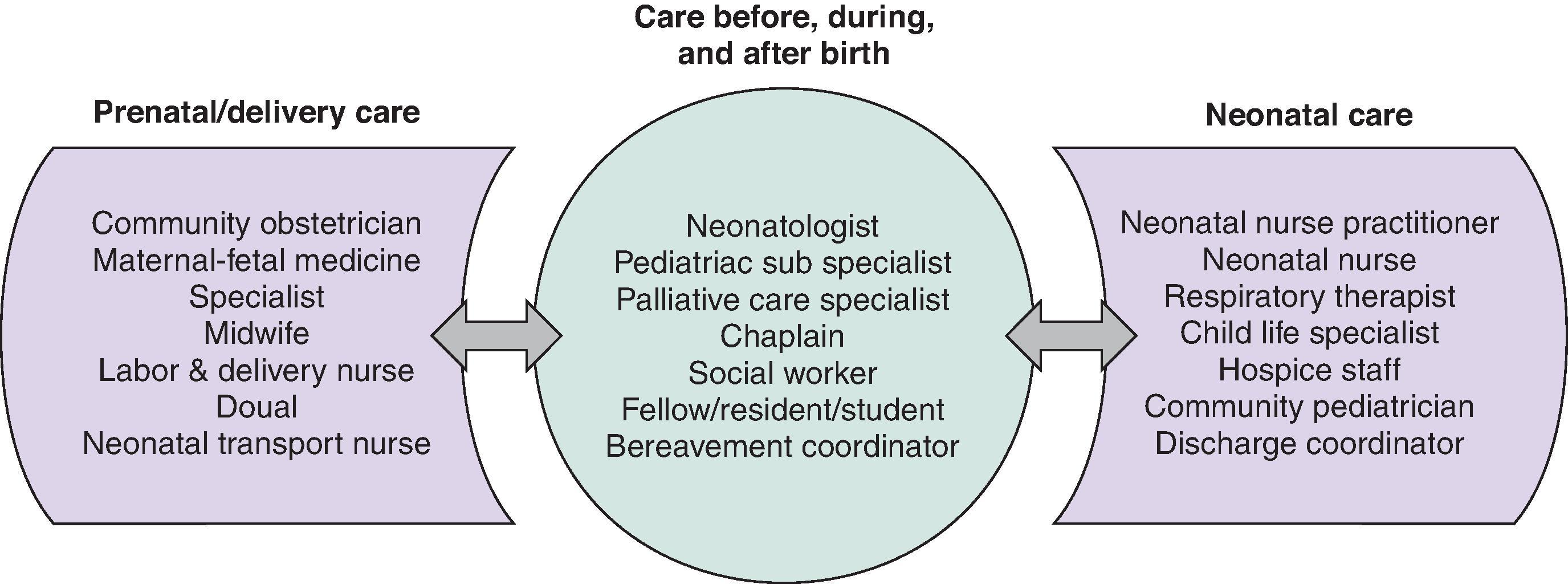
Primary palliative care can be delivered by any interdisciplinary provider as a matter of the routine management of seriously ill patients, as when obstetric social workers provide grief counseling, when neonatologists manage infant pain, or when nurses promote nonnutritive breastfeeding for maternal-infant bonding ( Fig. 88.1 ). Subspecialty palliative care is provided by interdisciplinary clinicians with additional training and certification in pain and symptom management, holistic family supports, and communication. Importantly, these services can span the inpatient/outpatient settings and often include extended bereavement support. Access to subspecialty PPC is growing across the United States.
Perinatal hospice may include a physical inpatient setting for infants receiving complex medications or technologies or who are actively dying. Perinatal hospice is also delivered at home. After a prenatal diagnosis of a serious fetal condition, perinatal hospice nurses, social workers, chaplains, child life specialists, or others can visit the family home to assist with birth plans, counseling, sibling supports, and preparation for end-of-life care. After birth, if infants are able to be discharged home, home hospice provides continuity of these services via intermittent home visits and 24/7 phone support. For families comfortable with death at home, hospice providers can provide comfort interventions for the infant, be present for the death, and initiate postmortem activities including death certificates and funeral details. Perinatal hospice providers also provide longitudinal bereavement support, sometimes with enhanced support during common trigger experiences such as additional pregnancies.
The core of all PPC and hospice is an interdisciplinary team that draws on the unique expertise of individual providers and prioritizes coordination and continuity to support families ( Fig. 88.2 ). Although referrals for perinatal hospice are based on expectations for death in infancy (e.g., within 6 months of hospice enrollment), there is greater variability in PPC referrals. Some centers use “trigger diagnoses,” for example, all infants born at <24 weeks’ gestation. Local palliative care resources must be adequate to support this approach. In centers without triggers, palliative care referral may be limited to patients with clearly life-threatening conditions or may include patients with complex chronic conditions that are debilitating yet not immediately life threatening, for example, infants with severe bronchopulmonary dysplasia and tracheostomy/ventilator dependence.
In this chapter we will review the existing evidence to support PPC clinical practices, education, and research.
Although pregnancy and childbirth have always included high mortality, the first publications regarding the concept of PPC programs were from Whitfield and Mangurten. , Whitfield et al. described the application of hospice concepts to neonatal care, including the family room or essentially the physical environment, the involvement of family in the decision-making process, and the hospice training of neonatal intensive care (NICU) nurses. Mangurten described a series of six infants and their process for medical care and death at home. The term perinatal hospice was first used in the obstetric literature, essentially describing it as an alternative to termination of pregnancy. That same decade, publications emerged describing the development and outcomes of neonatal and perinatal palliative services and end-of-life care. The provision of perinatal bereavement practices in birth centers and NICUs has subsequently become more standard, and continuing education in this specialty is available. For example, Resolve Through Sharing (resolvethroughsharing.org) offers three training programs that include palliative care: perinatal bereavement (PPC), neonatal and pediatric bereavement, and adult bereavement (adult palliative care).
A recent survey of PPC programs reported there are perinatal services in at least 30 states, with 70% of them being less than 10 years old. , These services exist in a wide variety of settings, from healthcare institutions to community- or faith-based organizations. It makes sense that programs may have varying levels of ability and comfort in providing PPC for different clinical scenarios and levels of diagnostic certainty, with varying access to multidisciplinary specialists and variable missions and visions of the program. The growth of PPC programs is exemplified by the ever-increasing number of professional publications. , ,
Identification of which infants and families might benefit from PPC often involves specific fetal/neonatal diagnoses ( Table 88.1 ). Catlin and Carter first described clinical situations in which one should consider neonatal palliative care, coming up with three generalizable categories: (1) newborns at the limits of viability, (2) newborns with congenital anomalies considered incompatible with prolonged life, and (3) newborns with overwhelming illness. The question then became whether these categories could be reasonably predicted prenatally when the disease or condition was diagnosed in utero. Choices about whether to incorporate PPC before birth relies on the degree of diagnostic and prognostic certainty and the meaning of the prognosis to the prospective parents. “Meaning” reflects the ethical principle of family values about what they believe is in the infant’s best interest. ,
| Category 1 | Life-threatening conditions for which curative treatment may be feasible but can fail Involving palliative care services may be necessary when treatment fails or is expected to fail. After successful curative treatment or clinical stability, there may no longer be a need for palliative care services. Examples of conditions: extreme prematurity, congenital heart disease, severe PPHN |
| Category 2 | Conditions in which premature death is inevitable Long periods of intense treatment or intensive care provision may be delivered with the aim of prolonging life and allowing some participation in normal activity. Examples of conditions: chromosomal abnormalities, bilateral renal agenesis |
| Category 3 | Progressive conditions without curative treatment options Treatment is exclusively palliative and may commonly extend over many months or years. Examples of conditions: spinal muscular atrophy, mitochondrial disorders |
| Category 4 | Irreversible but nonprogressive conditions causing severe disability, leading to susceptibility to health complications and likelihood of premature death Examples of conditions: severe hypoxic ischemic encephalopathy |
Historically, PPC was most commonly applied in cases in which the fetus was deemed to have a lethal condition. Other “trigger criteria” for PPC involvement have included diagnoses such as anencephaly, skeletal dysplasia, renal agenesis, and certain chromosomal defects. , , Over time, however, PPC has evolved and the lists of relevant diagnoses are changing. Some of this evolution has come from changing values, whereas others are from advances in medical technology. For example, trisomy 18 had been considered a lethal condition; however, some advocates have demanded more aggressive care, making it difficult to declare a case definitively lethal, although these children still have a life-limiting disorder. Fetal interventions are also changing “lethal” diagnoses, as with amnioinfusion for fetal renal agenesis, which may be able to preserve fetal lung development to permit live birth and eventual dialysis and renal transplant.
PPC is evolving beyond providing supportive end-of-life care only and can provide an extra layer of support to infants, families, and clinicians while medical treatments are attempted for serious diagnoses that may not necessarily pose a high risk of death.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here