Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
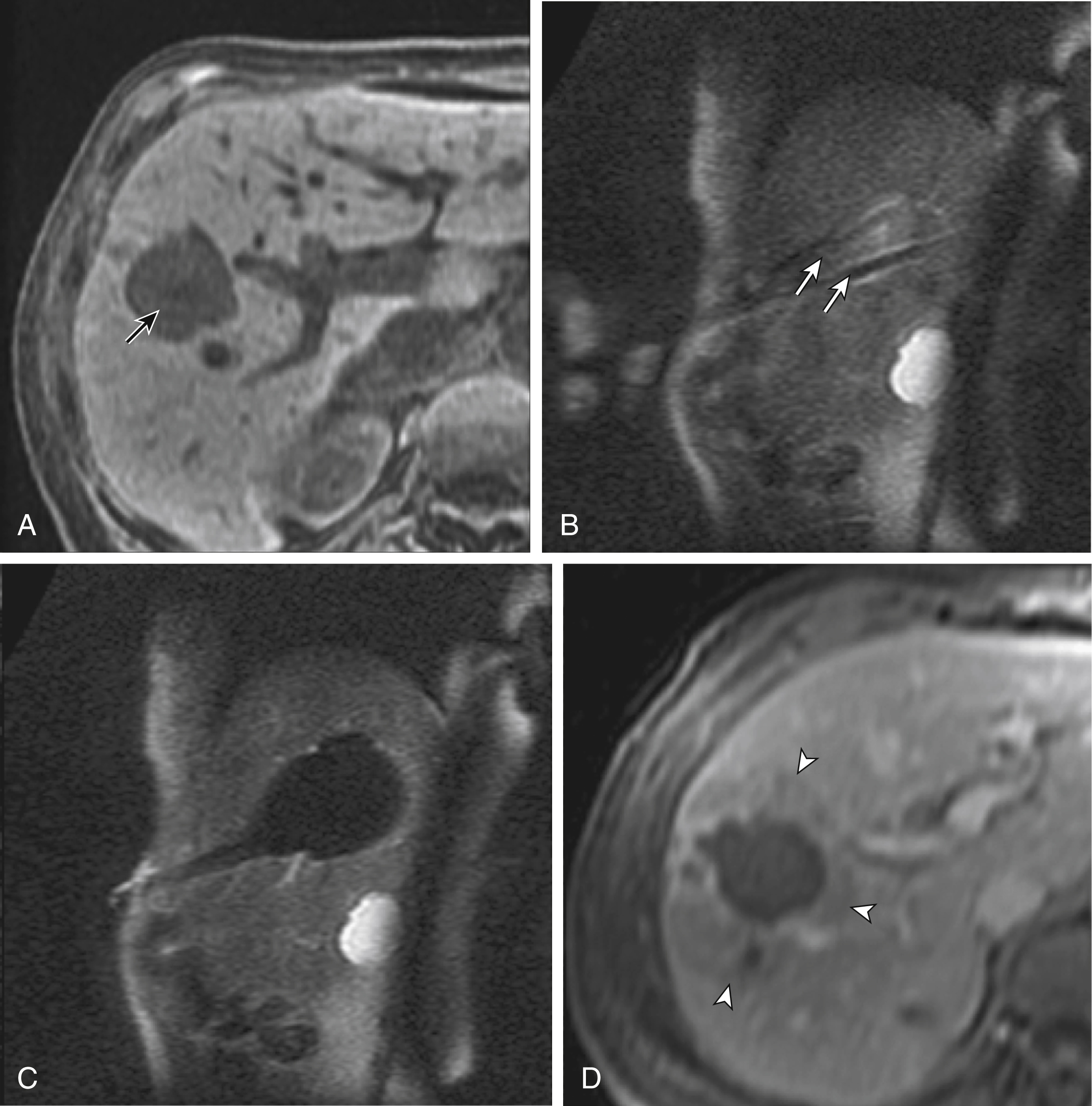
Cryoablation can be used to treat primary malignant liver lesions such as hepatocellular carcinoma (HCC), as well as benign lesions such as symptomatic hemangiomas and liver adenomas. Nonetheless, the most common use of cryoablation in the liver in the United States is for metastatic disease typically from colon, breast, and neuroendocrine primaries ( Fig. 98.1 ). Because only 10%–25% of patients with metastatic liver tumors undergo potentially curative surgical resection, percutaneous tumor ablation is a viable alternative. Likewise, a minority of patients with primary HCC are candidates for curative surgical resection. Tumors are often deemed to be surgically unresectable, because too much liver parenchyma would be sacrificed or because the tumor lies too close to major biliary or vascular structures, such that adequate margins cannot be obtained. Another restriction for surgery is various comorbid conditions, such as cardiopulmonary disease or poor nutritional status. A percutaneous approach allows treatment of these surgically challenging tumors because the tissue destruction can be targeted precisely at the tumor and the immediately surrounding adjacent liver parenchyma, with preservation of a greater percentage of normal parenchyma. Likewise, cryoablation may also be able to induce tumor necrosis when vascular or biliary structures are challenging for the surgeon because of proximity of the tumor to vital structures in the hepatic hilum (although radiologists too must exercise great caution in these same anatomic regions).
Cryoablation may also be indicated for patients who have pathologically proven metastatic lesions in whom surgical cure is not an option. Surgery may not be feasible because of bilobar disease, limited hepatic reserve, or cardiopulmonary compromise. Cryoablation generally is used for one to five lesions that are confined to the liver and measure up to 5 cm in diameter, with ablation efficacy decreasing with increased tumor size. A 2017 study noted the percentage of tumors without local hepatic progression 3 months after cryoablation as 93.4% (213/228) and 60.0% (18/30) for sizes less than 4 cm and for sizes 4 cm or greater respectively.
Most institutions consider the presence of metastatic disease outside the liver to be a relative contraindication to treatment by cryoablation alone, with the possible exception of lung or bone metastases in patients with breast cancer. Cryoablation is indicated for the treatment of residual tumor or local hepatic recurrence in patients who have previously undergone treatment with surgery or ablation, as well as new metachronous lesions after primary treatment.
Cryoablation has also been used to treat primary liver neoplasms, most commonly HCC. Indications for cryoablation of primary HCC are different from those for metastatic disease because of the underlying pathology. HCC is caused by underlying chronic liver disease that is usually secondary to hepatitis or alcoholic liver disease. Because of the underlying disease, the only definitive treatment for HCC is liver transplantation. As a result of the limited availability of donated livers and the high cost of transplantation, only a very small percentage of patients can undergo this treatment option. Surgery can offer complete resection of the first HCC and any satellite lesions, but a second or even further lesions may have already developed, or will develop in many patients. If surgical resection was chosen to treat the primary lesion, few patients will be able to undergo a second resection. Ablation affords the possibility of complete destruction of the first and subsequent lesions, without significant loss of functioning liver parenchyma. We have treated patients up to five times percutaneously for secondarily diagnosed lesions. Strategically, patients undergo surveillance, and as new lesions appear, they can also undergo ablation.
Cryoablation has also been used to treat benign liver lesions, specifically, hemangiomas and adenomas. Adenomas are seen predominantly in younger women taking oral contraceptives; the tumors occasionally cause abdominal pain. Cessation of oral contraceptives is first-line therapy, but with persistent problems (especially pain), more invasive treatment may be necessary. Cryoablation is a valuable alternative because of the amount of liver that can be preserved and the low risk involved in the ablation procedure.
Percutaneous cryoablation is a relatively safe procedure and there are few absolute contraindications to its use. As with most invasive procedures, the only absolute contraindications are an uncorrectable coagulopathy or an uncooperative patient. Contraindications to general anesthesia can be considered relative because the procedure can be done under intravenous conscious sedation if needed. However, intravenous conscious sedation is suboptimal if extended breath-holds will be necessary and the patient is not able to be completely cooperative.
When cryoablation is used to treat liver masses, there are several hazardous areas where special care needs to be taken to avoid damage to adjacent structures. Ablating liver lesions that are adjacent to the hepatic hilum, gallbladder, stomach, kidney, pancreas, and colon can be accomplished, but careful planning and execution are essential. Vascular structures are relatively resistant to cryoablation because of the warming effects of flowing blood; however, the biliary system is vulnerable to injury, especially if there are bacteria in the bile ducts. If the lesion to be ablated is juxtaposed to major branches of the biliary system, warm fluid can be circulated through the system via a catheter placed percutaneously or endoscopically. Care also needs to be taken not to cause damage to structures outside the liver, such as the adjacent stomach or bowel.
Sometimes the positioning of the patient (i.e., prone vs. supine) can provide adequate distance to avoid injury to critical structures. If positioning of the patient does not provide adequate safety of adjacent structures, sterile water, dextrose, or a normal saline barrier can be interposed ( Fig. 98.2 ). This is accomplished percutaneously by injecting sterile fluid through a fine needle between the lesion and the bowel to be displaced, termed hydrodissection. Overall, when care is taken in both planning and execution of cryoablation, it is quite a safe procedure.
During the early days of cryosurgery, the probes were cooled with liquid nitrogen. Because these probes were relatively large (3- to 8-mm outer diameter), for years cryoablation was practical only in a surgical setting. Because the size of these probes was suboptimal, a complicated Seldinger technique was used that required several minutes to position and reposition the probes. Even though these probes were effective in causing tissue destruction, the probe size and handling of the liquid nitrogen were negative features in light of the now contemporary gas-based systems.
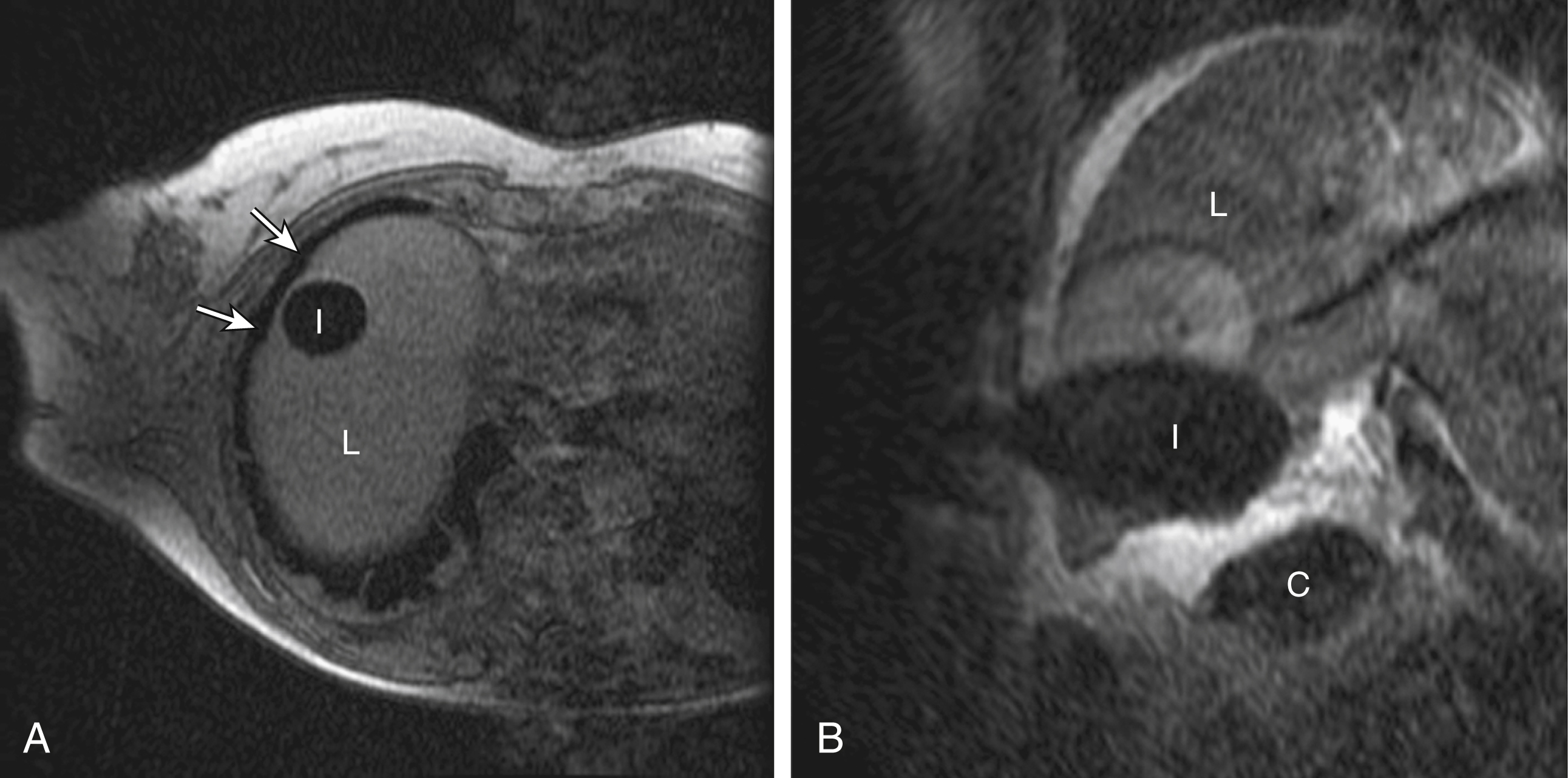
The argon gas–based systems that were developed in the 1990s have replaced liquid nitrogen devices. Argon systems work on the Joule-Thompson principle, in which low temperatures are achieved by the rapid expansion of a high-pressure gas through a thin aperture ( Fig. 98.3 ). Because of the low viscosity of argon gas, it can be circulated rapidly within the probe tip. This allows faster cooling at the probe tip, which hastens removal and repositioning (if necessary) of the cryoprobes. After the freezing phase is complete, high-pressure helium gas can then be circulated through the probe tip to cause rapid thawing. Helium provides an effect opposite to that of argon gas under the Joule-Thompson principle: helium causes a warming of the probe that allows rapid thawing for probe removal from the frozen tissue or repositioning.
There are many cryoablation manufacturers coming into existence; two major manufacturers of cryoablation equipment are BTG PLC (Arden Hills, MN) and EndoCare, Inc. (Endo Pharmaceuticals, Chadds Ford, PA). Both companies use an argon/helium-based system to cool and thaw the probe tip, respectively, and have stand-alone consoles that are connected to gas tanks. Both systems have a similar computer-based interface that demonstrates the vital statistics of the different probes and their respective temperatures ( Fig. 98.4 ). Galil Medical and EndoCare cryoprobes for percutaneous ablation are needle-like, 17-gauge in size. The Galil system can accommodate up to 25 probes; the EndoCare system up to 8 probes. Other manufacturers focus on the treatment of specific conditions such as atrial fibrillation and breast cancer, and include the manufacturers Sanarus and ArtiCure.

All three main cross-sectional imaging techniques can be used to guide percutaneous placement of cryoprobes for ablation. Ultrasound, computed tomography (CT), and magnetic resonance imaging (MRI) each have advantages and disadvantages. Ultrasound was first used in the early 1980s; its utility has since expanded to guide percutaneous cryoablation. Ultrasound allows real-time imaging during probe placement, and therefore major structures such as the gallbladder, large bile ducts, and larger hepatic vessels are well visualized and can be avoided.
The iceball that is created during cryoablation is intensely echogenic on ultrasound; this allows real-time monitoring as the iceball forms and propagates. Thus damage to the surrounding normal liver parenchyma is limited. The main drawback of ultrasound is the distal acoustic shadow produced by the iceball. Because of the echogenicity of the iceball, ultrasound cannot penetrate beyond it; therefore, structures distal to the iceball are not visualized because of the acoustic shadowing. This can be problematic when trying to avoid critical structures that are deep to the tumor being ablated. Reverberation artifact and the critical angle effect also may be problematic when ultrasound guidance is used. The critical angle effect can cause the iceball to appear speciously larger, whereas reverberation causes apparent echoes within the iceball. The critical angle effect is caused by variation in the speed of sound as it travels through soft tissue versus ice, and is more apparent when using a vector transducer than a linear transducer.
CT has many attributes that make it an appealing imaging choice for ablation. CT is widely available, and is often primarily used to detect and monitor lesions that have been ablated. CT also shows the anatomy of the liver and adjacent structures well. This allows identification of adjacent structures that may need to be avoided, such as major vessels, the gallbladder, and bowel. In soft tissue, such as the liver parenchyma and solid tumors, the iceball is generally well seen as a hypodense region ( Fig. 98.5 ). The margins of cell death and the visible iceball also correlate well when using CT. One drawback of the use of CT for image-guided ablation is the exposure of the patient and personnel to ionizing radiation. In a retrospective study of 20 CT-guided percutaneous liver tumor cryoablations, the total effective dose for the procedure was 72 ± 18 mSv. Although that report suggests ways to reduce such exposure, it does call attention to an added risk with CT guidance. Of course, the uncertain risk due to the radiation is weighed against the imminent health risks associated with the disease state for which the ablation is being employed, or the risks of other forms of therapy, such as radiation therapy or chemotherapy.
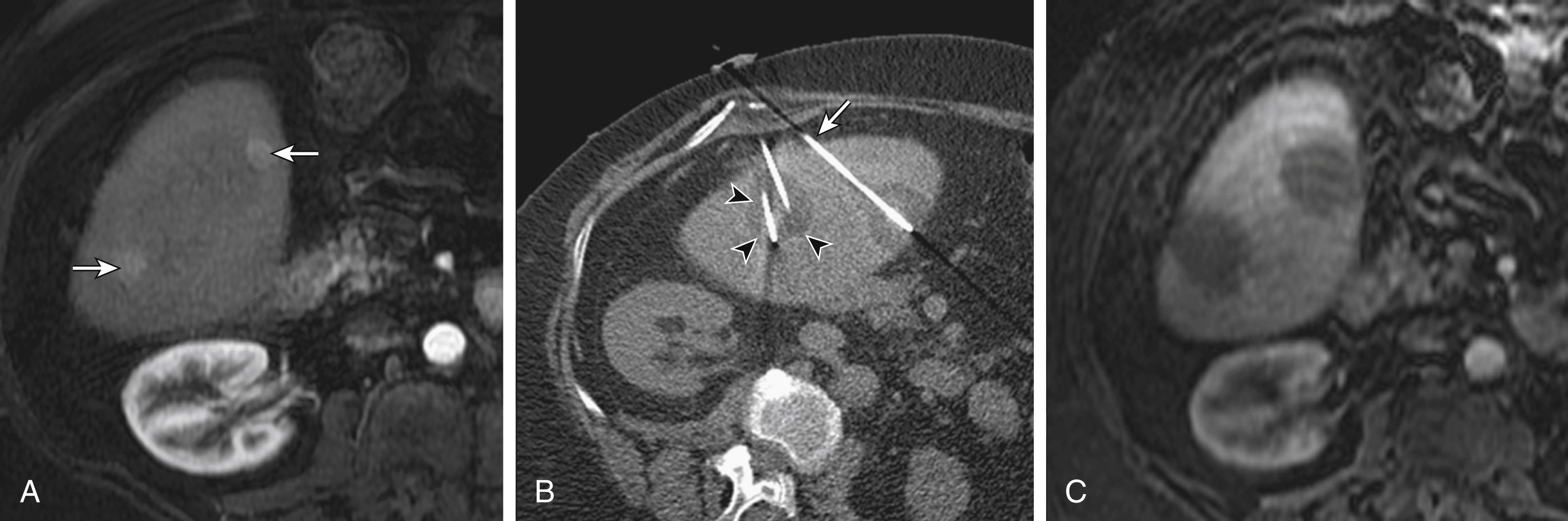
One technological assistance to identifying a tumor location in unenhanced CT images is to “register” preprocedural MRI images with an intraprocedural CT scan. Contemporary efforts use a technique of nonrigid registration to superimpose the MRI scan onto the CT scan, so that the two studies overlie each other. The resulting information-rich MRI-CT can improve tumor visualization during interventional planning, targeting, and monitoring.
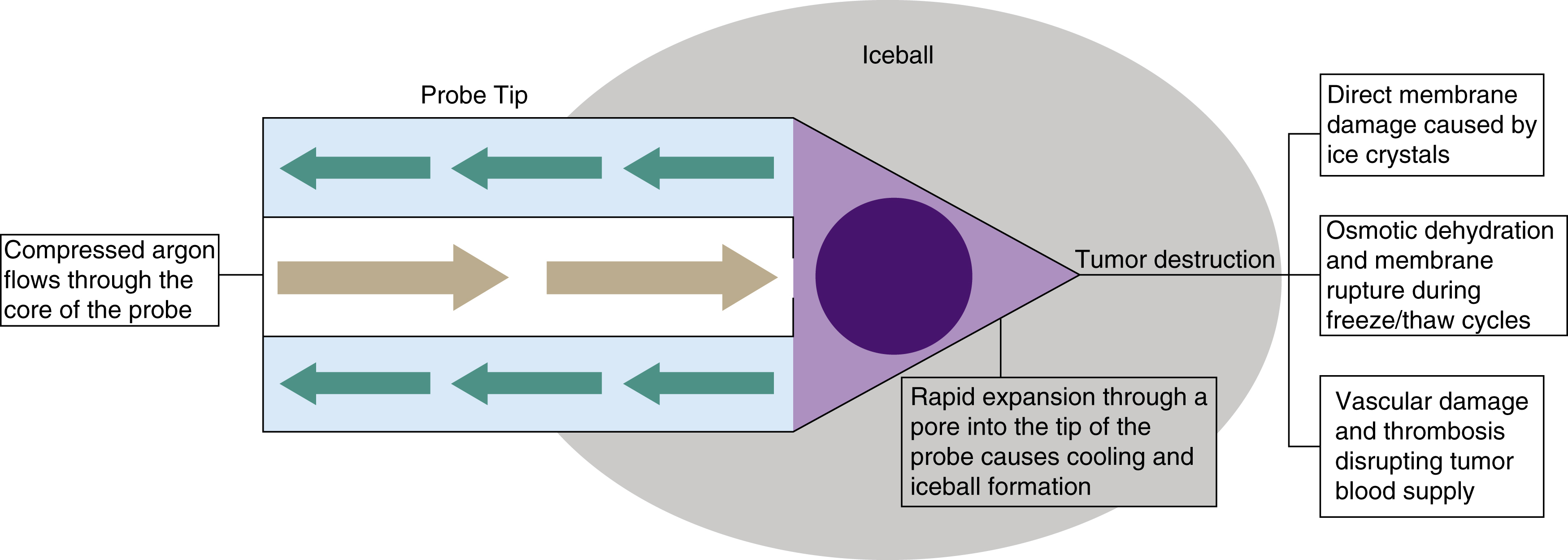
In recent years, MRI has been used for a variety of interventional procedures and ablations. In one institution’s experience of over 300 cryoablation procedures, two-thirds were guided by MRI. MRI has a distinct advantage over CT in that the tumor is nearly always distinguishable from normal liver parenchyma without the aid of intravenous contrast agents. The multiplanar capability of MRI is another advantage. The cryoprobes can be accurately placed and verified in all three planes—axial, sagittal, and coronal. Cryoablation can be performed in traditional MRI scanners with the development of MRI-compatible probes and other instruments. However, with open or wide-bore systems, the radiologist has sufficient access to the patient and can guide placement of the probes during cryoablation. This allows nearly real-time imaging during ablation and greater accuracy in controlling the developing iceball. Another benefit of MRI is the ability to assess the temperature within the iceball and neighboring tissues because of T1-weighted imaging characteristics. Like ultrasound and CT, the iceball on MRI, visible as a signal void region on all conventional pulse sequences, corresponds well to the actual ablative zone size. However, MRI demonstrates the demarcations from iceball to tumor to normal parenchyma without any interference or artifact, unlike ultrasound and CT, and MRI avoids radiation as well. Finally, unlike ultrasound and CT, the signal characteristics of a liver tumor allow it to be visualized apart from the iceball throughout the procedure. This is a distinct advantage, because the goal is to treat the entire tumor with a sufficient margin while minimizing the effect on the surrounding liver parenchyma.
Positron emission tomography (PET) and PET/CT have been proposed as image-guidance modalities for cryoablation and radiofrequency ablation (RFA). The role of fluorine-18 fluorodeoxyglucose intraprocedurally is the subject of nascent research of the general hypothesis that nuclear medicine imaging could assist in interventions. In a recent study of 12 patients having undergone thermal ablation (3 of which were cryoablation) in the presence of fluorine-18 fluorodeoxyglucose, no decrease in the avidity of the fluorine-18 fluorodeoxyglucose was observed in light of the exposure to the extreme temperatures of the treatments. Thus, although the tracer may be useful in targeting the metabolically active target, it may serve little use in monitoring the ablation or assessing acute effects. The utility of a postablation injection may have some role; certainly tracers with half-lives shorter than fluorine-18 fluorodeoxyglucose may open new paradigms for ablation.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here