Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The predominant aim in managing critically ill neurosurgical patients is to prevent cerebral ischaemia and exacerbation of neurological injury.
This is achieved by manipulation of a variety of neurophysiological parameters including intracranial pressure (ICP), cerebral perfusion pressure (CPP) and cerebral blood flow (CBF).
Knowledge of the aforementioned neurophysiological principles is important in understanding the mechanism of action and application of therapeutic interventions in a neuro-critical care setting.
Initial assessment of the critically ill neurosurgical patient requires a systemic, methodical and reproducible approach to identify, resuscitate and treat life-threatening insults in the most important sequence in which they occur.
A variety of techniques allow the multi-modal monitoring of critically ill neurosurgical patients allowing individualisation of treatment; trends and variability over a time course provide more useful information than isolated measurements.
Complications that are general to all neurosurgical patients, and those that are specific to the each neurosurgical pathology should be investigated for an identified in a deteriorating critically ill neurosurgical patient.
The diagnosis of brain death is important in critically care settings and familiarity with institutional, regional and national guidance is essential.
Understanding concepts pertaining to the management of critically ill neurosurgical patients is vital for optimizing outcomes. The nervous system is vulnerable not only to effects from the initial insult it suffers from a pathologic process (primary brain or spinal cord injury) but also to systemic factors, which exacerbate this primary injury (ie, secondary brain or spinal cord injury). Critically ill neurosurgical patients are managed in dedicated neurocritical care units (NCCUs). This spectrum includes patients admitted in extremis following their initial injury for preoperative optimization and stabilization, patients in the immediate postoperative phase following elective surgery, and any previously stable patient in a ward setting that suffers a neurologic deterioration.
This chapter provides a succinct summary of key concepts regarding the management of critically ill neurosurgical patients including the following:
Neurophysiologic principles of cerebral homeostasis, cerebrospinal fluid (CSF) flow, cerebral blood flow (CBF) and cerebral perfusion pressure (CPP), intracranial pressure (ICP), and cerebral ischemia and its pathophysiologic impact on the nervous system
Initial assessment of and etiologies of deterioration in critically ill neurosurgical patients
Basic concepts of management in NCCUs
Principles of neurologic monitoring including ICP, jugular venous oxygen saturation (SjvO 2 ), brain tissue oxygen tension (PbtO 2 ), and transcranial Doppler (TCD) sonography
Specifics of general care in critically ill neurosurgical patients including management of raised ICP, seizures, infection, and electrolyte derangements
Special considerations on critical care management of neurosurgical pathologies including traumatic brain injury (TBI), vascular pathology (aneurysmal subarachnoid hemorrhage [aSAH], arteriovenous malformations [AVMs], intracranial hemorrhage), brain tumors, posterior fossa surgery, neuromodulation and epilepsy, pituitary surgery, and spinal cord injury
Concepts regarding diagnosis of brain death
It is beyond the scope of this single chapter to comprehensively cover all topics to the degree each deserves. The reader is advised to refer to the variety of excellent monographs and texts on the subject where necessary.
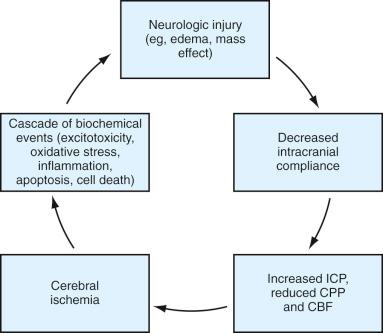
The most significant complication of the majority of neurosurgical pathologies is cerebral ischemia. It is a by-product of a propagating vicious cycle starting with the initial neurologic injury leading to a reduction in intracranial compliance with increasing ICP and a reduction in CPP and CBF with the resultant ischemic injury exacerbating the neurologic injury ( Fig. 26.1 ).
The predominant aim of NCCU management in critically ill neurosurgical patients is to optimize systemic physiology, contribute to neuroprotection, and control ICP to allow restoration of CPP and CBF, thereby preventing ischemia and limiting secondary brain or spinal cord injury. Understanding the manipulation of the aforementioned parameters requires a brief discussion of the relevant neurophysiologic concepts underpinning CSF production and flow, CBF, CPP, and ICP.
CSF production is approximately 450 to 500 mL/24 hours and predominantly via three sources: 60% to 70% by choroid plexus (within the lateral, third, and fourth ventricles) with the remaining 30% being extrachoroidal (ventricular ependymal lining, dural lining of spinal nerve roots, brain parenchyma). Absorption is via arachnoid granulations and villi into dural venous sinuses and is dependent on venous pressure. The balance between production and absorption may be altered in pathologic states necessitating CSF diversion to prevent alterations in ICP. Pharmacologic agents such as furosemide (impacts on chloride transport) and acetazolamide (inhibition of carbonic anhydrase) can reduce CSF production.
Despite its relatively small size (~2% of total body mass), the brain has the highest metabolic requirement of any organ, necessitating a consistent and reliable blood flow to provide continuously high levels of oxygen delivery and energy substrates (predominantly glucose). It consumes the following:
15% of the resting cardiac output (CO) with an average CBF of 750 mL/min
20% of the basal oxygen consumption with an average of 50 mL/min
25% of the basal glucose consumption
CBF is directly proportional to the CPP and inversely proportional to the cerebrovascular resistance (CVR) of the intracranial vessels:
The CVR is predominantly a factor of the vessel diameter, which is regulated by smooth muscle contractility in vessel walls: smooth muscle contraction causes vasoconstriction, which decreases vessel diameter with a resultant increase in CVR and vice versa. The CPP is directly related to the mean arterial pressure (MAP) and the ICP via the following equation:
CBF is regulated by a variety of factors including the following :
Metabolic demand (including neurogenic and metabolic factors)
Autoregulation (mediated by neurogenic and myogenic mechanisms)
Arterial carbon dioxide tension (PaCO 2 ) and oxygen tension (PaO 2 )
CBF is regionally variable, and the distribution parallels and reflects the degree of metabolic activity in different parts of the brain (flow-metabolism coupling) . The average CBF is 50 mL/100 g of tissue/min with areas of increased neuronal activity having a higher cerebral metabolic rate and therefore increased regional CBF (average in gray matter, 80–110 mL/100 g of tissue/min; average in white matter, 25 mL/100 g of tissue/min).
Metabolic activity is reflected by the cerebral metabolic rate of oxygen consumption (CMR O 2 ) and the cerebral metabolic rate of glucose utilization (CMR Glucose ). The close matching of flow metabolism means that although there is regional variation in CBF, CMR O 2 , and CMR Glucose , the overall oxygen extraction fraction (OEF) remains relatively constant (~40%). The regulatory changes in flow-metabolism coupling have a short latency (~1 sec) and are mediated by regional metabolic and neurogenic factors.
Metabolic factors exert their effect via a negative feedback mechanism. The initially increased metabolic activity increases the level of local metabolic factors precipitating an increase in perfusion and CBF. This leads to an increased washout of these factors with an associated reduction in flow. Examples of vasodilatory factors (which increase flow) include nitric oxide (NO), specific prostaglandins (PgE 2 and PgI 2 ), and adenosine. The local levels of these factors may also increase with increased activity during “stress” states (eg, hypoxia, hypotension, seizures). Vasoconstrictive factors (which decrease flow) include free calcium ion, thromboxane (TxA 2 ), and endothelin.
Neurogenic mechanisms work via a combination of sympathetic activity (α-2 adrenergic activity is vasoconstrictive, and β-1 adrenergic activity is vasodilatory) and local neural factors (eg, acetylcholine [ACh], NO, serotonin [5-HT], dopamine [DA], substance P, neuropeptide Y).
Depression of cerebral function (eg, anesthesia, hypothermia, sedation) all suppress metabolism (CMR O 2 , CMR Glucose ) with a coupled reduction in CBF, whereas hyperthermia and seizure activity increase metabolism and CBF. It is estimated that for every 1°C change in temperature, the CMR O 2 and CBF can change by as much as ~5%.
Autoregulation describes the ability of the cerebral vasculature to maintain a relatively constant CBF despite fluctuations in CPP by regulation of the CVR of intracranial vessels. It works independently of other mechanisms of CBF control such as flow-metabolism coupling and PaCO 2 ( Fig. 26.2 ).
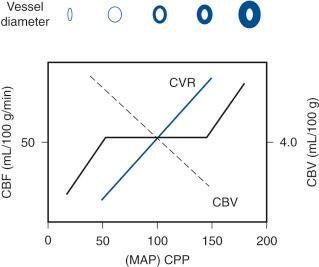
Autoregulation works within CPP limits (usually between 50 and 150 mm Hg), although there is significant regional variation in the brain and among individuals. Outside of these limits, however, the CBF is directly dependent on CPP: above 150 mm Hg, an increase in CPP results in increased CBF with forced vasodilatation of cerebral arterioles, increased cerebral blood volume (CBV), ICP, and a resultant disruption of the blood-brain barrier and risk of cerebral edema or hemorrhage; conversely, below 50 mm Hg, a decrease in CPP results in a significant drop in CBF, leading to ischemia.
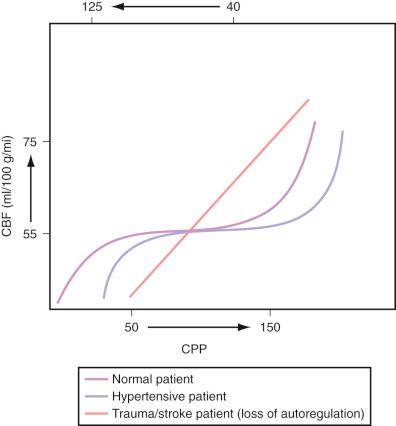
Autoregulation is mediated by myogenic reflexes within the resistance intracranial vessels (predominantly tone and contractility within smooth muscle in arteriole walls) and neurogenic factors (metabolic factors, neural factors, sympathetic activity as described earlier), and these factors are usually slower compared to those of flow-metabolism coupling. Other relevant clinical factors impacting autoregulation include (1) inhalational anesthetics (autoregulation impaired in a dose-dependent fashion), (2) preexisting hypertension (the autoregulation curve is shifted to the right with a narrower plateau and therefore blood pressure required clinically to maintain constant CBF may be higher than expected; targeting lower blood pressures expected with “normal” patients may place the patient in the linear part of the curve with a resultant fall in CBF and ischemic risk), and (3) disruption of the blood-brain barrier in intracranial pathologic processes (eg, trauma, tumors, stroke) where autoregulation is lost ( Fig. 26.3 ).
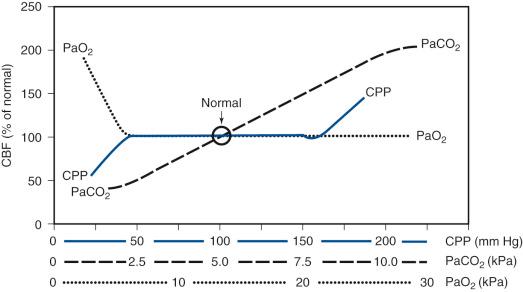
Arterial carbon dioxide tension is a clinically important regulator of CBF; it crosses the blood-brain barrier readily and changes extravascular pH. Increasing PaCO 2 (hypercapnia) precipitates vasodilatation with a reduction in CVR and an increase in CBF (up to an upper limit where vasodilatory effects are maximal). Conversely, decreasing PaCO 2 (hypocapnia) causes vasoconstriction with increased CVR and decreased CBF and CBV. It is estimated that for 1 mm Hg change in PaCO 2 (1 kPa is equivalent to 7.5 mm Hg), the CBF may change by as much as 4% (2 mL/100 g of tissue/min). Clinically in patients with decreased intracranial compliance and therefore raised ICP, hyperventilation-mediated hypocapnia can reduce the CBF, CBV, and therefore ICP.
The manipulation of PaCO 2 to control ICP should, however, only be used as a short-term measure until a definitive method of ICP control is instituted. The reasons are twofold: (1) persistent hypocapnia causes vasoconstriction to a maximal limit beyond which tissue hypoxia and cerebral ischemia ensue together with an associated reflex vasodilation, and (2) the effect of decreased PaCO 2 is mediated by an increase in the perivascular pH, which is reversed by a corresponding decrease in extracellular fluid bicarbonate to normalize the pH (usually within ~6 hours).
Arterial oxygen tension impacts on CBF but not as significantly as carbon dioxide; CBF is usually unchanged with decreasing PaO 2 until it drops below a threshold (~8 kPa) after which a vasodilatory response is seen. Hyperoxemia may produce some cerebrovascular vasoconstriction, which is postulated to be an evolutionary neuroprotective measure against oxygen free radicals ( Fig. 26.4 ).
Benzodiazepines and the majority of intravenous (IV) anesthetic agents (eg, etomidate, propofol, thiopental) reduce CMR O 2 and CBF and therefore ICP. This reduction is often in a dose-dependent fashion. Autoregulation, flow-metabolism coupling, and responsiveness to CO 2 remain intact. However, in critically ill neurosurgical patients (eg, traumatic brain injury), flow-metabolism coupling may be impaired and therefore the reduction in CBF (flow) may exceed that of CMR O 2 (metabolism), leading to a mismatch and therefore widened cerebral arteriovenous oxygen gradient and impaired perfusion and ischemia. This must be borne in mind as agents such as propofol—widely used due to a short t 1/2 allowing rapid emergence if required—may induce precipitous hypotension and a decrease in CPP, especially in hypovolemic patients. Inhalational anesthetics reduce CMR O 2 but increase CBF via a vasodilation effect. Autoregulation is impaired in a dose-dependent fashion. Ketamine increases CMR O 2 , CBF, and ICP and therefore is often avoided in critically ill neurosurgical patients.
ICP is defined as the pressure within the intracranial space relative to atmospheric pressure. Normal ICP may be between 8 and 15 mm Hg, but it is subject to substantial individual variation and physiologic fluctuation (eg, related to posture [supine/standing] and mechanisms such as coughing/straining). The intracranial volume within the intact skull vault is fixed, and the ICP within is dependent on the total volume of contents within the skull.
The brain parenchymal volume takes into consideration extra- and intracellular compartments and contributes ~80% of the total volume (~1400 mL). The blood volume is inclusive of arterial and venous blood and contributes ~10% (~150 mL), whereas the CSF volume also contributes ~10% (~150 mL). The Monro-Kellie doctrine states that an increase in volume of one compartment requires an equal reduction in volume of the other compartments to maintain a constant intracranial pressure within the fixed skull. Of the three compartments the least compressible is the brain parenchyma, whereas the most amenable are the CSF and blood compartments.
Increased intracranial volume (eg, a space-occupying lesion such as a tumor or hematoma) is initially buffered by displacing intracranial CSF into lumbar cisternal subarachnoid spaces, increasing venous outflow, and reducing CBF and CBV. This initially prevents an increase in ICP. However, there is a limit to which these measures can compensate for increasing intracranial volume. This dynamic relationship is represented by the classical pressure-volume curve ( Fig. 26.5 ). The differential change in pressure per unit volume (ΔP/ΔV) is elastance and its reciprocal is compliance (ΔV/ΔP).
![Figure 26.5, Pressure-volume curve. Zone A: Compensatory and buffering mechanisms (decrease in CSF and venous volumes) are intact and therefore large changes in volume cause little or no change in ICP (ie, low elastance [ΔP/ΔV] with high compliance [ΔV/ΔP]). Zone B: As compensatory measures progressively reduce, the change in ICP for the same change in volume starts to increase (ie, increasing elastance and decreasing compliance). Zone C: Once the threshold for compensatory and buffering capacity has been exceeded (the “decompensation point”), small increase in volume results in a substantial and often exponential increase in ICP (ie, high elastance with low to almost no compliance). Figure 26.5, Pressure-volume curve. Zone A: Compensatory and buffering mechanisms (decrease in CSF and venous volumes) are intact and therefore large changes in volume cause little or no change in ICP (ie, low elastance [ΔP/ΔV] with high compliance [ΔV/ΔP]). Zone B: As compensatory measures progressively reduce, the change in ICP for the same change in volume starts to increase (ie, increasing elastance and decreasing compliance). Zone C: Once the threshold for compensatory and buffering capacity has been exceeded (the “decompensation point”), small increase in volume results in a substantial and often exponential increase in ICP (ie, high elastance with low to almost no compliance).](https://storage.googleapis.com/dl.dentistrykey.com/clinical/CriticalCareManagementofNeurosurgicalPatients/4_3s20B9780323431408000263.jpg)
The major complication with persistent and prolonged ICP elevation is twofold: (1) it results in a decrease in CPP (CPP = MAP – ICP) with resultant ischemic injury and (2) it precipitates “shifting” and displacement of cerebral tissue across intracranial compartments with neural tissue compression and devastating complications (“herniation” syndromes; Table 26.1 ).
| Herniation Type | Structures Compressed | Complications and Features |
|---|---|---|
| Cingulate/Subfalcine Mesial frontal lobe (cingulate gyrus) herniates under the falx cerebri to the contralateral side |
Anterior cerebral artery | Contralateral paresis of the leg |
| Frontal horn of lateral ventricle | Hydrocephalus | |
| Lateral (Uncal) Tentorial Mesial temporal lobe (uncus) herniates across tentorial incisura compressing the rostral brainstem (midbrain) |
Ipsilateral cranial nerve III | Ipsilateral fixed, dilated pupil |
| Ipsilateral cerebral peduncle | Contralateral hemiparesis | |
| Reticular activating formation | Impaired consciousness level | |
| Ipsilateral posterior cerebral artery within ambient cistern | Blindness from occipital lobe infarction | |
| Kernohan Notch Syndrome Variant of lateral (uncal) tentorial herniation whereby compression of contralateral structures against the contralateral tentorial incisura occurs |
Contralateral cranial nerve III | Contralateral fixed, dilated pupil |
| Contralateral cerebral peduncle | Ipsilateral hemiparesis | |
| Central/Diencephalic Diencephalic structures and midbrain are compressed and displaced either from inferior or superiorly across the tentorial incisura |
Midbrain vertical gaze center | Loss of vertical up-gaze with tonic down-gaze |
| Pontine structures | Bilateral fixed and pinpoint pupils | |
| Cardiorespiratory centers | Abnormal respiratory pattern Cushing reflex (bradycardia and hypertension) Cardiac arrest |
|
| Tonsillar Cerebellar tonsils pass through the foramen magnum and compress the medulla and cervicomedullary junction |
Cardiorespiratory center in the medulla | Abnormal respiratory pattern Cushing reflex (bradycardia and hypertension) Cardiac arrest |
| Motor control center | Decorticate or decerebrate posturing |
Following the introduction of ICP monitoring, and the finding that increased ICP may reduce CBF and that raised ICP (20–25 mm Hg) was associated with poor outcomes, protocol-driven strategies for controlling ICP and CPP in patients with brain injury have become a cornerstone in modern NCCUs.
Avoidance of cerebral ischemia is one of the critical aspects in limiting the impact of secondary brain or spinal cord injury. The brain lacks capacity for essential nutrient storage to be used for energy expenditure with minimal reserves of oxygen and energy substrates. The tolerance for reduction in CBF is therefore low.
The pathophysiologic processes underpinning ischemia and subsequent infarction are complex and interlinked but broadly speaking involve the following mechanisms: excitotoxicity, tissue acidosis, free radical production, inflammatory cascade activation, cerebral edema, apoptosis, and cell death.
The initial impairment in cerebral perfusion, ischemia, and the resultant lack of adenosine triphosphate (ATP) production results in a failure to maintain normal ionic gradients. Uncontrolled depolarization occurs, followed by the release of excitatory neurotransmitters (glutamate) and calcium. The excitotoxicity exacerbates the depolarization and drives other processes involved in cell necrosis and death. The absence of oxygen leads to tissue acidosis as a result of anaerobic metabolism and lactate production. The mechanism by which hyperglycemia results in poorer outcomes following neurologic injury is postulated to be because it provides a further substrate for continued anaerobic metabolism.
The excitotoxicity drives the activation of neuronal and inducible nitric oxide synthase (nNOS and iNOS, respectively) with the resultant NO production generating free radicals. Free radical–mediated DNA damage and damage to cell membranes result. Damage to cell membranes can further impact worsening ionic gradients by impairing protein channels involved in ionic transport. DNA damage and ischemia result in the activation of an inflammatory cascade via the up-regulation and nuclear transcription of pro-inflammatory cytokines (eg, adhesion molecules). Inflammatory cell recruitment and activation increase (eg, microglia), all of which continues the free radical–mediated injury.
The disruption of ionic transport mechanisms as a result of cell membrane injury precipitates uptake of fluid from extracellular spaces resulting in neuronal swelling even in the presence of an intact blood-brain barrier (cytotoxic edema). The subsequent breakdown of the blood-brain barrier then also leads to vasogenic edema, as unregulated transport of plasma proteins into cells occurs, increasing the osmotic drive for fluid influx. Cerebral edema increases ICP, worsens perfusion, and exacerbates ischemia.
The combination of excitotoxicity, tissue acidosis, free radical production, inflammatory activation, and cellular edema independently and in combination produce mitochondrial activation together with the release of cytochrome C from mitochondrial membranes (this also occurs due to mitochondrial membrane injury). The effect is activation of caspases and other proteolytic enzymes, which leads to apoptosis and cell death.
Many of the pathophysiologic processes described earlier that contribute to ischemia-related injury although damaging in the acute phase are also critical in the long term as the eventual healing and repair process begins with these mechanisms. The restoration of autoregulation including CO 2 reactivity and eventual healing with the formation of (usually nonfunctional) scar tissue may take from 4 to 6 weeks.
Global ischemia occurs with a global reduction in CBF (eg, hypoxic-ischemia injury secondary to cardiac arrest). Focal ischemia results when there is a focal reduction in blood flow in a major vessel: the infarct core is the region usually supplied by the smallest arterioles and end arteries that rapidly undergoes irreversible cell death; the surrounding penumbra is a zone where there is evidence of neuronal dysfunction and electrical silence, but it has not yet undergone depolarization, excitotoxicity, and irreversible cell death. This penumbra can be salvaged with restoration of CBF. Failure to restore perfusion will progressively incorporate the penumbra into the core infarct and increase its size. The vascular flow thresholds at which stepwise deterioration occurs vary depending on the basal metabolic activity of the region (eg, gray matter will intrinsically have higher metabolic rates and higher CBF requirements in comparison to white matter), but on average CBF < 8 to 10 mL/100 g of tissue/min results in irreversible neuronal death ( Table 26.2 ).
| Cerebral Blood Flow Threshold (mL/100 g of tissue/min) |
Impact on Neuronal Function |
|---|---|
| 30 | Minimum vascular flow rate for maintaining neuronal function |
| 20–30 | Neuronal dysfunction with EEG slowing |
| 10–20 | Reversible neuronal dysfunction with salvage possible on restoration of cerebral blood flow EEG suppressed, evoked potentials absent Continued progressive impairment of perfusion will result in delayed neuronal death |
| <10 | Irreversible neuronal dysfunction and cell death Total energy failure with loss of ionic balance, depolarization, and excitotoxicity |
The size of the penumbra and core depends on the strength of the collateral supply to the region, and principles underpinning the use of perfusion imaging are intended to help characterize the relative proportions of the core infarct versus the penumbra, which helps to predict the impact of salvage and reperfusion therapy and to guide prognosis.
A systematic approach is employed for assessing any critically ill neurosurgical patient. A variety of approaches exist, pioneered by trauma societies (Advanced Trauma Life Support [ATLS]), resuscitation councils (Advanced Life Support [ALS]), and critical care and surgical societies (Care of the Critically Ill Surgical Patient [CCrISP]). The basic principles are similar: a systematic, methodical, and reproducible approach to identify, resuscitate, and treat life-threatening insults in the most important sequence in which they occur—that is, airway (A), breathing (B) and respiratory function, circulatory (C) and cardiovascular function with fluid resuscitation, neurologic status and disability (D), and overall exposure (E) and assessment of other organ systems—the “ABCDE” approach. In trauma and neurosurgical patients, consideration is always given to the cervical spine, especially in patients at risk of spinal instability and spinal cord injury, and precautions are taken to preserve immobilization. Adherence to such a systematic method ensures that all practitioners have a methodical way to approach and assess any critically ill neurosurgical patient, identify physiologic derangement, and communicate with other medical personnel in a consistent manner while optimizing the patient's physiologic status. In neurosurgical patients, the goal is maintenance of cerebral (and spinal) oxygenation and perfusion, and control of intracranial pressure to limit secondary injury to the nervous system to achieve optimal outcomes.
Maintenance of a patent airway for adequate oxygenation is paramount: the brain is exquisitely sensitive to hypoxia and hypercapnia with significant effects on CBF, CPP, and ICP control. Deterioration in consciousness level also compromises the ability to protect the airway, increasing the risk of airway obstruction and aspiration. A variety of techniques exist for the purposes of airway control ranging from simple airway maneuvers (eg, “jaw thrust”), to the use of adjuncts (eg, oropharyngeal, nasopharyngeal, laryngeal mask airways), to definitive endotracheal intubation. Table 26.3 summarizes some indications to consider the use of intubation and mechanical ventilation in critically ill neurosurgical patients.
| System Affected | Examples of Pathologic Processes |
|---|---|
| A irway | Airway injury with risk of obstruction (eg, major neck trauma in context of head injury, burns with high risk of airway edema, anaphylaxis) |
| B reathing and respiratory dysfunction | Lung injury (eg, major trauma with pulmonary injury) Respiratory failure (eg, neurogenic pulmonary edema, infection and aspiration pneumonia, pulmonary venous thromboembolism) |
| C irculation and cardiovascular dysfunction | Impaired cardiac function (eg, major trauma with cardiac injury) |
| D isability and neurologic dysfunction | Loss of airway reflexes (eg, decreased consciousness level, brainstem or cranial nerve injury with lack of gag reflex, high cervical spinal cord injury) Intracranial pressure control Status epilepticus |
| E xposure and other organ systems | Acid-base dysfunction Severe sepsis |
In the elective postoperative phase, causes of airway obstruction may relate to airway edema or hematoma (eg, following anterior cervical spine approaches, carotid endarterectomy) or, in posterior fossa surgery, dysfunction of the brainstem and lower cranial nerves.
A rapid assessment of pulmonary function must be made to exclude any acute pulmonary causes for neurologic deterioration. In trauma patients in particular, acute life-threatening injuries such as tension pneumothorax, open pneumothorax, hemothorax, and flail chest must be excluded. In the early postoperative phase following elective surgery, pneumothorax may be a complication following central venous catheter insertion. In previously stable patients pulmonary infection, pulmonary edema (cardiac in origin or neurogenic secondary to a sympathetic surge following subarachnoid hemorrhage), and pulmonary venous thromboembolism are all important differentials to exclude with appropriately directed investigations in the setting of a pulmonary deterioration.
Ensuring stable hemodynamic function with adequate cerebral perfusion pressures is critical in neurosurgical patients. In patients with traumatic brain injury (TBI), severe hypotension (systolic blood pressure < 80 mm Hg) is a noteworthy independent factor contributing significantly to poor outcome and impacting mortality. Extrapolating this concept to ensure that hypovolemia and hypotension are identified and rapidly corrected in most neurosurgical pathologies is of paramount importance. In patients with cerebral vasospasm following subarachnoid hemorrhage, hypovolemia and hypotension can accelerate ischemic injury. In trauma patients, cardiac tamponade should be excluded.
Although a degree of hypertension may be tolerated—in patients with raised ICP, mass lesions, or subarachnoid hemorrhage, an intensive sympathetic activation may occur to drive cerebral perfusion pressures and maintain cerebral blood flow—significant hypertension (eg, systolic blood pressure > 180 mm Hg or mean arterial pressures > 120 mm Hg) itself may lead to adverse neurologic outcomes especially in the context of intracranial hemorrhage (eg, the presence of ruptured unsecured aneurysms) or in the early postoperative phase following cranial or spinal surgery, where operative hemostasis may be disrupted and precipitation of hemorrhage within surgical field may occur.
Causes for cardiac dysfunction may include primary cardiac pathologies (eg, myocardial infarction especially in patients with preexisting cardiovascular morbidities), hemorrhage in other organ systems in the setting of major trauma (eg, abdominal injuries, pelvic injuries), or may be related to sepsis or neurology (raised ICP, brainstem dysfunction, excessive sympathetic activation following subarachnoid hemorrhage, spinal cord injury with neurogenic shock, sympathetic disruption, and autonomic hyperreflexia following spinal injury). Fluid resuscitation together with cardiorespiratory support with invasive hemodynamic monitoring and inotropic support may be indicated.
Neurologic assessment in a critically ill neurosurgical patient must be rapid but systematic and focused. Airway protection, oxygenation, and optimization of hemodynamic status and cerebral perfusion should have already occurred as detailed earlier. Evaluation must include (1) an assessment of consciousness level; (2) pupillary size, light response, and reactivity; and (3) motor assessment of upper and lower extremities. More detailed and complete examination (eg, complete cranial nerve function, detailed cognitive assessment) should be performed if the hemodynamic and neurologic stability of the patient permits.
A variety of scores exist for evaluating consciousness level. The Glasgow Coma Score (GCS) is one example. Strengths include the ease of application, good inter- and intraobserver reproducibility, and its ability to capture neurologic deterioration anatomically based on the sequential structures affected, and the fact that motor score in particular correlates with prognosis and outcome. Limitations such as the inability to evaluate the verbal component in intubated patients and lack of assessment and incorporation of brainstem reflexes have resulted in the development of other tools (eg, the FOUR Score). Nonetheless the GCS remains one of the most widely used scores for urgent assessment of consciousness level and neurologic deterioration, as well as patient stratification in research ( Table 26.4 ).
| Component Assessed | GCS | FOUR | |
|---|---|---|---|
| Eyes | 4 | Open spontaneously | Open, tracking, blinking to command |
| 3 | Open to voice | Open, not tracking | |
| 2 | Open to pain | Open to loud voice | |
| 1 | Closed | Open to pain | |
| 0 | N/A | Closed | |
| Total Eye Score | 4 (min = 1; max = 4) | 4 (min = 0; max = 4) | |
| Verbal | 5 | Alert and orientated to time, place, and person | Not incorporated |
| 4 | Confused conversation | ||
| 3 | Inappropriate words | ||
| 2 | Inappropriate sounds | ||
| 1 | No verbalization | ||
| 0 | N/A | ||
| Total Verbal Score | 5 (min = 1; max = 5) | ||
| Motor | 6 | Obeys commands | N/A |
| 5 | Localizes to painful stimulus | ||
| 4 | Withdraws to painful stimulus | Thumbs up, fist, peace sign | |
| 3 | Abnormal flexion response (decorticate posture) | Localizes to painful stimulus | |
| 2 | Abnormal extension response (decerebrate posture) | Flexion response to pain | |
| 1 | No response | Extension response to pain | |
| 0 | N/A | No response or generalized myoclonic response | |
| Total Motor Score | 6 (min = 1; max = 6) | 4 (min = 0; max = 4) | |
| Brainstem reflexes | 4 | Not incorporated | Pupil and corneal reflex present |
| 3 | 1 pupil fixed and dilated | ||
| 2 | Pupil or corneal reflex absent | ||
| 1 | Pupil and corneal reflex absent | ||
| 0 | Absent pupil, corneal, and cough reflexes | ||
| Total Score | 4 (min = 0; max = 4) | ||
| Respiration | 4 | Not incorporated | Not intubated, regular breathing |
| 3 | Not intubated, Cheyne-Stokes respiration | ||
| 2 | Not intubated, irregular breathing | ||
| 1 | Intubated, triggering breaths on ventilator | ||
| 0 | Intubated, not triggering breaths on ventilator | ||
| Total Score | 4 (min = 0; max = 4) | ||
| TOTAL Score | Out of 15 Max = 15 Min = 3 |
Out of 20 Max = 20 Min = 0 |
|
The causes of neurologic deterioration and impairment in consciousness level may be structural (with specific neurosurgical pathologies having stereotypical complications that need to be excluded; Table 26.5 ) or secondary to seizures or other metabolic and physiologic factors (eg, airway related, hypoxia, hypercapnia, hemodynamic abnormalities, temperature, electrolytes, blood glucose, acid-base dysfunction, and pharmacologic including hypnotic, sedative, and opioid excess).
| Neurosurgical Pathology | Possible Cause for Neurologic Deterioration |
|---|---|
| Traumatic brain injury |
|
| Aneurysmal subarachnoid hemorrhage |
|
| Intracerebral hemorrhage |
|
| Cerebellar hemorrhage |
|
| Postoperative (eg, resection of tumor, spinal decompression) |
|
Deterioration may manifest itself clinically with a progressive or sudden change in consciousness level or features of cerebral herniation (see Table 26.1 ). In intubated and ventilated patients, neurologic deterioration may manifest with the progressive changes in invasive monitoring parameters (ICP, PbtO 2 , or hemodynamics). In awake patients, clinical features of raised intracranial pressure include headache, nausea, and vomiting; neurologic deficits including false localizing signs (eg, sixth cranial nerve palsy secondary to generalized increase in ICP); and papilledema (a late sign). The absence of papilledema does not exclude raised ICP. Its presence is merely indicative of chronically elevated intracranial pressure with transmission through the optic nerve sheath in communication with the subarachnoid space. Radiologic correlates of raised ICP on imaging that must be identified when assessing imaging in neurologically deteriorating patients are based on the neurophysiologic compensatory measures: displacement of intracranial CSF into lumbar cisterns manifests as loss of sulcal CSF spaces, obliteration of basal cisterns, collapsed and slit-like ventricles; cerebral herniation syndromes may be manifest on radiologic imaging such as uncal herniation across the tentorium, subfalcine and tonsillar herniation, and brainstem compression at the foramen magnum.
The aim is to confirm that deterioration has occurred, to identify possible causes including the use of diagnostic imaging where required (eg, CT, MRI), and to anticipate the need for either surgical intervention or admission to, and management in, a neurocritical care setting if indicated.
Exposure entails a rapid assessment of the other major organ systems and correction of any other parameters that may be relevant in critically ill neurosurgical patients that may affect the outcome and possible neurosurgical intervention. For example, in patients with spinal cord injury, decompression of the gastric contents and bladder is imperative to avoid possible complications secondary to autonomic hyperreflexia. Other common considerations include an assessment of electrolytes, glucose and renal function, hematologic parameters that may increase risk of hemorrhage (eg, thrombocytopenia, pharmacologic anticoagulants), and excessive use of pharmacologic agents (eg, opioid overdose).
A variety of neurosurgical patients may require admission to an NCCU. These include (1) patients in the immediate postoperative phase following either elective or emergency surgery, (2) previously stable patients with a neurologic or systemic deterioration that require intensive care–level monitoring and management, and (3) critically ill neurosurgical patients admitted directly due to the severity of their condition. As with the assessment of a critically ill neurosurgical patient, a systematic approach is required when evaluating and managing patients in the NCCU to ensure that physiologic parameters are optimized and that there is close monitoring to detect any neurologic deterioration and achieve optimal outcomes. The mnemonic “ABCDE FLAT HUGS” is an aide-memoire of the critical parameters that require regular assessment ( Table 26.6 ).
| System | Parameters |
|---|---|
| A — A irway | Adequacy of airway, type of airway (eg, endotracheal tube, tracheostomy) |
| B — B reathing | Respiratory rate, oxygen saturation (SaO 2 ), PaO 2, PaCO 2 , acid-base status (pH, lactate, bicarbonate) |
| C — C irculation and c ardiovascular | Heart rate, rhythm, blood pressure |
| D —Neurologic d isability | Consciousness level (Glasgow Coma Score/FOUR Score), pupil size, symmetry and reactivity, peripheral limb motor and sensory function |
| E — E xposure and other organ systems | Temperature, renal function, electrolytes, fluid balance and urine output |
| F — F eeding | Enteral feeding if possible (or parenteral nutrition) |
| L — L ines and invasive monitoring | Invasive monitoring (if indicated): central venous pressure catheter, arterial line for invasive blood pressure, pulmonary artery catheter, urinary catheter |
| A — A nalgesia, a ntiepileptics, a ntimicrobials | Analgesia—verbal or visual scales for assessment, World Health Organization (WHO) analgesic ladder Antiepileptics—appropriate seizure control Antimicrobials—monitoring and treatment of infection |
| T —Venous t hromboembolism prophylaxis | Mechanical prophylaxis—thromboelastic stockings, pneumatic compression devices Pharmacologic prophylaxis (if indicated)—low-molecular-weight heparin, unfractionated heparin |
| H — H ead up and ICP stabilization measures | Elevate the head above heart and protocol driven strategy for ICP control |
| U — U lcer (gastric) prophylaxis and nausea/vomiting | Gastric protection against stress ulceration (eg, proton-pump inhibitors) and antiemetics |
| G — G lycemic control | Maintain glucose within normal range (4.4–8.3 mmol/L; 80–150 mg/dl) |
| S — S pecific neurologic monitoring and neurosurgical pathology-related concerns | Neurologic monitoring—ICP, SjvO 2 , PbtO 2 , TCD Special concerns depending on neurosurgical pathology (eg, postoperative steroids and electrolytes, osmolality and fluid balance following pituitary surgery) |
Hypoxia is a significant independent risk factor for worse outcomes and increasing mortality in the context of patients with traumatic brain injury. Critically ill neurosurgical patients should have a definitive assessment of airway patency, and steps should be taken to ensure it is secured as soon as possible.
Total O 2 content within the blood is based on (1) the amount of O 2 dissolved in plasma (as per Henry's law, dependent on the solubility of O 2 and PaO 2 ) and (2) the O 2 –carrying capacity of hemoglobin (dependent on SaO 2 and the concentration of hemoglobin). Assuming a temperature of 37°C and a hemoglobin concentration ([Hb]) of 150 g/L, in arterial blood (with SaO 2 97% and PaO 2 13.3 kPa), there are approximately 200 mL of O 2 /L; in mixed venous blood (SaO 2 75% and PaO 2 5.6 kPa) there are 150 mL of O 2 /L. The degree of oxygen flux and usage is approximately 50 mL/L. With a cardiac output of 5 L/min, the oxygen flux and usage are 250 mL/min. Hence it is imperative to understand that oxygen delivery depends on temperature (which determines the solubility of O 2 ), cardiac output, PaO 2 and SaO 2 , and hemoglobin concentration. The meticulous optimization of these parameters is vital to ensure adequate cerebral oxygenation and perfusion and therefore limit secondary injury.
The aim should be to provide adequate oxygenation and avoid hyper- or hypocapnia. Targets vary depending on the patient comorbid status, the presence of preexisting respiratory comorbidities, and clinical status, but where feasible, the aims should be oxygen saturation (SaO 2 ) ≥ 97%, PaO 2 ≥ 11 to 13 kPa, and PaCO 2 4.7 to 5.3 kPa (normocapnia). Mechanisms to increase oxygenation include increasing the inspired oxygen fraction (FiO 2 ), increasing the inspiratory time to expiratory time cycling (IT : ET ratio from 1 : 2 to 2 : 2, respectively), and applying positive end-expiratory pressure (PEEP ≤ 10 mm Hg). Peak inspiratory pressures should not exceed 35 mm Hg to ensure minimal interference with cerebral venous drainage.
Prophylactic hypocapnia via hyperventilation (minute ventilation [MV] = tidal volume [V T ] × ventilatory rate [V R ]) should be avoided, as it causes cerebral vascular vasoconstriction with the risk of worsening cerebral ischemia. For the purposes of ICP control, it is a short-term measure only until more definitive measures to control ICP are instituted. Patients that are intubated and on mechanical ventilation should have adequate sedation (intravenous hypnotic; eg, propofol, midazolam), analgesia (eg, opioid), and, if needed, a neuromuscular blocking agent to avoid ventilator-associated stress, gag, and the patient fighting against the ventilator—all of which can precipitate systemic hypertension, distress, and, via the transmission of increased intrathoracic pressures, an increase in ICP.
Attempts to wean the patient off the ventilator as soon as clinically feasible and aim for extubation should be considered. There are multiple benefits to this strategy, including the ability to perform a clinical neurologic examination and reduce the risk of ventilator-associated complications including ventilator-associated pneumonia (VAP). There are significant differences in the majority of critically ill neurosurgical patients in comparison to patients in general critical care units : most will have normal baseline pulmonary function tests (except elderly patients with preexisting chronic obstructive pulmonary disease); most will require only synchronized intermittent mandatory ventilation (SIMV) or pressure support ventilation (PSV); and other strategies such as prone ventilation, permissive hypercapnia, and inverse ratio ventilation are usually avoided and rare. As such, ventilator dependence is less common with rapid weaning expected.
Exceptions may be patients with significant polytrauma or high cervical spinal cord injury. In situations where a prolonged period of mechanical ventilation is anticipated, consideration should be made for early tracheostomy (performed as an open surgical procedure or percutaneous). Benefits include increasing patient comfort and ability to tolerate tracheal tubes without significant gag, thereby allowing neurologic examination without sedation to occur more easily, improved length of NCCU stay, more effective airway clearance and bronchial toilet of secretions, and a decreased risk of tracheolaryngeal stenosis secondary to prolonged intubation.
Apart from some specific circumstances (eg, aSAH-associated vasospasm where hypervolemia may be indicated), in most critically ill neurosurgical patients, the aim is to arrive at normovolemia and normotension to achieve stable cerebral perfusion. Basic equations pertaining to cardiovascular function include the following:
Cardiac output (CO) = Stroke volume (SV) × Heart rate (HR)
Blood pressure (BP) = Systemic vascular resistance (SVR) × Cardiac output (CO)
Pulse pressure (PP) = Systolic blood pressure (SBP) – Diastolic blood pressure (DBP)
Mean arterial pressure (MAP) = ( ![]() DBP +
DBP + ![]() SBP) or (DBP +
SBP) or (DBP + ![]() PP)
PP)
Circulatory and fluid status and cardiovascular function may be monitored using noninvasive or invasive means, and this involves a combination of clinical and biochemical parameters. Clinical parameters include body weight, HR, BP, and hourly assessment of input-output fluid balance including urinary output. Biochemical parameters include hematocrit, acid-base status including lactate, electrolytes (sodium), renal function (urea and creatinine), serum and urine osmolalities, and urine specific gravity. Invasive hemodynamic monitoring techniques include the use of central venous pressure (CVP) or, in certain circumstances, pulmonary artery flotation catheters (PAFCs). The former is especially useful to guide the adequacy of fluid resuscitation especially in circumstances where osmotic diuresis (eg, mannitol, furosemide) is used in ICP control, which makes use of urine output less reliable. The latter allows for the calculation of a variety of hemodynamic parameters including SVR, CO, and pulmonary artery capillary wedge pressure (PACWP)—all of which become important especially in the context of guiding fluid therapy and inotrope use. Trends of CVP and PACWP rather than absolute values are more indicative of fluid status. Some critical care specialists recommend the use of pulse pressure variability (% PPV) or systolic blood pressure variability (% SBPV) as a better predictor of response to fluid therapy.
In most neurosurgical pathologies, the aim of fluid resuscitation and management should be to achieve normovolemia, normal electrolytes, normal serum osmolalities, and normoglycemia. Daily fluid requirements are approximately 40 mL/kg/24 hr with hourly requirements calculated as (1) 4 mL/kg for every kilogram from 0 to 10 kg of body weight, (2) 2 mL/kg for every kilogram from 11 to 20 kg of body weight, and (3) 1 mL/kg for every kilogram of body weight from 20 kg onward. A urine output of 1 mL/kg/hour should be the aim to avoid oliguria. Fluid management should also take into consideration variable factors such as the impact of temperature, fever, and respiratory dysfunction on increasing insensible fluid losses; the impact of anesthesia and sedation-induced cardiac depression and vasodilation; preoperative or perioperative deficits; and the redistribution of third space fluid losses. The daily sodium requirement is 1 to 2 mmol/kg (or mEq/kg), and the daily potassium requirement is 0.5 to 1 mmol/kg (or mEq/kg).
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here