Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The atlantoaxial joint is the most mobile and the most unstable joint of the body.
The round and flat articular surface of the joint allows circumferential movements but makes it susceptible to instability.
Apart from the more commonly identified anteroposterior type, atlantoaxial instability can also be rotatory, lateral, vertical, or translatory.
Atlantoaxial instability can be diagnosed on the basis of an abnormal increase of atlantodental interval and also on the basis of abnormalities in facetal alignment.
Atlantoaxial instability can be the nodal point of pathogenesis of a number of common clinical entities like basilar invagination, Chiari malformation, syringomyelia, cervical spondylosis, and ossification of the posterior longitudinal ligament.
The craniovertebral junction is a complex formation whose architecture perfectly caters to the needs of the strongest and most mobile regions of the spine and allows free passage to the most critical neural and vascular structures. The human spinal pillar has a Y-shaped configuration. The rostral “V” of the “Y,” which is composed of the suboccipital bone, the atlas vertebra, and the axis vertebra, constitutes the craniovertebral junction. Although the occipitoatlantal joint is the strongest joint, the atlantoaxial joint is the most mobile joint of the spine. Mobility and stability are the hallmarks of the craniovertebral junction.
The occipitoatlantal joint is the most stable joint, and instability of this joint is extremely rare. On the other hand, the flat and round articular surfaces that cater to circumferential movements at the atlantoaxial joint also make it susceptible to instability. The term craniovertebral instability can be synonymous with atlantoaxial instability because, whereas atlantoaxial instability is relatively common, occipitoatlantal instability is significantly infrequent and is only rarely identified in cases with severe trauma and in children who are affected in a “syndromic” manner. It may not be incorrect to state that atlantoaxial instability is the most common spinal instability.
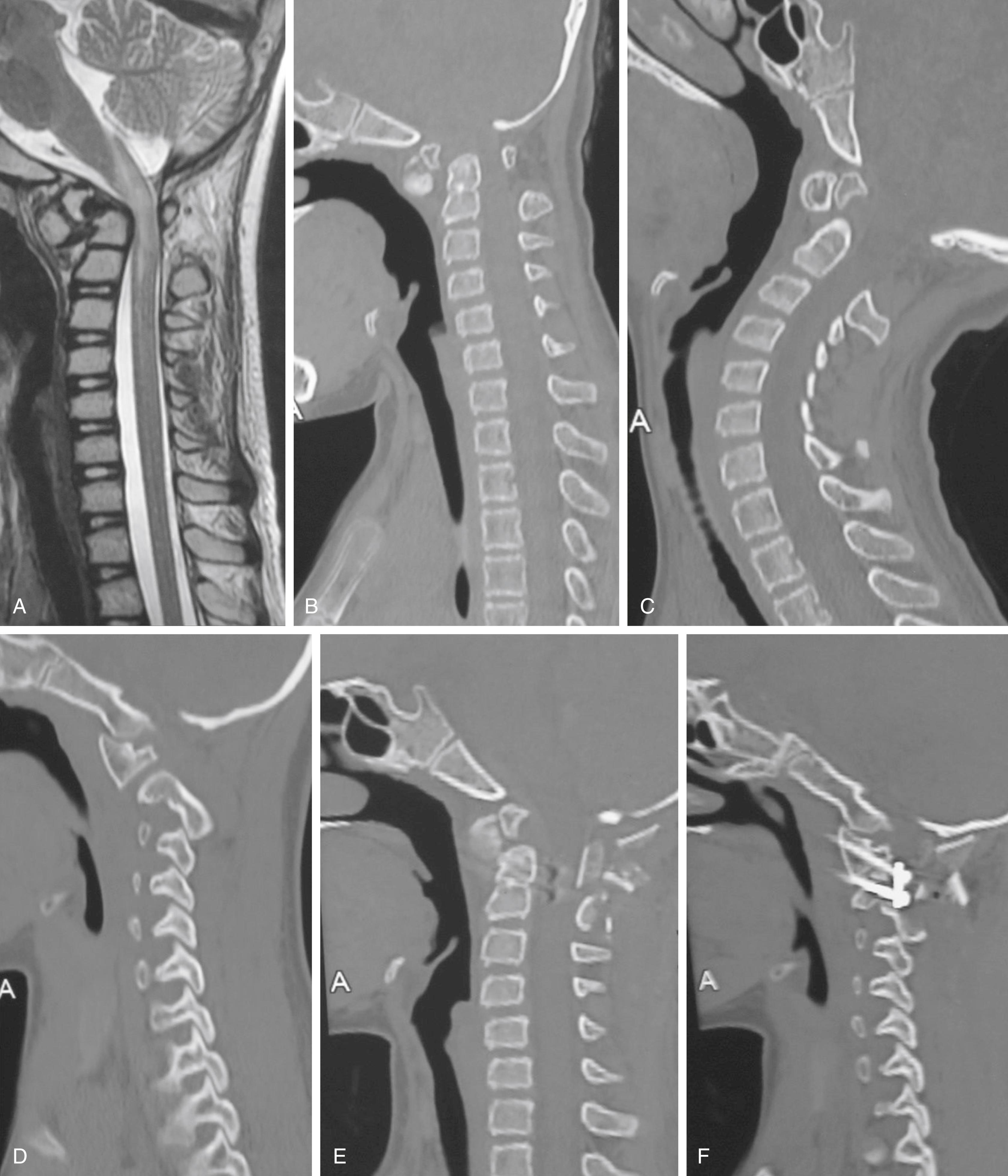
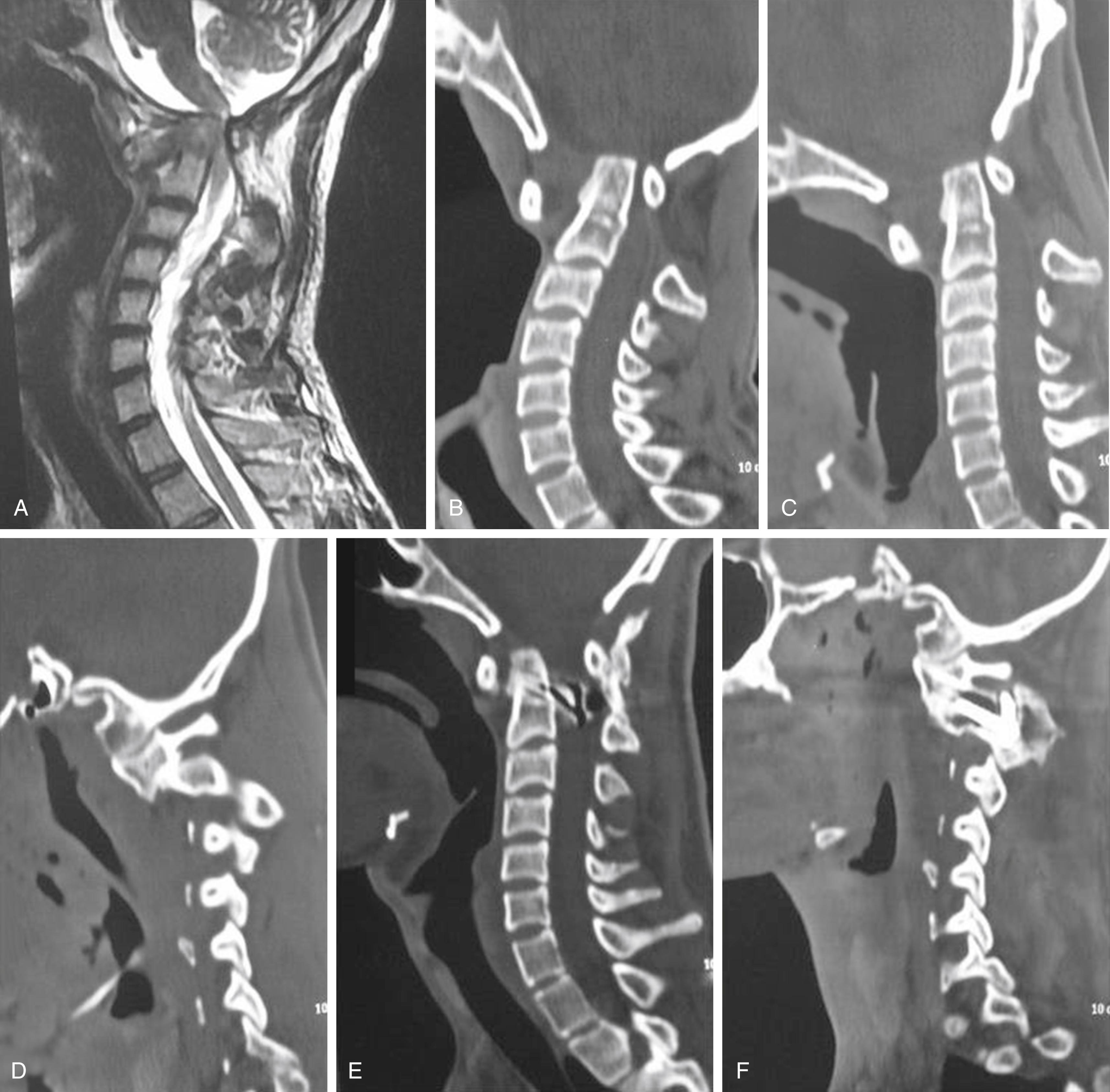
Computerized imaging has drastically changed the preoperative assessment of patients with atlantoaxial dislocation from the era when only plain radiology was available to investigate and diagnose atlantoaxial dislocation. An abnormal increase in the atlantodental interval on dynamic lateral radiographs with the head in flexion and extension has been the determining criterion for diagnosing atlantoaxial instability. An increase in the atlantodental interval of more than 3 mm on flexion of the head is considered to be diagnostic of atlantoaxial instability. In children, an atlantodental interval of more than 5 mm is generally considered to indicate the presence of atlantoaxial instability. When the atlantodental interval reduces on extension, the atlantoaxial dislocation is “mobile” and “reducible” , ( Fig. 24.1 ). If the dislocation reduces only partially on extension, the dislocation is called “partially reducible” atlantoaxial instability. If the dislocation does not reduce on extension, it is labeled as “fixed” or “irreducible” atlantoaxial instability ( Fig. 24.2 ). Modern computer-based imaging identifies instability by direct evidence of dural and neural compression opposite the odontoid process. The treatment protocol for craniovertebral junction instability has essentially been based on this premise for over 50 years. Although atlantoaxial fixation was recommended for mobile and reducible atlantoaxial dislocation, anterior transoral or posterior foramen magnum “decompression” surgery was recommended when the atlantoaxial dislocation was “fixed” or “irreducible.”
Rotatory atlantoaxial dislocation occurs when the facet of the atlas is dislocated posteriorly in relation to the facet of the axis on one side and anteriorly on the contralateral side. Depending on the location of the facets, rotatory atlantoaxial dislocation can be of various types, namely, complete or incomplete. Such a dislocation results in painless torticollis; it is usually identified in young children. The child presents with the head in a typical “cock robin” position. As there is no pain, neural deficit, or other symptom, and the only problem is abnormal neck posture, the management of such cases needs to be precise and based on understanding of biomechanics of the region.
This type of dislocation is diagnosed when, on flexion of the head, the odontoid process migrates rostrally without affecting the atlantodental interval ( Fig. 24.3 ). Vertical dislocation can be mobile, reducible, or fixed.
When the facet of atlas is dislocated lateral to the facet of axis, it is labeled as lateral atlantoaxial dislocation. Such dislocation is more commonly seen when the arch of the atlas is fractured or is bifid, and the two segments of atlas are consequently dislocated laterally in relationship with the facet of the axis.
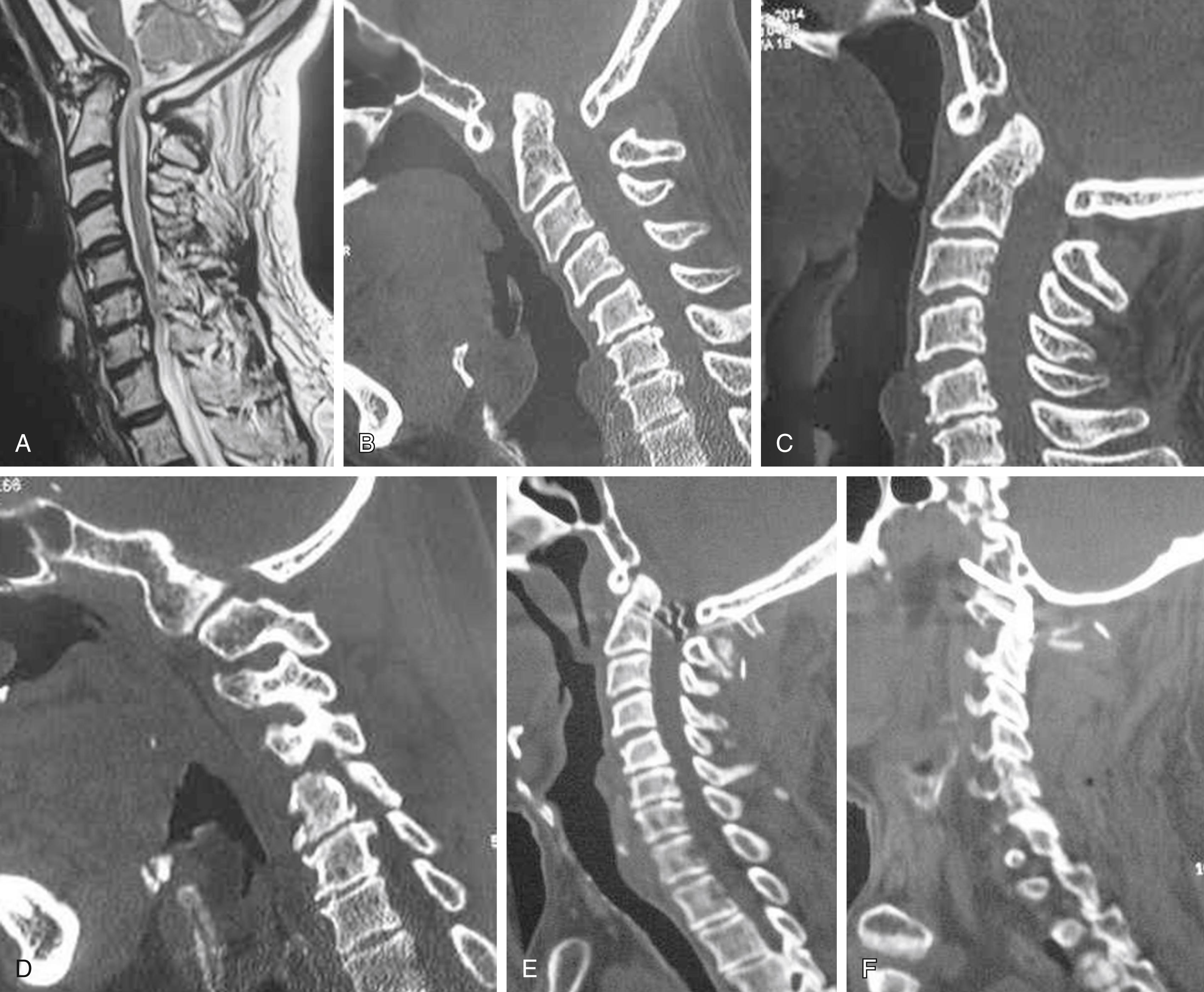
Goel recently classified atlantoaxial dislocation on the basis of alignment of facets on the lateral profile imaging with the head in neutral position. Type 1 atlantoaxial facetal instability is when the facet of the atlas is dislocated anterior to the facet of the axis. Type 2 atlantoaxial facetal instability is when the facet of the atlas is dislocated posterior to the facet of the axis. Type 3 atlantoaxial instability is when the facets of the atlas and axis are in alignment, and instability is diagnosed only on the basis of a high degree of clinical suspicion and confirmed by direct manual manipulation of bones during surgery. Because the atlantodental interval may not be altered, and there may not be any dural or neural compression opposite the odontoid process, type 2 and type 3 atlantoaxial facetal instability are sometimes labeled as “central” or “axial” atlantoaxial instability. Neural compression is a hallmark of type 1 atlantoaxial facetal dislocation, and the presenting symptoms are relatively acute. On the other hand, the presenting symptoms in types 2 and 3 are usually chronic or longstanding. In chronic and longstanding atlantoaxial dislocation, protective or reparative natural changes in the musculoskeletal and neural structures are prominent. Such changes include the complex of basilar invagination, Chiari formation, and syringomyelia.
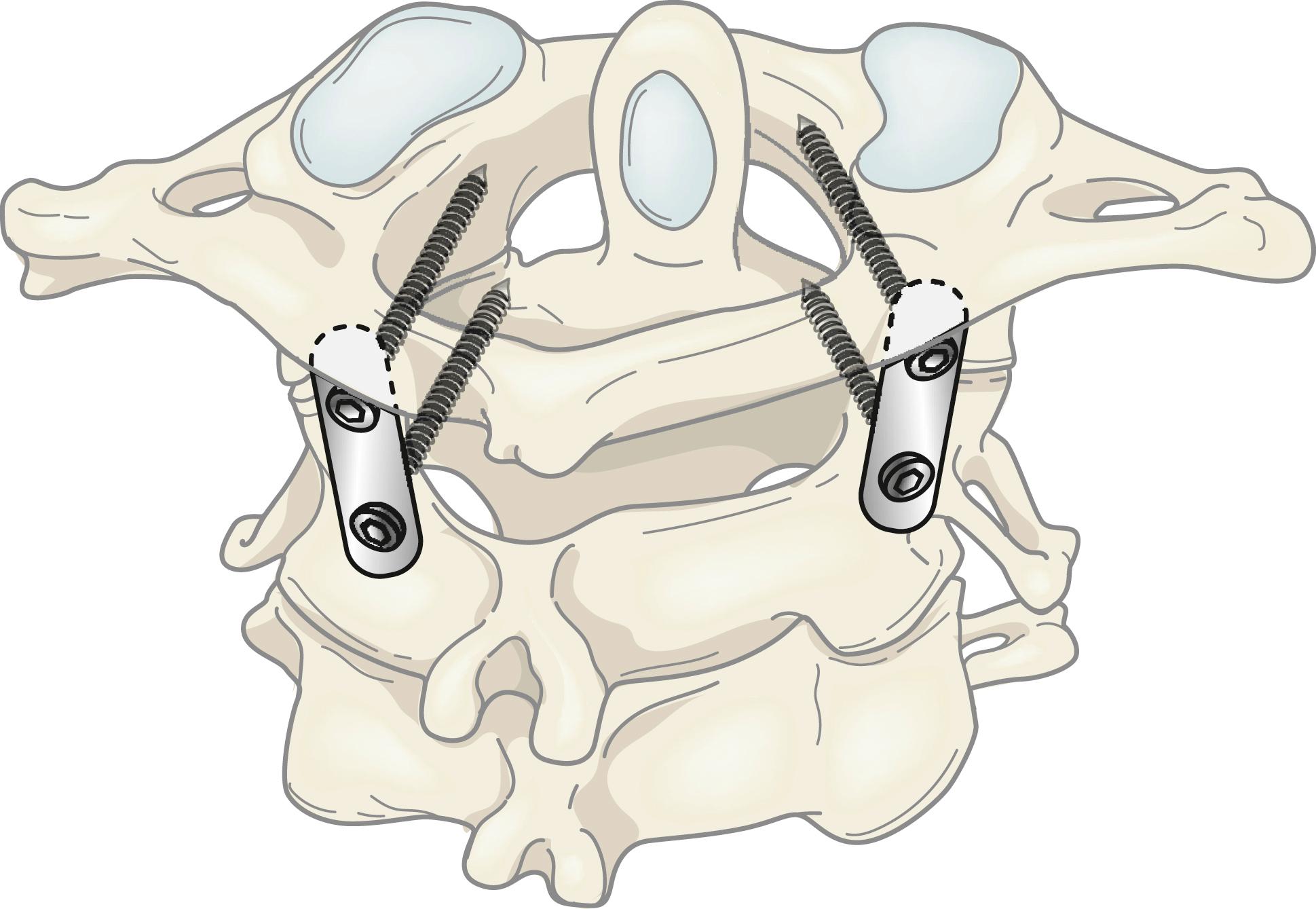
Atlantoaxial stabilization is a complex surgical procedure. The surgery requires thorough anatomic familiarity with the region and has to be done precisely, under “microscopic” vision, and effectively. No compromises are usually accepted. The primary aims of surgery are to remove or denude the articular cartilage of the atlantoaxial articulation, introduce bone graft within the articular cavity, and subsequently perform metal fixation that will stabilize the region and permit bone fusion. , Additionally, all muscles attached to the large C2 spinous process have to be sectioned. The muscles are normally so strong that they can break any metal implant. The aim of the surgical procedure is to achieve solid arthrodesis of the atlantoaxial joint. Elimination of a source of power by sectioning the muscles and paralyzing the fulcrum of activity at the joints by denuding the articular cartilage and packing with bone graft are critical surgical steps. The metal implant has to be strong and capable to provide “zero” movement for a period of about 2 months and provide an opportunity for bone healing. Subsequently, the fused bone will hold the implant, and metal hold is unnecessary. Whilst successful surgery can be gratifying both to the patient and to the treating surgeon, any complication can be equally devastating. Essentially, all surgical steps should be clearly understood and precisely performed.
Atlantoaxial instability is the issue, and atlantoaxial stabilization is the treatment. A fixation procedure that involves only the atlantoaxial segment is biomechanically most stable. Inclusion of the occipital bone and the subaxial bone increases the length of the metal implant and unnecessarily stabilizes normally functioning spinal segments. The long implant is biomechanically weak and has the potential to weaken, as bone fusion at multiple spinal segments is a difficult goal to achieve. Bone harvested from the patient’s own iliac crest has been universally identified to be superior to any other form of bone graft or artificial material.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here