Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Approximately 45% of all pregnancies in the United States are unintended, and among women who experience unintended pregnancy, more than half are not using contraception. By age 45, at least half of U.S. women will experience an unintended pregnancy, and one in four will have had an abortion.
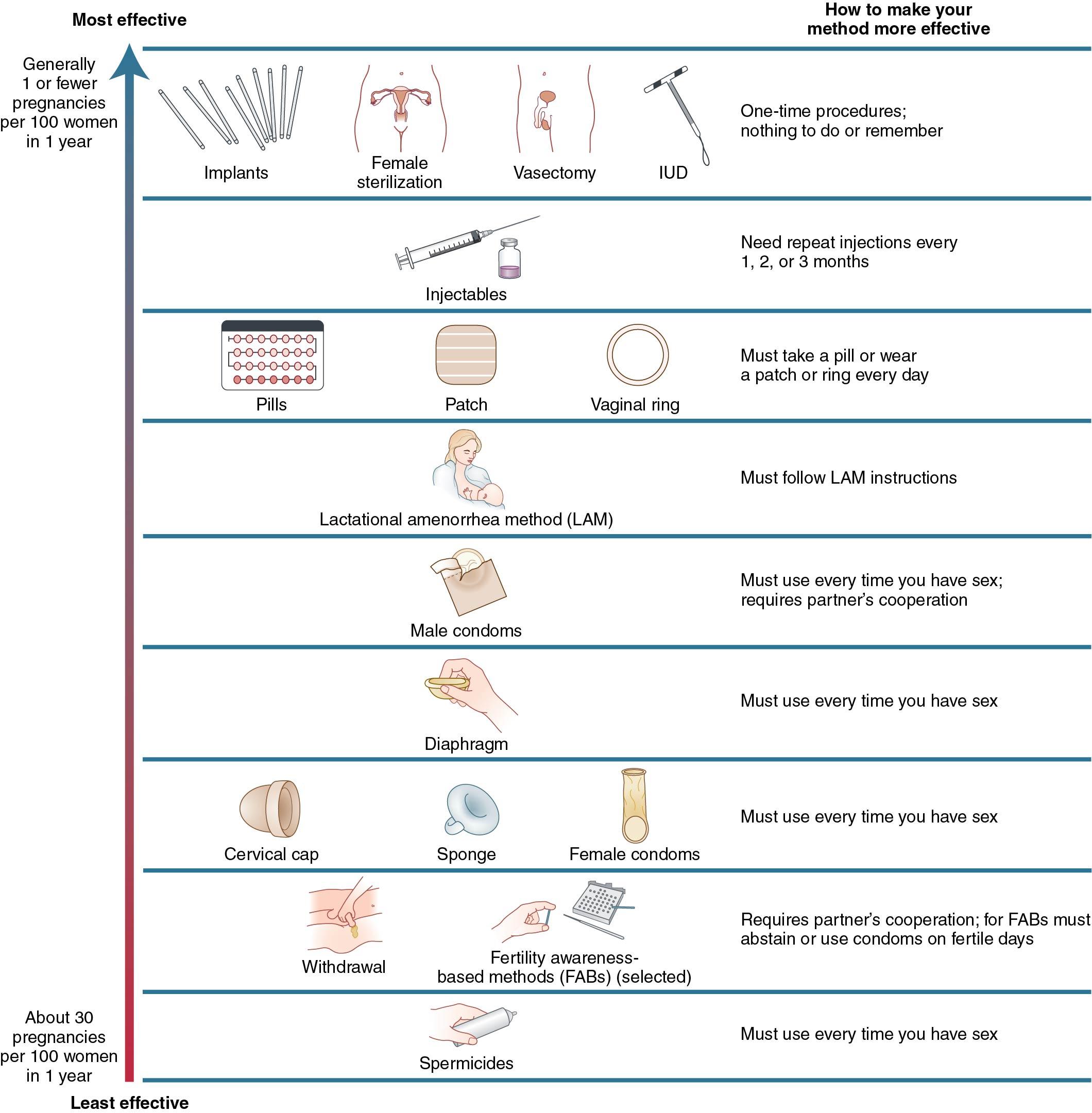
Failure rates in the first year of contraceptive use are highest for coitus-related methods (e.g., withdrawal, periodic abstinence, condoms, barrier methods) followed by combined contraceptives (pill, patch, ring) and the progestin injection. Intrauterine devices (IUDs), implants, and sterilization have typical use failure rates of less than 1%, similar to that of sterilization.
Combined hormonal contraceptives increase a woman’s risk of venous thromboembolism (VTE) about threefold to approximately 1 in 1000 per year. Women with risk factors for VTE or cardiovascular disease (e.g., obesity, age older than 35, smoking, a personal or family history of clotting disorder) should use effective birth control methods without estrogen.
The most effective method of emergency contraception is the copper IUD, followed by a single dose of oral ulipristal acetate. An oral dose of levonorgestrel is somewhat less effective but available over the counter.
First- and second-trimester medical and surgical abortions are common and safe. Overall, abortions have a lower complication risk than carrying a pregnancy to term. Access to legal and safe abortion is a cornerstone of maternal health.
Contraception is nearly a universal health care need among those who can become pregnant . About 99% of women aged 15 to 44 who have ever had sexual intercourse report use of at least one contraceptive method at some point ( ). In the United States, 70% of the 64 million women aged 15 to 44 are at risk of unintended pregnancy; they are sexually active, not infertile, and not trying for pregnancy. Of those at risk, about 10% do not use contraception. About 45% of pregnancies in the United States are unintended, and among women who experience unintended pregnancy, more than half are not using contraception ( ).
Tubal sterilization (18.6%), the oral contraceptive pill (12.6%), long-acting reversible contraceptive (LARC) methods (10.3%), and condoms (8.7%) comprise the most commonly used methods ( Table 13.1 ) ( ). Distinct advantages and disadvantages characterize contraceptive methods. Clinicians should be able to explain the unique features of each method, must identify medical contraindications to a given method and offer safe and effective alternatives, and should keep the risks of pregnancy in mind when discussing methods. For healthy women, and especially for medically challenging patients, pregnancy risks generally exceed risks related to contraception.
| Characteristic | % |
|---|---|
| Using contraception | 64.9 |
| Female sterilization | 18.6 |
| Male sterilization | 5.9 |
| Pill | 12.6 |
| Male condom | 8.7 |
| Long-acting reversible contraceptives | 10.3 |
| Depo-Provera, contraceptive ring, or patch | 3.2 |
| All other contraceptive methods | 5.6 |
| Not using contraception | 35.1 |
| Never had sexual intercourse or did not have sex in the past 3 months | 17.0 |
| Pregnant, postpartum, or seeking pregnancy | 7.5 |
| Nonuser who had sexual intercourse in the past 3 months | 7.9 |
| All other nonusers | 2.7 |
Health care outcomes improve when provider counseling incorporates patient preferences. In contraception counseling, communication between the patient and provider can affect initiation and continuation of birth control. Most women value personal autonomy when making decisions about contraception more than they do in other areas of medicine ( ).
Shared decision making (SDM) provides a useful counseling tool. Using this model, the clinician contributes medical expertise, and the patient contributes her values and preferences. Priorities vary; therefore counseling should be tailored to each individual woman. SDM works particularly well in contraception counseling because most methods of birth control are safe for most women. A shared decision-making approach correlates with improved patient satisfaction compared with decisions driven solely by the provider or the patient ( ).
Most women initiating contraception are healthy, and in general the risks of pregnancy outweigh the risks of most contraceptive methods. However, there are certain medical conditions that may contraindicate using a particular method. The health care provider must be aware of these specific contraindications to ensure that a given method is both acceptable to the patient and safe.
The World Health Organization (WHO) publishes detailed guidelines listing the medical eligibility criteria for the use of individual contraceptive methods. These regularly updated guidelines can be downloaded from the WHO website ( www.who.int/reproductivehealth ) ( ). The Centers for Disease Control and Prevention (CDC) also publishes regularly updated medical eligibility criteria tailored to U.S. practice; CDC guidelines are available for download along with a companion app ( www.cdc.gov/reproductivehealth ) ( ).
All contraceptive methods have a typical use effectiveness (pregnancy rate given actual, real-life conditions including occasional inconsistent or incorrect use) and perfect use effectiveness (pregnancy rate given correct and consistent use with every act of intercourse). Pregnancy rates can vary widely between typical and perfect use depending on the method ( Table 13.2 ). In general, coitus-related methods and more user-dependent methods are less effective than “forgettable methods” such as LARC. Combining any method with a condom decreases the risk of sexually transmitted infection acquisition.
| Method | % of Women Experiencing an Unintended Pregnancy Within the First Year of Use | % of Women Continuing Use at 1 Year ‡ | |
|---|---|---|---|
| Typical Use * | Perfect Use † | ||
| No method § | 85 | 85 | |
| Spermicides ∥ | 21 | 16 | 42 |
| Female condom ¶ | 21 | 5 | 41 |
| Withdrawal | 20 | 4 | 46 |
| Diaphragm ** | 17 | 16 | 57 |
| Sponge | 17 | 12 | 36 |
| Parous women | 27 | 20 | |
| Nulliparous women | 14 | 9 | |
| Fertility awareness–based methods †† | 15 | 47 | |
| Ovulation method † | 23 | 3 | |
| TwoDay method † | 14 | 4 | |
| Standard Days method † | 12 | 5 | |
| Natural Cycles †† | 8 | 1 | |
| Symptothermal method †† | 2 | 0.4 | |
| Male condom ¶ | 13 | 2 | 43 |
| Combined and progestin-only pills | 7 | 0.3 | 67 |
| Evra patch | 7 | 0.3 | 67 |
| NuvaRing | 7 | 0.3 | 67 |
| Depo-Provera | 4 | 0.2 | 56 |
| Intrauterine contraceptives | |||
| ParaGard (copper T) | 0.8 | 0.6 | 78 |
| Skyla (13.5 mg LNG) | 0.4 | 0.3 | |
| Kyleena (19.5 mg LNG) | 0.2 | 0.2 | |
| Liletta (52 mg LNG) | 0.1 | 0.1 | |
| Mirena (52 mg LNG) | 0.1 | 0.1 | 80 |
| Nexplanon | 0.1 | 0.1 | 89 |
| Tubal occlusion | 0.5 | 0.5 | 100 |
| Vasectomy | 0.15 | 0.1 | 100 |
* Among typical couples who initiate use of a method (not necessarily for the first time), the percentage who experience an accidental pregnancy during the first year if they do not stop use for any reason other than pregnancy. Estimates of the probability of pregnancy during the first year of typical use for fertility awareness–based methods, withdrawal, the male condom, the pill, and Depo-Provera are taken from the 2006-2010 National Survey of Family Growth (NSFG) corrected for underreporting of abortion.
† Among couples who initiate use of a method (not necessarily for the first time) and who use it perfectly (both consistently and correctly), the percentage who experience an accidental pregnancy during the first year if they do not stop use for any other reason. See the text for the derivation of the estimate for each method.
‡ Among couples attempting to avoid pregnancy, the percentage who continue to use a method for 1 year.
§ This estimate represents the percentage who would become pregnant within 1 year among women now relying on reversible methods of contraception if they abandoned contraception altogether.
∥ 150 mg gel, 100 mg gel, 100 mg suppository, 100 mg film.
** With spermicidal cream or jelly.
†† About 80% of segments of Fertility Awareness Based Methods (FABM) use in the 2006-2010 National Survey of Family Growth (NSFG) were reported as calendar rhythm. Specific FABM methods are too uncommonly used in the U.S. to permit calculation of typical use failure rates for each using NSFG data; rates provided for individual methods are derived from clinical studies. The Ovulation and TwoDay methods are based on evaluation of cervical mucus. The Standard Days method avoids intercourse on cycle days 8 through 19. Natural Cycles is a fertility app that requires user input of basal body temperature (BBT) recordings and dates of menstruation and optional luteinizing hormone (LH) urinary test results. The Symptothermal method is a double-check method based on evaluation of cervical mucus to determine the first fertile day and evaluation of cervical mucus and temperature to determine the last fertile day.
This chapter presents contraceptive methods according to efficacy, with the methods that most effectively prevent pregnancy presented first followed by the less effective methods. This framework of contraceptive effectiveness follows the communication tool offered by the WHO ( Fig. 13.1 ) but is not a one-size-fits-all formula for counseling. For example, one study found lack of side effects and affordability were key to acceptability, in addition to efficacy ( ). Identifying preferences is key because a patient may feel misunderstood or reluctant to seek health care if her provider emphasizes effectiveness when she places greater value on another feature such as bleeding patterns.
Once selected, method initiation can usually begin immediately if desired. In the case of regular menstrual cycles, all methods can be initiated in days 1 through 5 of the menstrual cycle with expected immediate contraceptive protection. Outside of these cycle days , providers can also recommend initiation when reasonably sure, based on history and urine pregnancy testing, that a woman is not pregnant ( ). This is the quick start method . Quick start helps to avoid pregnancies that occur while waiting for menses to begin. After quick starting, the copper intrauterine device (IUD) is immediately effective. For other methods, providers should recommend a backup method such as abstinence or a barrier contraceptive for 1 week while awaiting contraceptive protection. When a health care provider is not reasonably certain about pregnancy, the benefits of initiating methods such as the birth control pill, implant, or injectable likely outweigh the risks. For intrauterine devices, the patient and provider should use SDM to explore the benefits of the device against the risks of an unlikely but possible pregnancy. After a quick start, initiators should be encouraged to repeat a pregnancy test if menses does not return or if pregnancy symptoms emerge. Occasionally pregnancy may occur after initiating a method using quick start. Contraceptive hormones are not teratogenic, and it is safe to continue pregnancies after a quick start or in other instances of contraceptive failure if desired.
Fallopian tube and vas deferens occlusion (sterilization) offer safe and highly effective contraception. In contrast to reversible or temporary methods, sterilization is permanent.
The decision to undergo sterilization should be made solely by the individual in consultation with a provider. The history of sterilization in the United States raises ethical concerns that must be considered, even today. Thousands of forced sterilization procedures occurred in the United States, disproportionately to poor women and women of color, whereas other women were denied sterilization because of provider beliefs ( ). Prospective studies document that up to 20% of women younger than age 30 report regret after sterilization ( ). If women wish to conceive after tubal sterilization, in vitro fertilization is likely necessary and is performed more often than tubal reconstructive surgery in these patients. Age should not be a barrier, however; younger women who are well informed and desire permanent sterilization can be offered the procedure. Providers offering sterilization should understand federal and local rules related to waiting periods, age, and disability status.
Vasectomy is a safe and highly effective outpatient procedure that takes about 20 minutes. More than 300,000 vasectomies are performed annually in the United States. After identifying and cutting the vas deferens, the ends of the vas are closed by ligation or fulguration and then replaced in the scrotal sac. This procedure prohibits sperm from passing into the ejaculate. After about 13 to 20 ejaculations, the ejaculate becomes sperm free but otherwise unchanged.
Vasectomy offers important advantages over tubal sterilization. The procedure is relatively low cost (it is the most cost-effective method) and can be performed in an office setting using local anesthesia. No entry into the peritoneal cavity occurs, and efficacy is easily verified when a semen sample confirms the absence of sperm. Until that time, another method of birth control must be used. In the United States, reversal requests range from 5% to 7% among men who have had a vasectomy. Vas reanastomosis, a difficult and meticulous procedure, offers a success rate of approximately 50% ( ).
Tubal sterilization prevents fertilization by cutting, occluding, or removing the fallopian tubes. Methods in the United States include laparoscopy anytime outside of pregnancy and postpartum sterilization concurrent with cesarean delivery or immediately after a vaginal delivery. About half of sterilization procedures occur in the postpartum period ( ).
Tubal sterilization is highly effective, with failure rates similar to LARC methods. The Collaborative Review of Sterilization (CREST), a prospective study of more than 10,000 women who underwent transabdominal sterilization that included 14 years of follow-up, provided information related to many aspects of tubal sterilization. Findings included a 5-year cumulative failure probability of 13 per 1000 procedures, with failures sometimes occurring years later. Younger women had a higher risk of failure. Postpartum partial salpingectomy carried the lowest 10-year cumulative risk of failure (7.5 per 1000 procedures); the rate with bipolar fulguration was higher ( ).
The CREST study occurred before the widespread adoption of Filshie clips, transcervical sterilization, and salpingectomy techniques. Some data show a 10-year cumulative failure rate of 2 to 3 per 1000 procedures for the Filshie clip ( ). Data are less clear for transcervical sterilization; Gariepy calculated a first-year failure rate of 57 in 1000 ( ). Clinicians lack sufficient information on expected failure rates for salpingectomy; however, the low failure rate of partial salpingectomy may serve as a proxy. If pregnancy occurs after tubal sterilization, location should be ascertained immediately because these pregnancies are often ectopic.
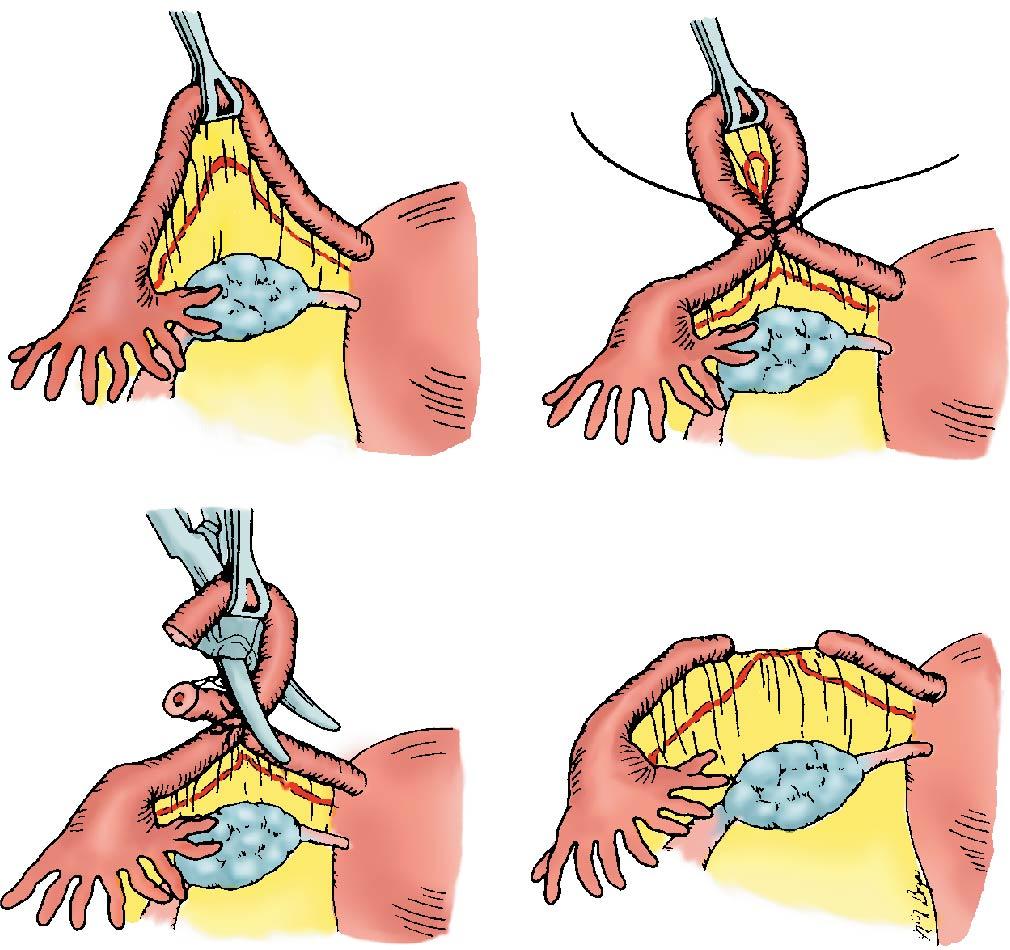
Tubal occlusion can occur during cesarean section, immediately postpartum through an infraumbilical minilaparotomy while the uterus is still enlarged and the tubes can be easily identified, or, as is commonly used outside the United States, during an interval minilaparotomy. Ligation and resection of a portion or the entirety of both fallopian tubes using a technique such as bilateral salpingectomy or the modified Pomeroy method is common ( Fig. 13.2 ). These methods typically involve general or regional anesthesia. Laparoscopic sterilization methods include salpingectomy, bipolar cautery, the Filshie clip, and the Silastic band (Falope ring).
No hysteroscopic sterilization methods are available in the United States. The Essure device, which involved hysteroscopic placement of microinserts in the fallopian tubes with eventual tubal tissue ingrowth and occlusion, was voluntarily withdrawn by the manufacturer in 2018 because of a decrease in sales after an increase in patient reports of adverse events ( ). Women with Essure devices in place can continue using it safely. For patients experiencing complications, management options include removal via laparoscopic salpingotomy, salpingectomy or cornuectomy, hysteroscopic removal, and hysterectomy if clinically indicated ( ).
Tubal sterilization with occlusion methods reduces the risk of ovarian cancer. Strong data suggest that many serous, endometrioid, and clear cell carcinomas begin in the fallopian tube rather than the ovary. Opportunistic salpingectomy, or the removal of both fallopian tubes in their entirety for the purposes of ovarian cancer risk reduction, appears to be a safe method of permanent sterilization with risks comparable to occlusion methods of tubal ligation. The risks and benefits of both techniques should be discussed with patients who desire permanent sterilization ( ).
The intrauterine device and implant (LARC methods) are highly effective and provide an option of years-long use without further clinician visits or medication refills. Unlike sterilization, LARC methods are immediately reversible with a rapid return to fertility . Very few medical contraindications to LARC exist. Although upfront costs can be high, these methods do not incur maintenance costs. LARC users typically report high continuation rates and user satisfaction. The American Congress of Obstetricians and Gynecologists (ACOG) recommends that it is safe to offer nulliparous women and adolescents LARC methods . ( ).
Practitioners should be mindful that women can face biased or even coercive contraceptive counseling practices and feel pressured to choose long-acting methods like LARC based on the priorities of the clinician rather than the patient ( ). This becomes particularly important for low-income women and women of color, who more often report lower quality family planning health care interactions than their higher-income and white counterparts. In some studies, providers were more likely to recommend IUDs to black and Hispanic women of low socioeconomic status ( ). Conflict and coercion can arise when a patient requests LARC removal and a clinician expresses reluctance or delays or even refuses to perform a removal. Patient requests for LARC removal should be honored, regardless of clinicians’ wishes.
The LARC methods available in the United States include the Paragard T380A copper intrauterine device, several levonorgestrel intrauterine systems (LNG-IUSs), and a single-rod etonogestrel subdermal implant (Nexplanon). No LARC methods contain estrogenic components. In the United States, LARC use increased among contraceptive users from 2% in 2002 to 8.5% in 2009 and 11.6% in 2012 ( ).
The IUD is the most commonly used reversible method of contraception worldwide and offers a safe and highly effective method with similar failure rates for typical and perfect use. First-year failure rates with the copper T380A IUD and the LNG-releasing IUD (LNG-IUD) are less than 1%, with the annual incidence of accidental pregnancy decreasing steadily thereafter. After 12 years, the cumulative pregnancy rate of the copper T380A IUD reaches 1.7%. At 5 years of use, the pregnancy rate for the LNG-IUD is about 1.1%. These pregnancy rates are comparable to those after surgical sterilization. Contraindications to IUD insertion include pregnancy, pelvic inflammatory disease, endometritis, uterine or cervical malignancy, and a müllerian anomaly or myomas that significantly distort the uterine cavity. For additional information on medical contraindications, please see the CDC Medical Eligibility Criteria (MEC) ( ).
The copper T380A IUD (Paragard) ( Fig. 13.3 , A ) is the only copper-bearing IUD currently marketed in the United States, although other copper IUDs are undergoing U.S. clinical trials. Because of the constant dissolution of copper (in amounts less than that ingested in the normal diet), copper IUDs require periodic replacement. The copper T380A is currently approved for use in the United States for 10 years and maintains its effectiveness for at least 12 years .
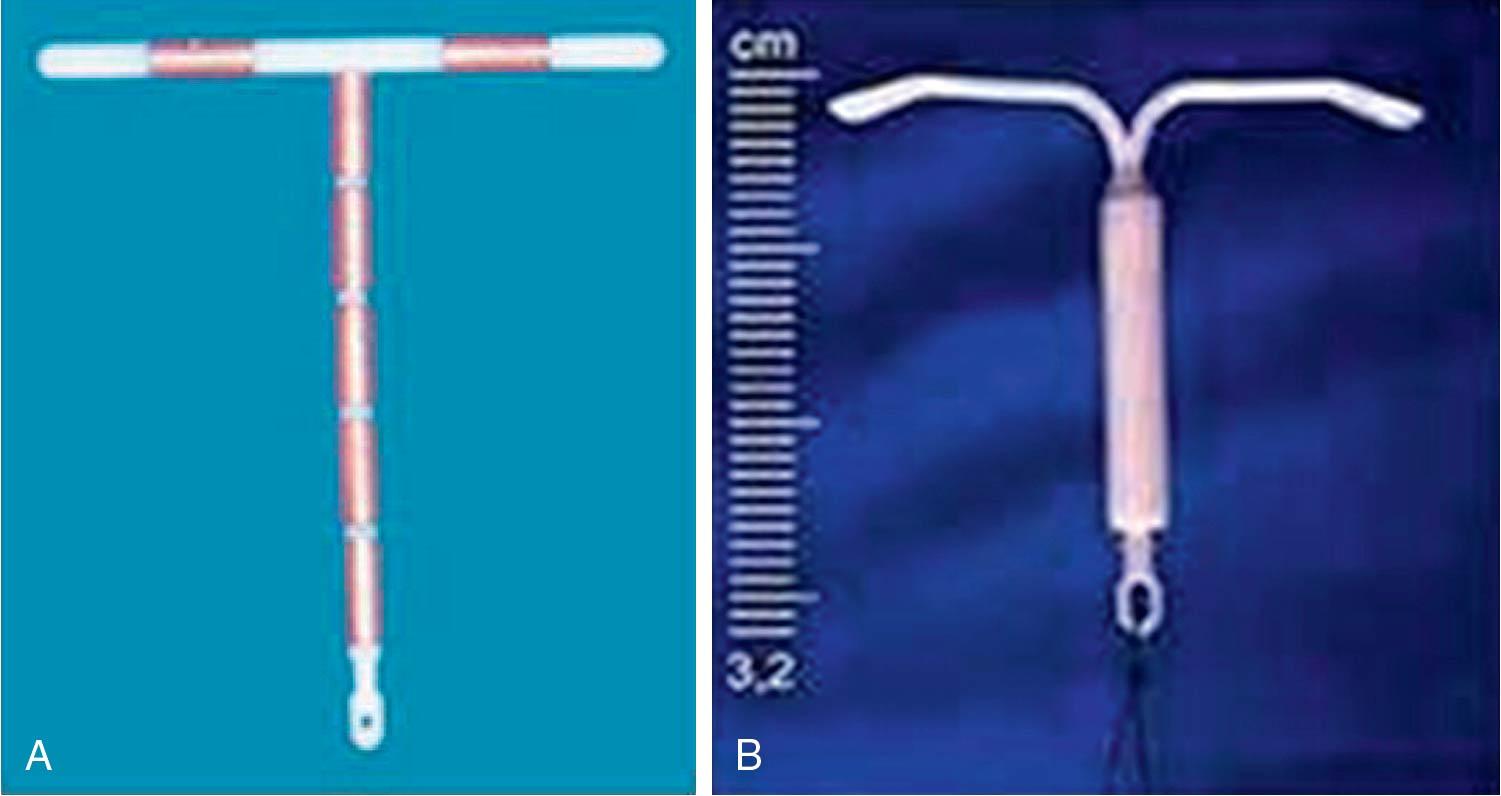
A progestin reservoir in the vertical arm of a T-shaped IUD also provides long-term effectiveness. Two LNG-IUD types, Mirena and Liletta (see Fig. 13.3 , B ), contain a total of 52 mg of levonorgestrel, which is released at a rate of about 20 μg of LNG daily into the endometrial cavity. These LNG-IUDs maintain a high level of effectiveness for 5 years; data suggest high effectiveness continues for 7 years ( ), and both are undergoing clinical trials for further extended use. Progestin-releasing IUDs reduce menstrual blood loss and treat heavy menstrual bleeding and related iron deficiency anemia .
In addition, a 13.5-μg LNG-releasing IUD device with a slightly smaller body than the Liletta and the Mirena is approved for up to 3 years of use (Skyla), and another device with 19.5 mg LNG was approved for 5 years of use (Kyleena). For the purposes of this chapter, we refer to the with 20-μg releasing LNG IUD devices when discussing the LNG-IUD.
All IUDs induce a local and sterile inflammatory response within the endometrium that incapacitates sperm thereby preventing fertilization of the ovum. This sterile inflammatory response was the only mechanism of inert historical IUDs. Modern IUDs contain either copper or progestin that augments local effects and improves efficacy. No IUD causes abortion; all contraceptive effects are preimplantation.
Copper markedly increases the extent of the inflammatory reaction with accumulation throughout the uterine lumen, the cervix, and probably the fallopian tubes. In addition, copper impedes sperm transport and viability in the cervical mucus . Because of these changes, very few, if any, sperm reach the oviducts, and the ovum usually does not become fertilized. The very small numbers of fertilizations that do occur underlie the failure rate of these devices. The primary effect of the progestin in the LNG-IUD is to thicken cervical mucus . Thickened mucous impedes sperm mobility and access to the upper genital tract. Additionally, the LNG-IUD decreases tubal motility and produces a thin, inactive endometrium . The low levels of circulating steroid sometimes inhibit ovulation. Systemic LNG levels are lower in IUD users than users of LNG-containing implants or oral pills.
Most insertions are straightforward and accomplished on the first attempt. Women who are nulliparous and/or experience dysmenorrhea report more pain during insertion than parous women and those without menstrual pain ( ). Cervical preparation with misoprostol does not increase the success of insertion and increases pain. Ibuprofen or naproxen administered before insertion does not reduce insertion pain but is helpful for cramping during the hours afterward. Multiple trials show that topical anesthesia does not affect insertion pain, although a paracervical block may decrease it, particularly in nulliparous women. Clinicians should receive training in correct insertion technique as detailed in the product labeling
Most women who discontinue use of the copper IUD do so for heavy or prolonged menses or intermenstrual bleeding related to increased local prostaglandin release in response to the IUD. On average, copper IUD users experience about 1 additional day of bleeding per cycle . Heavy bleeding decreases with time and rarely leads to anemia . In contrast, LNG-IUD users experience a reduction in menstrual bleeding as early as 3 months after insertion that persists for the duration of use . After 24 months, 50% of users report amenorrhea and 25% oligomenorrhea ; providers should discuss the possibility of eventual amenorrhea with patients before insertion because some may find this unacceptable.
Uterine perforation is a rare ( 1 in 1000 insertions ) but potentially serious complication. Perforation is usually fundal and occurs at the time of insertion . IUDs correctly inserted entirely within the endometrial cavity do not migrate through the uterine muscle into the peritoneal cavity. With experienced providers, the risk of perforation is less. Straightening the uterine axis with a tenaculum and measuring the cavity with a uterine sound before IUD insertion reduces perforation risk. Perforation risk is slightly higher in women currently breastfeeding.
The clinician should rule out perforation if the user cannot feel the IUD strings and did not observe that the device was expelled. To assess missing strings, the provider can use ultrasound to locate the device. If the device is not located with ultrasonography, a radiograph visualizing the abdomen and pelvis should be performed ; all IUDs will be visible on a plain radiograph. IUDs outside the uterus usually can be removed by means of laparoscopy. In a study of 61,448 women with at least a year of follow-up, no IUD perforations led to serious clinical complications beyond the need for laparoscopic retrieval ( ).
The widespread use of transvaginal ultrasound has led to the discovery that IUDs can sit in the uterine cavity below the fundus. In asymptomatic individuals, the device should be left in place if entirely within the uterine cavity . However, if the stem of the device is visible at the external cervical os or any part of the IUD is visualized below the internal os on ultrasound, the IUD should be removed.
A pregnancy with an IUD in place is rare. Among the few IUD users who do become pregnant, an ectopic location is more likely than among pregnant women without an IUD . Therefore in the case of a positive pregnancy test, a pelvic ultrasound must be performed to locate the pregnancy. If intrauterine, the device should be removed. Pregnancies that occur with an IUD in place have a higher incidence of spontaneous abortion or infection . After IUD removal, the complication rate becomes similar to that of a pregnancy without an IUD. In the case of an undesired pregnancy, a vacuum aspiration can be performed to remove both the pregnancy and the device.
The risk of infection after IUD insertion is small and decreases with time . The placement process, not the device itself or its threads, creates a transient risk of infection, as does any transcervical procedure. In a meta-analysis of randomized controlled trials (RCTs), routine use of prophylactic antibiotics preceding IUD insertion did not change the risk of pelvic infection ( ). An IUD may be placed without results from cervical screening for infection; however, if a provider has clinical suspicion of infectious endocervicitis, testing for gonorrhea and chlamydia should be performed and the IUD insertion delayed. Providers caring for women undergoing routine insertion or care with an IUD in place should follow standard sexually transmitted infection (STI) screening guidelines.
Positive gonorrhea or chlamydia screening tests that occur with an IUD in place can be successfully treated without removing the IUD. For patient with symptoms of pelvic inflammatory disease (PID) and an IUD, an antibiotic regimen for PID approved by the CDC should be used with close clinical follow-up. If the infection does not improve within 48 to 72 hours of treatment or if there is evidence of tubo-ovarian abscess, the device should be removed and an alternative method initiated ( ).
Routine cytologic testing can identify Actinomyces organisms during cervical screening with IUDs in place. If the woman is asymptomatic, no treatment is indicated. In the rare event of pelvic infection, treatment includes IUD removal and an appropriate course of antibiotics (usually penicillin).
Several long-term studies indicate IUD use is associated with a reduction in risk of developing cervical and endometrial cancer. Data are promising for the use of the LNG-IUS as a fertility-sparing treatment of early stage endometrial cancer. To date, few studies have evaluated whether hormonal IUD use changes the risk of breast cancer; however, it is an active research question.
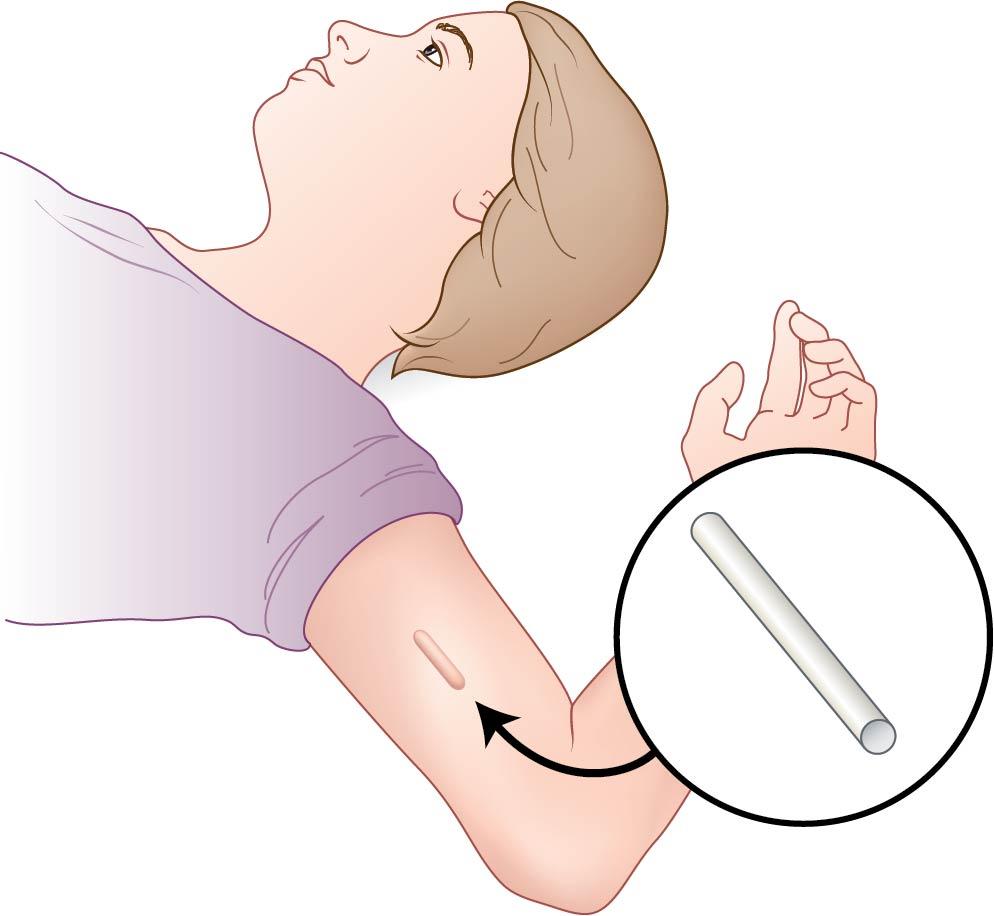
Subdermal implants, which consist of one or more thin flexible rods containing a progestin hormone rank, among the most effective methods of contraception, with an effectiveness equal or superior to that of sterilization and IUDs. In the United States one implant is available, Nexplanon, which contains 68 mg of etonogestrel (ENG) . Nexplanon is approved for 3 years of use ; however, preliminary studies indicate continued effectiveness for 5 years ( ). The implant inhibits ovulation and thickens cervical mucus. After removal, serum etonogestrel levels decline to undetectable within a week. Ninety percent of users ovulate within 1 month after removal.
In clinical trials, continuation rates are high at 50% to 80% until 2 years. Bleeding irregularities are the most common reason for discontinuation, accounting for about 60% of early removals . As with other progestin-only methods, nearly all women experience changes in their regular bleeding pattern. Women may experience amenorrhea or infrequent, frequent, or prolonged bleeding. Unlike depo-medroxyprogesterone acetate (DMPA) or the LNG-IUS, the bleeding patterns of individual women will be unpredictable.
U.S. providers must complete a Food and Drug Administration (FDA)–mandated training program before providing Nexplanon implants . After skin infiltration with local anesthesia, the implant is inserted superficially into the subdermal tissue of the nondominant upper arm posterior to the groove between the bicep and triceps. The insertion site is closed with adhesive without the need for suture ( Fig. 13.4 ), and the procedure usually takes less than a minute to complete. From the subdermal space, the steroid diffuses into the circulation at a constant rate. At the end of use, the implant must be removed. The removal site is infiltrated with local anesthetic and the implant removed through a 2- to 3-mm incision then closed with adhesive (see Fig. 13.4 ). Correct, superficial insertion enhances the ease of removal; improperly placed deep implants are more difficult to remove. If nonpalpable, an implant can be identified using imaging of the upper arm. Rare cases (1 per 100,000 insertions) of distant migration of the implant to the pulmonary artery have been reported ( ).
Systemically absorbed hormonal contraceptives primarily prevent pregnancy by suppressing gonadotropins. The progestin component suppresses the luteinizing hormone (LH) surge, which inhibits ovulation. Methods that contain estrogen prevent a rise in follicle-stimulating hormone (FSH), which inhibits follicular development through a synergistic effect with the progestin. Estrogen also stabilizes the endometrium, which prevents unscheduled bleeding. In addition, secondary contraceptive effects of progestins include thickening cervical mucus, which makes it less permeable to sperm; thinning the endometrium, which makes it less suitable for implantation; and impairing tubal motility, which interferes with gamete transport.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here