Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
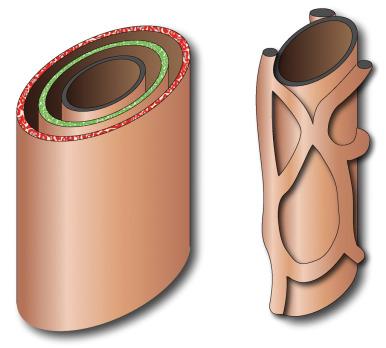
Hepatorenal fibrocystic disorders are a group of associated congenital anomalies of the liver and kidney caused by malformation of the embryonic ductal plates formed by bipotential progenitor hepatoblasts surrounding portal venous ramifications ( Fig. 87.1 ). They include choledochal cysts, Caroli disease, hepatic fibrosis, biliary hamartomas, and cystic liver disease. The specific type of fibrocystic disorder depends on the size of the embryonic duct with faulty development ( Table 87.1 ) and may be associated with renal cystic disease.
| Disorder | Duct Size | Renal Association |
|---|---|---|
| Congenital hepatic fibrosis | Small | ARPKD |
| Biliary hamartoma | Small | |
| Polycystic liver disease | Medium | ADPKD |
| Caroli disease | Large Intrahepatic | ARPKD |
| Choledochal cyst | Large extrahepatic |
Choledochal cysts, which are among the most frequent of congenital hepatobiliary anomalies, are a fusiform or saccular dilation of the bile ducts. The Todani classification system is commonly used to categorize these anomalies into five general types (with several subtypes) that differ based on etiology, pathogenesis, appearance, and presentation ( Fig. 87.2 ).
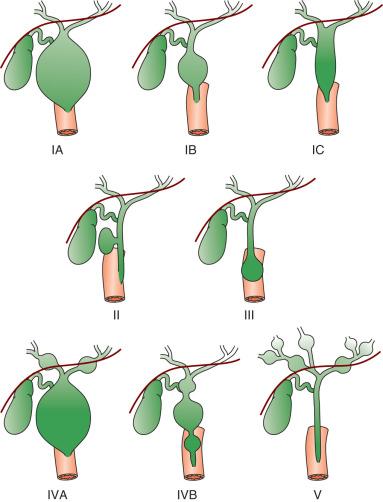
The most common choledochal cyst is the Todani type I, found in 80% to 90% of cases. It involves variable lengths and degrees of common bile duct dilatation and is further classified into subtypes IA, IB, and IC. Todani types IA, B, and C describe cystic dilation of the entire extrahepatic bile duct, segmental dilation below the cystic duct, and fusiform/cylindrical dilation of entire extrahepatic bile duct, respectively. Type I choledochal cysts are more common in girls than boys in Western countries, but the sex ratio is equal in Asia. About 65% of all reported cases are from Japan. Todani type II choledochal cysts are rare, found in only 2% of cases, and consist of one or more diverticula of the common bile duct. Todani type III occurs in 1.5% to 5% of cases and involves dilation of the intraduodenal portion of the duct forming a cystlike mass termed a choledochocele with both the common bile and pancreatic ducts emptying into it. Todani type IVA consists of multiple intrahepatic and extrahepatic biliary dilatations and occurs in 10% of patients with choledochal cysts. Type IVB involves multiple extrahepatic biliary cysts, without intrahepatic involvement, and it is extremely rare. Todani type V is synonymous with Caroli disease. It may be difficult to differentiate between a type I cyst with intrahepatic dilatation from stagnation and the true type IV A cyst. This differentiation, however, is not necessary for treatment. Intrahepatic dilation will improve postoperatively in type I cysts.
Several theories for the pathogenesis of type I choledochal cysts exist. In addition to the ductal plate malformation described previously, other theories suggest cyst formation due to obstruction of the distal biliary duct and/or reflux of pancreatic enzymes into the biliary tree, due to anomalous pancreaticobiliary junction (PBJ).
When the junction of a common bile duct and pancreatic duct form a common channel outside the sphincter of Oddi, it is considered anomalous. The anomalous junction outside the sphincter mechanism is thought to allow reflux of pancreatic secretions into the biliary tree and vice versa, and likely plays a role in pathogenesis of choledochal cysts and predisposes to pancreatitis as well as the formation of stones, polyps, and cancer.
Type II choledochal cysts, have been theorized to result from prenatal rupture of the common bile duct with subsequent healing. Type III choledochal cysts may be the sequelae of ampullary obstruction or congenital duplication of the duodenum at the ampulla. The intrahepatic cysts seen in types IV and V are thought to be due to primary ductal ectasia resulting from ductal plate malformation.
Choledochal cysts may present in infancy with cholestatic jaundice, clinically inseparable from neonatal hepatitis or biliary atresia. In older children and young adults, the clinical presentation is variable. The characteristic triad of abdominal pain, obstructive jaundice, and fever is seen in a minority of patients present. Abdominal pain is the most characteristic presentation, followed by obstructive jaundice, fever, pale stools, splenomegaly, hepatomegaly, and a palpable mass. Pancreatitis can be a presentation in older children, particularly in type IV A. The most common complication of a choledochal cyst is ascending cholangitis. Long-term complications, such as hepatic cirrhosis with subsequent portal hypertension, can occur. Carcinoma of the biliary tree has a 20-fold increased incidence in patients with choledochal cysts. This risk is low in the first decade but increases with advancing age. Spontaneous cyst rupture has also been reported.
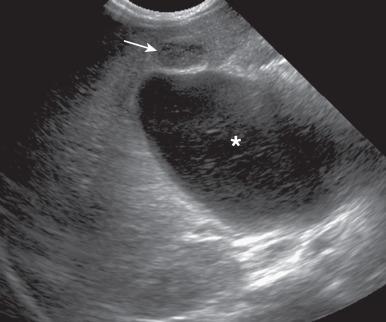
Sonography is usually the initial imaging study. The markedly dilated common bile duct in types I and IV choledochal cyst is readily discernible. The gallbladder can usually be identified adjacent to the dilated common duct ( Fig. 87.3 ). Sludge or stones may be identified within the dilated ducts. Type III cysts may cause mass effect at the Ampulla of Vater ( e-Fig. 87.4 ).

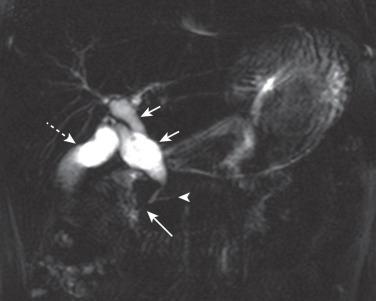
Abdominal magnetic resonance imaging (MRI) with cholangiopancreatography (MRCP) is the modality of choice to delineate the type of cyst, the length of the involved duct, the presence and location of protein plugs or calculi, the PBJ, and the length of the common channel ( Figs. 87.5 and 87.6 ). A common pancreaticobiliary channel of more than 15 mm in length is considered abnormal in adults. However, there is limited data on normal length of common channel in children, with one recent study using 5 mm as a cut-off value while another found an average length of 9.25 mm.
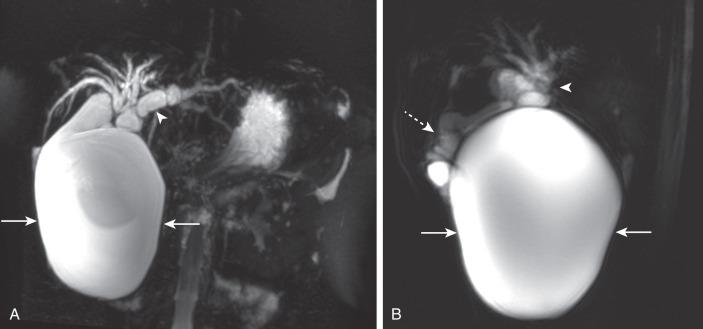
MRI is also useful for evaluation of any associated abnormalities such as masses, portal hypertension, and renal abnormalities. Contrast-enhanced MRCP with hepatocyte specific contrast media such as gadobenate and gadoxetate can be used to demonstrate communication between choledochal cyst and the biliary tree and to evaluate postoperative bile leak, as can hepatobiliary scintigraphy. Computed tomography (CT) may have a limited role in evaluation of choledochal cyst when MRCP is not available.
With improved diagnostic imaging, the role of percutaneous transhepatic cholangiography (PTC) and endoscopic retrograde cholangiopancreatography (ERCP) is usually reserved for therapeutic intervention.
Due to the potential long-term sequelae, surgical excision and hepatojejunostomy are performed as definitive treatments. Patients with intrahepatic cysts are closely monitored for cholangitis, cholestasis, and stone formation. Antibiotics are administered in the setting of acute cholangitis. Medical therapy can be instituted to reduce the risk of cholestasis and promote bile flow.
Caroli disease, also classified as Todani type V choledochal cyst, is a segmental nonobstructive dilation of the intrahepatic bile ducts. It is characterized by multifocal saccular dilation of intrahepatic ducts. It can be associated with stone formation, cholangitis, hepatic abscesses, and cholangiocarcinoma later in life.
Leading theories on the etiology of Caroli disease include maldevelopment of the large intrahepatic ductal plates. Other postulated mechanisms include: occlusion of the hepatic artery in the neonatal period with associated ischemia of the bile ducts versus abnormal growth rate of the biliary epithelium and supporting connective tissues with lack of the normal involution of ductal plates. This process leads to ectatic biliary ducts surrounding the portal triads. In Caroli syndrome , which involves large and small ductal plate abnormalities, there is associated hepatic fibrosis. Caroli hepatic ductal ectasia may also be associated with extrahepatic ductal plate abnormalities and choledochal cysts (Todani IVA choledochal cyst) as discussed previously. An association also exists with renal disorders including autosomal recessive polycystic kidney disease (ARPKD), medullary sponge kidney, and nephronopthisis. Although typically a diffuse process, monolobar Caroli disease has been reported, with 88% involving the left lobe.
Although the disease is present from birth, most patients do not present until later in life when abdominal pain secondary to cholangitis and cholestasis leads them to seek medical attention. The abdominal pain may also be related to hepatic abscesses (secondary to cholangitis) or to biliary stones (secondary to cholestasis). Patients with associated hepatic fibrosis may present with symptoms and signs of portal hypertension.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here