Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The term arthrogryposis encompasses all congenital joint contractures. This includes arthrogryposis multiplex congenita in which multiple joints are contracted, amyoplasia which includes a characteristic pattern of upper extremity contractures, and distal arthrogryposis which is a set of 10 genetic disorders with associated hand and feet contractures. Treatment depends on the joint(s) involved and the associated functional limitations. Ensuring adequate shoulder internal rotation and elbow flexion for feeding and elbow extension for perineal care is key for improving patient independence.
Camptodactyly is a congenital flexion contracture of the proximal interphalangeal (PIP) joint, most commonly affecting the small finger but occurring in any digit. It can present in infancy (type I), in adolescence (type II), or in association with a syndrome (type III). Mild cases have minimal functional impairment, but more severe contractures may require intervention. Splinting and stretching are usually attempted first. Refractory cases may benefit from release of tight skin, flexor digitorum superficialis (FDS) tendon, an analomous lumbrical/interosseous insertion, and/or the proximal interphalangeal (PIP) joint.
Thumb-in-palm or clasped thumb deformity, occurring in isolation or in association with distal arthrogryposis or cerebral palsy, is characterized by a flexion and adduction contracture of the thumb. Those children with persistent contracture causing functional impairment after a trial of splinting warrant surgical intervention. A variety of techniques for release with skin grafting or local flap coverage have been described. Release of a tight adductor pollicis or first dorsal interosseous muscle or the carpometacarpal joint may also be required.
Arthrogryposis is a general term used to describe congenital joint contractures, which can be genetic, environmental, neurologic, or idiopathic in nature. When a patient has joint contractures present in two or more body areas, they may be classified as having arthrogryposis multiplex congenita (AMC), regardless of the underlying etiology. AMC has an overall prevalence of one in 3000 live births and has been associated with over 300 different disorders. Subcategories of AMC include a myoplasia , an idiopathic disorder accounting for about one-third of AMC cases that involves a characteristic pattern of multiple symmetric upper extremity contractures often associated with craniofacial and gastrointestinal anomalies, and distal arthrogryposis , a set of 10 genetic disorders with the hand and feet contractures which are typically associated with a syndromic presentation or other congenital anomalies.
When affecting a single area of the body, congenital joint contractures are considered “isolated”. This includes isolated digital contractures such as camptodactyly and thumb-in-palm deformity discussed later in this chapter.
In the 2020 update of the Oberg, Manske, Tonkin (OMT) congenital hand upper extremity classification system, congenital contractures, including AMC and its subcategories, were reclassified as dysplasias rather than malformations due to an initially normal limb development which is subsequently altered. In recent years, an increasing number of abnormal or dysplastic cell functions and genetic mutations have been identified in AMC, particularly in association with genetic and syndromic types.
Due to the numerous conditions associated with AMC, there are a variety of proposed underlying pathophysiologic processes resulting in the congenital joint contractures. In patients with neuromuscular pathology, joint contractures are posited to result from decreased in utero movement due to abnormalities in the central or peripheral nervous systems, motor endplates, and/or muscle. Generalized connective tissue disorders and fetal crowding due to oligohydramnios, a bicornate uterus, or twin/multiple pregnancies have been implicated in other cases.
While the exact etiology of amyoplasia, the most common type of AMC, is unknown, generalized neuromuscular underdevelopment related to anterior horn cell hypoxia from impaired fetal circulation has been suggested due to the associated findings of decreased muscle mass, facial angiomas, and intestinal atresias, or abdominal wall defects. It occurs sporadically with no yet-identified genetic mutation or heritability.
Distal arthrogryposes (DAs), however, demonstrate autosomal dominant inheritance with variable penetrance. Mutations in multiple genes related to troponin, myosin, and fast-twitch myofiber contraction ( TNNI1 , TNNT3 , TPM2 , MYH2 , MYH3 , MYH8 , and MYH13 ) have been identified in familial cases of DA. The exact mechanism by which these mutations impact myofiber contractility remains unclear.
AMC may be identified on prenatal ultrasound or present postnatally with notable congenital contractures of joints in the upper and/or lower extremities. Most children with arthrogryposis are otherwise healthy. In cases of amyoplasia, DA, or other syndromic presentations of AMC, however, children may have craniofacial, respiratory, gastrointestinal, or other neurologic conditions. Family history may be positive in cases of DA or other heritable neuromuscular disorders.
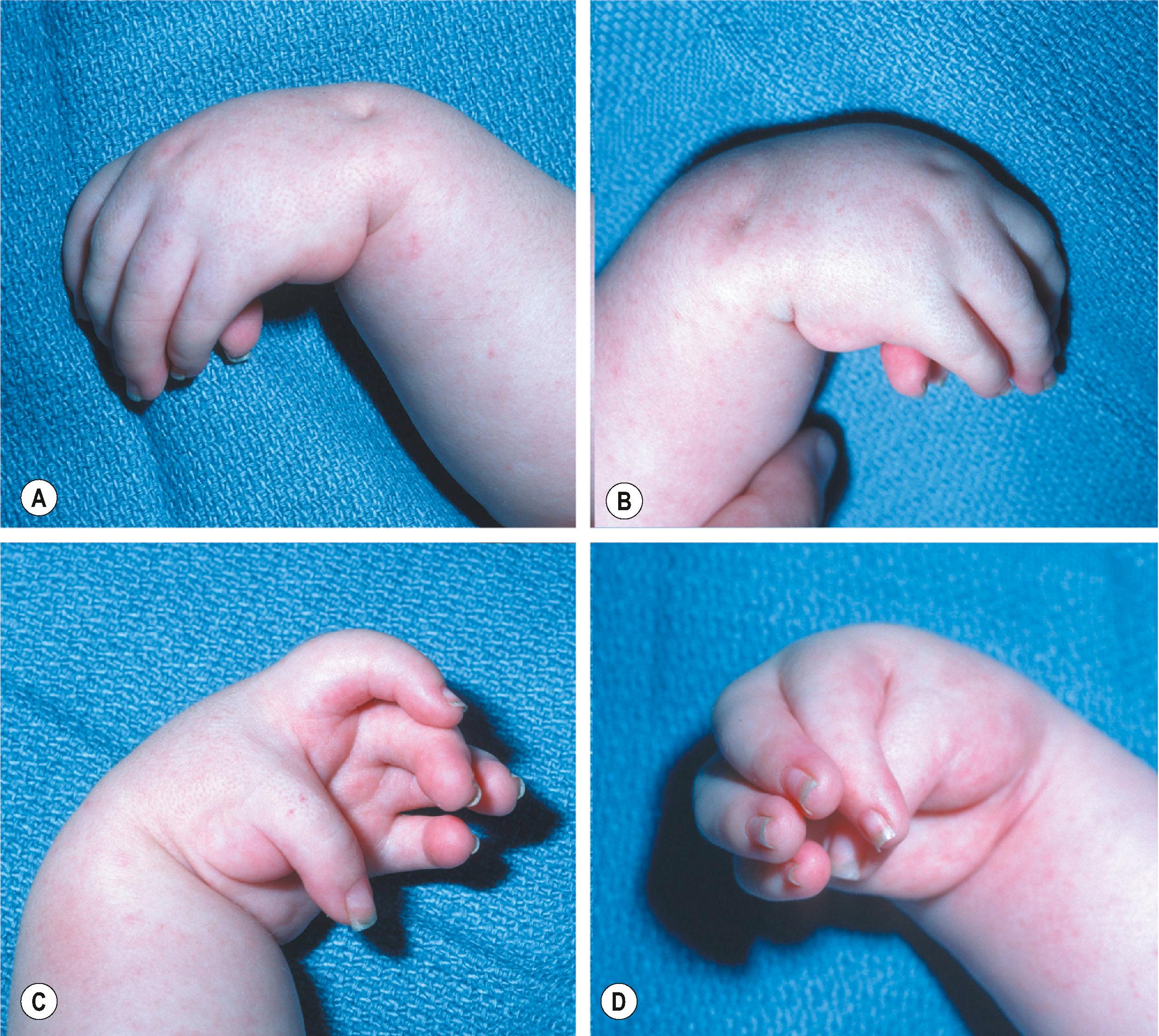
Children with amyoplasia classically present with internally rotated and adducted shoulders, extended elbows, flexed and ulnarly deviated wrists, stiff fingers, and thumbs positioned in the palm ( Fig. 38.1 ). Lower extremity contractures are typically also present. Midline facial hemangiomas, gastroschisis, and bowel atresia have also been reported. With distal arthrogryposis, hands and feet are involved with limited involvement of more proximal joints. Eleven different types of distal arthrogryposis have been described. In the upper extremity, major diagnostic criteria include the presence of camptodactyly or pseudocamptodactyly, absent fingers, hypoplastic and/or absent flexion creases, and ulnar deviation at the wrist.
Patients in whom upper extremity contractures limit function and interfere with activities of daily living despite nonoperative measures with orthoses and therapy may be candidates for surgery to address their arthrogryposis. Careful assessment of which joints are involved and the baseline range of motion is necessary. This may be difficult in younger children, but observing the performance of tasks such as feeding or playing with toys may be helpful. It is important to ensure that the planned surgery will not take away important functional skills. For example, an external rotation humeral osteotomy should be avoided in a patient in whom the internal rotation contracture is needed for perineal hygiene. Similarly, elbow flexion contracture release may be ill-advised in patients with limited active flexion who rely on the flexion contracture to bring their hand to their mouth. When bilateral upper extremity contractures are present, the surgical needs for each limb may be different to preserve different functions with each limb.
Initial management of upper extremity contractures begins shortly after birth with gentle stretching and range-of-motion exercises. Splinting or serial casting can also be utilized to improve joint positioning. For patients in whom adequate correction is not achieved with nonoperative measures, several surgical techniques exist depending on the location and severity of the contractures present.
In patients with shoulder internal rotation and adduction contractures, such as those with amyoplasia, a humeral external rotation osteotomy may be used to correct a lateral-facing palm position to a forward- or medial-facing position, allowing for a palm-to-palm grasp. This can improve function in hand-to-mouth functions and bimanual tasks. Both a proximal and distal humeral osteotomy have been described, each stabilized with a rigid plate and screw construct. Care must be taken to maintain adequate internal rotation for midline function and perineal care. Elbow flexion contractures may need to be corrected first as the associated forearm pronation contracture may be difficult to distinguish from true internal rotation. Elbow release and humeral osteotomy can be performed in combination or in a staged fashion.
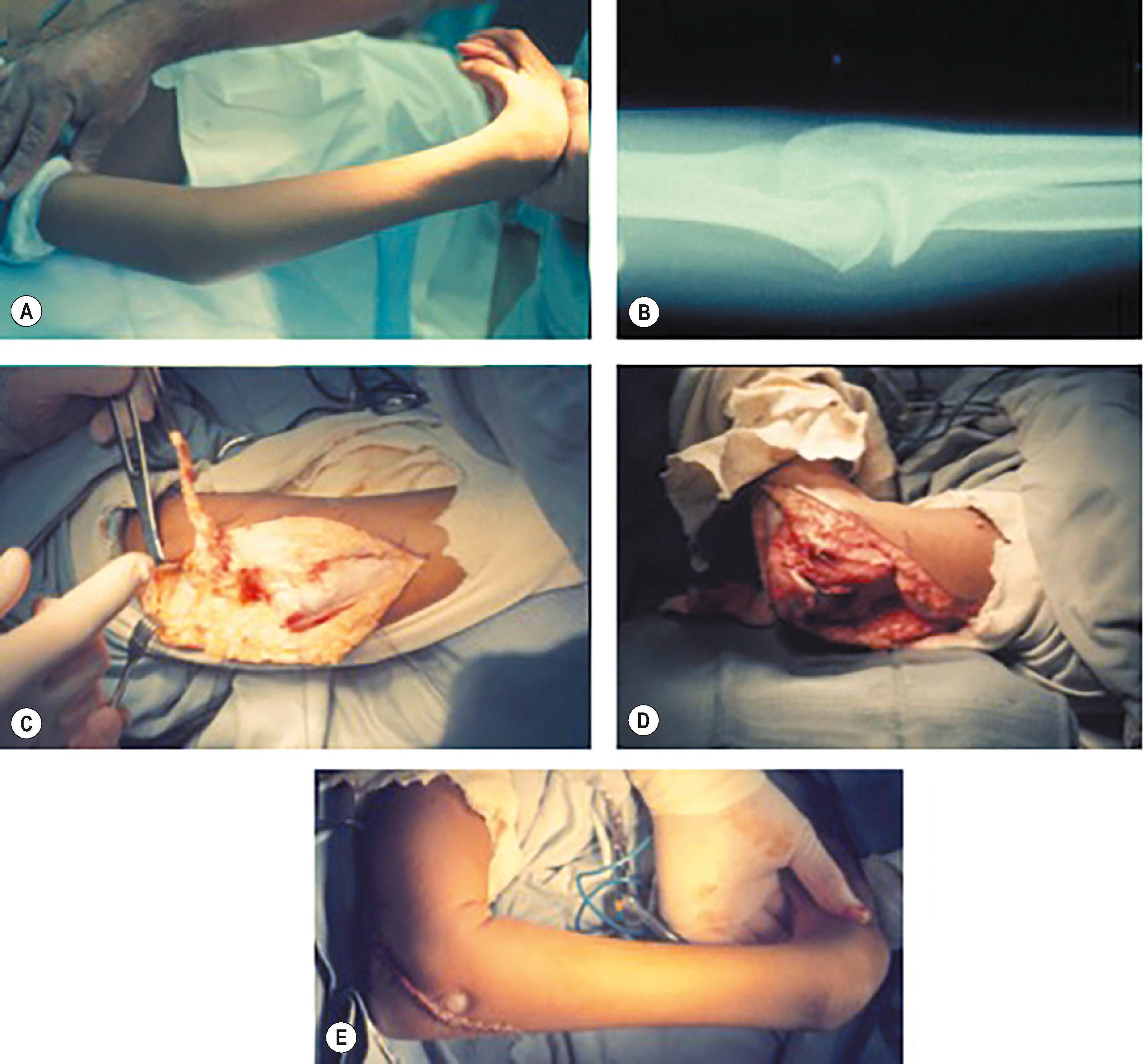
While some patients with arthrogryposis may have elbow flexion contractures with or without associated pterygium, most have a functioning triceps which overpowers weaker elbow flexors, resulting in an extension contracture. Patients with less than 30° of flexion or inadequate flexion for feeding by 1–2 years of age, despite splinting and stretching efforts, may benefit from elbow contracture release. Most authors advocate for subcutaneous transposition of the ulnar nerve prior to elbow release in order to protect the nerve. This is followed by triceps tendon release and lengthening with a “W” or “V-to-Y” flap followed by posterior elbow capsule release until at least 90° (preferably 120°) of elbow flexion can be achieved. Care must be taken to prevent destabilization of the medial and lateral collateral ligaments. Fig. 38.2 demonstrates correction of an elbow extension contracture with triceps release and posterior elbow capsulotomy with transfer of the long head of triceps to the proximal ulna through a bone tunnel to augment active flexion.
Patients may have both extension contractures and a lack of active flexion.
Contracture release should be performed first with subcutaneous transposition of the ulnar nerve for protection, triceps lengthening, and posterior elbow capsulotomy.
If augmentation of active flexion is needed, the long head of triceps can be transferred to the proximal ulna at the time of extension contracture release.
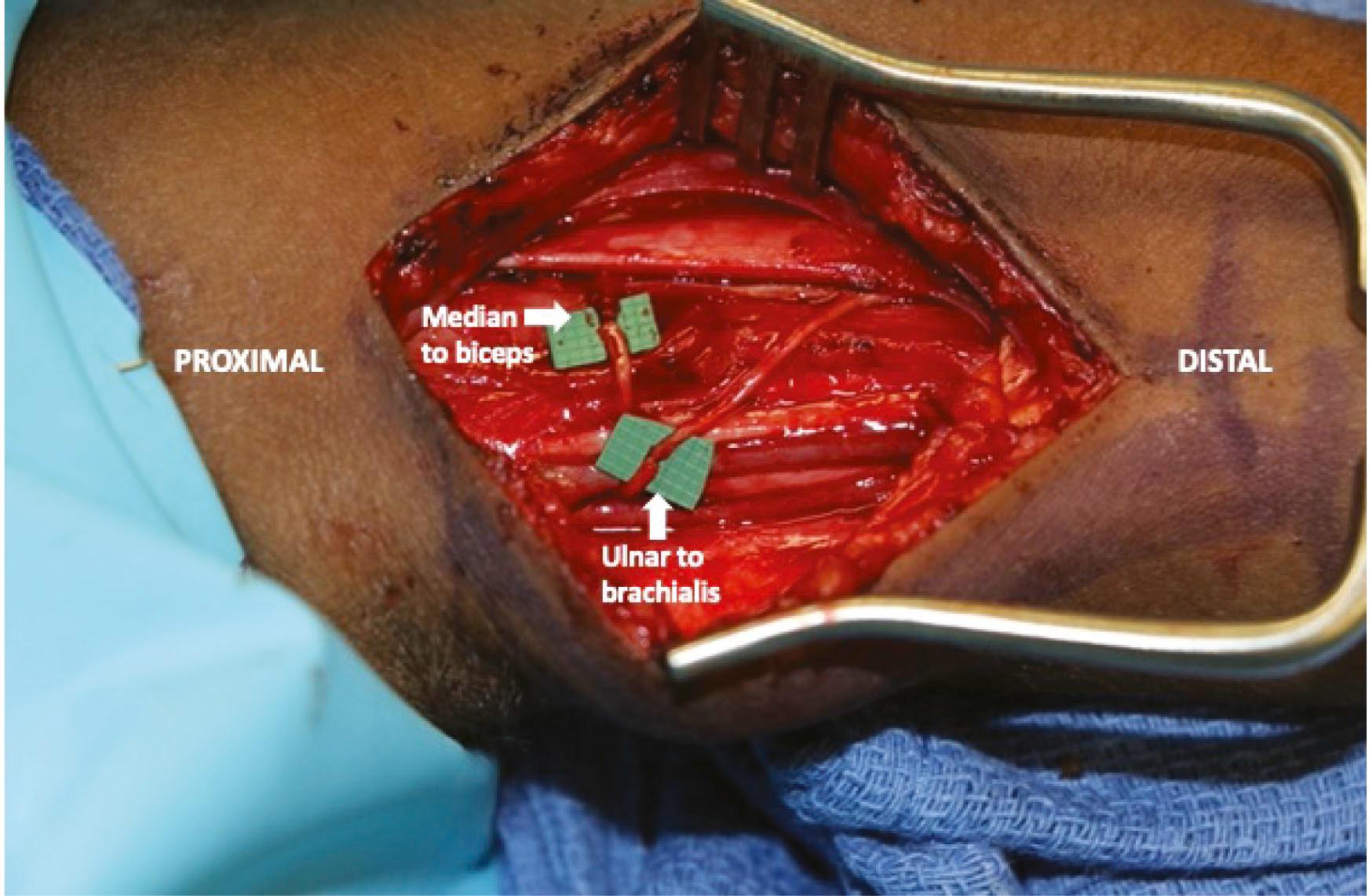
Even after release of elbow extension contractures, patients with arthrogryposis affecting the elbow typically have very minimal, if any, active elbow flexion. Multiple techniques have been described for improving elbow flexion, including Steindler flexorplasty and transfers of the long head of triceps, pectoralis major, bipolar latissimus, and gracilis free muscle. More recently, nerve transfers have been demonstrated as an option for augmenting active elbow flexion in certain patients with AMC. This includes the double Oberlin transfer in which an ulnar nerve fascicle is transferred to the brachialis motor branch and a median nerve fascicle is transferred to the biceps motor branch (or vice versa) ( Fig. 38.3 ).
For tendon transfers, technique selection is based on surgeon preference and on which donor muscle is expendable. Magnetic resonance imaging (MRI) may be useful to assess donor muscle development as physical exam can be difficult in younger children. Care should also be taken to ensure that a patient has good passive motion and the ability to be compliant with the rigorous postoperative therapy needs, as these muscle transfers have the potential to worsen flexion contractures which can result in deterioration in function. In both cases, early splinting or serial casting has been shown to improve wrist position and range of motion.
Children with arthrogryposis can experience wrist flexion or extension contractures, classically flexion with amyoplasia and extension with DA. For patients in whom nonoperative measures fail to achieve acceptable wrist positioning or contractures recur, surgical intervention may be necessary. Most of these procedures improve wrist extension in exchange for some loss of wrist flexion. With flexion contractures in patients with adequate extension to reach neutral, tenotomies or lengthening of the flexor carpi radialis (FCR) and flexor carpi ulnaris (FCU) with release of the volar fascia may be adequate to improve extension. Transfer of extensor carpi ulnaris (ECU) to extensor carpi radialis brevis (ECRB) can be added to correct any associated ulnar deviation. More severe flexion contractures typically require a dorsal carpal wedge osteotomy, which has been described with or without ECU tendon transfer. A biplanar osteotomy can also be designed to correct both flexion contracture and ulnar deviation simultaneously. Proximal row carpectomy and wrist arthrodesis have also be described for refractory or recurrent cases.
Extension wrist contractures tend to be better tolerated. Procedures to correct associated shoulder rotation or elbow contractures can provide adequate range of motion for necessary functions, such as eating and perineal care.
Surgical options to improve finger and thumb position and function will be discussed in detail later in this chapter in the sections on camptodactyly and thumb-in-palm deformity.
Although postoperative care varies depending on the nature and location of the surgery, most procedures are followed by orthotic use and physical and/or occupational therapy. Osteotomies typically require splinting or casting for 4–6 weeks with serial radiographs to monitor bony healing. Therapy is beneficial for motor retraining following tendon or muscle transfers, as well as with optimizing passive and active range of motion after any procedure.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here