Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Total temporomandibular joint replacement (TMJR) is indicated for the treatment of inflammatory arthritis not responsive to other modalities of treatment, recurrent fibrous and/or bony ankylosis, failed tissue grafts, failed alloplastic temporomandibular joint (TMJ) reconstruction, or loss of vertical mandibular height and/or occlusal relationship (secondary to bone resorption, trauma, developmental abnormality, or pathologic lesion). Early joint replacements using autologous tissue had a high rate of complication, particularly ankylosis (32.7%) and overgrowth (16.4%). Alloplastic TMJR more readily conforms to the given anatomy, is less susceptible to systemic disease, does not require a donor site, and allows for early physical therapy. Initial prostheses were derived of proplast-teflon, silicone, or metal, all of which led to high rates of failure. Metal-on-metal stock prostheses were subsequently developed but faced similar challenges. These stock implants had difficulty with large orthognathic movements, issues with posterior TMJ dislocation, and problems treating patients with anomalous anatomy. Large orthognathic movements place significant angulation on the TMJ prosthesis, and previous implants were not designed to handle such strain. Additionally, stock joints may not fit the glenoid fossa or mandibular ramus and body in patients with anatomic variation.
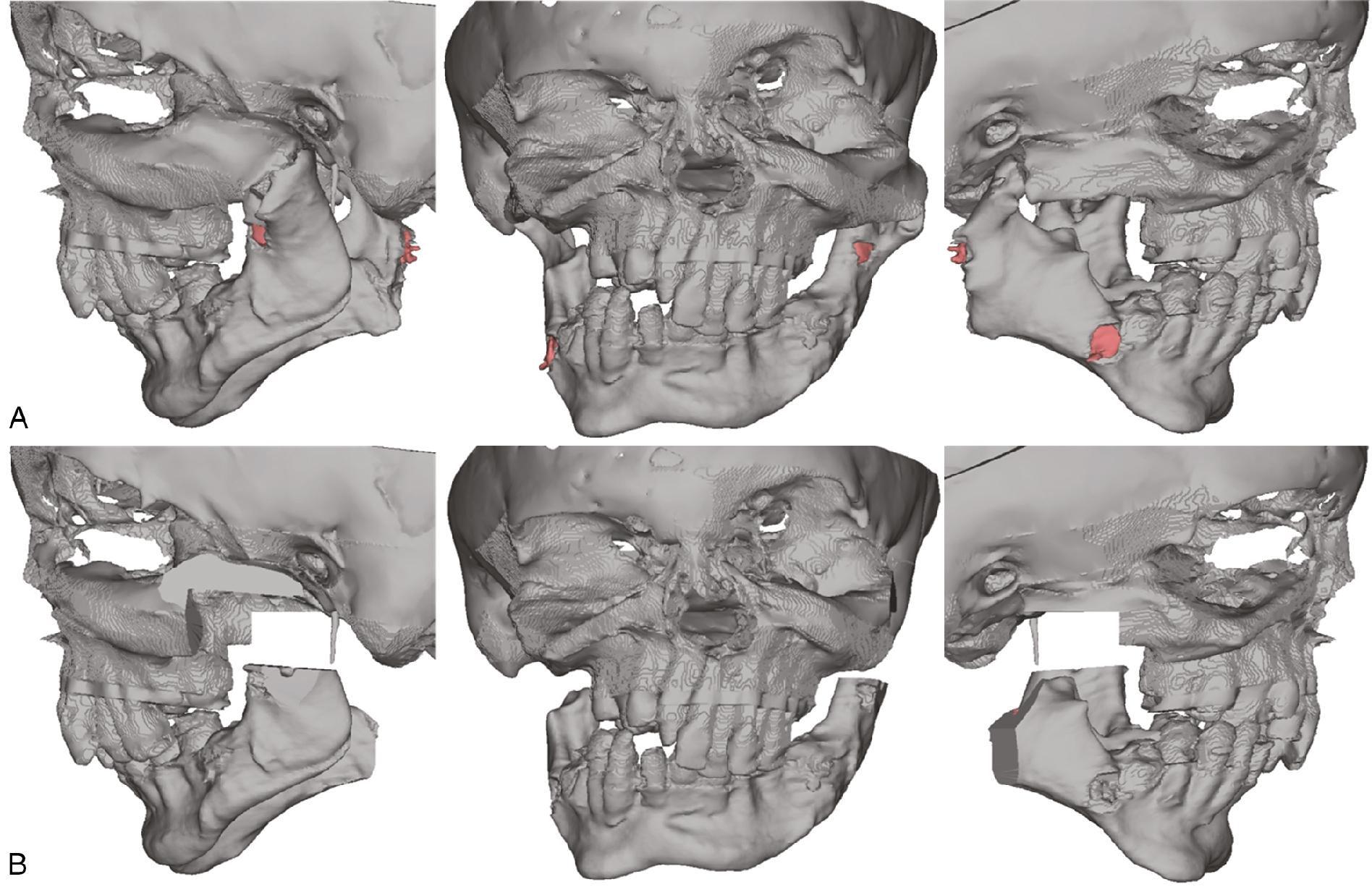
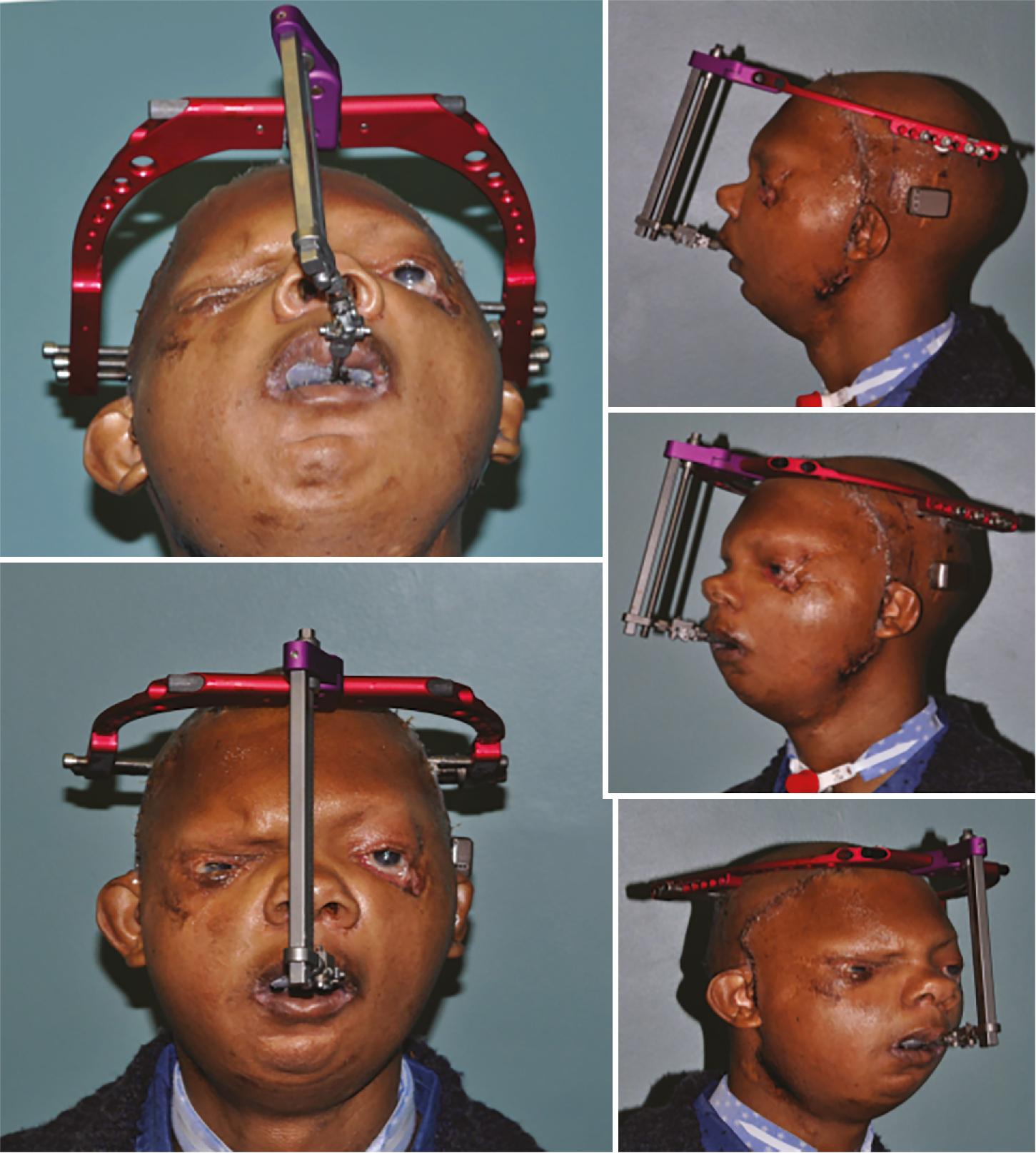
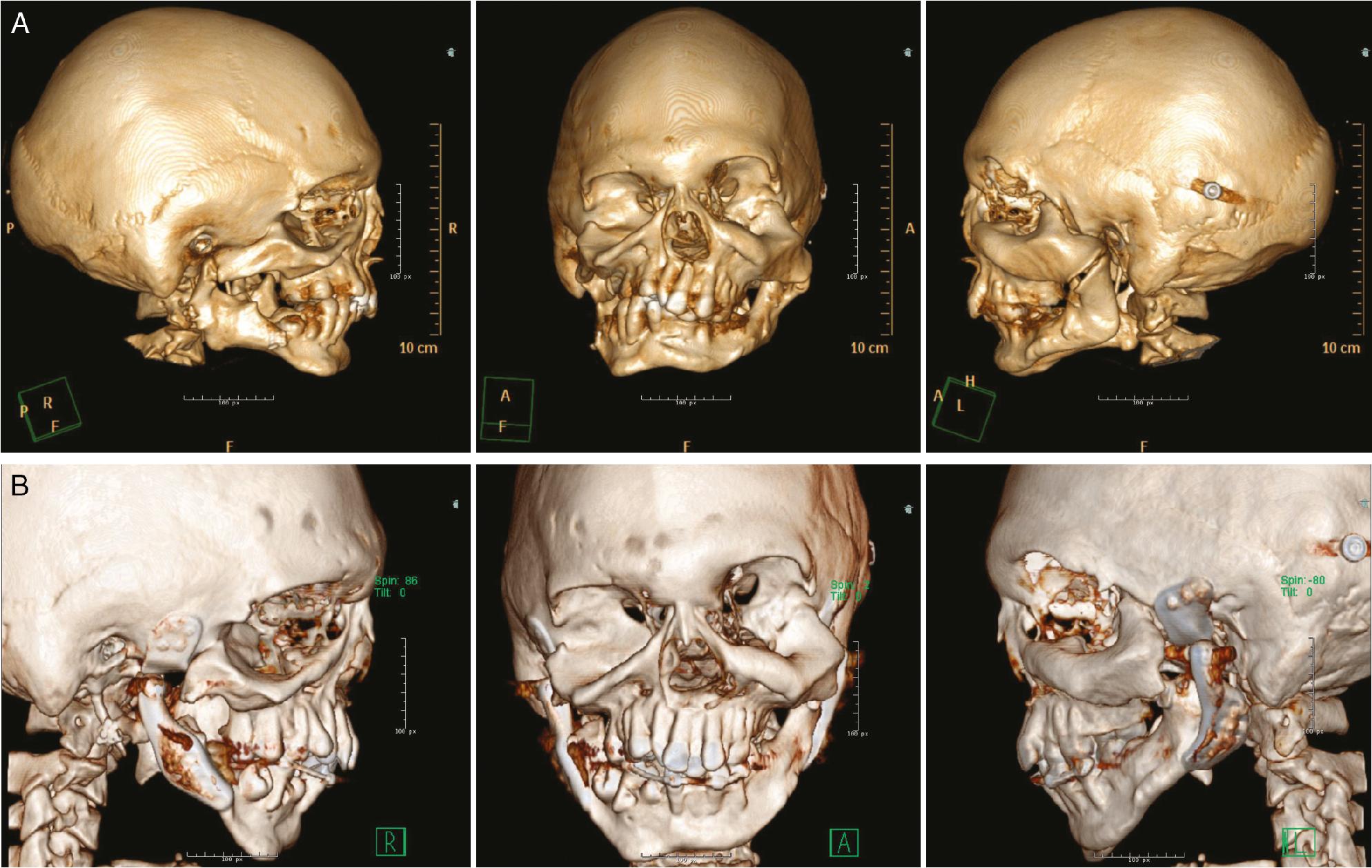
Computer-assisted design/computer-assisted manufacture (CAD/CAM) technology has addressed many of the challenges faced by these traditional implants and is quickly gaining popularity as the custom TMJR components interface well with the host anatomy. , In 2015, Wolford proposed his protocol for concomitant TMJR and orthognathic surgery using CAD/CAM surgical simulation, which is widely used by surgeons. CAD/CAM allows for the development of custom TMJR prostheses made of titanium alloy and polyethylene. This metal-on-polyethylene design is better suited to handle the angulation that large orthognathic movement places on the implant, and results in less torque on the contralateral TMJ during jaw movement and implant placement. Greater customization also allows for the design of a larger posterior stop on the temporal component of the implant, minimizing the risk of posterior TMJR dislocation. Computer-assisted planning and CAD/CAM design allows the surgeon to view the proposed prosthesis on the models from multiple vantage points to ensure the validity of the design.
Anatomic models are produced from a computed tomography (CT) scan or from the images of the computer-assisted planned surgical movements and osteotomies. The custom TMJ prosthesis is then made using a CAD/CAM wax model. The components of the prosthesis are designed to be patient-fitted, which improves long-term stability and safety. This also allows the prosthesis to fit anomalous glenoid fossa and mandibles. Osteotomy sites and osseous resection for condylar as well as temporal fossa components of the prosthesis can also be planned virtually using CAD/CAM technology. This improved accuracy in osteotomies subsequently allows for greater accuracy in predicted concurrent orthognathic movements.



Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here