Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The differential diagnostic lists that follow in this chapter serve as a starting point for evaluation of an unknown skin biopsy. Such lists have some advantages over algorithms because they provide multiple pathways for getting back on track toward the correct diagnosis. By contrast, some algorithms provide fatal forks in the road that, if selected incorrectly, might lead the pathologist toward a misdiagnosis based upon too much emphasis upon one criterion. Instead, it is best to consider multiple criteria in concert.
The most important clinical questions are location of lesions (arms, head, legs, etc.), symptoms (pruritus, pain, etc.), duration (acute or chronic), arrangement of lesions (solitary, generalized, annular, linear, etc.), morphology (macules, papules, plaques, vesicles, etc.), and color (red, blue, brown, black, white, yellow, etc.). The smart pathologist will not read out a skin biopsy of an inflammatory condition without calling for clinical information. Some pseudomalignancies are distinguished from bona fide malignancies mainly by clinical differences (1.118). The difference between a lichenoid keratosis and lichen planus, which may be nearly identical histologically, for example, primarily rests upon the former being a solitary papule and the latter being a rash with more than one lesion. In the OJ Simpson trial, I learned that if the glove does not fit, you must acquit. In dermatopathology, this means that if the pathologic diagnosis does not fit with the clinical situation, you must go back and reconcile.
Pathologists organize most of the histologic findings of skin lesions according to epidermal changes, dermal changes, adipose changes (panniculitis, if inflammatory), patterns or arrangements of inflammatory or neoplastic cells, and specific types of cells found. Architecture of skin lesions (arrangements of cells) is considered along with cytologic changes such as atypia. Cytologic atypia (hyperchromatism, pleomorphism, prominent nucleoli, increased nuclear to cytoplasmic ratio, and abnormal mitoses) is subjective, and the precise quantification of atypia into mild, moderate, or severe is in the eye of the beholder to some extent. Atypia is often used as evidence of malignancy, but it must be considered along with clinical findings and the lesion architecture. Dermatopathologists with a background in clinical dermatology tend to emphasize the clinical information and cellular architecture over the cytologic features. Those with a pathology background often stress cytology at the expense of clinical features and architecture. If the histologic findings do not fit the clinical situation, then the disparity must be rectified!
The art of pathology is to be dogmatic about the diagnosis as often as possible, while not being afraid to hedge and give a differential diagnosis when the diagnosis is uncertain. The correct diagnosis sometimes must be expressed as a list of probabilities, and the helpful pathologist should list the possibilities in the order of likelihood. Pathologists may be subcategorized into home-run hitters and hedgers. The home-run hitters try to “force” a diagnosis, and give only one most likely diagnosis. They are either very, very correct and look very smart, or else they strike out and miss the diagnosis completely. This can be dangerous. For example, they might diagnose a lesion as a definite Spitz nevus, which subsequently is found to be a melanoma when it metastasizes. Most Spitz nevi can be diagnosed with relative certainty, but there are always those difficult cases for which all the experts can have their opinions, using the best of criteria, but for which there remains an element of uncertainty. Simple histology has its limits in predicting biologic behavior.
Hedger pathologists , by contrast, seldom make a specific diagnosis, and instead often give a long differential diagnostic list, even to the point of listing histologic possibilities that are ridiculous from a clinical standpoint. They rarely strike out, but they are sometimes not very helpful, and are not appreciated by clinicians. Frequently these pathologists might add the comment to the report that “clinical correlation is recommended,” feeling that this will relieve them from having to do any correlation themselves. They dream of the clinician doing the correlation based upon the pathologist’s microscopic description. Unfortunately, some of the clinicians are in no better position to do the correlation either, so then this type of report becomes worthless. Someone simply has to take the responsibility for making sense of it all and doing the correlation, and simply punting this duty back and forth between the clinicians and the pathologists does no good. Sometimes they actually may need to speak to one another. The lack of clinical correlation is one of the biggest problems seen frequently in dermatopathology, probably more commonly than errors of fact. Wise pathologists avoid the two extremes of the home-run hitter and the hedger.
Acantholysis (1.2)
Atrophy of epidermis (1.9)
Dyskeratosis (1.27)
Follicular plugging (1.47)
Horn cysts (1.59)
Hypergranulosis (1.60)
Hyperplasia of epidermis (1.61)
Hypogranulosis (1.63)
Liquefaction degeneration of basal layer (1.64)
Necrotic keratinocytes (1.87)
Papillomatosis (1.102)
Parakeratosis (1.104)
Pseudoepitheliomatous (pseudocarcinomatous) hyperplasia (1.116)
Spongiosis (1.132)
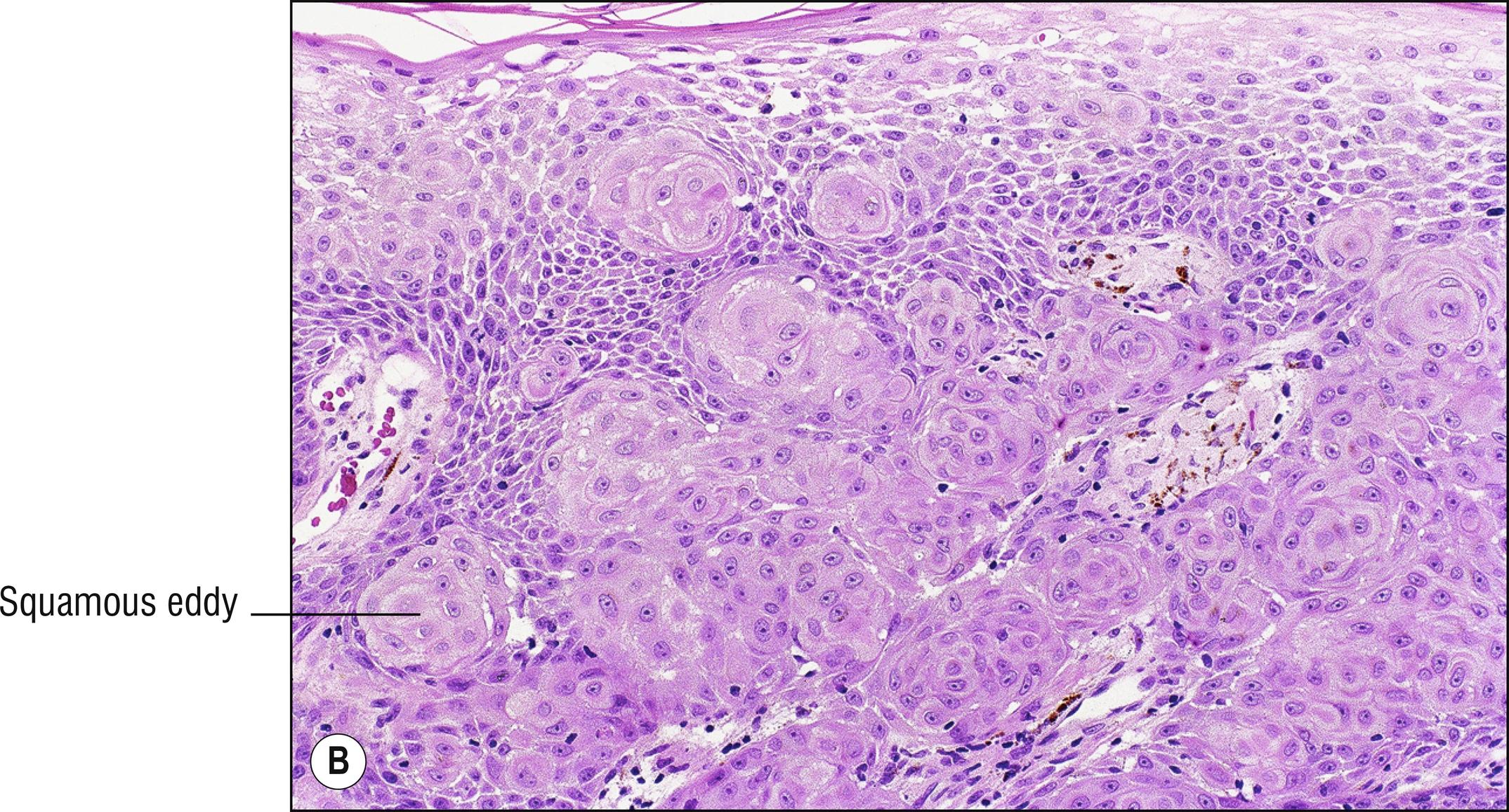
Squamous eddies, keratin pearls, and squamatization (1.134)
Transepidermal elimination (1.140)
Vacuolization of keratinocytes (1.144)
Atrophy of dermis (1.8)
Black deposits (1.12)
Blue amorphous material (1.15)
Brown deposits (1.17)
Calcification (1.19)
Edema of dermis (1.30)
Elastic tissue changes (1.31)
Eosinophilic pink amorphous material (1.35)
Hemosiderin (1.58)
Melanin incontinence (1.79)
Mucin and myxomatous changes (1.83)
Scars, sclerosis, fibrosis (1.125)
Thrombi (1.137)
Basaloid cells (1.11)
Clear or pale cells (1.22)
Eosinophils (1.36)
Epithelioid cells (1.38)
Extravasated erythrocytes (1.40)
Foam cells (1.46)
Granulomas (1.51)
Lymphocytes and histiocytes (1.76)
Mast cells (1.78)
Multinucleated giant cells (1.84)
Neutrophils (1.89)
Plasma cells (1.111)
Small cells (“oat cells”) (1.130)
Spindle cells (1.131)
Epidermotropism and pagetoid proliferation (1.37)
Folliculitis (1.47)
Grenz zone (1.53)
Interface dermatitis (1.64)
Interstitial dermatitis (1.65)
Lichenoid dermatitis (1.72)
Nodular and diffuse dermatitis (1.91)
Panniculitis (1.101)
Perivascular dermatitis, superficial (1.109)
Perivascular dermatitis, superficial and deep (1.109)
Single filing of cells (1.128)
Vasculitis (1.145)
(see also Trunk lesions 1.141, Umbilicus lesions 1.143)
Accessory nipple (29.12)
Cutaneous endometriosis (29.9)
Dysplastic nevus (20.5)
Melanocytic nevus (20.5)
Omphalomesenteric duct remnant (29.11)
Pemphigoid gestationis (6.3)
Pruritic urticarial plaques of pregnancy (3.6)
Seborrheic keratosis (18.2)
Striae (27.2)
Acantholysis is the loss of cohesion between keratinocytes as a result of dissolution of intercellular connections, sometimes resulting in an intraepidermal vesicle. Acanthocyte is an old name for keratinocyte, and means “prickle cell,” referring to the desmosomal spines that normally connect the cells. The process differs from spongiosis (1.9) in that acantholytic keratinocytes tend to be rounded rather than elongated, the desmosomal spines appear destroyed rather than stretched, and exocytosis of lymphocytes into the epidermis is usually absent. Dyscohesive melanocytes in melanoma (20.11) may resemble acantholysis (20.11), but in this situation the term acantholysis is not used (call it “dyscohesion”).
Actinic keratosis (sometimes) (18.8)
Darter’s disease (11.3)
Familial dyskeratotic comedones (10.1)
Galli-Galli disease (17.10, rare)
Hailey–Hailey disease (5.5)
Herpes virus infection (14.2)
Impetigo (occasionally) (12.2)
Incidental finding or artifact
Pemphigus (all varieties, 5.4)
Pityriasis rubra pilaris (2.10, rarely)
Squamous cell carcinoma (sometimes) (18.11)
Acantholytic acanthoma (benign horn-like growth with acantholysis)
Staphylococcal scalded skin syndrome (12.2)
Transient acantholytic dermatosis (Grover’s disease) (5.6)
Warty dyskeratoma (18.7)
This is a clinical group of conditions characterized by erythematous papules, pustules, and/or comedones, resembling acne (pilosebaceous unit inflammation). See also Follicular eruptions (1.47), Neutrophil eruptions (1.89), and Comedones (1.24).
Acne variants (10.1)
Arthropod bites (15.7)
Bowel bypass syndrome (4.1)
Candidiasis (13.4)
Dermatitis herpetiformis (6.5)
Drug-induced acneiform eruptions (3.5)
Folliculitis (10.2)
Grover’s disease (5.6)
Impetigo (12.1)
Miliaria (10.6)
Perioral dermatitis (10.1)
Pustular vasculitis (4.1)
Pyoderma faciale (10.1)
Varicella (14.2)
Alopecia is hair loss. It is commonly subdivided into scarring and non-scarring. Some pathology laboratories prefer to section punch biopsies of alopecia both horizontally and vertically, to maximize the view of more follicles. This author is not a fan of horizontal scalp biopsy sections, but nevertheless they are popular. Vertical scalp biopsies perform comparably to horizontal ones, but some laboratories prefer to receive two biopsies, one for vertical sectioning and one for horizontal, or to subdivide and section a single biopsy both ways.
Alopecia areata (10.9)
Androgenetic alopecia (10.12)
Drug-induced alopecia (3.5)
Genodermatoses: Ectodermal dysplasia (11.2), Progeria (9.6), Rothmund–Thomson syndrome (11.5), etc.
Hair shaft disorders (most are not covered in this book): trichorrhexis nodosa, monilithrix, trichorrhexis invaginata (11.1), pili annulati, pili torti, trichothiodystrophy, mechanical trauma, etc.
Lipedematous alopecia (10.13)
Psoriasis, severe (2.8)
Seborrheic dermatitis, severe (2.1)
Syphilis, secondary (12.13)
Telogen effluvium (10.14)
Temporal arteritis
Thyroid disease
Traction alopecia (can scar if severe, 10.11)
Trichotillosis (10.11)
Acne keloidalis nuchae (10.2)
Alopecia mucinosa (10.8)
Alopecia neoplastica (secondary to neoplasm, especially metastatic, on the scalp, Chapter 28 )
Aplasia cutis congenita (17.4)
Burns (6.7)
Folliculitis (10.2)
Herpes zoster (14.2)
Lichen planopilaris (2.11)
Lupus erythematosus (17.6)
Nevus sebaceus (21.2)
Pemphigoid, cicatricial (6.2)
Pseudopelade of Brocq (10.10)
Radiodermatitis (9.2)
Scleroderma and morphea (9.3)
Tinea capitis (13.1)
Trauma (10.11)
These lesions form clinical rings. Similar terms are gyrate and circinate. See also Serpiginous (1.127), Linear (1.73), and Reticulated (1.123).
Cutis marmarata (3.10)
Erythema ab igne (3.9)
Erythema annulare centrifugum (3.3)
Erythema chronicum migrans (12.14, Lyme disease, also in infectious group)
Erythema gyratum repens (3.4)
Erythema marginatum (3.1, rheumatic fever, also in infectious group)
Erythema multiforme (3.2)
Livedo reticularis (3.10)
Necrolytic migratory erythema (3.2)
Urticaria (3.1)
Chromomycosis, rarely annular (13.10)
Hansen’s disease (12.12)
Impetigo (12.1)
Lupus vulgaris (12.10)
Syphilis, more annular on the face in black skin (12.13)
Tinea (13.1)
Warts, especially recurring after cryotherapy (14.1)
Granuloma annulare and actinic granuloma (7.1)
Sarcoidosis (7.5)
Eczema, especially nummular (2.1)
Erythrokeratodermia variabilis (11.1)
Ichthyosis linearis circumflexa (11.1)
Lichen planus (2.11)
Pityriasis rosea (2.4)
Psoriasis (2.8)
Reiter’s disease (circinate balanitis, 2.8)
Seborrheic dermatitis (2.1)
Chronic bullous disease of childhood (6.4)
Linear IgA bullous dermatosis (6.4)
Pemphigus (5.4)
Subcorneal pustular dermatosis (2.8)
Basal cell carcinoma (18.14)
Desmoplastic trichoepithelioma (22.2)
Mycosis fungoides (24.1)
Sebaceous hyperplasia (21.1)
Targetoid hemosiderotic hemangioma (25.2)
Elastosis perforans serpiginosa (9.13)
Lupus erythematosus (especially subacute cutaneous lupus erythematosus, 17.6)
Porokeratosis (18.4)
Purpura annularis telangiectodes (Majocchi’s disease, 4.8)
(see also Hand lesions 1.56, Leg lesions 1.67)
Actinic keratosis (18.8)
Arthropod bites (15.7)
Basal cell carcinoma (18.14)
Contact dermatitis (2.2)
Eczema (2.1)
Erythema multiforme (3.2)
Granuloma annulare (3.1)
Keratosis pilaris (10.5)
Lentigo simplex (20.3) and solar lentigo (20.4)
Lichen planus (2.11)
Melanocytic nevus (20.5)
Psoriasis (especially elbows, 2.8)
Solar purpura (4.15)
Squamous cell carcinoma (18.11)
Trauma
Atypical mycobacteria (12.11)
Epidermal nevus (18.1)
Idiopathic guttate hypomelanosis (17.10)
Lichen striatus (2.5)
Lupus erythematosus (17.6)
Pseudoxanthoma elasticum (axilla, antecubital, 9.8)
Sporotrichosis (13.11)
Drug eruption (3.5)
Gonococcemia (12.18)
Gout (8.5)
Loefgren’s syndrome (7.5)
Lupus erythematosus (17.6)
Lyme disease (12.14)
Multicentric reticulohistiocytosis (7.8)
Psoriasis (2.8)
Pyoderma gangrenosum (4.12)
Reiter’s disease (2.8)
Relapsing polychondritis (17.8)
Rheumatic fever (12.2)
Rheumatoid arthritis (3.7, 4.1, 7.3)
Schmid’s triad (16.8)
Schnitzler syndrome (3.1)
Sepsis and subacute bacterial endocarditis (4.1)
Sweet’s syndrome (3.7)
Vasculitis (4.1)
Viral infections ( Chapter 14 )
Yersiniosis (1.7)
Dermal atrophy is a decreased thickness of the dermis. In most of these diseases, the epidermis is also atrophic (1.9). In some of them, the dermis is not actually thin, but adipose tissue is deposited higher up in the dermis than usual, or the fat clinically appears herniated, due to lack of dermal support, even though the dermis is not actually thin. Panniculitis ( Chapter 16 ) can also produce the appearance of dermal atrophy, although the atrophy is primarily in the adipose.
Acrodermatitis chronica atrophicans (12.14)
Aging skin (9.1)
Anetoderma (9.11)
Aplasia cutis congenita
Atrophoderma of Pasini and Pierini (9.4)
Corticosteroids (especially injected)
Focal dermal hypoplasia (Goltz syndrome, 11.8)
Morphea (9.4)
Nevus lipomatosus (29.1)
Piezogenic pedal papules (29.1)
Scars (27.2)
Epidermal atrophy is a decreased thickness of the epidermis, particularly the spinous layer.
Acrodermatitis chronica atrophicans (12.14)
Actinic keratosis , atrophic (18.8)
Aging , sun-damaged , or radiation-damaged skin (9.1, 9.2)
Anetoderma (9.11)
Aplasia cutis congenita (17.4)
Atrophie blanche (4.13)
Atrophoderma (9.4)
Corticosteroids (especially topical)
Degos disease (4.10)
Dermatomyositis (17.7)
Graft-versus-host disease, chronic (17.3)
Lichen planus, atrophic (usually acanthotic, 2.11)
Lichen sclerosus (9.5)
Lupus erythematosus (17.6, always consider when extreme atrophy)
Necrobiosis lipoidica (7.2)
Neoplasms in the dermis will often cause epidermal atrophy
Poikiloderma atrophicans vasculare (24.1)
Poikiloderma congenitale (11.5)
Porokeratosis (18.4, central portion sometimes)
Progeria (Werner’s syndrome, 9.6)
Scar (27.2)
Striae (27.2)
Acanthosis nigricans (18.5)
Acrochordons (27.4)
Axillary granular parakeratosis (1.27)
Candidiasis (13.4)
Chromhidrosis
Contact dermatitis (2.2)
Cystic hygroma (25.10)
Erythrasma (12.5)
Fibrous hamartoma of infancy (27.9)
Fox–Fordyce disease (10.7)
Hailey–Hailey disease (5.5)
Hidradenitis suppurativa (10.1)
Hyperhidrosis
Intertrigo (2.2)
Inverse psoriasis (2.8)
Neurofibromatosis (axillary freckling)
Pemphigus vegetans (5.4)
Pseudoxanthoma elasticum (9.8)
Scabies (15.9)
Seborrheic dermatitis (2.1)
Trichomycosis axillaris (12.5)
Basaloid cells are tumor cells that resemble basal cells of the epidermis (compare with small cells, 1.130). They have a dark oval nucleus and very little cytoplasm.
Basal cell carcinoma (18.14)
Seborrheic keratosis (18.2)
Ameloblastoma (18.14)
Cloacogenic carcinoma (18.14)
Sebaceous tumors (especially sebaceous adenoma, sebaceous epithelioma, and sebaceous carcinoma, Chapter 21 )
Follicular tumors (especially trichoepithelioma and pilomatricoma, Chapter 22 )
Sweat gland tumors ( Chapter 23 )
(compare with Brown deposits 1.17)
Amalgam tattoo (7.6)
Argyria (8.18)
Foreign bodies (7.6)
Mercury (7.6)
Tattoos (7.6)
(see also Blue clinical lesions 1.14 , Brown clinical lesions 1.18)
Angiokeratoma (25.2)
Angiosarcoma (25.7)
Black dermatographism (7.6)
Blue nevus (20.8)
Calciphylaxis (8.15)
Comedo, open (1.24)
Coumarin necrosis (4.18)
Deep fungus infection ( Chapter 13 )
Disseminated intravascular coagulation (4.14)
Ecthyma gangrenosum (12.17)
Eschar
Foreign body or exogenous substance (7.6)
Gangrene
Lentigo simplex (20.3), solar lentigo (20.4)
Melanoma (20.11)
Meningococcemia (12.19)
Purpura (1.120)
Terra firma dermatosis (dirt on the skin)
Vascular neoplasms ( Chapter 25 )
Venous lake (25.2)
Blister (see Vesicles, 1.147)
(see also Brown clinical lesions 1.18, Gray clinical lesions 1.54, and Black clinical lesions 1.13)
Argyria (3.5)
Blue nevus (20.8)
Cyanosis and methemoglobinemia
Cysts ( Chapter 19 , sometimes)
Dermal and subcutaneous nodules (various)
Drugs (3.5, especially chlorpromazine, antimalarials, amiodarone, ezogabine, clofazimine, minocycline)
Erythema dyschromicum perstans (3.11)
Foreign body or tattoo (7.6)
Hidrocystoma (19.11)
Maculae ceruleae (15.7, pediculosis)
Melanocytic nevus (20.5)
Melanoma (20.11)
Mongolian spot (20.10)
Nevus of Ota, Nevus of Ito (20.9)
Ochronosis (8.16)
Purpura (1.120)
Vascular neoplasms ( Chapter 25 )
Argyria (3.5)
Aspergillus infection (13.13)
Cyanosis
Drugs (3.5, tetracycline)
Heavy metal poisoning (mercury, copper)
Hemorrhage (1.121, old)
Pseudomonas infection (12.17)
Wilson’s disease
Anemia, iron deficiency
Corticosteroid therapy
Ehlers–Danlos syndrome (9.9)
Ezogabine
Marfan syndrome (9.9)
Minocycline
Myasthenia gravis
Nevus of Ota (20.9)
Ochronosis (8.16)
Osteogenesis imperfecta (9.9)
Pseudoxanthoma elasticum
Thinning of the sclera revealing retina
Buschke–Ollendorff syndrome (27.6, osteopoikilosis)
Conradi–Hunerman syndrome (11.1, chondrodysplasia punctata)
Ehlers–Danlos syndrome (9.9, hypermobile joints)
Epidermal nevus syndrome (18.1)
Epidermolysis bullosa dystrophica (6.6)
Goltz syndrome (11.8, osteopathia striata)
Incontinentia pigmenti (11.6)
Klippel–Trenaunay–Weber syndrome (25.1, bony hypertrophy)
Langerhans cell histiocytosis (24.18, osteolytic lesions)
Leishmaniasis (15.1, bony erosion)
Linear scleroderma (9.3, bony involvement)
Maffucci syndrome (25.1, dyschondroplasia)
Marfan syndrome (9.9, tall, pectus excavatum, arachnodactyly)
McCune–Albright’s syndrome (20.2, polyostotic fibrous dysplasia)
Mycetoma (13.14, erosion and deformity)
Nail–patella syndrome (triangular lunulae, iliac horns, renal failure)
Neoplasms (osteolytic lesions)
Neurofibromatosis (26.1, many bony changes)
Nevoid basal cell carcinoma syndrome (18.14, cysts, hypertelorism, frontal bossing, bifid ribs)
Nevus sebaceus syndrome (21.2)
North American blastomycosis (13.8, infection)
Osteogenesis imperfecta (9.9, brittle bones)
Pachydermoperiostosis (9.7, periosteal proliferation)
Rhinoscleroma (12.9)
Rhinosporidiosis (13.15)
Scrofuloderma (abscess, 12.10)
Syphilis, congenital (12.13, dactylitis, epiphysitis, osteoperiostitis, saddle nose, Higoumenakis sign, saber shins)
T-cell leukemia-lymphoma (24.3, osteolytic lesions)
Xanthoma disseminatum (7.13, osteolytic lesions)
Dematiacious fungi (13.3, 13.10, 13.16)
Foreign bodies (7.6)
Formalin pigment (acid formaldehyde hematin). This is a brown precipitate resulting from hemoglobin in formalin with a pH below 6. It is a common artifact, especially in areas of red blood cells
Gout (8.5)
Hemosiderin (1.58)
Melanin (1.79)
Monsel’s solution (7.6, ferrous subsulfate, used for hemostasis)
Ochronosis (8.16)
Oxalosis (yellow–brown, 8.15)
(see also Black clinical lesions 1.13, Blue clinical lesions 1.14)
Acanthosis nigricans (18.5)
Accessory nipple (29.12)
Albright’s syndrome (20.2)
Cronkhite–Canada syndrome (1.49)
Dermatofibroma (27.1)
Dermatosis papulosa nigra (18.2)
Dowling–Degos disease (17.10)
Drugs (3.5, phenothiazines, meclorethamine, psoralen, arsenic, etc.)
Dyskeratosis congenita (11.4)
Endocrinopathies (17.10, Addison’s disease, Cushing’s disease, etc.)
Erythema ab igne (3.9)
Erythema dyschromicum perstans (2.15)
Fixed drug eruption (3.5)
Goltz syndrome (11.8)
Granuloma faciale (4.2)
Hemochromatosis (8.17)
Incontinentia pigmenti (11.6)
Laugier–Hunziker syndrome (17.10)
Leopard syndrome (20.3)
Liver and kidney disease (1.75, 1.66)
Macular amyloidosis (8.40)
Melanocytic neoplasms ( Chapter 20 )
Melasma (17.10)
Ochronosis (8.16)
Pellagra (2.1)
Phytophotodermatitis (1.110)
Pigmented basal cell carcinoma (18.14)
POEMS syndrome (24.12)
Post-inflammatory hyperpigmentation (17.10)
Riehl’s melanosis (17.10)
Seborrheic keratosis (18.2)
Stasis dermatitis (2.1)
Terra firma dermatosis (dirt on the skin)
Tinea nigra (13.3)
Tinea versicolor (13.2)
Transient neonatal pustular melanosis (5.2)
Urticaria pigmentosa (24.17)
Calcium salts appear as dark blue to purple, brittle deposits on H&E stain (shatter into shards like peanut brittle candy that has been cut by a butter knife). Sometimes instead it has the appearance of bluish granular material. Calcium salts can be stained with alizarin red (more specific) or von Kossa stains (black). Eosinophilic laminated psammoma bodies (1.35) will sometimes calcify, and are seen in meningioma, papillary thyroid carcinoma, and ovarian carcinoma. Schauman bodies are round, blue, calcified, laminated inclusions in multinucleated macrophages, usually seen with sarcoidosis (7.5), but also seen with other granulomas (1.51). Calcareous bodies (purplish oval calcified concretions) are seen with cysticercosis (15.3) and other parasites.
Acrodermatitis chronica atrophicans (12.14)
Basal cell carcinoma (18.14)
Calcifying aponeurotic fibroma (27.16)
Calciphylaxis (8.15)
Cysts (especially pilar, 19.2)
Dermatomyositis (17.7)
“Dystrophic” calcification (8.15)
Foreign bodies, trauma, and injection sites (7.6)
Gout (8.5)
“Metastatic” calcification (8.15)
Osteoma cutis (29.8)
Panniculitis ( Chapter 16 , especially pancreatic fat necrosis, lupus profundus, and subcutaneous fat necrosis of the newborn)
Perforating calcific elastosis (9.8)
Peyronie’s disease (27.15)
Pilomatricoma (22.3)
Proliferating trichilemmal cyst (22.4)
Pseudoxanthoma elasticum (9.8)
Subepidermal calcified nodule (8.15)
Scleroderma (9.3, especially CREST syndrome)
Trichoepithelioma (22.2)
(see also Lip lesions 1.74)
Acrodermatitis enteropathica (17.1)
Actinic cheilitis (18.8)
Candidiasis (13.4)
Cheilitis granulomatosis (7.7)
Contact dermatitis (2.2)
Drugs (retinoids, etc., 3.5)
Erythema multiforme (3.2)
Herpes simplex (14.2)
Lip licking (2.2)
Sarcoidosis (7.5)
Squamous cell carcinoma (18.11)
Verruca plana (14.1)
Xerotic eczema (2.1)
(see also Linear lesions 1.73)
Mondor’s disease (4.16)
Sclerosing lymphangitis of penis (4.16)
Superficial thrombophlebitis (16.7)
Trauma
Trousseau’s syndrome (4.16)
(see also Vacuolization of keratinocytes 1.144, Pale epidermis 1.99)
The cells of these neoplasms appear similar to foam cells (1.46), but the cytoplasm is more uniformly pale or clear rather than bubbly. The paleness is usually due to the removal of a substance from the cytoplasm during processing, generally glycogen, mucin, or lipid.
Adipose tumors ( Chapter 29 )
Balloon cell nevus and balloon cell melanoma (20.5 and 20.11)
Clear cell acanthoma (18.6)
Clear cell basal cell carcinoma (18.14)
Clear cell hidradenoma (23.9)
Clear cell sarcoma (20.11)
Clear cell syringoma (23.7)
Eccrine carcinoma (23.13)
Hidroacanthoma simplex (23.10)
Metastatic renal cell carcinoma (28.4)
Pagetoid diseases (1.37)
PEComa (27.21)
Pilomatricoma (shadow cells, 22.3)
Sebaceous gland tumors ( Chapter 21 )
Squamous cell carcinoma (18.11)
Trichilemmoma (22.5)
“Cleft” is used here to mean an empty space. It may have previously contained fluid, crystals, lipid, or some other material that was removed during processing of the tissue, but in some cases it is simply an artifact. We have excluded vesicles and bullae, vascular spaces, and spaces in which there is some evidence of materials within them.
Actinic keratosis (18.8): occasional separation at dermal/epidermal junction (“Freudenthal’s lacunae”)
Amyloidosis (8.4) and Colloid milium (8.2): fissured clefts within hyalinized material
Basal cell carcinoma (18.14): prominent retraction of tumor from surrounding stroma (“stromal retraction”)
Cholesterol clefts: oblong-shaped clefts
Cysts (19.1): clefts around loose keratin flakes
Darier’s disease (11.3) and warty dyskeratoma (18.7): suprabasal lacunae
Gout (8.5): needle-shaped clefts within gouty deposits
Lichen planus (2.11): occasional cleft between dermal/epidermal junction due to liquefaction degeneration (“Max Josef space”)
Paraffinoma (7.6): Swiss cheese holes in dermis
Scleredema (8.12) and sclerotic fibroma (27.1): clefts between collagen bundles
Spitz nevus (20.6): prominent clefts around melanocytic nests
Subcutaneous fat necrosis and sclerema neonatorum (16.4 and 16.5): small needle-shaped clefts in the subcutaneous fat
Acne variants (10.1)
Dilated pore of Winer (22.1)
Familial dyskeratotic comedones (10.1)
Favre–Racouchot syndrome and actinic damage (9.1)
Nevus comedonicus (18.1)
Trichofolliculoma (22.1)
Trichostasis spinulosa (22.1)
A cyst is a closed cavity or localized sac containing fluid or some fluctuant material, often lined by epithelium. Unlined cysts are sometimes called pseudocysts. The horn pseudocysts of seborrheic keratosis are called pseudocysts because they are really invaginations of a papillomatous epidermis. Most of the “ true “ lined cysts are in Chapter 19 . Others are listed here.
Abscess (12.1)
Auricular pseudocyst (19.13)
Conventional cysts ( Chapter 19 )
Digital mucous cyst (8.9)
Focal mucinosis (8.11)
Follicular neoplasms (especially pilomatricoma, Chapter 22 )
Ganglion cyst (8.9)
Hemangioma (25.1)
Lymphangioma (25.10)
Mucocele (8.10)
Pilonidal cyst (10.1)
Sweat gland neoplasms (especially solid-cystic hidradenoma, Chapter 23 )
Acanthosis nigricans (18.5)
Bullosis diabeticorum (6.9)
Candidiasis (13.4)
Diabetic dermopathy (pigmented macules of shins, 17.10)
Granuloma annulare, disseminated (7.1)
Hemachromatosis (8.17)
Leg ulcers (1.142)
Lipodystrophy (16.11)
Necrobiosis lipoidica diabeticorum (7.2)
Perforating dermatosis, acquired (9.12)
Progeria (9.6)
Scleredema diabeticorum (8.12)
Xanthomas (7.9)
(see Fig. 1.27A–C )
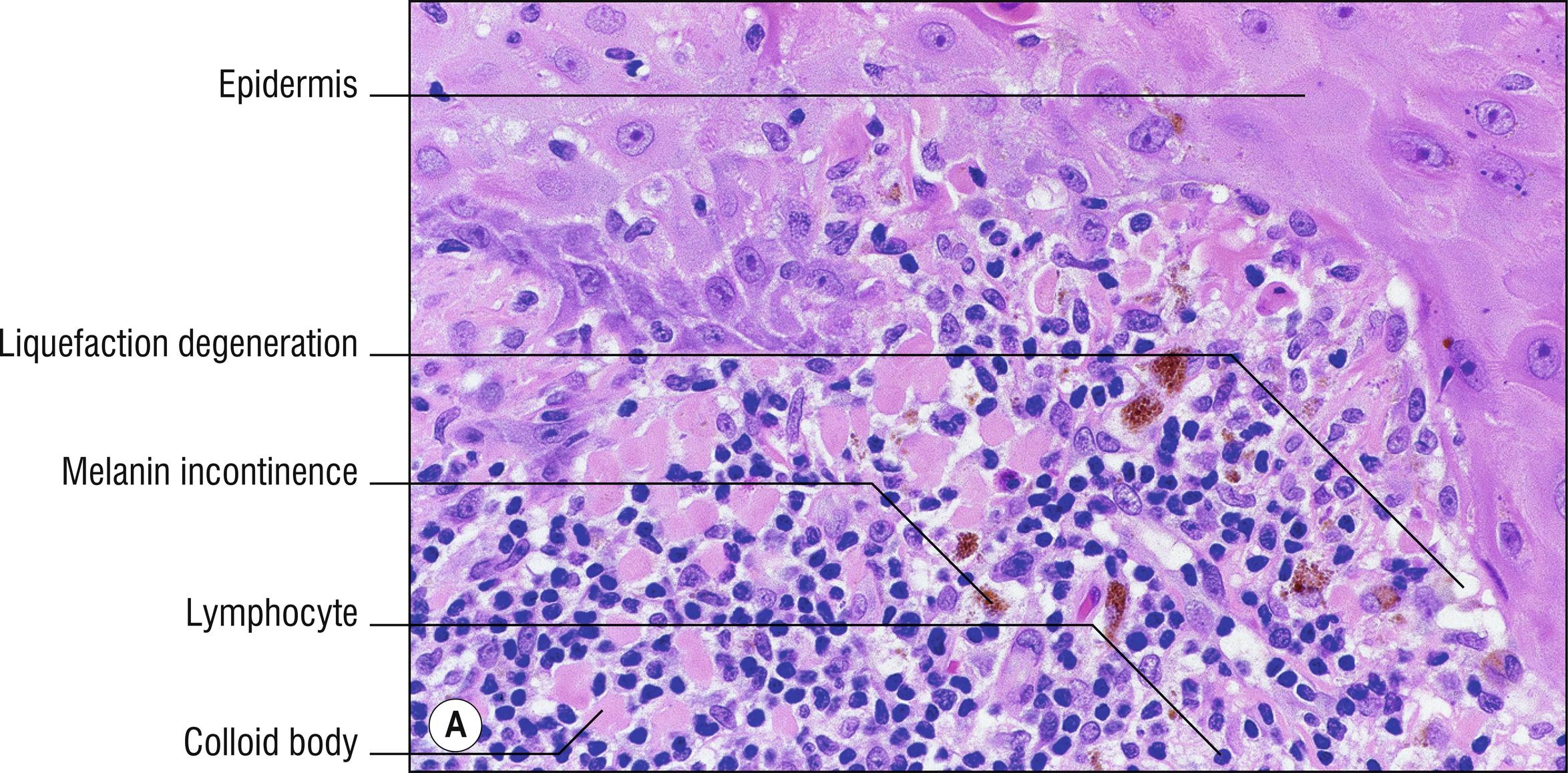

Dyskeratotic cells are abnormally or prematurely cornified individual keratinocytes in the epidermis that stain intensely pink with the H&E stain. A small remnant of a basophilic nucleus may be present. Similar pink blobs have been called colloid bodies , cytoid bodies , hyaline bodies , Kamino bodies (in Spitz nevus), or Civatte bodies when they are present in the deep epidermis or superficial dermis. Colloid bodies generally occur in diseases in which there is interface dermatitis and liquefaction degeneration of the basal layer (1.64), and may actually represent altered collagen or basement membrane, fibrin, and immunoglobulin, as well as degenerated keratinocytes. Caterpillar bodies are linear dyskeratotic cells, colloid bodies or degenerated basement membrane material found on the roof of a blister of porphyria cutanea tarda (8.1), resembling a caterpillar. Corps ronds and grains are acantholytic dyskeratotic cells. Corps ronds have a round nucleus, often with a perinuclear halo, while grains have a more oval, grain-like nucleus. There has been considerable confusion regarding the distinction between dyskeratotic, apoptotic , and necrotic keratinocytes. All appear intensely pink with the H&E stain. They may be impossible to distinguish with routine staining, or they may all represent the same thing. For example, in graft-versus-host disease, some authors refer to these cells as dyskeratotic, while others say that they are necrotic. Hence, there is some duplication between these two lists of diseases (see Necrotic keratinocytes, 1.87).
Acrodermatitis enteropathica (17.1)
Arthropod bites (15.7)
Darter’s disease (11.3)
Familial dyskeratotic comedones (10.1)
Graft-versus-host disease (17.3)
Grover’s disease (5.6)
Hailey–Hailey disease (5.5)
Herpes virus infections (14.2)
Incontinentia pigmenti (verrucous second stage, 11.6)
Lichen planus (2.11)
Lichen sclerosus (9.5)
Lichen striatus (2.5)
Lupus erythematosus (17.6)
Many epithelial neoplasms, especially malignant and irritated benign epidermal tumors ( Chapter 18 ) and irritated benign and malignant adnexal tumors ( 21 , 23 )
Orf and milker’s nodules (14.5)
Pagetoid dyskeratosis: a peculiar incidental finding of dyskeratosis in pale keratinocytes with orthokeratosis, of uncertain significance (1.37)
Porokeratosis (18.4)
Spitz nevus (Kamino bodies, 20.6)
Viral warts (14.1)
Warty dyskeratoma (18.7)
Acanthoma fissuratum (2.3)
Accessory tragus (29.10)
Actinic keratosis (18.8)
Atypical fibroxanthoma (27.12)
Auricular pseudocyst (19.13)
Basal cell carcinoma (18.14)
Calcinosis (8.15)
Chondrodermatitis nodularis helicis (17.9)
Epidermoid cyst (19.1)
Keloid (27.2)
Lentigo maligna (20.11)
Lupus erythematosus (17.6)
Lupus pernio (7.5)
Ochronosis (8.16)
Relapsing polychondritis (17.8)
Seborrheic dermatitis (2.1)
Solar lentigo (20.4)
Squamous cell carcinoma (18.11)
Venous lake (25.2)
Weathering nodules (9.1)
(see also Papulosquamous 1.103)
Eczematous diseases are those characterized by scaling and erythema, and often spongiosis and parakeratosis, suggesting epidermal changes. Papulosquamous diseases are often lumped together with eczematous diseases, but the “splitters” consider papulosquamous lesions to be more hyperkeratotic, thicker and more heaped-up, and more sharply demarcated than eczematous lesions. Further discussion of eczema appears in Section 2.1. Most of the diseases that might be called eczematous appear in Chapter 2 , but others that may exhibit similar clinical morphology are listed here.
Acrodermatitis enteropathica (17.1)
Darier’s disease (11.3)
Desquamation post-erythema in viral exanthems, Kawasaki’s disease, sunburn, scarlet fever, and drug eruptions
Drug eruptions (most are not eczematous, 3.5)
Eczematous and papulosquamous diseases ( Chapter 2 )
Exfoliative erythroderma (1.39)
Follicular mucinosis (10.8)
Ichthyosis (11.1)
Immunodeficiencies (especially Wiscott–Aldrich syndrome, X-linked agammaglobulinemia, 2.1)
Inborn errors of metabolism (especially phenylketonuria, Hurler’s syndrome, Hunter’s syndrome, 2.1, 8.14)
Langerhans cell histiocytosis (purpuric, seborrheic dermatitis-like, 24.18)
Mycosis fungoides (24.1)
Onchocerciasis (15.5)
Scabies (15.9)
Tinea (13.1)
Dermal edema produces paleness in the dermis by the accumulation of interstitial fluid. Paleness in the dermis can also be due to mucin accumulation (1.83). Edema in the epidermis is called spongiosis (1.132).
Acute eczema (2.1)
Arthropod bites (15.7)
Burns (6.7)
Cellulitis and erysipelas (12.3)
Contact dermatitis (2.2)
Erythema multiforme (3.2)
Fixed drug eruption (3.5)
Lichen sclerosus (9.5)
Lymphedema
Polymorphous light eruption (17.5)
Sweet’s syndrome (3.7)
Urticaria (3.1)
Vasculitis (4.1)
Vesiculobullous diseases (1.147, especially pemphigoid, herpes gestationis, bullous mastocytosis, bullous lupus erythematosus, dermatitis herpetiformis)
Elastic tissue changes may not be apparent with the H&E stain. An index of suspicion is necessary so that special stains, such as the Verhoeff–van Gieson stain may be done.
Acrokeratoelastoidosis (2.15)
Actinic granuloma (7.1)
Anetoderma (macular atrophy) (9.11)
Blepharochalasis (9.10)
Connective tissue nevus (27.6)
Cutis laxa (9.10)
Elastofibroma (27.6)
Elastosis perforans serpiginosa (9.13)
Erythema ab igne (3.9)
Mid-dermal elastolysis (9.15)
Pseudoxanthoma elasticum (9.8)
Perforating calcific elastosis (9.8)
Scars and keloids (27.2)
Solar elastosis (9.1)
Striae distensae (27.2)
Calcinosis cutis (8.15)
Dermatitis herpetiformis (6.5)
Epidermolysis bullosa (6.6)
Frictional lichenoid dermatosis (2.3)
Granuloma annulare (7.1)
Lichen simplex chronicus and prurigo nodularis (2.3)
Lipoid proteinosis (8.3)
Psoriasis (2.8)
Rheumatoid nodule (7.3)
Tuberous xanthoma (7.9)
The following neoplasms have a tendency to be sharply circumscribed or encapsulated in the dermis or the subcutaneous fat, without an obvious connection to the epidermis.
Angioleiomyoma (29.6)
Giant cell tumor of tendon sheath (27.9)
Lipomas (29.2)
Neurilemmoma (26.2)
Neurofibroma (26.1)
Pilomatricoma (22.3)
Solitary glomus tumors (25.5)
Sweat gland tumors ( Chapter 23 ): hidradenoma papilliferum, cylindroma, nodular hidradenoma, eccrine spiradenoma
Angiolymphoid hyperplasia with eosinophilia (25.4)
Atopic dermatitis (2.1)
Churg–Strauss syndrome (4.5)
Coccidioidomycosis (13.6)
Drug eruptions (3.5)
Eosinophilia–myalgia syndrome (3.5)
Eosinophilic fasciitis (9.3)
Hypereosinophilic syndrome (24.16)
Internal malignancy
Mycosis fungoides (24.1)
Parasitosis (internal or in skin, Chapter 15 )
Pemphigoid (6.1)
Schmid’s triad (16.8)
Urticaria (3.1)
Eosinophilic material appears in these diseases (usually in the dermis). The terms hyaline or hyalinized are often used to refer to homogenized pink material in general. Hyaline is generally periodic acid-Schiff (PAS)–positive and diastase resistant. The term sclerosis (1.125) is used for hyalinized collagen with decreased fibroblasts. Psammoma bodies are laminated, hyalinized, or calcified structures that may be found with meningioma (26.6), melanocytic nevus (20.5), thyroid carcinoma, or psammomatous melanotic Schwannoma (26.2).
Amyloidosis (8.4)
Ancient melanocytic nevus (20.5)
Colloid (hyaline) bodies (1.27)
Colloid milium (8.2)
Corticosteroid material
Eosinophilic cellulitis (flame figures, 3.8)
Fibrin and thrombi (1.137)
Fibrous proliferations (scar, keloid, fibromatosis) (1.125, Chapter 27 )
Gout (see Section 8.5)
Granuloma with caseation (1.51)
Juvenile hyaline fibromatosis (8.3)
Kamino bodies (1.27)
Lichen sclerosus (9.5)
Lipoid proteinosis (8.3)
Necrobiosis lipoidica (7.2)
Necrosis (1.86, 1.87)
Porphyria (especially erythropoietic protoporphyria, 8.1)
Radiodermatitis , chronic (9.2)
Rheumatoid nodule (7.3)
Russell bodies (1.111)
Scleroderma (9.3)
Sweat gland tumors (especially cylindroma, eccrine spiradenoma, and nodular hidradenoma, Chapter 23 )
Vasculitis (especially hyalinizing segmental vasculitis, in which vessel walls become hyalinized, Chapter 4 )
(see Fig. 1.36A , B )
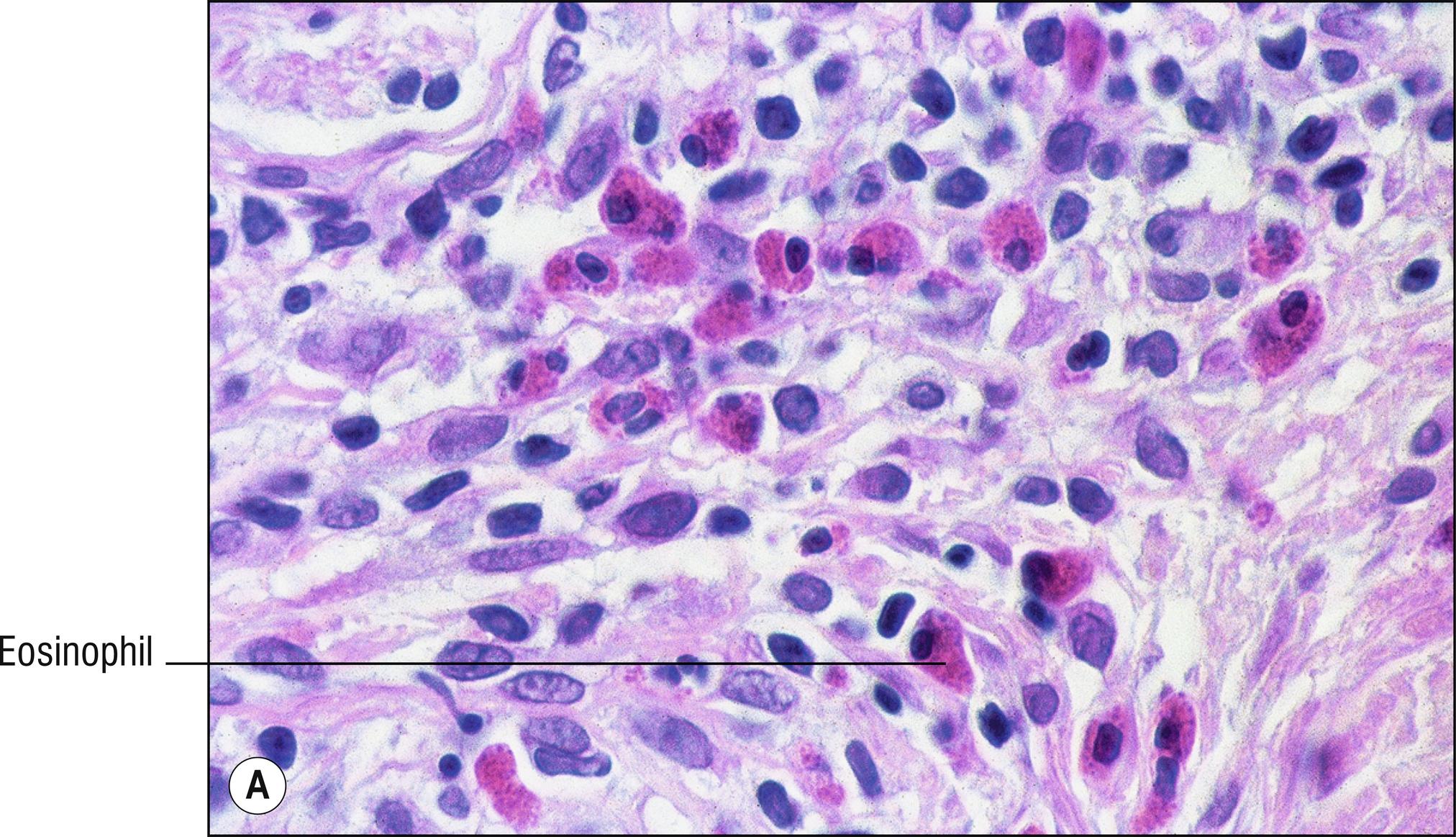
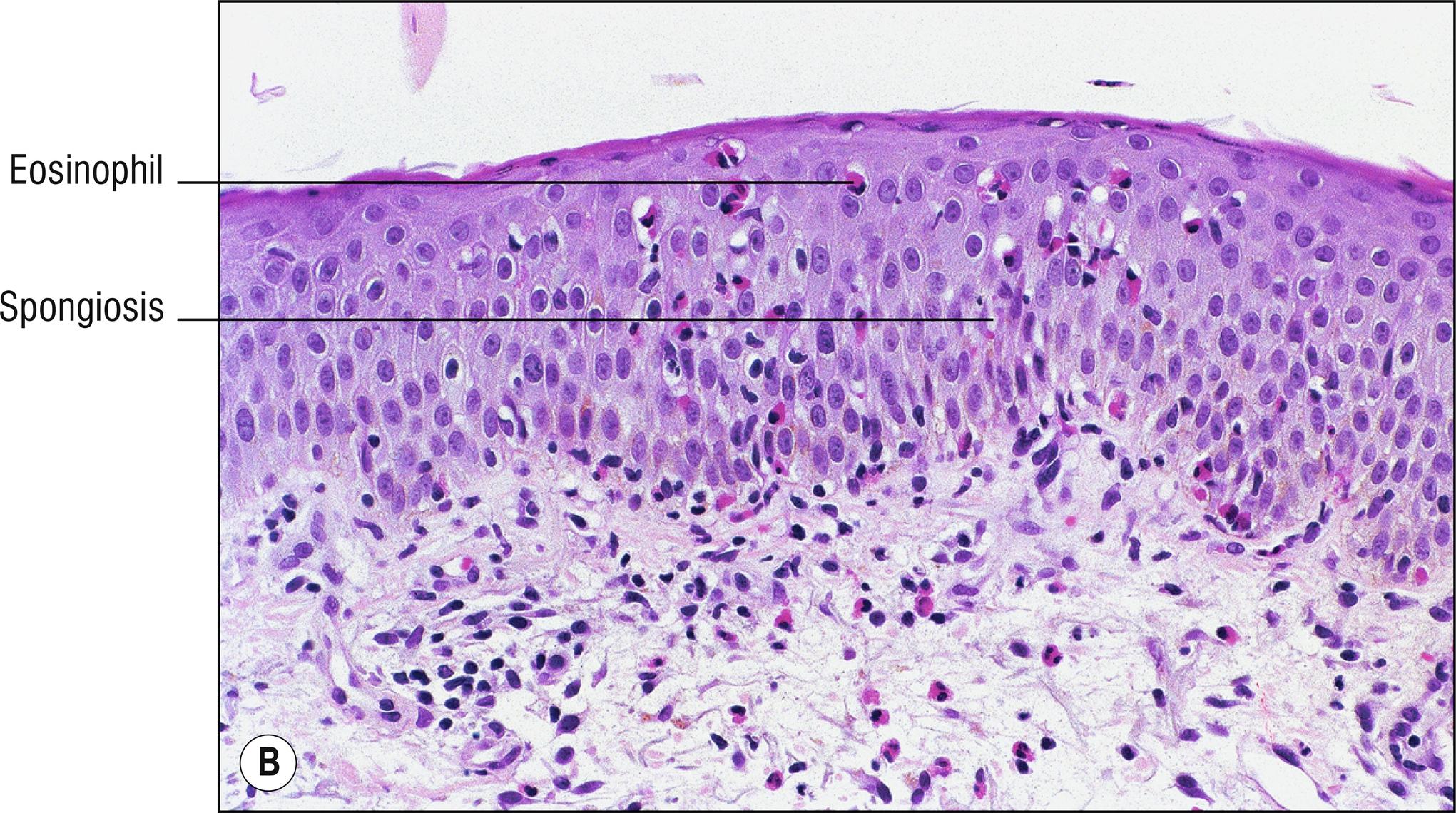
Eosinophils have a bilobed nucleus (fewer lobes than neutrophils), and prominent eosinophilic granules in the cytoplasm. The presence of eosinophils in the skin can be non-specific, but the following conditions should be considered if eosinophils are easy to find. Some diseases, such as lupus erythematosus, usually do not have eosinophils at all.
Allergic contact dermatitis (2.2)
Arthropod bites (15.7)
Eosinophilic pustular folliculitis (10.2)
Erythema toxicum neonatorum (5.3)
Incontinentia pigmenti (11.6)
Pemphigus and pemphigoid (5.4 and 6.1)
Angiolymphoid hyperplasia with eosinophilia (25.4)
Arthropod bites and parasitic infestations ( Chapter 15 )
Coccidioidomycosis and occasionally other deep fungi (13.6)
Contact dermatitis (2.2)
Dermatitis herpetiformis (6.5)
Dermatophytosis (sometimes, 13.1)
Drug eruptions (3.5)
Eczema (especially atopic dermatitis) (2.1)
Eosinophilic cellulitis (Wells syndrome) (3.8)
Eosinophilic dermatosis of hematologic malignancy
Eosinophilic pustular folliculitis (10.2)
EPPER (eosinophilic polymorphic pruritic eruption associated with radiotherapy, 9.2)
Erythema multiforme (sometimes, 3.2)
Granuloma annulare (sometimes, 7.1)
Granuloma faciale (4.2)
Hodgkin’s lymphoma (24.15)
Hypereosinophilic syndrome
Juvenile xanthogranuloma (7.10)
Langerhans cell histiocytosis (24.18)
Mycosis fungoides (24.1)
Pemphigoid gestationis (6.3)
Pemphigus (5.4) and pemphigoid (6.1)
Pruritic urticarial papules and plaques of pregnancy (PUPPP, 3.6)
Urticaria (3.1)
Urticaria pigmentosa (24.17)
Urticarial vasculitis (4.1), eosinophilic vasculitis (4.1), and Churg–Strauss vasculitis (4.5)
(see also Clear cell neoplasms 1.22)
Epidermotropism refers to migration of malignant cells into the epidermis, usually without significant spongiosis. Exocytosis refers to the migration of cells (usually lymphocytes, neutrophils, or eosinophils) into the epidermis, usually in association with spongiosis (1.132), and usually used for benign conditions. Pagetoid cells are cells in the epidermis, often pale or atypical, resembling Paget’s disease. Pagetoid cells may or may not arrive in the epidermis by means of epidermotropism. Pagetoid melanocytes ( Chapter 20 ) are best known in melanoma, but are also seen in benign melanocytic neoplasms such as Spitz nevus, pigmented spindle cell nevus, congenital nevus in neonates, recurrent nevus, and acral nevus. Care must be taken not to mistake melanocytes in tangentially sectioned epidermis for pagetoid cells, nor to mistake common artifactual vacuoles around keratinocytes for pagetoid cells (1.144).
Paget’s disease : pale cells with adenocarcinoma staining features. Carcinoembryonic antigen (CEA), EMA, CK-7, CK-8, usually positive. Mucin in cytoplasm is often positive with mucicarmine, Alcian blue, colloidal iron, and PAS with and without diastase. Basal cells are often compressed and uninvolved. No dyskeratosis
Bowen’s disease (squamous cell carcinoma in situ, 18.10): pale keratinocytes may be present which contain glycogen (PAS positive, diastase labile) with frequent dyskeratosis (1.27). Full-thickness atypia often involves basal cells also. High molecular weight keratin positive. Mucin stains, CEA, EMA, CK-7, CK-8, and low molecular weight keratin negative. However, cases have been published with exceptions, such as positive staining for CK-7 and EMA. Usually no pagetoid cells in the stratum corneum, which sometimes occurs with Paget’s disease and melanoma
Borst–Jadassohn phenomenon: discrete clones of basaloid, squamatized, or pale keratinocytes in the epidermis that appear different than their neighbors. This can be benign or malignant. It is mainly seen with irritated seborrheic keratosis (18.2) or Bowen’s disease (18.10), and rarely with hidroacanthoma simplex (a form of eccrine poroma limited to the epidermis, 23.10).
Melanoma (20.11): S-100 (very sensitive, but not specific), HMB-45 and MART-1 (both very specific, but not sensitive) stains positive. Fontana melanin stain is also positive, but is less useful because keratinocytes may contain melanin transferred from melanocytes. Melanosomes by electron microscopy
Mycosis fungoides (24.1): malignant T-lymphocytes (sometimes cerebriform) in spaces called Pautrier microabscesses. Stains such as CD45 (leukocyte common antigen, used for screening), CD4 (T-helper cells), and CD3 (pan-T cells) usually positive
Lymphomatoid papulosis (24.5): CD30 positive large atypical lymphocytes, and most smaller ones in the epidermis stain with T-cell markers
Langerhans cell histiocytosis (24.18): malignant Langerhans cells, often kidney-shaped nuclei, CDla or S-100 positive
Sebaceous carcinoma (21.5): oil red-O stain positive (need frozen section). Sometimes Bowenoid changes (oil red-O negative carcinoma) in the epidermis coexist with sebaceous carcinoma in the dermis. Adipophilin and EMA positivity is useful if frozen section not available
Merkel cell tumor (26.7): small cell tumor (1.130) is almost always present also in the dermis, in addition to the epidermotropic cells. Sometimes Bowen’s disease can coexist, or the small cells enter the epidermis. Merkel cell carcinoma cells are usually positive for CK20 (perinuclear dot pattern) and neuron-specific enolase
Clear cell acanthoma (18.6): discrete clone of pale keratinocytes in a psoriasiform epidermis, positive for glycogen and keratin
Hidroacanthoma simplex (23.10): this is an eccrine poroma with Borst–Jadassohn features, and sweat ducts are present
Pagetoid dyskeratosis (1.27)
Epidermotropic adnexal carcinoma (23.13): rare
Epidermotropic metastatic carcinoma or melanoma: very rare. Usually carcinoma or melanoma cells within the epidermis imply that a neoplasm is primary, but in this case metastatic melanocytes or epithelial cells actually infiltrate the epidermis. This usually can only be diagnosed with certainty when more than one lesion is present, making it more apparent that the lesions are metastatic.
Epithelioid cells are defined as cells that resemble (-oid) epithelial cells (keratinocytes). They have large oval, pale, vesicular nuclei and abundant eosinophilic cytoplasm. The term “epithelioid cell” confuses neophytes because it is most often used to describe large monocyte-derived macrophages (histiocytes, 1.76) that often form granulomas, but is also used to describe many tumor cells that have a similar appearance. Sometimes immunostaining may be needed to identify the type of epithelioid cell. Vimentin will stain all of these (all mesenchymal lesions) except most examples of squamous cell carcinoma (an epithelial neoplasm). SCC stains with cytokeratin cocktail, while epithelioid sarcoma stains with both vimentin and cytokeratin. True histiocytes found in granulomas, atypical fibroxanthoma, and malignant fibrous histiocytoma usually stain with CD68 or alpha-1 antitrypsin. S-100 protein stains melanocytic neoplasms and Langerhans cell histiocytosis. CD la stains only the Langerhans cell histiocytosis. CD31, CD34, and Ulex stain most vascular neoplasms with proliferating endothelial cells (see Chapter 30 ).
Granulomas (1.51)
Melanoma (20.11)
Spitz nevus (spindle and epithelioid cell nevus, 20.6)
Squamous cell carcinoma (18.11)
Angiolymphoid hyperplasia with eosinophilia (“histiocytoid” hemangioma, 25.4)
Atypical fibroxanthoma (27.12)
Epithelioid angiosarcoma (25.7)
Epithelioid sarcoma (27.14)
Langerhans cell histiocytosis (24.18)
Malignant fibrous histiocytoma (27.11)
This is a term used by clinicians for generalized scaling and erythema over an extensive part of the body. It is important to try to determine one of the causes in the following list. The histology depends on which of these is the underlying etiology.
Contact dermatitis (2.2)
Crusted “Norwegian” scabies (15.9)
Darier’s disease (11.3)
Dermatomyositis (17.7)
Drug eruption (3.5)
Eczema (2.1)
Graft-versus-host disease (17.3)
Ichthyosis variants (11.1)
Idiopathic erythroderma (common)
Immunodeficiencies, especially Wiskott–Aldrich syndrome (2.1), Omenn syndrome (2.1)
Mycosis fungoides (especially Sezary syndrome) (24.1)
Onchocerciasis (15.5)
Pemphigus foliaceus (5.4)
Pityriasis rubra pilaris (2.10)
Post-erythema stage of viral exanthems ( Chapter 14 )
Psoriasis (2.8)
Scarlet fever (12.2)
Staphylococcal scalded skin syndrome (12.2)
(see also Purpura 1.120)
Mucha-Habermann disease (2.14) is by far the most common, although erythrocytes may enter the epidermis occasionally in other diseases.
Amyloidosis (8.4)
Cellulitis (12.3)
Gonococcemia (12.18)
Herpes virus infections (14.2)
Langerhans cell histiocytosis (24.18)
Meningococcemia (12.19)
Pityriasis lichenoides (2.14)
Pityriasis rosea (sometimes) (2.4)
Stasis dermatitis (2.1)
Vascular neoplasms ( Chapter 25 )
Vasculitis and purpuric diseases ( Chapter 4 )
(see also Eyebrow lesions 1.42, Eyelid lesions 1.43, Blue clinical lesions 1.14)
Albinism (11.9, nystagmus)
Ataxia telangiectasia (11.2, bulbar telangiectasia)
Atopic dermatitis (2.1, cataracts)
Behçet’s syndrome (4.11, uveitis)
Cat scratch disease (12.15, Parinaud’s oculoglandular syndrome)
Congenital syphilis (12.13, interstitial keratitis)
Cytomegalovirus (14.9, retinitis)
Hansen’s disease (12.12, iritis)
Herpes virus infections (14.2, keratitis, iritis)
Ichthyosis (11.1, mostly corneal changes)
Incontinentia pigmenti (11.6, rarely blindness, strabismus)
Juvenile xanthogranuloma (7.10, xanthogranulomas, glaucoma, iritis)
Kawasaki’s disease (14.10, conjunctivitis)
Loefgren’s syndrome (7.5, iritis)
Neurofibromatosis (26.1, Lisch nodules of iris)
Pretibial myxedema (8.7, exophthalmos)
Pseudoxanthoma elasticum (9.8, angioid streaks, retinal hemorrhages, blindness)
Reiter’s disease (2.8, conjunctivitis, iritis)
Relapsing polychondritis (17.8, ocular inflammation)
Rothmund–Thompson syndrome (11.5, cataracts)
Sarcoidosis (7.5, iritis)
Sturge–Weber syndrome (25.1, glaucoma)
Toxoplasmosis (15.15, chorioretinitis)
Tuberous sclerosis (27.3, several complications)
Vogt–Koyanagi–Harada syndrome (17.2, uveitis)
(see also Madarosis 1.77)
Alopecia areata (10.9)
Dermoid cyst (1.42)
Porphyria (especially EP and PCT, 8.1): hypertrichosis
Seborrheic dermatitis (2.1): scale and erythema
Ulerythema ophryogenes (10.5): follicular plugging and scale
(see also Madarosis 1.77)
Acne rosacea (10.1)
Acrochordon (27.4)
Amyloidosis (8.4)
Angioedema (3.1)
Anthrax (12.4)
Ascher’s syndrome (7.7)
Atopic dermatitis (2.1)
Basal cell carcinoma (18.14)
Cat scratch disease (12.15)
Cellulitis, orbital (12.3)
Chagas disease (Romana’s sign, 15.14)
Chalazion and sty (10.1)
Cicatricial pemphigoid (6.1)
Contact dermatitis (2.2)
Dacryocystitis
Dermatomyositis (heliotrope, 17.6)
Herpes simplex (14.2)
Hidrocystoma (19.11)
Kawasaki syndrome (conjunctivitis, 14.10)
Lipoid proteinosis (8.3)
Measles (conjunctivitis, 14.7)
Milia (19.1)
Molluscum contagiosum (14.4)
Myxedema (8.6)
Necrobiotic xanthogranuloma (7.11)
Pediculosis (phthirus pubis on eyelashes, 15.7)
Reiter’s syndrome (conjunctivitis, 2.8)
Sebaceous carcinoma (4.5)
Seborrheic dermatitis (2.1)
Seborrheic keratosis (18.2)
Stevens–Johnson syndrome (3.2)
Syringoma (23.7)
Thyroid disease
Trichinosis
Vitiligo (17.2)
Xanthelasma (7.9)
(see also Nose lesions 1.95, Eyelid lesions 1.43, Eyebrow lesions 1.42)
Acne (10.1)
Actinic keratosis (18.8)
Atopic dermatitis (especially infants, 2.1)
Basal cell carcinoma (18.14)
Contact dermatitis (2.2)
Demodicosis (15.8)
Dermatosis papulosa nigra
Dilated pore of Winer (22.1)
Epidermoid cyst (19.1)
Follicular neoplasms (most, Chapter 22 )
Herpes simplex and varicella zoster (14.2)
Impetigo (12.1)
Lentigo maligna (20.11)
Lentigo , solar (20.4)
Lupus erythematosus (17.6)
Melanocytic nevus (20.5)
Melasma (17.10)
Nevus sebaceus (21.2)
Photocontact dermatitis (2.2)
Photodermatitis (1.110)
Photodrug reaction (3.5)
Pityriasis alba (2.6)
Port wine stain (25.1)
Pseudofolliculitis barbae (10.2)
Sebaceous hyperplasia (21.1)
Seborrheic dermatitis (2.1)
Seborrheic keratosis (18.2)
Spider hemangiomas (1.136)
Squamous cell carcinoma (18.11)
Verruca plana (14.1)
Angiolymphoid hyperplasia with eosinophilia (25.4)
Angiosarcoma (25.7)
Atypical fibroxanthoma (27.12)
Chronic actinic dermatitis (2.2)
Eosinophilic folliculitis (10.2)
Erysipelas (12.3)
Fifth disease (14.7)
Follicular mucinosis (10.8)
Gianotti–Crosti syndrome (14.11)
Granuloma faciale
Leishmaniasis (15.1)
Lepromatous leprosy (12.12)
Lupus vulgaris (12.10)
Lymphocytoma cutis (24.14)
Nevus of Ota (20.9)
Palisaded encapsulated neuroma (26.8)
Pemphigus erythematosus (5.4)
Polymorphous light eruption (17.5)
Sarcoidosis (7.5)
Sebaceous neoplasms, most ( Chapter 21 )
Solar urticaria (3.1)
Subepidermal calcified nodule (8.15)
Tinea facei (13.1)
Warty dyskeratoma (18.7)
(see also Morbilliform 1.81)
Dermatomyositis (17.7)
Lupus erythematosus (17.6)
Still’s disease
Drug eruption (3.5)
Leukemia, lymphoma ( Chapter 24 )
Loefgren’s syndrome (7.5)
Pustular psoriasis (2.8)
Sweet’s syndrome (3.7)
Weber–Christian disease (16.2)
Foam cells (foamy cells) have a bubbly (foamy) cytoplasm. Most are macrophages (1.76) that have phagocytized lipid material, but some are cells of another derivation that have a similar multivacuolated cytoplasm. Compare with clear cells (1.22). Touton giant cells (1.84) are macrophage-derived multinucleated cells that contain lipid. A wreath of nuclei encircles a smooth pink cytoplasm, and a foamy cytoplasm is present outside the wreath. Touton giant cells are mainly seen in juvenile xanthogranuloma, but can occasionally be seen in other xanthomatous conditions as well.
Atypical fibroxanthoma (27.12)
Atypical mycobacteria and rarely other bacterial infections ( Chapter 12 )
Balloon cell nevus and balloon cell melanoma (20.5 and 20.11)
Dermatofibroma (uncommonly, 27.1)
Fox–Fordyce disease (10.7)
Granular cell tumor (more granular than foamy, 24.18)
Hibernoma (29.4)
Juvenile xanthogranuloma (7.10)
Langerhans cell histiocytosis (24.18)
Leprosy (lepromatous) (12.12)
Liposarcoma (29.5)
Malakoplakia (12.21)
Necrobiotic xanthogranuloma (7.11)
Panniculitis (any type may exhibit foam cells if there is damage to adipose, but foam cells are most characteristic of Weber–Christian disease, Chapter 16 )
Pneumocytosis (15.12)
Rhino scleroma (12.9)
Sebaceous gland tumors ( Chapter 21 )
Verruciform xanthoma (7.12)
Xanthoma disseminatum and other histiocytosis variants (7.13)
Xanthomas (7.9)
Follicular plugging is hyperkeratosis within hair follicles (usually in the infundibulum). In some of these conditions, there is adnexocentric inflammation around follicles or other adnexal structures such as sweat glands. A few of these just appear to be follicular on a clinical basis, such as some of the transepidermal elimination diseases.
Acne variants (10.1)
Atopic dermatitis (2.1)
Darier’s disease (keratosis follicularis) (11.3)
Eczema with follicular accentuation (2.1)
Follicular mucinosis (10.8)
Folliculitis variants (10.2)
Fox–Fordyce disease (10.7)
Graft-versus-host disease (follicular type) (17.3)
Hidradenitis suppurativa (10.2)
Ichthyosis vulgaris (11.1)
Keratosis pilaris (10.5)
Kyrle’s disease (9.12)
Lichen planopilaris (2.11)
Lichen sclerosus (9.5)
Lichen simplex chronicus (2.3)
Lichen spinulosus (10.5)
Lupus erythematosus (17.6)
Miliaria (actually is sweat duct occlusion, 10.6)
Mycosis fungoides, follicular variant (24.1)
Perforating folliculitis (10.3)
Pityriasis rubra pilaris (2.10)
Prurigo nodularis (2.3)
Scurvy and phrynoderma (4.17)
Seborrheic dermatitis (2.1)
Transepidermal elimination diseases (1.140)
Trichostasis spinulosa (10.4)
(see also Hands 1.56, and also Palm and sole 1.100)
Acral lentiginous melanoma (20.11)
Acral pseudolymphomatous angiokeratoma (24.14)
Atherosclerotic ulcers
Buerger’s disease (4.19)
Chilblains (3.12)
Clear cell sarcoma (20.11)
Contact dermatitis (2.2)
Eczema (2.1)
Epidermolysis bullosa (6.6)
Foreign body granuloma (7.6)
Kaposi sarcoma (25.9)
Larval migrans (15.6)
Lichen planus (2.11)
Mycetoma (13.14)
Purpuric glove and sock syndrome (14.7)
Stasis dermatitis and ulcers (2.1, 16.9)
Tinea pedis (13.1)
Tungiasis (15.11)
Arsenical keratoses (keratoses, especially of palms and soles, GI carcinoma, 18.9)
Birt-Hogg Dube syndrome (GI polyps and cancer, 22.6)
Cowden’s disease (trichilemmomas, GI polyps or malignancy, 22.5)
Cronkite–Canada syndrome (hyperpigmentation, alopecia, GI polyps, enteropathy, 17.10)
Dermatomyositis (rash, internal malignancy, 17.7)
Extramammary Paget’s disease (Paget’s disease on skin, GI carcinoma, 18.13)
Gardner’s syndrome (cutaneous cysts, lipomas, desmoid tumors, GI adenomatous polyps, often malignant, 19.1)
Kaposi sarcoma (vascular skin lesions, GI vascular lesions, 25.9)
Leser–Trelat syndrome (rapid onset of seborrheic keratoses, GI carcinoma, 18.2)
Muir–Torre syndrome (sebaceous neoplasms, keratoacanthoma, GI carcinoma, 21.3)
Necrolytic migratory erythema (rash, glucagonoma, 3.2)
Neurofibromatosis (neurofibromas, café-au-lait macules, GI polyps, 26.1)
Pancreatic fat necrosis (panniculitis, pancreatitis or pancreatic carcinoma, 16.8)
Peutz–Jegher’s syndrome (lentigines of lips, small intestinal polyps with malignant potential, 20.3)
Tylosis (palmar–plantar keratoderma, esophageal carcinoma, 2.15)
Blue rubber bleb nevus syndrome (25.1)
Degos disease (infarction and bleeding, 4.10)
Ehlers–Danlos syndrome (9.9)
Epidermolysis bullosa (6.6)
Hemangiomatosis (25.1)
Kaposi sarcoma (25.9)
Osler–Weber–Rendu syndrome (1.136)
Pseudoxanthoma elasticum (9.8)
Vasculitis (especially Henoch–Schoenlein purpura, 4.1)
Acrodermatitis enteropathica (17.1)
Aphthous stomatitis (17.11)
Bowel bypass syndrome (4.1)
Carcinoid (28.5)
Crohn’s disease of the skin (7.7)
Cronkhite–Canada syndrome (17.10)
Dermatitis herpetiformis (gluten sensitive enteropathy often asymptomatic, 6.5)
Erythema nodosum (16.1)
Graft-versus-host disease (17.3)
Mastocytosis (24.17)
Pyoderma gangrenosum (4.12)
Pyoderma vegetans (4.12)
Pyostomatitis vegetans (4.12)
Reiter’s disease (2.8)
Scleroderma (malabsorption, diarrhea, 9.3)
Sweet’s syndrome (3.7)
Typhoid fever (12.2)
Yersiniosis (12.23)
Omphalomesenteric duct remnant (29.11)
(see also Mouth lesions 1.82)
Addison’s disease (melanosis, 17.10)
Amalgam tattoo (pigment, 7.6)
Ameloblastoma (tumor, 18.14)
Cowden’s disease (22.5)
Drug-induced hyperplasia (phenytoin, nifedipine, cyclosporine, etc., 3.5)
Gingivitis due to infection or irritation
Juvenile hyaline fibromatosis (hyperplasia, 8.3)
Kaposi sarcoma (tumor, 25.9)
Leukemia, lymphoma (bleeding, Chapter 24 )
Leukoplakia , traumatic or premalignant (1.71)
Lipoid proteinosis (hyperplasia, 8.3)
Melanoma (tumor, 20.11)
Mucosal pemphigoid (ulcers, 6.2)
Papillon–Lefevre syndrome (periodontitis, 2.15)
Paraneoplastic pemphigus (ulcers, 5.4)
Pemphigus vulgaris (ulcers, 5.4)
Racial pigmentation
Scurvy (bleeding, 4.17)
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here