Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Orthopaedic surgeons continue to see an increase in the incidence of sports-related injuries with much of the population becoming active in more strenuous activity. Nonspecific complaints of pain in the foot, ankle, calf, or shin are often reported, with shin pain as the most common presentation. Evaluation of leg pain requires not only knowledge of the anatomy and biomechanics of the lower extremity but also an understanding of the pathology of the injury. Conducting a thorough history and physical examination and appropriately interpreting diagnostic tests are essential to the establishment of an accurate diagnosis. In addition, specific details regarding physical activity, including training regimens, surface conditions, and shoewear, must be determined because these factors also play a significant role in the diagnosis.
Because several etiologies may present with similar characteristics, patients must be evaluated for multiple conditions. The differential diagnosis of chronic leg pain includes the following conditions: bony or soft-tissue tumors, chronic exertional compartment syndrome (CECS), claudication, isolated leg trauma, medial tibial stress syndrome (MTSS), muscle strains, nerve entrapment, popliteal artery entrapment syndrome (PAES), radiculopathy, referred pain from meniscal pathology, stress fractures, and tendinitis. Despite this wide range of diagnoses, several studies demonstrate that certain conditions are more prevalent among athletes, in particular. There have been reports in the literature of exertional leg pain occurring in 12.8%–82.4% of athletes. In a previous retrospective study of 150 patients with exercise-induced leg pain, CECS was the most prevalent cause of pain, representing 33% of cases; stress fractures and MTSS accounted for 25% and 13% of cases, respectively. More recently, however, studies have shown MTSS to be the most common cause of chronic leg pain in the athlete, accounting for 13%–22% of injuries in runners and dancers, 35% of injuries in Naval recruits, and 5% of all athletic injuries. This chapter focuses on the most common causes of chronic leg pain in athletes, including MTSS, stress fractures, CECS, nerve entrapment, and PAES. The incidence, pathology, clinical presentation, and treatment options are discussed for each condition.
“Shin splits” is a nonspecific diagnosis of posteromedial leg pain commonly used to describe a wide variety of lower leg pain conditions, including chronic ECS, fascial hernia, muscle strains, periostitis, and stress fractures. One of the most common sites of overuse pain is the distal one-third of the medial border of the tibia. Because of this, MTSS may be the most accurate term for this because it describes both the location and the likely pathophysiology of the syndrome.
MTSS typically is observed in runners and individuals involved in jumping activities such as basketball, volleyball, and dancers. Both biologic and biomechanical factors have been reported as possible causes of MTSS. Although the tibialis posterior muscle historically has been implicated as the source of this condition, a study of 50 cadaveric legs revealed that the tibial posterior muscle was more lateral, indicating that this muscle was not a likely source of MTSS. Other studies have identified the soleus, flexor digitorum longus (FDL), and crural fascia as sources of the pain, with more focus on the soleus. Another theory suggests that the pain is due to bony overload of the tibia due to a bending stress produced with weight bearing.
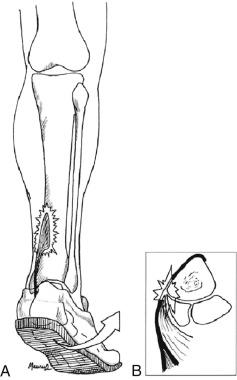
During running, heel strike occurs in relative supination, with pronation of the foot increasing until midstance. Because the soleus is the primary plantarflexor and invertor of the foot, it has been theorized that the medial portion of this muscle contracts eccentrically as the foot pronates ( Fig. 23.1 ). The repetitive eccentric contraction that occurs in hyperpronating athletes may explain the increased incidence of MTSS observed in such athletes. In addition, hyperpronation is a compensatory mechanism that occur in patients with hindfoot and forefoot varus, tibia vara, tight Achilles tendon, and tight gastrocnemius and soleus muscles, therefore such patients also are at increased risk for developing MTSS. Other risk factors for MTSS include female sex, increased weight, higher navicular drop, previous running injury, and greater hip external rotation with the hip in flexion.
The most common complaint associated with MTSS is a recurring, dull ache localized over the distal one-third posteromedial cortex of the tibia ( Case Study 23.1 ). MTSS tends to occur late in the sport season after prolonged activity, whereas stress fractures tend to occur early in an athletic season as stresses increase rapidly. Early in the development of MTSS, patients may experience pain at the beginning of a workout or run but feel a relief of symptoms with continued activity, only to be followed by a recurrence of pain either at the conclusion of the activity or some time afterward. Pain usually is alleviated with rest and generally does not occur at night. However, as this condition progresses, pain may occur throughout training or during low activity, such as walking, and possibly may continue during rest.
A 16-year-old female cross-country runner presented for evaluation of progressive right leg pain. Over the preceding 3 weeks, training intensity had been increased in preparation for a season-ending tournament. During that time, increasing pain developed over the distal medial leg. Initially, pain was present only at the conclusion of training but progressed to include soreness on first arising in the morning and with daily activities, forcing the patient to decrease training. She denied constitutional symptoms, history of trauma, or recent shoewear change.
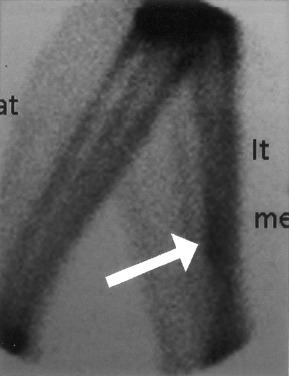
Physical examination was remarkable only for tenderness along the posteromedial cortex of the distal one-third of the tibia. Plain radiographs were normal. On the basis of a clinical diagnosis of MTSS, conservative treatment, consisting of cessation of training for 2 weeks, NSAIDs, and ice, was recommended. At the 2-week follow-up, only minor improvement had been achieved and the patient remained in significant pain. Consequently, a range-of-motion boot was implemented and a bone scan was ordered to rule out a possible stress fracture. Because the bone scan was negative, as indicated by a diffuse uptake in the delayed phase, the patient remained in the range-of-motion boot for an additional 4 weeks. After this period, activities of daily living were conducted without pain, permitting a gradual return to training over the ensuing 6 weeks.
The pathognomonic physical finding in MTSS is palpable tenderness along the posteromedial edge of the distal one-third of the tibia. In rare cases, erythema or localized swelling over the medial tibia also may be observed. Although studies have reported conflicting ranges of motion associated with MTSS, in theory, hypermobile pronating feet are at increased risk of MTSS. Therefore evaluation for foot pronation or subtalar varus also is recommended. Abnormal pulse, diffuse swelling, firm compartments, neurologic deficits, and vibratory pain are not associated with this syndrome.
Roentgenograms generally are normal in patients with MTSS but are recommended to rule out abnormalities associated with other conditions such as stress fractures and tumors. A three-phase bone scan is warranted to rule out stress fractures if a conservative treatment program does not alleviate pain. This type of bone scan is a valuable diagnostic tool used to differentiate between MTSS and stress fractures, because each condition has a distinct scintigraphic pattern. A bone scan demonstrating a longitudinal and diffuse pattern in the distal one-third of the tibia is indicative of MTSS ( Fig. 23.2 ). In general, only delayed images are positive in cases of MTSS, whereas both early and delayed images demonstrate uptake in cases of stress fracture. In addition, magnetic resonance imaging (MRI) is another diagnostic tool for MTSS. MRI will show periosteal reaction and bony edema with a sensitivity of 78%–89% and specificity of 33%–100%.
The recommended management of MTSS is multimodal, consisting of rest, nonsteroidal antiinflammatory drugs (NSAIDs), and ice. Physical therapy modalities such as iontophoresis and ultrasound also may be used. Initially, rest or a decrease in training for 2 to 3 weeks is suggested and may be curative without further workup. Cardiovascular conditioning may be maintained during this period with swimming, upper body weightlifting, and deep-water running. Stationary biking is another option but should be performed with the heel on the pedal, a precaution that will diminish muscular stress transmission to the leg. NSAIDs often are prescribed to relieve pain and to decrease possible inflammation. Ice may be used to further reduce swelling and inflammation. Addressing biomechanical abnormalities is also recommended. For example, excessive pronation may be corrected with the use of custom or off-the-shelf orthotics. Physical therapy modalities including massage, electrical stimulation, iontophoresis, ultrasound, and kinesio taping have also been used. A combination a home training program with extra-corporeal shock wave therapy has also been shown to be more effective than a home training program alone. If pain is present with walking or at rest, range-of-motion boots and/or walkers are used. In rare cases, crutches may be necessary.
If the patient has not experienced pain during conservative treatment, a gradual return to training may be initiated. Warm-up and cool-down routines, including stretching, are advised with each workout to prevent recurrence of symptoms. If the patient remains asymptomatic, progression of training is recommended at increments of 10% to 25% for 3 to 6 weeks. If symptoms return, activity should cease for at least 2 weeks before training is resumed at a lower intensity and duration.
Fasciotomies of the posterior compartments of the tibia are possible treatment options in patients with intractable MTSS. In these rare cases, fasciotomies may alleviate the pull of the soleus and deep compartment muscles on the corresponding fascial insertions. However, conservative management alone has been successful in treating MTSS cases, eliminating the need for surgical intervention.
MTSS pain actually may subside during workout but will recur following cessation of activity. Conversely, pain associated with chronic ECS and PAES does not subside during activity and tends to remain until activity is completed.
Pain is localized to the distal one third of the tibia in MTSS but is usually more proximal in the typical stress fracture.
Repetitive loading caused by overuse or overloading of the lower leg results in microtrauma to the bone that eventually may lead to stress fracture. Stress fractures of the tibia are more frequent and more problematic to treat than those of the fibula. Fibula stress fractures tend to heal more rapidly and generally do not require adjunctive therapy. Therefore, this section will focus on tibial stress fractures.
Athletes are particularly prone to stress fractures of the leg, and specific stress fractures are related to certain types of activities. For example, the more common posteromedial stress fracture usually is associated with running activities. Conversely, midanterior tibial cortex stress fractures often are associated with dancers and athletes involved in cutting and jumping activities.
Risk factors for developing a stress fracture include excessive training, training errors, biomechanical variants, and menstrual irregularities with corresponding changes in bone density. Excessive training, particularly common early in the athlete’s season, causes overuse or overloading, which may result in stress fracture. In addition, overlapping of sport seasons, which often occurs when teenage athletes participate in multiple sports, also may lead to an overuse scenario. Training errors, including changes in training surface, shoewear, and technique, often result in overloading, which may result in stress fracture. Weather and seasonal differences affect surface conditions for many outdoor sport activities and may increase the risk of stress fracture. For example, dry conditions and the fall season are both associated with hard ground surfaces, which result in an overloading environment for soccer players. Simple measures, such as watering soccer fields when the ground is hard, may reduce the risk of stress fracture and other injuries by minimizing loading conditions. Biomechanical factors, such as cavus feet, leg-length inequality, and muscular imbalance, also may increase the risk of developing a stress fracture. Finally, the female athletic triad of amenorhea, disordered eating, and low bone mineral density have been associated with an increased incidence of stress fractures.
The cause of stress fractures is multifactorial in nature and often results from an imbalance of natural bone formation and resorption cycle because of repetitive loading. One theory proposed to explain the mechanism of stress fracture suggests that muscle fatigue results in the transmission of excessive forces to the underlying bone, ultimately leading to stress fracture. Another hypothesis asserts that simple, repetitive weight bearing leads to a concentrated rhythmic muscle action, which causes excessive transmission of forces beyond the threshold of bone, thereby resulting in fracture. Forces from large posterior muscle groups, in particular, may cause increased tension on the anterior cortex of the tibia, possibly leading to the problematic midanterior tibial stress fracture.
Pain associated with tibial stress fractures is typically more proximal than that caused by MTSS ( Case Study 23.2 ). Although pain is normally localized to the fracture site, diffuse pain also may occur. Stress fracture pain will develop gradually, occurring initially as a mild ache following a specific amount of exercise and then subsiding. As the condition progresses, pain may become severe and occur during earlier stages of exercise and after cessation of activity. In rare cases, night pain also is possible. Any complaints of constitutional symptoms, including fever and fatigue, should raise concern of a possible tumor or infectious process.
A 16-year-old female soccer player related a 3-week history of anterior tibial pain localized approximately 7 cm below the tibial tubercle. Initially, pain was mild and occurred only with prolonged training. When the patient continued her training intensity, the pain progressed to the point at which training became difficult and persisted with daily activities; however, the patient did not seek treatment at this time. Before her final game, the patient stated that her pain was so severe she was unsure whether she should/could continue to play. Despite constant pain, the patient competed in the final game and experienced a noncontact tibial fracture while running.
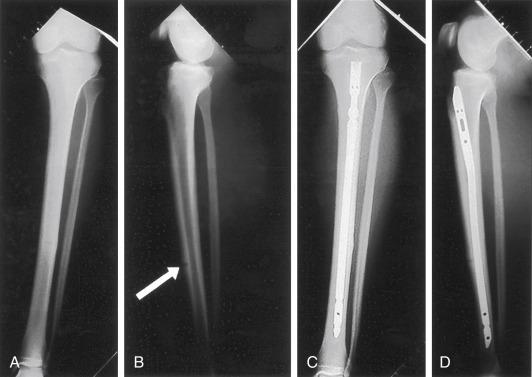
Roentgenograms confirmed the presence of a tibial fracture with an intact fibular that was located at the anterior tibial cortex approximately 7 cm below the tibial tubercle, corresponding to the site of a presumed existing stress fracture. Conservative treatment was recommended and involved long-leg casting for 3 months. Because of minimal bone healing, determined by radiographic evaluation, long-leg casting continued and pulsed electromagnetic stimulation was added for 1 month. Following the use of the long-leg cast, a long-leg fracture brace was used with continued pulsed electromagnetic stimulation.
After 6 months of conservative treatment, aching continued at the fracture site on weight-bearing ambulation. Subsequent plain radiographs and computed tomography (CT) scan indicated small areas of spot weld healing but a largely inadequate bridging callus. Consequently, operative treatment involving reamed intermedullary nailing of the tibia without fibular osteotomy was performed. Approximately 4 months following surgery the fracture was completely healed, and by 8 months postsurgery the patient returned to playing soccer.
In addition to obtaining a history of pain and symptoms, training and activity also should be investigated to identify possible errors that may increase the risk of stress fracture. Recent changes in activity level, such as increased quantity or intensity of training, modifications in training surface, shoewear alterations, and technique should be noted. Inquiries regarding diet also should be conducted because the presence of eating disorders increases the risk for stress fracture. Furthermore, obtaining menstrual histories of female athletes also is pertinent because oligomenorrhea and delayed menarche both increase the risk of stress fracture. Finally, a review of systems is suggested to assess general health, medications, and personal habits to identify any additional factors possibly influencing bone health.
On gross physical examination, the leg will appear normal. Compartments should be soft and the posteromedial aspect of the middle to distal one-third of the tibia should not be tender. Joint range of motion usually is normal, but gait analysis may reveal biomechanical risk factors. Neurovascular examination typically is normal in the absence of any associated abnormalities. Palpation will reveal tenderness localized to the fracture site. In addition, erythema or localized swelling also may be noted. An ultrasound or a tuning fork will produce vibratory pain over the site of the stress fracture. Hopping on one foot may also reproduce pain. In long-standing fractures, a palpable bony thickening may be present.
A clinical diagnosis of stress fracture often may be made solely on the basis of the history and physical examination, but diagnostic imaging may confirm the diagnosis or assist in identifying the stress fracture in questionable cases. Plain radiographs should be performed as the first imaging step but may be negative, because radiographic abnormalities often are not observed until 2 to 3 weeks after the onset of symptoms and may not appear at all if activity modification has been performed. Radiographic abnormalities may appear as a faint periosteal reaction, a fluffy area of callus, or a cortical lucency. If radiographic examination demonstrates the presence of a stress fracture, no further imaging is necessary.
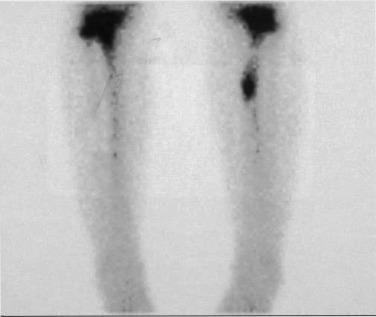
A three-phase bone scan is indicated when suspicion of stress fracture remains despite negative radiographs. The specific scintigraphic pattern of a stress fracture demonstrates focal uptake in the area of fracture ( Fig. 23.3 ). MRI, another diagnostic option, differentiates among fracture, tumor, and infection and also localizes the pathology. An MRI also is useful in differentiating between longitudinal stress fractures and MTSS, the more commonly observed overuse injury, because bone scans of these conditions demonstrate identical diffuse uptake in the distal one third of the tibia ( Case Study 23.3 ).
A 47-year-old woman who regularly walks for cardiovascular fitness presented with complaints of left lower leg pain. The patient described a “deep-aching” pain in the lower one-third of her leg. Over the past 3 months, pain increased with continuation of the patient’s walking program and began to occur at night, eventually resulting in limitation of activity. Her medical history was significant for osteoporosis and systemic lupus erythematosus, which was treated with multiple medications.
Neurovascular and physical examinations were grossly normal. No swelling was observed, but palpation revealed mild tenderness along the distal tibia. Plain radiographs did not reveal the presence of a fracture or periosteal reaction. An MRI was ordered to differentiate between the suspected longitudinal stress fracture and possible MTSS and subsequently demonstrated a longitudinal stress fracture in the tibial metaphysis with surrounding bone edema ( Fig. 23.5 ). Conservative treatment involving a range-of-motion boot and nonweight-bearing ambulation was recommended. Six weeks following treatment, plain radiographs demonstrated a slight callus formation, indicative of the healing process. As a result, the patient was instructed to progress from partial to full weight-bearing ambulation over a 4-week period. Full weight-bearing ambulation in a range-of-motion boot continued for an additional 4 weeks, with subsequent introduction of a regular shoe. At 4½ months, the patient resumed her walking program with a gradual increase in mileage.

In addition to its diagnostic capabilities, imaging also assists in differentiating among the various types of stress fractures. For example, radiographs depicting a small lucency or a “dreaded black line” in the midanterior cortex of the tibia are indicative of a midanterior cortex tibial stress fracture ( Fig. 23.4, A ). Because of the relatively avascular nature of this portion of the tibia, a bone scan initially may be interpreted as negative, but closer examination will depict an area of decreased uptake at the fracture site. If this type of fracture is not initially diagnosed and treated, a complete fracture may result. Conversely, plain radiographs of longitudinal tibial stress fractures often are normal, whereas bone scans will demonstrate increased uptake in the lower tibia.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here