Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Child abuse and neglect constitute a pediatric public health problem of enormous magnitude. Their contribution to morbidity and mortality throughout life has been shown to be much greater than had previously been realized. More than a million children are abused every year in the United States; approximately 140,000 incur serious injuries and nearly 20,000 are left with permanent physical disabilities, such as cerebral palsy and blindness. The estimated to cost the system is over 2 trillion dollars annually. The toll on emotional development is much more significant, with research showing long-term detrimental effects of adverse childhood experiences on health outcomes, quality of life, and life span.
Although there has been a decline in substantiated cases of physical and sexual abuse, mortality rates have not changed significantly. Improved recognition and health care have resulted in a much larger percentage of children being saved. Caffey in the late 1940s and then Kempe and co-workers in the early 1960s fostered a marked increase in the recognition of the physical manifestations of abuse. Subsequent passage of legislation in all 50 states mandating that suspected cases be reported to the proper authorities increased the incidence of reporting. Also, societal standards have changed; some of what is currently regarded as abuse was once sanctioned as discipline.
Five major forms of abuse have been described: (1) physical abuse, (2) sexual abuse, (3) physical neglect, (4) emotional abuse, and (5) medical child abuse. Not infrequently, a child is the victim of more than one form with some degree of emotional abuse associated with all forms. For purposes of reporting to child protection authorities, under child protection laws, the abuse or neglect generally must result from the acts or omissions of a parent, guardian, custodian, or other caretaker of the child, although a child can be abused by non-caretakers. There are often significant differences with requirements for law enforcement reporting, depending on jurisdiction.
Of reported cases about 60% involved neglect, 19% physical abuse, 9% sexual abuse, and 5% were identified as emotionally maltreated, although these figures may vary widely by jurisdiction depending on state laws. These figures may significantly underestimate the actual number, because it is estimated that for every case reported, many go unreported. Clearly, some, perhaps many, reports concerning truly abused children are inaccurately determined to be unfounded. Sometimes this is because of regulations; for example in some states if a perpetrator cannot be clearly identified, or if the identified perpetrator is not a household member despite the fact that the child has clearly been the victim of abuse, the report may be unfounded. Misleading/deceptive histories, limited investigative resources, lack of witnesses, inability or unwillingness of victims and family members to attest to the fact that abuse has occurred, and jurisdictional regulations all contribute to this phenomenon.
Fatality statistics have also been found to have limited accuracy. The National Child Abuse and Neglect Data System (NCANDS) estimates that there were about 1720 deaths in 2017, an increase from approximately 1500 cases in 2003, which is likely due to improvements in the reporting and investigation of child fatalities. This probably reflects improved recognition of child abuse–related deaths as a result of the institution of child death review teams in most states. This does not count the numerous “near fatal” cases. Of fatal victims, 40% to 50% are younger than 1 year old, and 85% to 90% are 5 years old or younger. Researchers looking at data from additional sources have determined that many, perhaps the majority, of deaths due to abuse are misclassified as due to accident, sudden unexplained infant death (SUID), or natural or unknown causes. Reasons for misclassification include incomplete medical evaluation, delay in or inadequate death scene investigation, or no scene investigation, insufficient training of coroners and pathologists about child abuse and the techniques and studies necessary to identify abuse at autopsy, failure to require manner and cause of death on death certificates, and poor communication among investigative agencies. Thus, most authorities believe 2000 deaths per year is a more accurate figure, although this, too, may be a significant underestimate. The number of deaths due to abuse of children younger than 5 years old is greater than the number due to motor vehicle accidents and fires combined and is more than twice the number of deaths due to accidental choking or suffocation, drowning, and falls combined.
The most common causes of death due to abuse are head trauma, abdominal trauma, and suffocation. Of these, intentional suffocation is most likely to go undetected, because autopsy findings may simulate SUID. It now appears that a large percentage of cases of SUID are actually due to accidental suffocation as a result of unsafe sleep. The Safe to Sleep campaign, which was begun by the National Institute of Child Health and Human Development, and efforts to educate parents about the risks of co-sleeping have reduced the incidence of these tragic deaths. Further review of co-sleeping deaths points to a disturbing number of cases in which the adult sleeping with the child has a history of substance misuse.
All sudden unexpected deaths in infancy warrant thorough investigation to facilitate accurate determination of cause, assess for possible foul play, and aid in future prevention. Certain historical points and physical findings may aid in distinguishing SUID from intentional suffocation. Infants dying of SUID are usually younger than 6 months old, previously well, or have only mild symptoms of an upper respiratory infection. Indicators pointing to potential abuse are subtle bruises or petechiae of the face and/or neck, a history of a recent hospitalization for an unexplained illness or for apnea, seizure-like activity, or a brief, resolved unexplained event (BRUE; formerly called apparent life-threatening event [ALTE] ) for which no cause could be found despite an extensive medical workup. This or a past history of multiple BRUEs and/or a history of prior sibling deaths attributed to SUID should raise strong suspicion of intentional smothering.
Child abuse is a phenomenon found in all socioeconomic, cultural, racial, ethnic, and religious subsets of society. The reported incidence per capita is greatest in lower socioeconomic groups. This stems in part from the numerous chronic stressors of living in poverty. It is also clear that well-educated parents of higher socioeconomic status can be abusive; however, when they are, they are less likely to be suspected or even when suspected, reported to authorities. This is in part because they “come across well,” because they tend to be well dressed, well spoken, more sophisticated, and are more confident in their interactions with physicians and others in authority. They are often better able to fabricate a plausible history of how the injury occurred “accidentally.” When reported, they are more likely to have the resources to have the case dismissed, or to be acquitted of the charges. It is very important not to rush to judgment of parents on the basis of appearance, dress, and level of sophistication. Young nonminority children evaluated for repeated injury and not reported are more likely to die from abuse .
The most valuable information is gained by a nonjudgmental approach, keeping an open mind in obtaining a thorough history, making careful behavioral and interactional observations, performing a meticulous examination, and ordering a well-considered laboratory and imaging evaluation before arriving at a diagnosis.
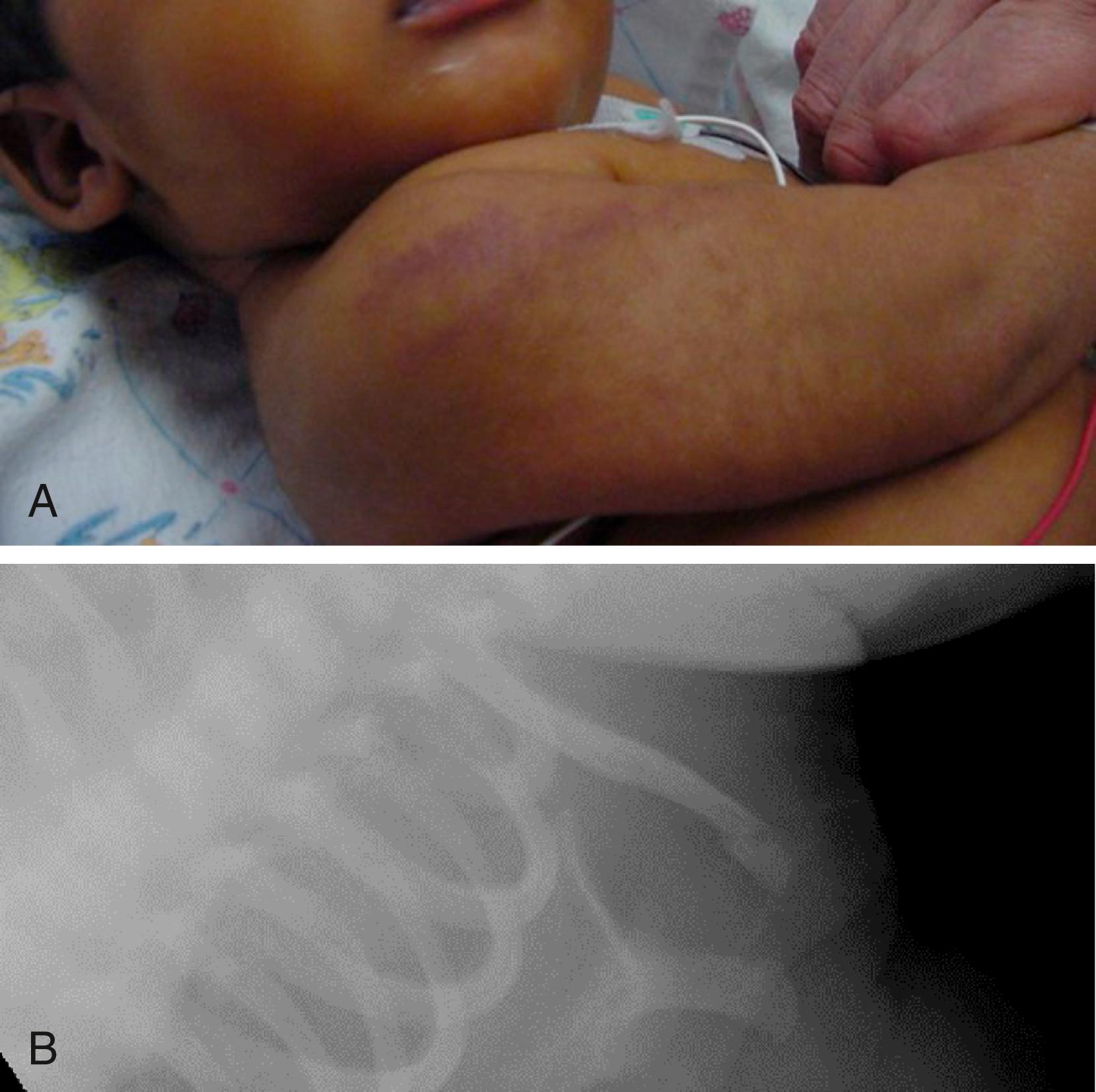
Many studies have shown that the siblings (contacts) of abused children (index children) are at much higher risk of being the victims of abuse themselves. It is now understood that violence in a household is typically widespread, and less likely to involve just one targeted or “scapegoat” child ( Fig. 6.31A and B ).
The caretaker risk factors for child abuse and neglect are:
Emotional and social isolation: Parents who are inadequately nurtured themselves as children are poorly equipped to adequately nurture their offspring.
Substance abuse
Certain mental illnesses
Domestic violence in the parental relationship
Being subjected to a sudden spate of major life stresses/crises, such as loss of job and financial security; loss of home; loss of parent, spouse, or sibling
The child risk factors for child abuse and neglect are:
Age younger than 3 years old
Being separated at birth from a parent at high risk for problems with attachment because of illness or prematurity, resulting in impaired bonding
Being small for gestational age, born with congenital anomalies, and/or having a chronic illness
Being perceived as difficult or different
Having attention-deficit/hyperactivity disorder (ADHD) or being oppositional or defiant
Foster children, unrelated children
Leaving a young infant in the care of a nonbiologically related male, often the mother’s boyfriend, has been shown to be a high risk factor for serious abuse.
One common thread connecting all of these risk factors appears to be one of unmet expectations, due to either unrealistic parental expectations of the child or the child’s inability to meet realistic expectations as the result of developmental delay, illness, temperament, hyperactivity, or inconsistent disciplining. This often stems from lack of caretaker understanding of normal child behavior and emotional development. The combination can then lead the parent or caretaker to attribute malicious intent to an infant who will not stop crying or to a toddler who has had a toilet training accident, is stubborn, or misbehaves. Once “malicious intent” is suspected, this can incite rage in someone with a short fuse.
With this background information, the approach to diagnosis of the major forms of abuse can now be addressed more specifically.
Physical abuse is defined as the infliction of bodily injury that causes significant or severe pain, leaves physical evidence, impairs physical functioning, or significantly jeopardizes the child’s safety. Individual states have varying definitions of abuse that require a report to Child Protective Services (CPS) and law enforcement agencies. Clinicians should become familiar with the statutes in their own states.
The severity of injuries caused by physical abuse ranges from isolated skin bruising to fatal head and abdominal trauma. It is well documented that physical abuse tends to be repetitive and that the severity of attacks tends to escalate over time; so does, correspondingly, the severity of injuries. Given this, early recognition, reporting, and intervention are essential in prevention of increased morbidity and mortality.
Presenting complaint (history of present illness [HPI]) red flags include:
A lack of history for identified injuries, both acute and noted older injuries.
History incompatible with the type or severity of injury. For example, the distribution of lesions or type of injury does not fit the mechanism reported; the history is consistent with a minor injury (short fall, rolled off couch), but evidence of major trauma is found; or multiple injuries of differing ages are found for which no prior care has been sought or adequate explanation provided.
History of the injury is vague, incomplete, lacks details, or was unwitnessed.
History details change over time. For example, the history provided to the referring primary care physician is different than the history provided to the emergency department physician.
History incompatible with the patient’s developmental stage. For example, a 4-month-old with a transverse femur fracture did not cause this injury by pulling to a stand at the coffee table. The history is incompatible with the sibling’s developmental age. For example, the 3-year-old sibling did not cause rib fractures in a 5-week-old infant by hugging the infant too tightly.
Significant delay between the time of injury and the time of presentation.
The parent or other adults in the home provide conflicting accounts of the injury.
Interactions between parents and the child are strained, hostile, or emotionless regarding severe injury.
Past medical history red flags are:
A history or evidence of repeated “accidents” or injuries (Sometimes these patients are seen at a number of different facilities.)
A history or evidence of multiple fractures or old scars suggestive of prior inflicted injury
Poor compliance with well-child care (e.g., missed visits, immunization delay)
History of ingestions
Parents offer historical data about substantial irritability, crying prior to the event, difficulty with feeding, worsening behaviors, particularly prior to the injury. Parents note that the child is clumsy, always climbing, likes to “be bad,” or is uncontrollable.
Few victims of physical abuse are brought in with a chief complaint of abuse. Most present with a chief complaint of an accidental injury or an unrelated chief complaint, such as a viral urinary tract infection (UTI) or irritability ( Boxes 6.1 and 6.2 ).
Vital signs
General appearance, demeanor
Nutritional status and growth parameters
Complete body surface examination
Palpation of each bone
Full general examination including the following:
Head and scalp, including head circumference in infants
Ears, nose, mouth (all mucosal surfaces), throat, and dentition
Cardiopulmonary examination
Palpation of abdomen and serial reexaminations to assess for evolving signs of intraabdominal injury
Palpation of regional nodes
Genitalia including inspection of urethral, vaginal, and anal orifices
Neurologic examination
Ophthalmologic examination including conjunctivae, sclerae, pupils, anterior chamber, and dilated retinoscopy
Developmental assessment
Note affect in describing the child
Relative lack of concern regarding severity/extent of injury
Negative comments regarding the child’s (especially an infant’s) behavior, appearance, or personality:
“She has a bad temper.”
“She’s mean.”
“He’s fussy, cries all the time.”
“She’s greedy, eats like a pig, and is never satisfied.”
“He likes to irritate me.”
Betrayal of unrealistic expectations:
“She should know better than to cry when I have a headache.”
Start with open-ended questions. Follow up with specific clarifying questions. If two parent figures are present, try to take history from each separately and out of child’s presence. Child should be interviewed alone, if age and condition permit (questions should be non-leading and age appropriate). How were major developmental milestones handled, methods of discipline used, list of caretakers and times, supports systems available, and family stressors?
Information about caregivers should include the duration and quality of relationships, history of their families of origin, including, parental relationships, quality of interaction/nurturing of parents as children, methods of discipline in household of origin, levels of education/employment, history of drug or alcohol abuse, history of psychiatric illness, history of prior Child Protective Service or law enforcement involvement or incarceration, history of childhood physical or sexual abuse.
History about the child should include as appropriate: nightmares/sleep difficulties, recent increased aggression, anxiety, depression, self-esteem, withdrawal, regression, increased activity/anxiety, posttraumatic stress disorder (PTSD) symptoms, change in appetite, self-inflicted injury, decrease in academic performance/school failure, running away, drug or alcohol use, fire setting, animal abuse, or law enforcement involvement.
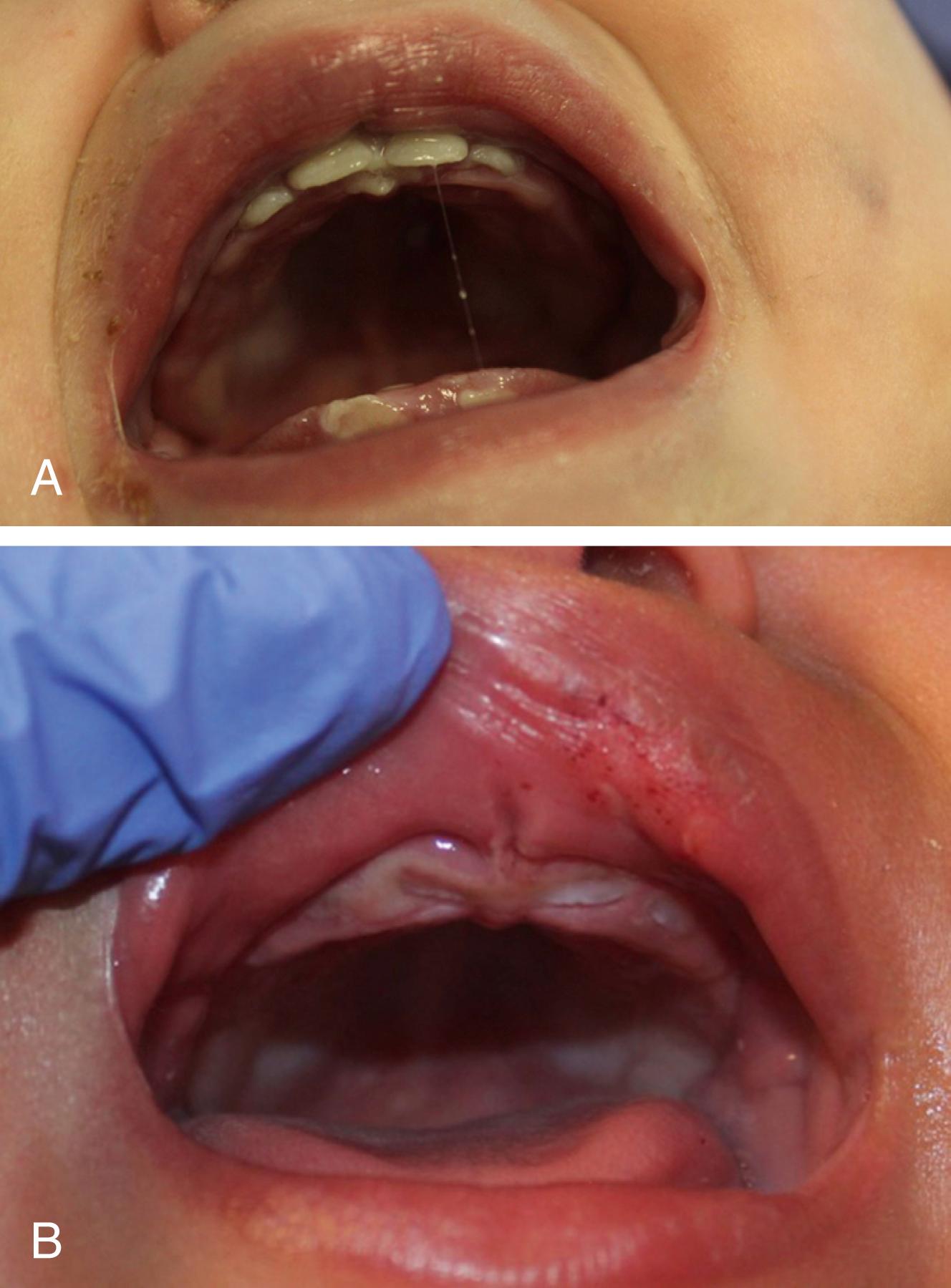
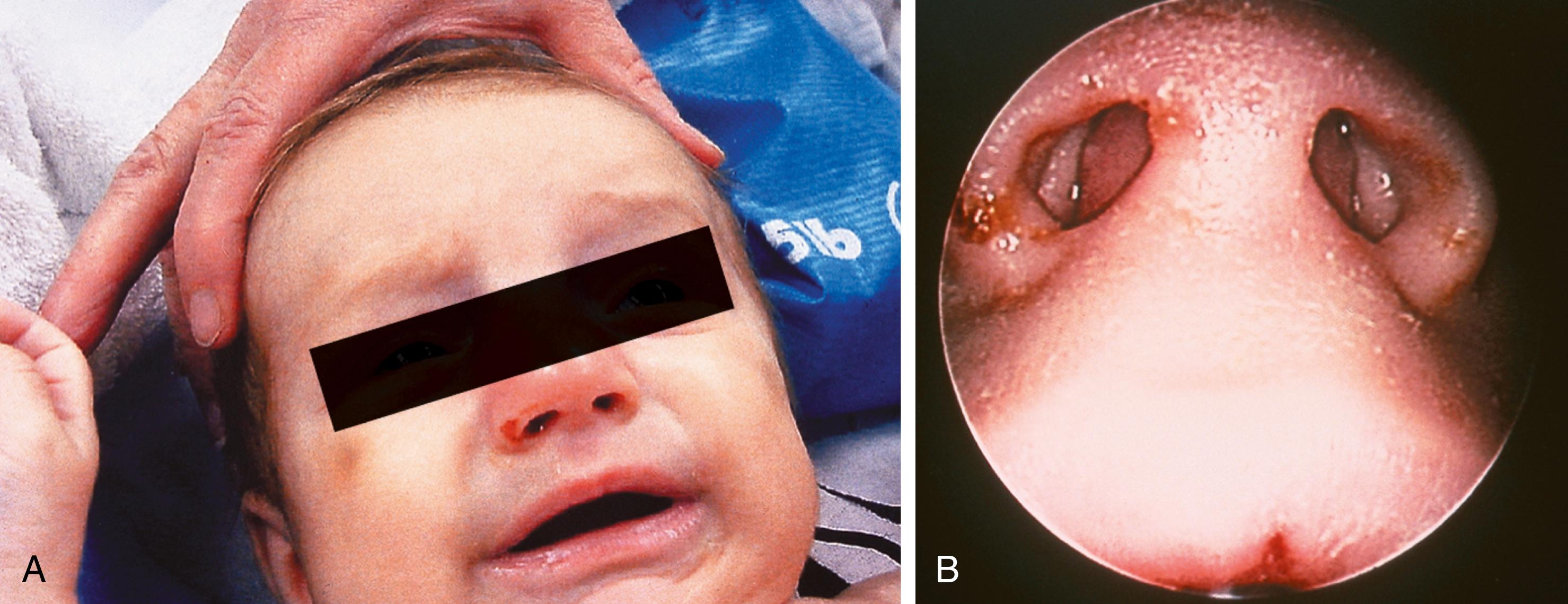
Sentinel injuries are defined as minor injuries that do not require any medical intervention but are often one of the first signs of physical abuse. These include injuries such as bruises, subconjunctival hemorrhages, or blood from the mouth or nose in non-mobile infants. The significance of these injuries is often only recognized in hindsight, after a major injury prompts the evaluation and diagnosis of physical abuse ( Figs. 6.1–6.3 ).


The most common manifestations of physical abuse are those visible on the surface of the skin. This includes bruises, welts, scars, abrasions, lacerations, tourniquet and bite marks, and burns. Bruising is one of the most common and readily visible injuries resulting from physical abuse, but it is often missed as a warning sign. Medical recognition of these warning signs coupled with appropriate action is critical in the prevention of recurrent abusive events. Despite differing opinions on the appropriateness or inappropriateness of physical methods of discipline, there is a general legal guideline distinguishing the boundary between discipline and abuse: Discipline does not inflict significant pain and does not cause physical injury or leave marks. Although corporal punishment is legal in all 50 states, research has proven this method of discipline to be ineffective and detrimental to healthy childhood development. Corporal punishment is associated with increased aggression in preschool and school-age children. It is also associated with an increased risk of mental health disorders and cognition problems. In the landmark 1998 Adverse Childhood Experiences study, the investigators found that spanking was associated with increased odds of suicide attempts, moderate-to-heavy drinking, and substance use disorder in adulthood independent of the risks associated with having experienced physical and emotional abuse as a child. The American Academy of Pediatrics (AAP) recommends that parents, other caregivers and adults interacting with children and adolescents should not use corporal punishment (including hitting and spanking), either in anger or as a punishment for or consequence of misbehavior, nor should they use any disciplinary strategy, including verbal abuse, that causes shame or humiliation.
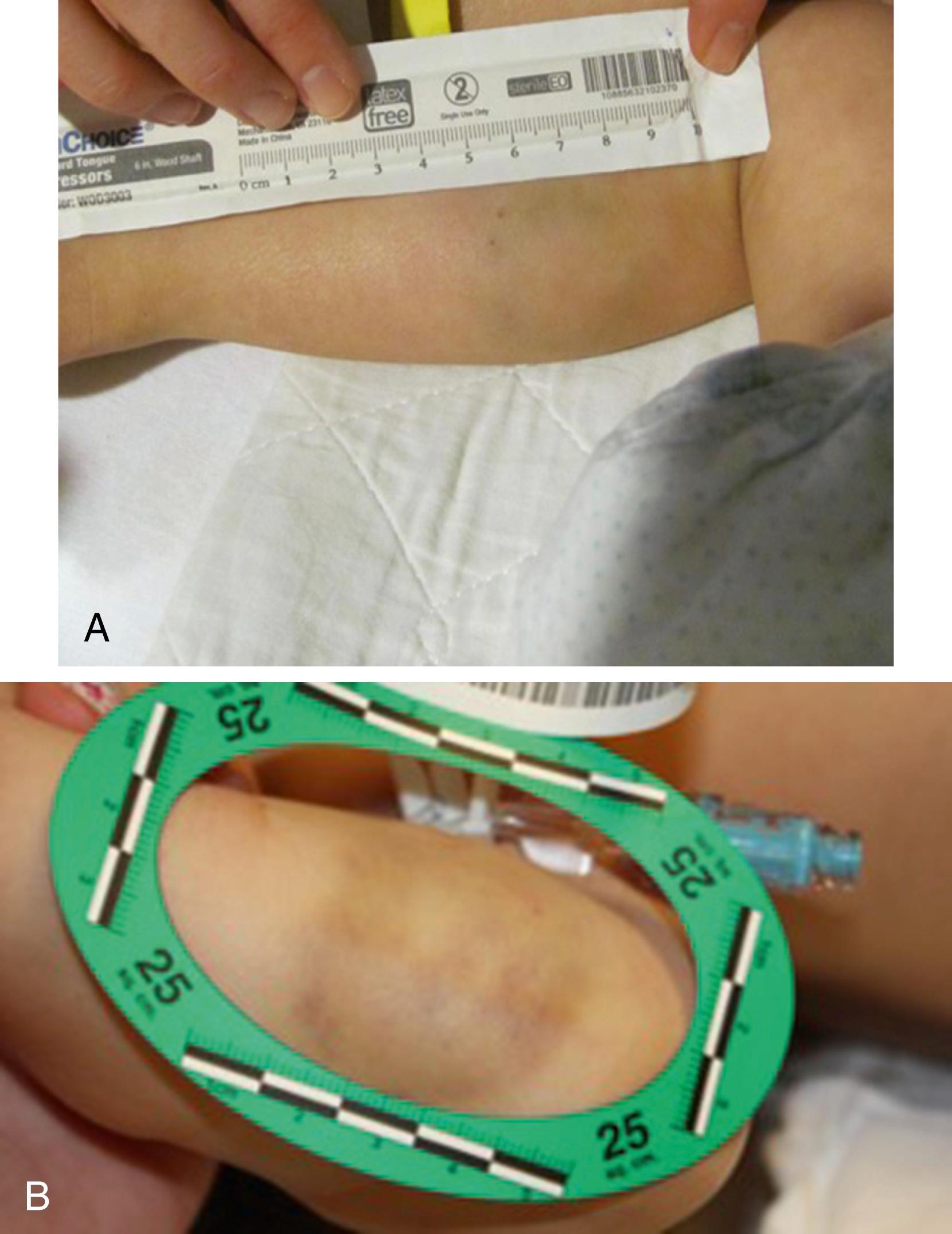
When a clinician has concerns for abusive injury, all external signs of trauma found should be carefully documented and, if possible, photographed with a measuring tool.
A bruise is an injury appearing as an area of discolored skin caused by an impact that ruptures underlying blood vessels. Blood leaks from the broken vessels into surrounding tissues, producing pain, swelling, and tenderness. The discoloration is a result of the blood seepage under the skin. On any day, nearly every ambulatory child has one or more bruises. Many bruises are the result of accidental play. However, it is possible to distinguish which bruises should raise concerns for physical abuse and which bruises are more consistent with accidental events. Bruises are the most common clinical finding in cases of physical abuse; they are seen in up to 75% of victims, and their presence should prompt a search for other, deeper injuries. Many factors can be informative.
It is critical to consider the child’s age and developmental abilities when evaluating bruises. If a child is not yet ambulatory, accidental bruises are exceptionally rare. A young infant is not moving and not generating a force to cause vessel damage/bruising. A 1999 study showed that only 0.6% of children younger than 6 months old have accidental bruises. Children begin to “cruise” shortly after this age, and accidental bruising rises to 19% of cruising infants. Hence, clinicians should remember, “If you do not cruise, you do not bruise.” Any bruise in a non-mobile infant should prompt a clinician to complete a thorough and thoughtful history, physical exam, and further diagnostic testing, as indicated. Bruising increases in toddlers as their motor skills increase.
Many bruises on ambulatory children are accidental. However, studies show that accidental bruises are not numerous at any given time. A 2010 study reported that the average number of bruises on a non-abused child was 1.5, and no child in this group had more than four bruises. In the same study, examining children who had been the victim of abuse, the average number of bruises was six, and the maximum bruises in this subset of the study was 25.
Most bruises in ambulatory children are small. Abusive bruises tend to be larger, with consideration that a hand or an object covered a larger area of skin and vessel rupture, rather than a single stair coming in contact with a shin to cause an accidental bruise. Abusive bruises appear more often in clusters, with consideration of repetitive abusive trauma, rather than a single soccer ball impacting a thigh during a child’s game.
Accidental bruises are most often over bony prominences. The most common sites of accidental bruises include shins, knees, and foreheads. Additionally, bruises directly over spinous processes or the iliac crest often have a clear accidental history.
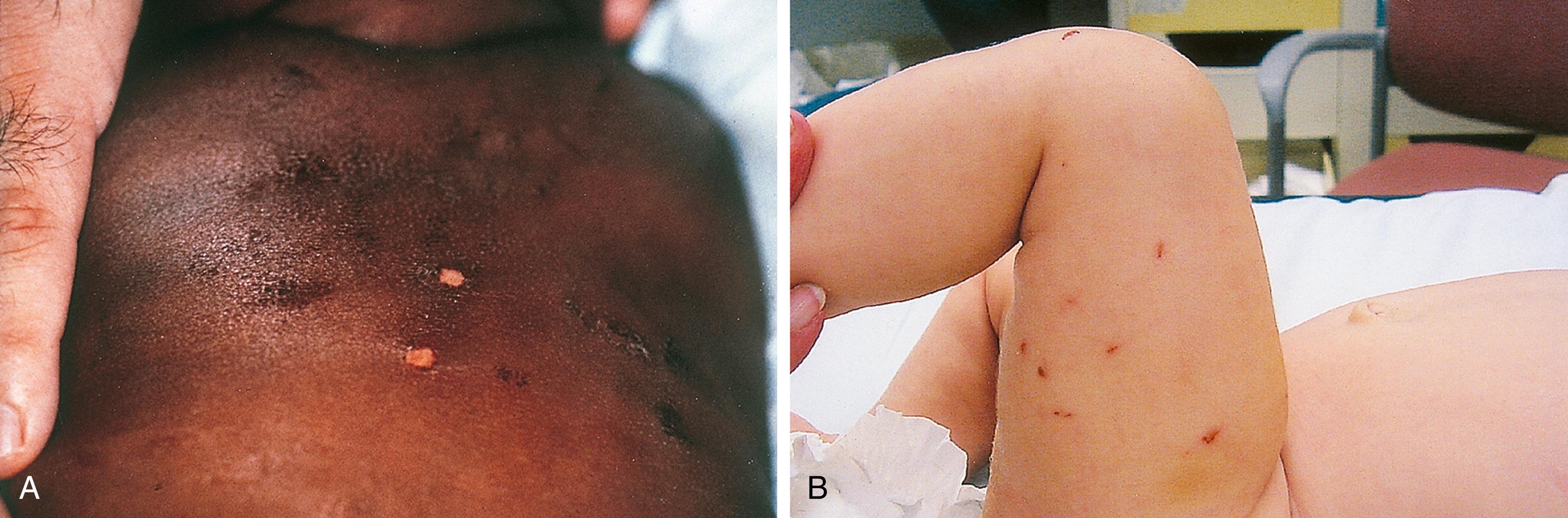
In contrast, abusive bruises are found where common sites of bruising from accidental play are not found. Specifically, bruising over soft areas is concerning for abusive trauma. This includes the torso area, abdomen, genital areas, ears, angle of jaws, neck, buttocks, and soft areas of arms and legs ( Fig. 6.4 ).

Bruises involving the head, face, mouth, neck, and ears are seen in a substantial percentage of physical abuse victims, approximately 50% of infants and 38% of toddlers (see Figs. 6.4 and 6.5 ). Subgaleal hematomas and contusions and petechiae involving the scalp may be the result of direct blows or impacts against a hard surface, or forceful hair pulling ( Fig. 6.6 ). Ear bruises are highly associated with abusive trauma. Bruising can be found in the inner folds of the ear, likely the result of a direct blow, and pinching the ears may result in bruises found on the outer edge and rear side of the helix (see Fig. 6.7 ).



Attempted smothering, choking, or severe and prolonged thoracic compression may produce showers of petechiae over the shoulders, neck, and face ( Fig. 6.8 ). The oral and conjunctival mucosa may be involved as well and should be carefully inspected (see Fig. 6.8E ). When strangulation is the mechanism, neck bruises may be visible (see Fig. 6.8B ). These petechiae may range from florid to faint and may be especially subtle when there has been a delay in seeking care. They can be mistaken for a rash if the examiner fails to check for blanching. Petechiae do not blanche.

Bruises involving the abdominal wall below the rib cage and above or anterior to the pelvic girdle are rarely seen with accidental injury. Of note, abdominal bruising is often absent in abuse directed toward the child’s abdomen because the distribution across substantial soft tissue permits movement of the blood vessels. In fact, many children with inflicted intraabdominal abusive injuries have little or no cutaneous evidence of trauma over the abdomen. When abdominal bruises are present, they are indicative of forceful grabbing or pinching or of forceful blunt impact (such as a punch or kick) ( Fig. 6.4F ). In these cases, abuse should be strongly suspected, and evidence of internal injury should be sought (see the Abdominal and Intrathoracic Injuries section and Fig. 6.59 ).
Bruising in the genital area may include direct trauma to the suprapubic area or genitalia. It may also include pinching of the penis and/or scrotum. These injuries are considered abusive until proven otherwise. This type of trauma can result in bruising and extraordinary swelling. Careful evaluation for scrotal hematomas, which can have serious sequelae if untreated, should be completed.
Bruises are often seen over the curvature of the buttocks and across the lower back after severe spankings, whether with a hand or an object ( Fig. 6.9 ). When linear marks from fingers, belt, or brush edges are seen, these tend to be horizontally or diagonally oriented (see Fig. 6.9B ). In some cases, a linear pattern of petechiae may be noted on either side of the gluteal crease (see Fig. 6.9C ). Despite their vertical orientation, these are also the result of forceful horizontal blows across tightly tensed glutei, as when the blows are delivered, the involved sites are closely apposed along the crease and thus are subject to maximal capillary distortion on impact.

Injuries inflicted with an object will often leave marks that reflect the outline of that object. Patterned injuries do not occur during normal play and should be considered abusive until proven otherwise. In many instances, the surface marks are recognizable imprints of the edge of an implement used, because the edge causes maximal capillary deformation on impact ( Fig. 6.10 ). Those most commonly seen are looped-cord marks, belt and belt-buckle marks, and switch marks, but almost any implement can be used.

Slap marks with an open hand can often leave a pattern consistent with the linear distribution of pressure from fingers (see Fig. 6.5 ). The hand leaves a negative imprint when the capillaries break under the slapping fingers, and the blood is pushed away from the point of contact. Slapping and direct hitting may produce diffuse bruising with petechiae (see Fig. 6.4 ).
Surface injuries involving more than one plane of the head or face are highly suspicious for abuse. An accidental event or “fall” does not typically involve multiple planes of the face and head. It is also important to recognize that contusions of the head, face, and ears are often associated with underlying intracranial injury, especially in infants.
The size, nature, and rate of healing of bruises depend on the amount of force applied; the firmness and shape of the impacting object or surface; and the duration of impact, as well as on the degree of skin thickness, its vascularity and depth, elasticity, and adipose padding of the underlying subcutaneous tissue. Hence, the initial appearance of bruises and the time it takes for them to resolve vary widely. Superficial bruises appear almost immediately and resolve more quickly than deeper contusions. The latter may not discolor the overlying skin for days and may take up to 2 weeks to resolve. Furthermore, the evolution of bruises in terms of color change is also variable. Although red, blue, and purple are more typical of fresh bruises, these colors can persist in some cases until resolution. Yellow, green, and brown are more characteristic of older bruises but can be seen relatively early in superficial bruises. Hence, it is difficult to determine the ages of ecchymotic lesions, but if tenderness, swelling, and/or fresh overlying abrasions are present, these findings are consistent with more recent injury.
In many cases of abuse, surface bruises and petechiae are faint or even imperceptible to the naked eye. Although bruises are relatively easy to see in victims with fair skin, they can be difficult to appreciate in children with darkly pigmented skin unless extra care is taken. This may also be because the bruises are early in their evolution, or it may be the result of fading due to delay in seeking care. Appreciation of the potential subtlety of bruises and petechial lesions may provide the only clinical clue that abuse has occurred and that other abusive injuries may be present.
When bruising is severe, deep, and extensive, underlying muscle breakdown may occur, resulting in myoglobinuria ( Fig. 6.10L ). When severe, this may precipitate renal failure unless the risk is recognized, appropriate tests performed, and aggressive treatment measures are instituted.
To avoid errors in diagnosis, children who present with multiple bruises in unusual locations that are not patterned should be thoroughly examined for evidence of an underlying coagulopathy, and screening coagulation studies should be performed before arriving at a final diagnosis ( Box 6.3 ).
Accidental bruising
Dermal melanosis
Henoch-Schönlein purpura and other vasculitides
Idiopathic thrombocytopenia purpura
Leukemia
Hemophilia
Ink, paint, or dye to the body
Epidermal nevi
Cultural practices of healing:
Cupping
Coining
Popsicle panniculitis
Erythema multiforme
Angioedema
Phytophotodermatitis
Chilblain (pernio)
Epidermolysis bullosa
Impetigo
Ehlers-Danlos syndrome
Trichotillomania
Alopecia areata
Obstetric trauma
Prematurity
Nutritional/metabolic disorders:
Rickets
Scurvy
Copper deficiency/Menkes disease
Renal osteodystrophy/secondary hyperparathyroidism
Hypervitaminosis A
Neoplasm
Physiological periosteal new bone growth
Skeletal dysplasia
Osteogenesis imperfecta (OI)
Bone demineralization
Leukemia or benign bone cysts
Caffey disease
Benign extra-axial fluid (BEAF) of infancy
Glutaric aciduria type 1 (GA1)
Abrasions are also seen in abuse victims, although less commonly than bruises. In some cases, outline bruises of forcefully applied weapons have an overlying abraded or even lacerated surface ( Fig. 6.11 ). Abrasions also may result from friction on impact with a hard surface or from being dragged across a carpet or other rough surface. Fingernails can be dug into the skin, leaving small curvilinear marks.
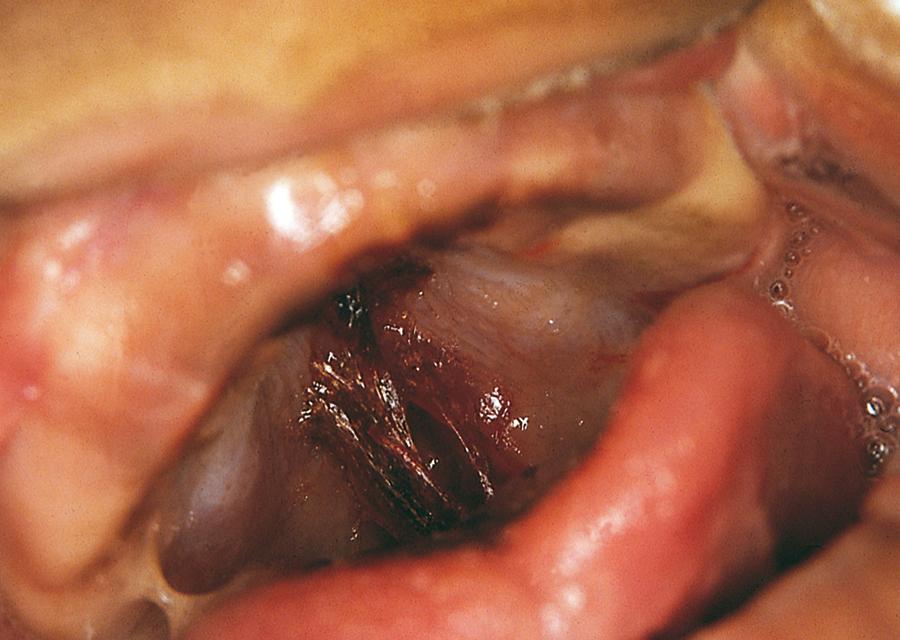
Strangulation and restraint marks result from attempts to hang, choke, or tie the child to a crib, bed, or chair. Abraded or blistered circumferential ligature marks can be seen in these cases ( Fig. 6.12 ).

Bite marks can be another manifestation of physical abuse. Lesions tend to be oval or semicircular. The impressions of the incisal surfaces may be variably clear, depending on the force applied and the age of the bite. Suction petechiae may be noted centrally in some fresh lesions. If the injury is distinct, the size enables the examiner to clearly distinguish between the bite of another child (primary teeth) and an adult bite (secondary teeth). Adult bites with secondary teeth are greater than 3 cm in diameter ( Fig. 6.13 ). Each bite mark should be carefully photographed in its entirety, and then photos should be taken perpendicular to the plane of the imprint of each arch, with a measuring tool in each photo.
Similar to bruises or abrasions, some patterns of burns are highly associated with abusive injury.
Abusive burns are more commonly seen in children under the age of 5. Young children with immersion burns into hot water without any associated splash marks or dip burns in a stocking-glove distribution are very concerning for abusive injury. Burns to the back, buttocks, or genital burns in infants and toddlers are concerning for abusive injury while being bathed. Histories that include an unexpected toileting accident can alert a clinician to concerns for a frustrated caretaker. Deep contact burns with a clear imprint of the hot surface should raise concerns of a thoughtful clinician. When considering abusive injury for a burn, an inconsistent history, an unusual pattern of injury, or delay in seeking medical attention increase concerns. It is important to evaluate for other injuries when a burn is suspicious for abuse or neglect ( Fig. 6.14 ).

Immersion scalds or dip burns are among the most common forms of inflicted burns. Typical patterns include symmetrical burns of hands or feet in a stocking-glove distribution, with a sharp line of demarcation at the level of the water line ( Fig. 6.15A ). Circumferential burns of the feet and lower legs along with burns of the perineum and flexor surfaces of the thighs are seen in children who are dipped in scalding water (see Fig. 6.15B and C ). Sparing of apposed skin surfaces in flexor creases may also be noted in these cases. At the recommended hot water tank setting of 120°F maximum, scalding burns can be prevented ( Table 6.1 ).

| Water Temperature (°F) | Duration of Exposure |
|---|---|
| 120 | 10 min |
| 130 | 30 s |
| 140 | 5 s |
| 150 | 2 s |
| 158 | 1 s |
There are some characteristics of burns that are commonly associated with accidental injuries. Accidental scalds typically occur when a hot liquid is spilled, producing a splash-and-droplet pattern in the case of a small spill ( Fig. 6.16A ) or an inverted arrowhead in cases of larger spills over the chest (see Fig. 6.16B ). The child usually presents with a history of having grabbed a cup of hot coffee, tea, or cocoa from the table while sitting on someone’s lap, or of having reached up and grabbed the projecting handle of a pot on the stove.
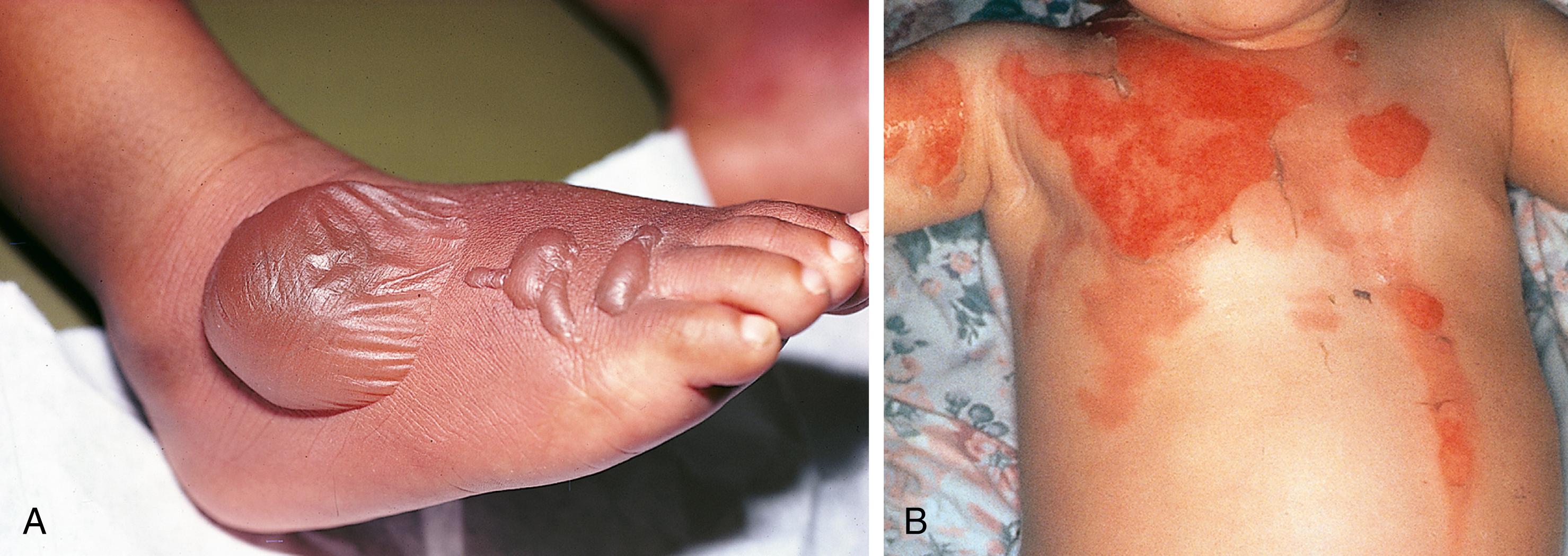
Contact burns show the imprint of the instruments used to inflict them and have a depth or degree of burn that is relatively even throughout. For example, one may see the imprint of a hot iron or of the grill of a space heater or radiator cover ( Fig. 6.17A–D ). No child with normal sensation would remain in contact with these objects long enough to incur such a burn. Burns caused by holding a hot hair dryer next to the skin leave an imprint of the screen that covers the heating element (see Fig. 6.17E ), and those inflicted with a curling iron produce cigar-shaped, deep partial- or full-thickness imprints (see Fig. 6.17F ). Most abusive contact burns are found in unusual locations for accidental burns, such as the extensor surfaces of the upper arms or legs, the back, chest, abdomen, or buttocks that are usually covered by clothing.

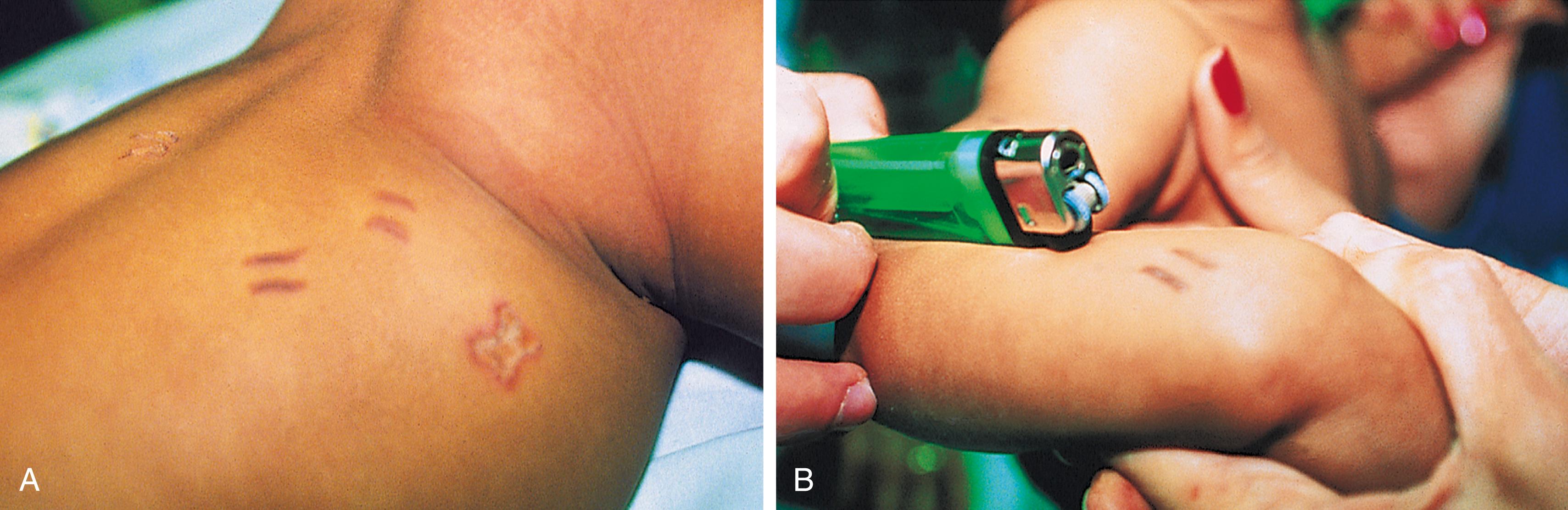
Inflicted cigarette burns usually leave sharply circumscribed, full-thickness imprints approximately 7 to 8 mm in diameter ( Fig. 6.18 ). These are surrounded by a deep, partial-thickness halo blister and then a rim of superficial erythema. A thick, black eschar soon forms over the central, full-thickness burn. Subacutely, these lesions fill in with granulation tissue, and on completion of healing, the child is left with a deep, punched-out scar. Other burning objects, such as a lighter, can create a distinctive pattern of inflicted burns as well. So-called “branding” injuries can also be seen on children ( Fig. 6.19 ).

It is important to examine the nose and mouth of the patient for intraoral injuries. This may include palate trauma or soft tissue lacerations caused by violently forcing a bottle, pacifier, or utensil into a child’s mouth. Additionally, labial frenulum tears, mucosa or gingiva bruising, or contusions to the lips are often the result of violent forceful trauma ( Fig. 6.20 ). Force-feeding with a spoon may produce contusions or lacerations of the lips, floor of the mouth, and tongue ( Fig. 6.21 ). The common complaint at presentation is spitting or vomiting up blood.
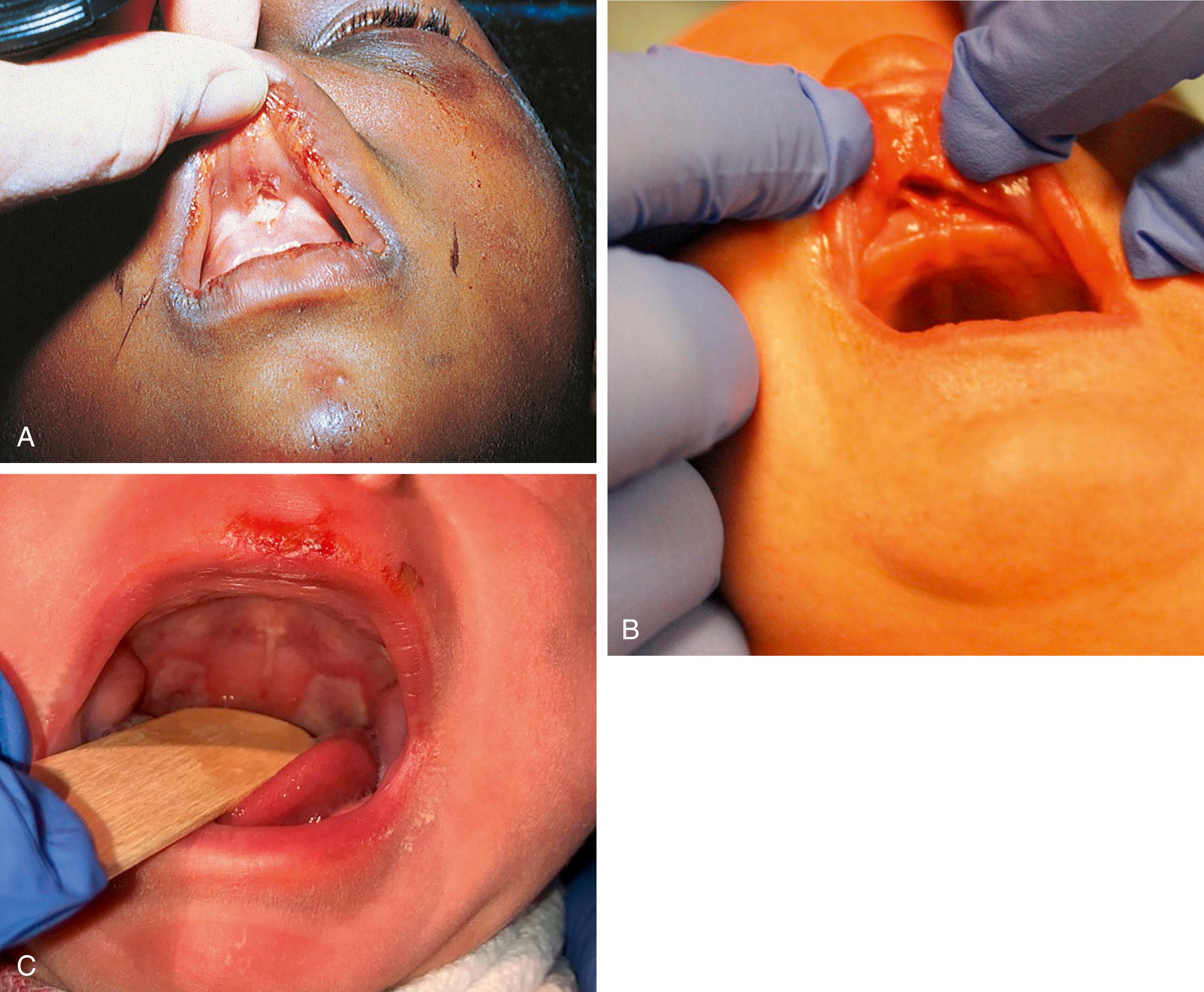
In older children, punches, slaps, or other direct trauma can cause lip lacerations and contusions, frenulum and gingiva tears (see Fig. 6.25 ), dental fractures, displacement injuries and avulsions, chin lacerations, and even mandibular fractures. These injuries can also stem from impact with hard surfaces when the child is violently pushed or thrown. Often these older victims present with a plausible history of accidental trauma and are not recognized as abuse victims. Sometimes the only clue that the injuries are abuse related is that the lesion is more severe than would be expected from the reported mechanism.
Nasal injuries may be due to direct blows or impacts. When mild, epistaxis may be the only manifestation. More severe injuries can result in fractures of the nasal bone or cartilage, septal deviation, and septal hematoma. The abused child with a septal hematoma is especially vulnerable to developing a septal abscess due to delay in presentation, and affected infants tend to present with external nasal swelling, fever, and respiratory distress due to nasal obstruction ( Figs. 6.3 and 6.22 ).
Skeletal injuries are reported in 11% to 55% of child abuse victims. Many fractures are clinically unsuspected. Multiple fractures are found in more than one-half of physically abused children.
The majority of fractures, 55% to 70% of all inflicted skeletal injuries, involve infants younger than 1 year old. Approximately 80% of abusive fractures are seen in children younger than 18 months old. In sharp contrast, this age group accounts for only 2% of all accidental fractures in children. Often, fractures are clinically occult, and diagnosis of inflicted fractures based on physical exam is nearly impossible in infants, because nondisplaced rib fractures, metaphyseal chip fractures, and bucket handle fractures have minimal swelling, even acutely, and heal with great rapidity. It is not possible to evaluate for occult fractures in a young child by palpation. Further, an accurate history of trauma is especially unlikely to be reported. When a history of injury is given, it is often one of a minor mechanism (a short fall). Furthermore, parents of abused children tend to minimize reports of pain, discomfort, and loss of function. Because healing is faster in the infant or young child (due to the thickness of the periosteum, which resists tearing, reducing risk of displacement, and due to its being richly invested with osteoblasts that facilitate healing), tenderness and pain on being picked up, or on motion, may abate within a few days. This is particularly true of rib and metaphyseal fractures and other nondisplaced fractures. Notably, most fractures sustained by healthy children are not associated with bruising at the time or presentation (10%) or within the first week (28%) after trauma.
Many fractures in children are accidental. However, there are some warning signs that should encourage the clinician to consider abusive etiology. Physical abuse must be considered in the following situations:
Infants and children with fractures that are highly associated with physical abuse. These include classic metaphyseal lesions, rib fractures, and sternum, scapula, or vertebral fractures. These fractures are described in more detail in the following sections.
Any fracture with a history that is not compatible with severity of injury
Any fracture in a non-ambulatory child, especially without a clear history or a known medical condition
Children with multiple fractures or a history of multiple fractures
In infancy, the cartilage of the chondro-osseous junctions adjacent to the metaphyses of long bones is poorly mineralized, making these structures the weakest points in long bones. Classic metaphyseal lesions are planar fractures through these sites when the bones are subjected to shearing forces. The periosteum overlying the epiphyseal cartilage is firmly adherent and extends close to the diaphysis to cover the subperiosteal bony collar. Thus, when fractures occur, these peripheral segments are visibly thicker.
Metaphyseal fractures can be produced by the application of torsional or tractional forces delivered when an extremity is grabbed and yanked. They can also occur by rapid, repetitive acceleration and deceleration as the extremities flail back and forth in the process of violent shaking. Metaphyseal fractures can be found in any long bone but are most commonly seen in the distal femur, proximal and distal tibias, and proximal humerus. They may cover the entire metaphysis or only a portion of it. Clinically, they are not associated with any significant soft-tissue swelling.
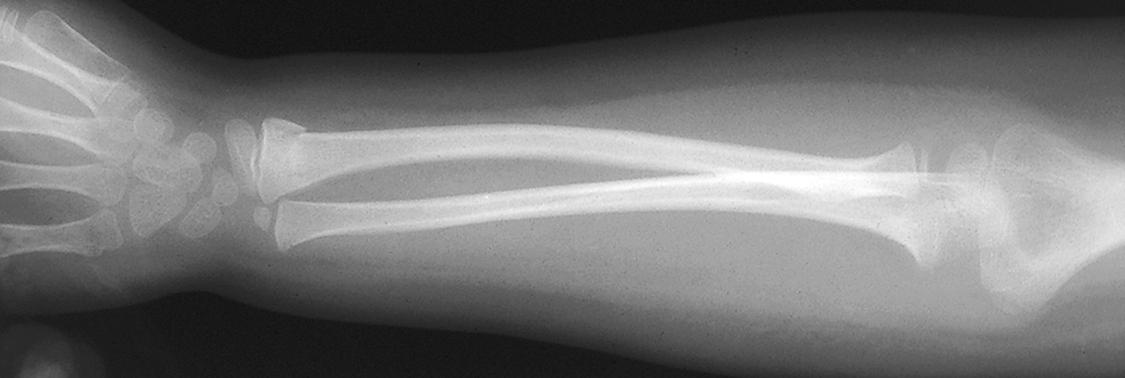
Radiographic manifestations of metaphyseal fractures have led to the terms metaphyseal chip or corner fractures and bucket handle fractures. The first derives from the fact that in the anteroposterior view the central portion of the fracture is often invisible and only a chip of bone is seen on either the lateral or medial aspect of the metaphysis, or both ( Fig. 6.23 ). Chips may also be seen on lateral projections. In some cases, a thin central metaphyseal lucency can be detected. Special oblique views are necessary to reveal the true extent of the fracture, because in this projection the separation of the metaphyseal disk becomes readily evident, resembling a bucket handle. Healing of metaphyseal fractures is not usually accompanied by prominent callus or extensive subperiosteal new bone formation.
![Fig. 6.23, (A) 6-week-old baby admitted with failure to thrive, found to have an upper frenulum tear, lip abrasions, injuries to his soft palate bilaterally, facial bruising, and his drug screen was positive for cocaine. On follow up x-rays, child found to have four healing posterior rib fractures. Additionally, child had gained weight well in a safe environment. (B) 7-week-old sibling of a 3 y/o victim of physical abuse. A skeletal survey revealed bilateral distal tibia bucket handle (classic metaphyseal lesion [CML]/corner) fractures. (C) X-rays 2 weeks later showed healing bilateral distal tibia bucket handle (CML/corner) fractures. (D) 6-month-old infant presented to care due to decreased use of left arm without any history of trauma. Child found to have a left proximal humerus CML, a torn frenulum, and buttock bruising. Fig. 6.23, (A) 6-week-old baby admitted with failure to thrive, found to have an upper frenulum tear, lip abrasions, injuries to his soft palate bilaterally, facial bruising, and his drug screen was positive for cocaine. On follow up x-rays, child found to have four healing posterior rib fractures. Additionally, child had gained weight well in a safe environment. (B) 7-week-old sibling of a 3 y/o victim of physical abuse. A skeletal survey revealed bilateral distal tibia bucket handle (classic metaphyseal lesion [CML]/corner) fractures. (C) X-rays 2 weeks later showed healing bilateral distal tibia bucket handle (CML/corner) fractures. (D) 6-month-old infant presented to care due to decreased use of left arm without any history of trauma. Child found to have a left proximal humerus CML, a torn frenulum, and buttock bruising.](https://storage.googleapis.com/dl.dentistrykey.com/clinical/ChildAbuseandNeglect/22_3s20B9780323777889000067.jpg)
Rib fractures are also relatively unique to abused infants. Because of the plasticity and pliability of the thoracic cage in infancy, application of major forces is required to break ribs, and accidental rib fractures are exceptionally rare. A 2006 systematic review with 923 children (0 to 14 years) who received cardiopulmonary resuscitation (CPR) showed that three children sustained rib fractures, and all cases were anterior fractures. Abusive causative mechanisms include violent shaking or squeezing while holding the infant by the chest. The ribs are subjected to marked anteroposterior compression forces, and the posterior ribs are levered against the fulcrum of the vertebral bodies and their transverse processes. This often produces rows of multiple, posterior rib fractures, located near the costovertebral articulations ( Fig. 6.24 ). Extreme squeezing of the chest with or without shaking can produce fractures at multiple sites along the rib arcs. Most of these infants have no history of trauma and symptoms are nonspecific. Hence, the appropriate imaging is necessary.
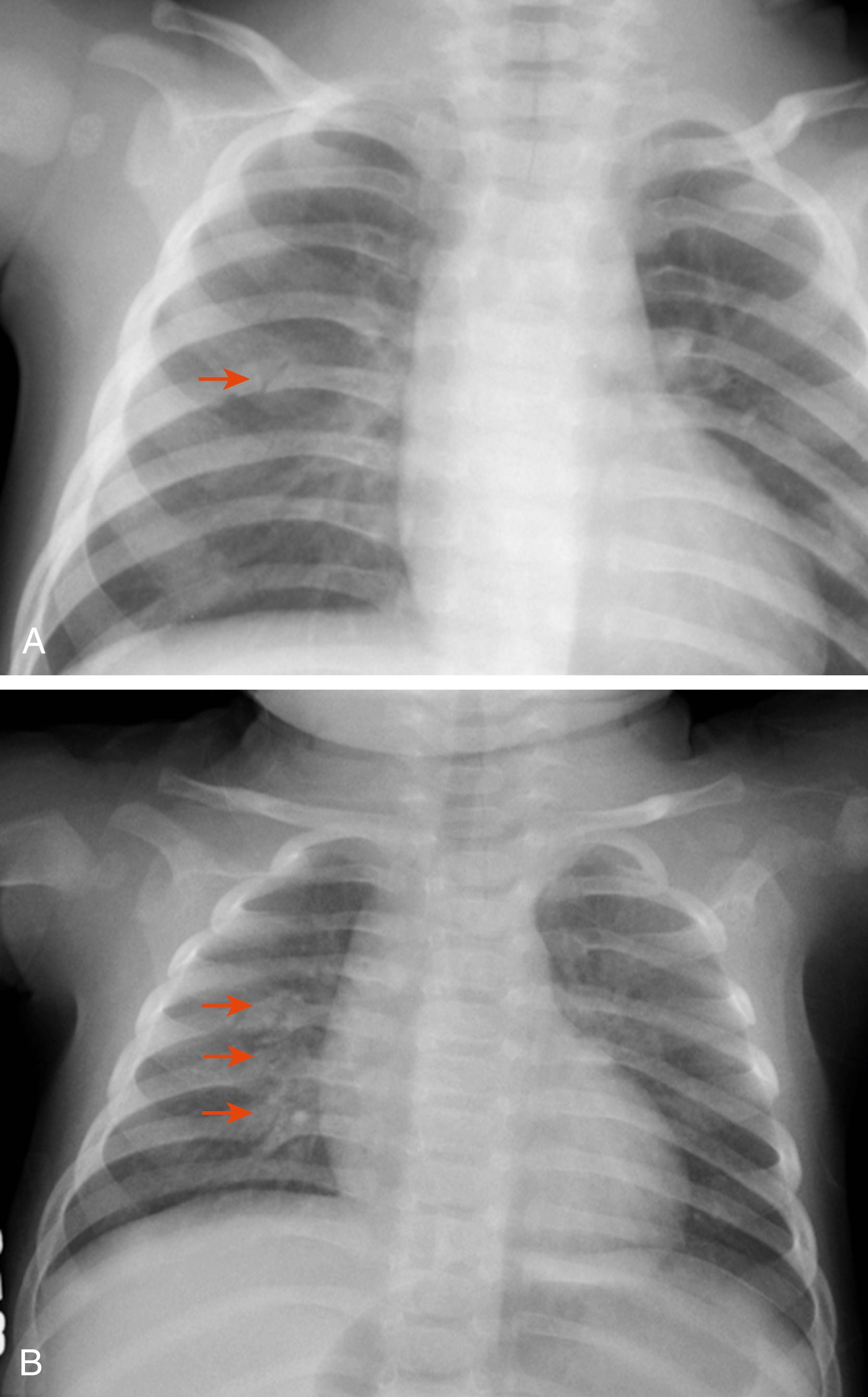
Like metaphyseal fractures, rib fractures are not often associated with soft tissue swelling or bruising. When fractures involve the lower rib cage, associated abdominal injury should be considered ( Fig. 6.25 ).
Radiographically, rib fractures may not be visible before the appearance of callus and/or subperiosteal new bone. It is the standard of care that a repeat skeletal survey is completed 10 to 14 days after the initial x-rays. These follow-up films can reveal fractures not visible on the first study. An early sign of healing, seen 5 to 10 days post injury on standard radiographs, consists of a vertical lucency at the site of the fracture surrounded by soft callus with indistinct margins. Subsequently (at 14 to 21 days), callus takes on a more nodular appearance with sharper margins and is then termed hard callus . Reinjury can result in florid callus formation. Complete remodeling and radiographic disappearance occur within a few months in the absence of reinjury.
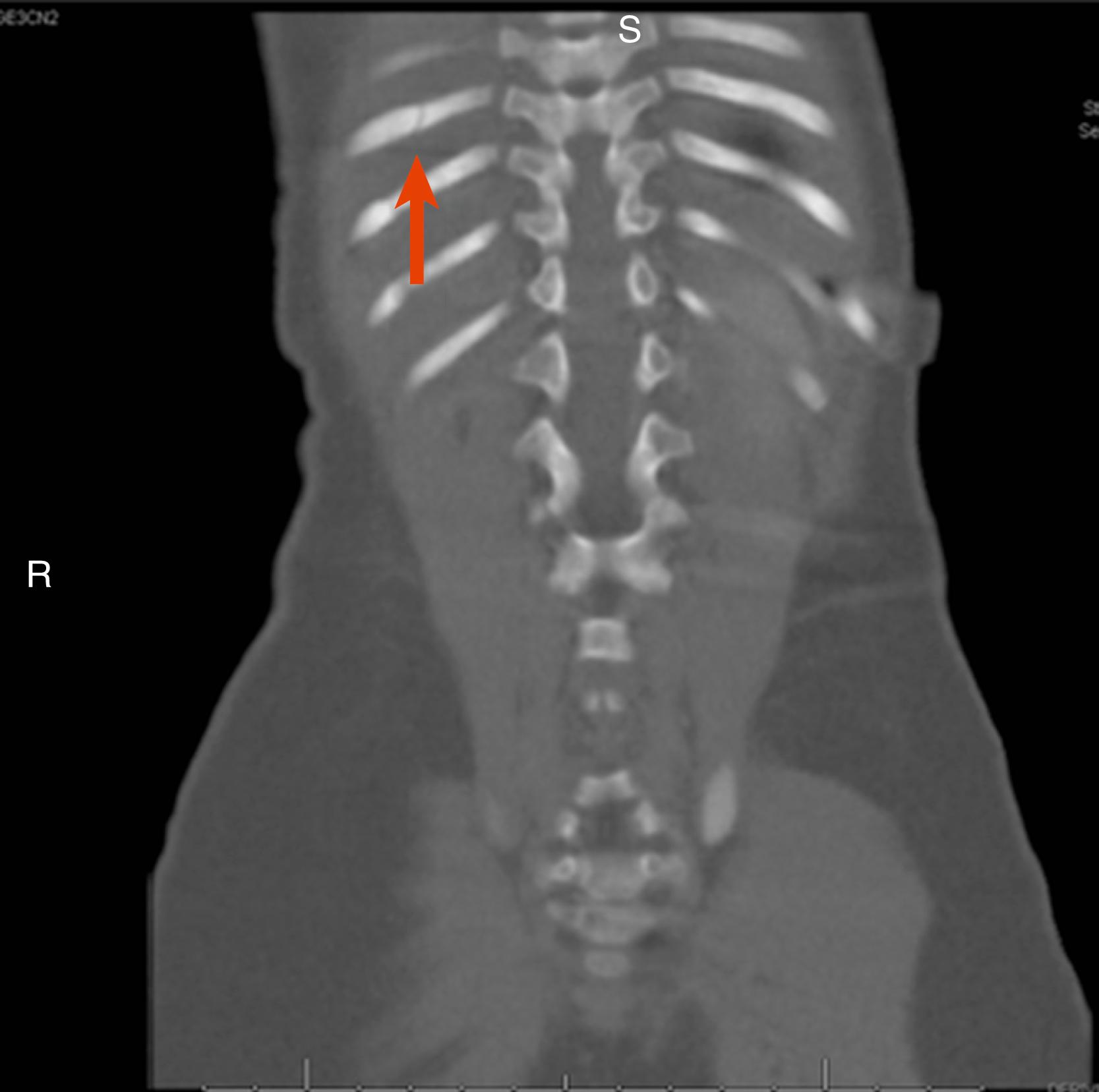
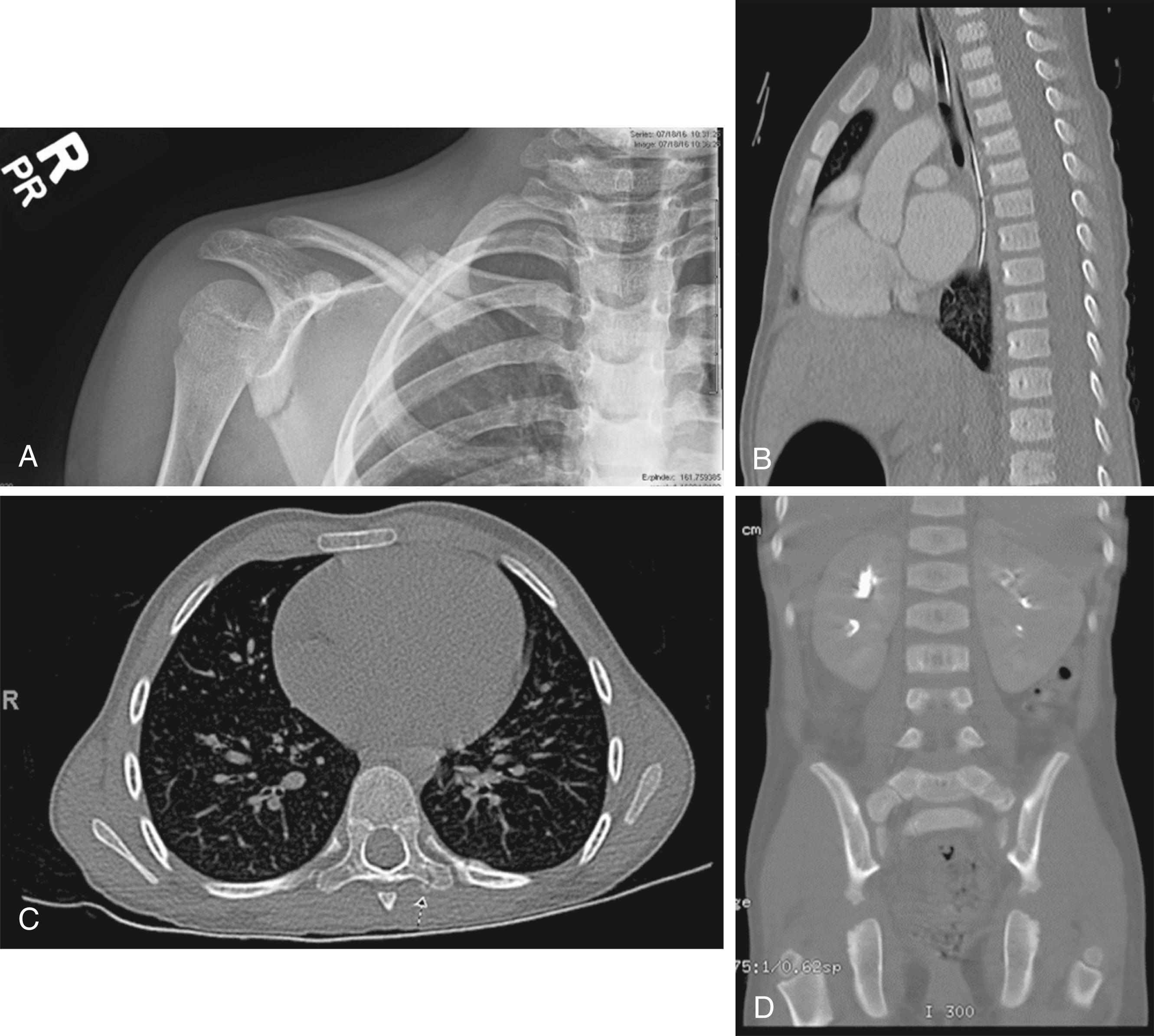
Vertebral fractures, scapula fractures, and sternal fractures are rare. However, each of these fractures is highly specific for physical abuse. Scapular fractures of the acromion probably result from shearing forces during shaking or traction to the upper extremities. Fractures to the body of the scapula or the sternum are the result of very high force blunt trauma. Each of these fractures is unusual but highly associated with inflicted trauma ( Fig. 6.26 ).
Abusive fractures have been described in virtually every bone in the body, and any single fracture can be the result of accident or abuse, particularly when considering the age of the child and the history provided. Below are some fractures in the context of a lack of history or a history that does not fit with the developmental age of the child, which should be very concerning.
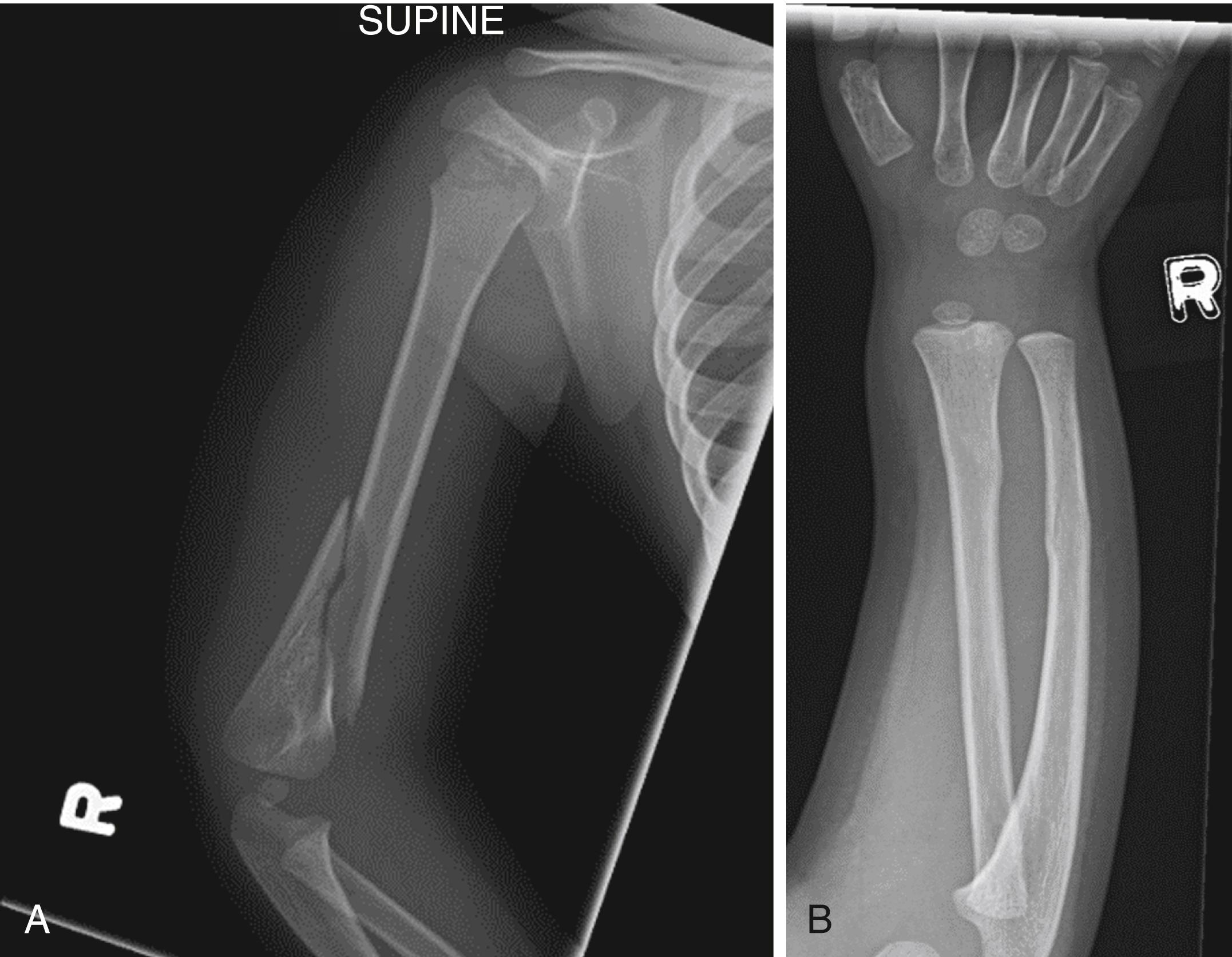
Long bones may fracture through the diaphysis in a variety of patterns. Transverse, oblique, spiral, or compression fractures may all be seen. These fractures take a substantial amount of force. Although not specific for inflicted injury, diaphyseal fractures are highly suspect when found in infants who are not yet crawling or walking, especially when seen in the absence of a history of significant trauma. An understanding of the direction and magnitude of force required to produce a given type of diaphyseal fracture compared to the provided history is important to try to distinguish between accidental and inflicted injury ( Figs. 6.27 and 6.28 ).

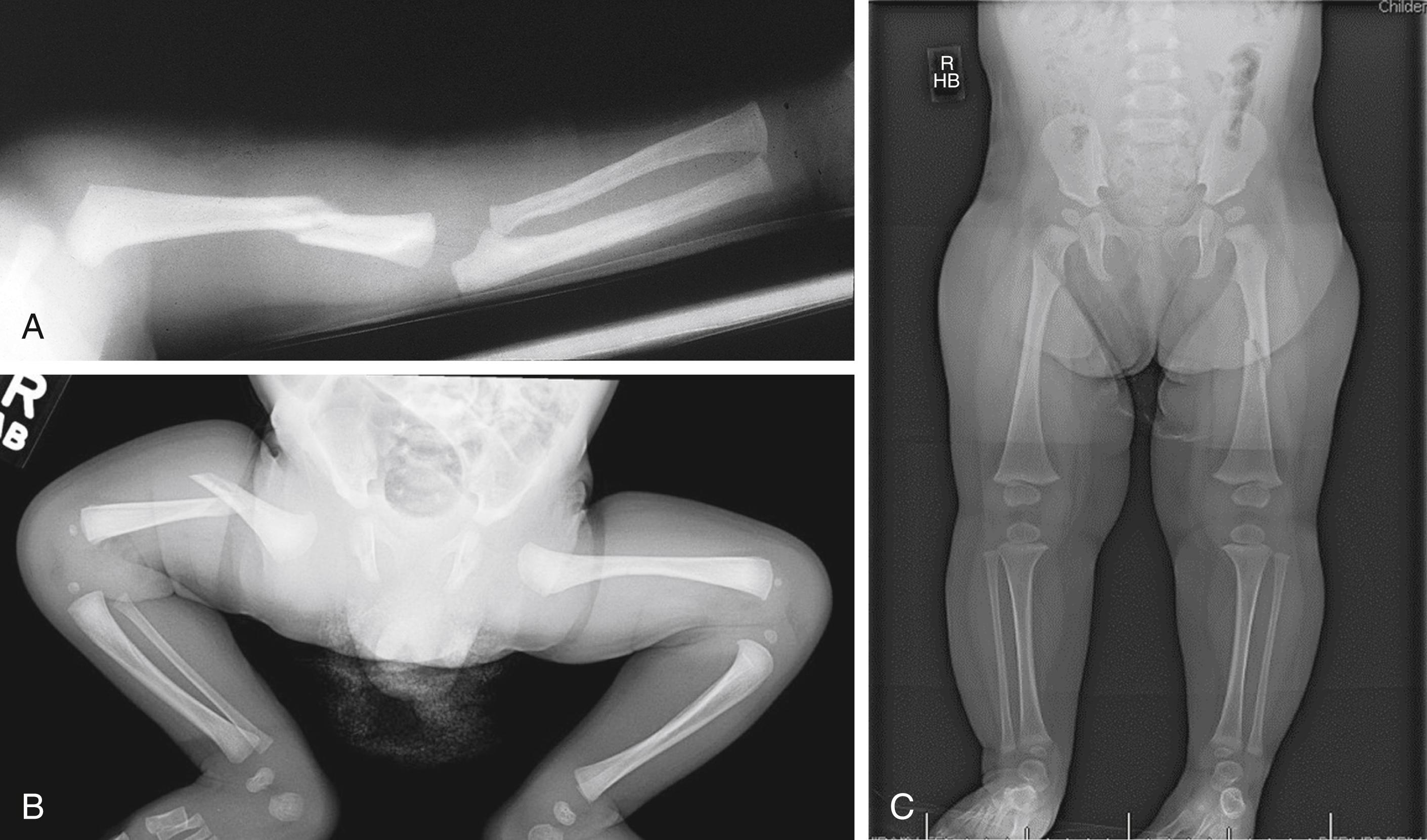
Although more commonly accidental in origin, torus or buckle fractures can be the result of abuse, especially in very young children. When mild with only slight cortical buckling, they are the result of mild-to-moderate compression forces delivered in a direction parallel or nearly parallel to the axis of a long bone. When higher energy forces are delivered, whether accidental or inflicted, there is usually some degree of angulation; in such cases, it may be more accurate to classify them as a form of compression injury ( Fig. 6.29 ). More severe forms involving the femur or tibia can be caused by throwing or slamming a child feet first or onto the knees on a hard surface.
Transverse fractures are high-energy injuries that are much more likely to be accompanied by acute soft tissue swelling and deformity. Transverse fractures are often the result of a rapidly delivered direct blow perpendicular to the long axis of a bone, such as “karate chop” or “night stick” injury ( Fig. 6.30 ). They can also occur when a child is thrown or swung and, in the process, hits an extremity against a hard edge such as that of a table, as a result of falls of greater than 6 feet, and when half of an extremity is held with both hands and snapped. Violently yanking a child up from his crib while holding an extremity or grabbing an arm and yanking it upward or sideways when the child is fixed in position by the belt of a highchair or infant seat are possible etiologies for these fractures. Inflicted supracondylar humerus fractures of the compression/distraction type are the result of grabbing an arm and yanking it into hyperextension ( Fig. 6.31 ).

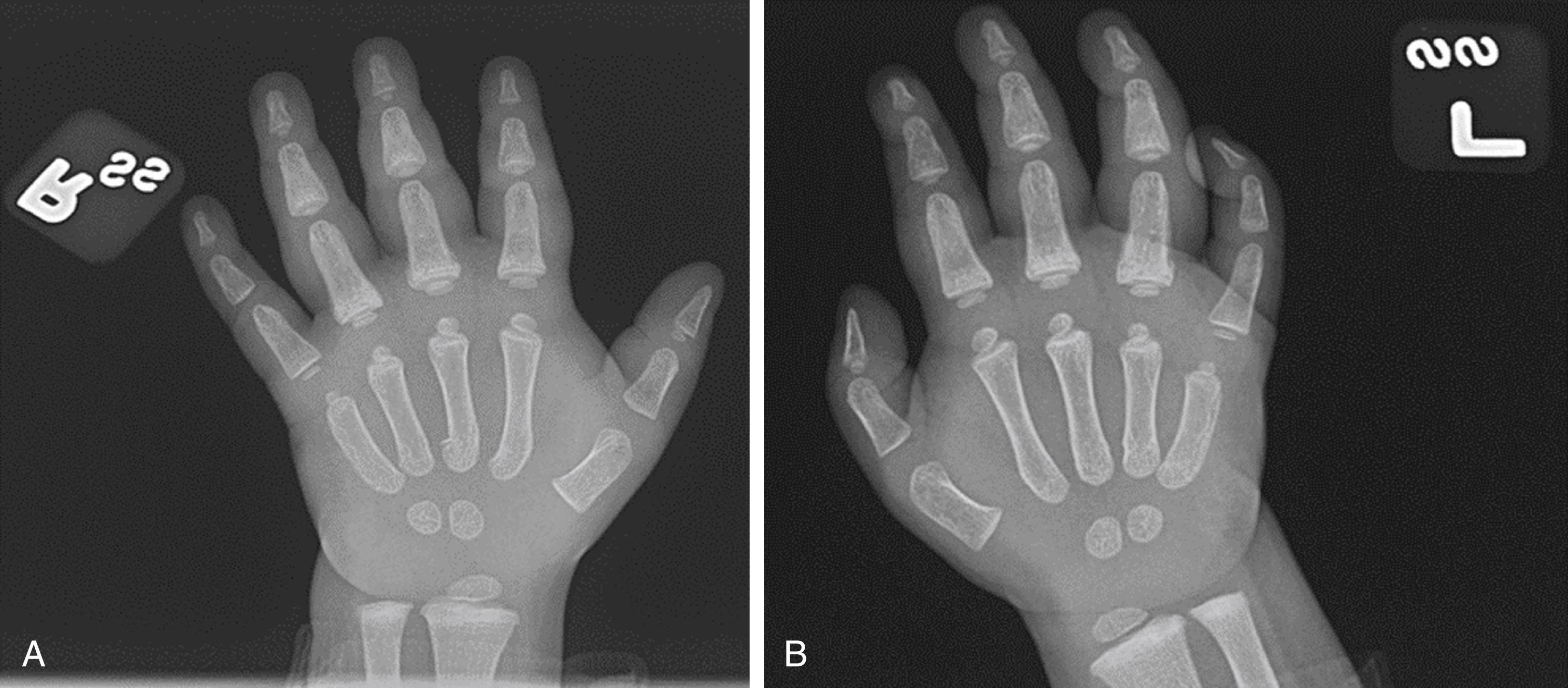
Vertebral body fractures, metacarpal and metatarsal fractures, distal or proximal clavicular fractures, and complex skull fractures are concerning for physical abuse ( Fig. 6.32 ). Vertebral body fractures are due to compression, typically associated with a child being slammed down violently and axial loading transmitting through the vertebral canal ( Fig. 6.26B ). Cervical fractures are usually the result of violent hyperflexion or hyperextension. Below the cervical spine, most fractures occur near the thoracolumbar junction. Fractures of the hands and feet are relatively uncommon but important findings to consider physical abuse. These tend to be clinically occult when first seen. Grabbing and yanking, twisting, or bending the hand or foot tend to produce metacarpal/metatarsal fractures. Subtle subperiosteal new bone formation and/or medullary sclerosis are common radiographic findings. Forced hyperextension of the phalanges can cause buckle fractures at their bases (see Fig. 6.33 ).
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here