Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Combined-modality therapy (CMT) is a treatment option for patients with locally advanced squamous cell carcinoma of the head and neck, most often in three clinical scenarios: (1) chemoradiation delivered concomitantly for an enhanced local treatment effect, known as concurrent chemoradiotherapy; (2) chemoradiation as adjuvant therapy after definitive surgical resection; (3) initial induction chemotherapy followed by concurrent chemoradiotherapy known as sequential chemoradiotherapy.
Functional organ preservation is possible with CMT without compromising survival in many patients with locally advanced oropharyngeal, hypopharyngeal, and laryngeal cancer.
For patients at high risk of disease recurrence after definitive surgical resection, cisplatin administered concomitantly with radiotherapy (RT) results in higher overall survival than single-modality RT, especially in patients with surgical pathology that shows positive margins or extracapsular nodal extension.
Induction chemotherapy followed by concurrent chemoradiotherapy (sequential therapy) might be considered for patients at high risk for distant metastasis if the patient has a good performance status.
For recurrent, unresectable, and metastatic disease, combination drug therapy produces higher response rates than single-agent treatments. Platinum compounds (cisplatin and carboplatin), fluorouracil, and taxanes (docetaxel and paclitaxel) are preferred agents.
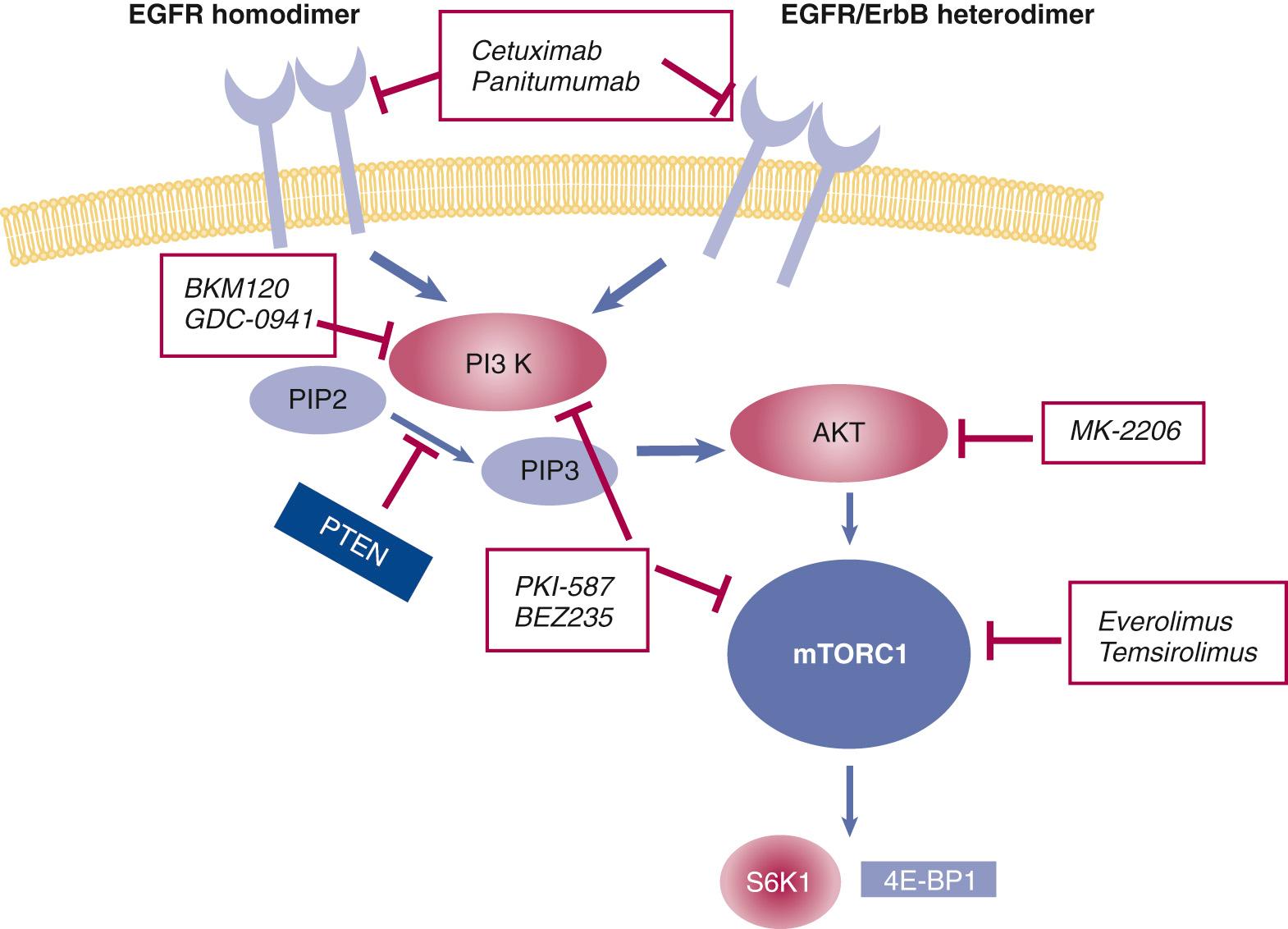
Molecularly targeted agents directed at the epidermal growth factor have emerged as important strategies for the treatment of head and neck cancers. When added to RT, cetuximab has been shown to improve survival for patients with locally advanced disease. Cetuximab added to a platinum–fluorouracil regimen improves overall survival in patients with recurrent or metastatic disease.
Another group of targeted therapy agents, the programmed cell death 1 (PD-1) inhibitors, such as nivolumab and pembrolizumab, have proven to be efficacious and safe to consider for recurrent or metastatic disease as second-line therapy.
The head and neck surgeon frequently cares for patients with squamous cell cancer of the head and neck (SCCHN), who will receive chemotherapy as a component of treatment. Often, these patients have locally advanced or metastatic disease not amenable to curative therapy with surgery or radiotherapy (RT) as single modalities. Chemotherapy may be administered concomitantly with RT (concurrent chemoradiotherapy, or CRT), in sequence with definitive RT or surgery (induction/neoadjuvant therapy), or as a single-modality treatment for patients with recurrent or metastatic disease not amenable to local curative approaches. Biologic agents targeted at specific molecular pathways involved in carcinogenesis and cancer cell proliferation, such as the epidermal growth factor receptor (EGFR) pathway, have been increasingly studied in these settings as well. This chapter focuses on chemotherapy and targeted biologic therapy as systemic strategies, their associated efficacy and potential toxicity, and current directions in clinical research.
Multidisciplinary care has become part of the fabric of caring for patients with head and neck cancer and should include a registered dietician and a speech therapist. Surgeons should be familiar with the basic principles of integrating systemic therapy as a component of combined-modality programs, the design and results of the key clinical trials, and promising experimental approaches of chemotherapy and targeted agents under study.
Before 1970, both in the community and at academic centers, chemotherapy had a limited role in the management of squamous cell carcinoma (SCC). This related to the focus of treatment with powerful local modalities, such as surgery and RT, for a diverse group of malignancies for which achieving local disease control was and still is of major importance. A commonly accepted plan for patients with stage III or IV disease of multiple sites was to perform surgical resection if feasible and then proceed to postoperative RT. Medical therapies for most cancers were in a formative state. In squamous cancers, the only drug with clearly established activity, used worldwide, was the folic acid analog methotrexate. Since then, the field has burgeoned with active cytotoxic agents, and there is a more general understanding of how best to study new compounds and integrate their use into already effective and often curative treatment plans. Assessment criteria for the study of novel compounds have become more uniform and reproducible; clearly defined parameters are now in place for the objective evaluation of response and survival time, and statistical guidelines are available to assist the design of clinical research trials to establish efficacy, determine whether toxicity risks are acute or long term, and judge outcomes in comparison with standard therapies.
The identification of the metal compound cis-diamminedichloroplatinum II (cisplatin) as a potential anticancer agent by Rosenberg in 1968 galvanized clinical research efforts to develop novel agents. This eventually led to the testing of combination chemotherapy regimens early on for the palliative benefit of patients with locally recurrent and distant metastatic cancers. After highly active chemotherapy regimens were identified, drug therapy was incorporated into combined-modality approaches for treating the newly diagnosed patient with locally advanced disease. The objectives of integrating chemotherapy into primary management were to increase local and distant tumor control to advance progression-free survival (PFS) and overall survival (OS) times. Dr. Muhyi Al-Sarraf demonstrated the high activity level of cisplatin and infusional 5-fluorouracil (5-FU) when administered as the initial treatment. Rapid regression of tumor was achieved in a majority of patients, with clinically complete responses in about 40%, without a substantial increase in the morbidity of subsequent surgery or RT. Moreover, in a proportion of patients with responding tumors, no histologic evidence of residual tumor was found in resected specimens. This subset of patients achieved superior OS, an observation that led to trials to test “nonsurgical” treatment programs that initially consisted of induction chemotherapy (IC) followed by RT versus more standard surgical resection for selected patients with cancers of the oropharynx and larynx, most notably the Veterans Administration (VA) larynx study, with objectives of maintaining curative outcomes but also achieving organ preservation. In addition to investigational trials that used chemotherapy before definitive local therapy, concomitant primary and surgical adjuvant chemotherapy and radiotherapy (CRT) have undergone extensive testing and have become components of care for many patients.
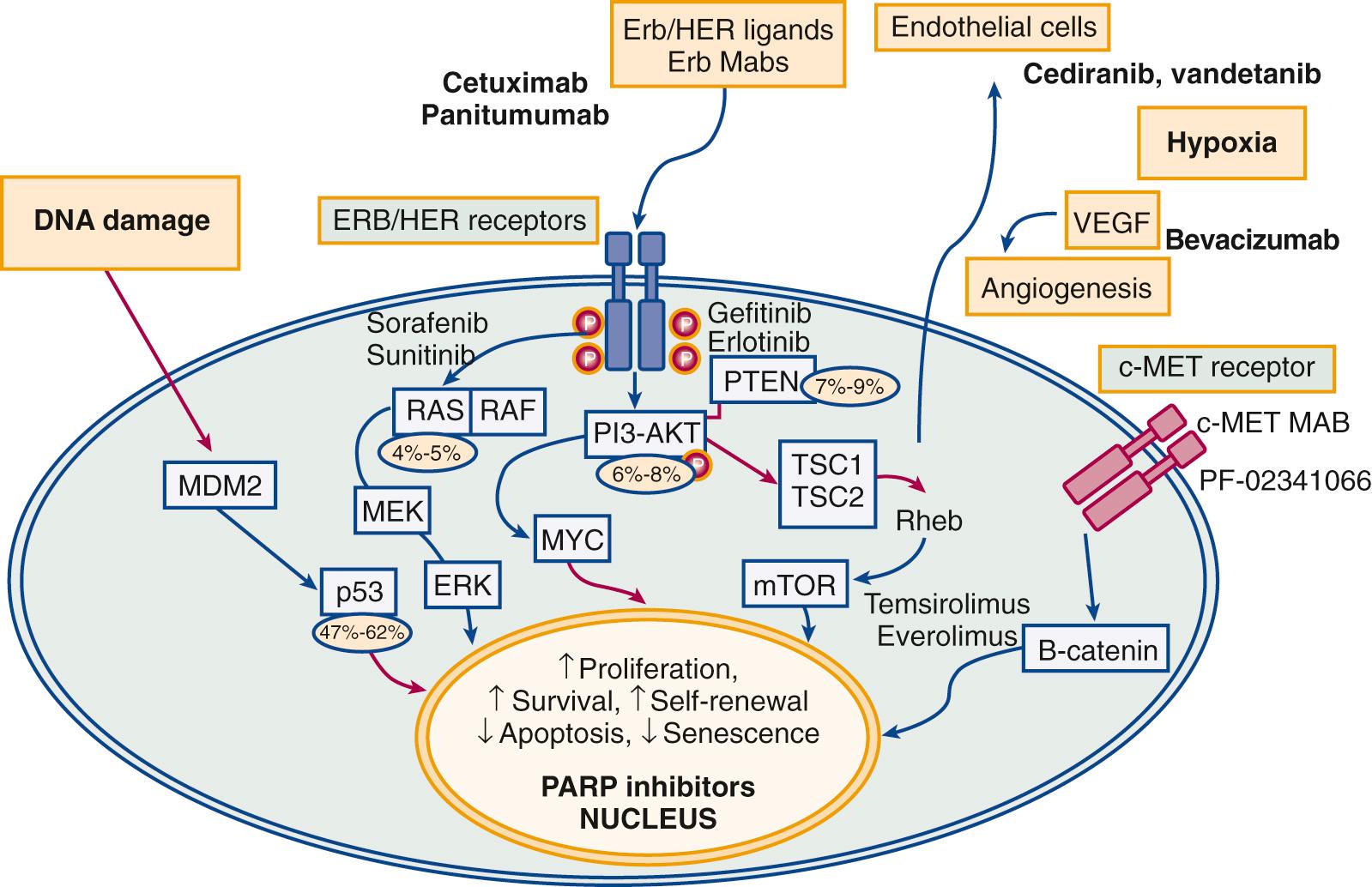
A new class of drugs— targeted biologic agents or molecular targeted agents —has become available for the treatment of cancer. These compounds have a distinct mechanism of action: they block specific molecular pathways that may drive cancer cell proliferation. As a result, molecularly targeted drugs exhibit antiproliferative, proapoptotic, antiangiogenic, and CRT-sensitizing properties that contribute to clinical antineoplastic effects. Adverse events associated with these drugs differ from the classic side effects observed with cytotoxic agents and are largely determined by the target pathway inhibited. Bonner and colleagues demonstrated that cetuximab, a biologic agent that targets EGFR ( Fig. 76.1 ), when given concomitantly with RT improves PFS and OS of patients with head and neck cancer, without an apparent increase in the incidence of severe RT-induced “in-field” side effects. This study has been accepted as a compelling indication that biologic agents will become accepted therapeutic agents in the treatment of SCCHN. Moreover, the report stimulated an exciting era for research and clinical management of SCCHN.
In the following sections, the roles of chemotherapy and biologic therapy in the treatment of locally advanced and recurrent or metastatic SCCs are discussed. Systemic therapy as a single-modality treatment has no current role as a curative treatment option. However, the addition of CRT has been demonstrated to improve local control and survival, both as a definitive treatment approach with organ-preservation goals and after surgical resection for patients at high risk for tumor recurrence. For locally advanced disease, chemotherapy given as an induction strategy before definitive RT or CRT may also affect survival. The study data for combination chemotherapy consisting of docetaxel, cisplatin, and 5-FU will be discussed.
Over recent years, the causative role for human papillomavirus (HPV), especially subtype 16, has been recognized in the pathogenesis of an increasing and very substantial percentage of oropharyngeal SCCs. Transmission is sexual. The E6 and E7 viral oncogenes are overexpressed, with associated dysregulation of the cell cycle that affects cell survival through enhanced degradation of the p53 protein and disruption of the function of the retinoblastoma gene–encoded protein. Indeed, molecular studies suggest that HPV-positive tumors have relatively minimal genomic alterations and that, stage for stage, prognosis is better than in patients with HPV-negative tumors, which tend to have complex genomic alterations that include mutations in TP53, NOTCH1, FAT1, phosphatidylinositol 3 kinases (PIK3), HRAS, and FBXW7 ; loss of p16 expression through gene deletion, mutation, or methylation; and amplification and overexpression of the cyclin D1 and EGFR genes. In patients with HPV-positive malignancies, the risk of second primary cancers in nonsmokers appears to be low, approximately 6% at 5 years compared with a 20% to 30% incidence in patients treated for tobacco-associated SCCHN. This distinct entity, the HPV-positive cancer, has changed the patient spectrum in head and neck clinics across Europe and the United States, influencing management and clinical research initiatives. Outcomes data will be considered in the discussions in the following sections.
Although surgery and/or RT achieve a cure in a high percentage of patients with early stage I and II SCCHNs, conventional treatment does not achieve cure for the majority of those with locally advanced disease, and treatment for recurrent disease with chemotherapy is far from satisfactory. Thus, much effort has been directed toward improvements in primary treatment programs with advances in combined-modality therapy (CMT). To this end, the following three general approaches have been established:
CRT for organ preservation, in which chemotherapy is given simultaneously with RT to enhance its effect as a definitive, potentially curative treatment, preferably for patients who less likely have risk of distant metastases (N0 and N1 presentations).
CRT as adjuvant therapy, in which chemotherapy and RT are simultaneously administered after surgery in high-risk patients in an effort to improve local tumor control.
Initial IC is followed by concurrent chemoradiotherapy, known as sequential chemoradiotherapy, which provides the additive advantages of both IC and concurrent chemoradiotherapy. This modality is usually considered for good performance status patients with a high risk of distant metastasis.
For early-stage cancers of the larynx, definitive RT or conservation laryngeal surgery produces excellent tumor control with preservation of speech and swallowing functions. These approaches are discussed in Chapter 107, Chapter 108, Chapter 109, Chapter 110 . However, a majority of patients with SCCHN come to medical attention with stage III or IV M0 disease and may require extensive or radical surgery, with potential deleterious effects on cosmesis and/or speech or swallowing function, depending on the primary site. In the 1990s, the dual objectives of improving survival and preserving organs represented major challenges and became the primary focus in clinical trial development. This ultimately led to the VA Laryngeal Cancer Study, which tested a nonsurgical alternative for locally advanced SCC of the larynx, matching IC followed by definitive RT against laryngectomy with postoperative RT.
IC with cisplatin-based regimens were found to be highly active, with clinical partial and complete responses observed in 80% to 90% of previously untreated patients. Therefore, it was postulated that a substantial response to initial treatment with chemotherapy would lead to an improvement of therapeutic efficacy for surgery or RT. If so, RT might then become an acceptable alternative to laryngectomy with organ preservation. In the VA study, 332 patients with stage III or IV SCC of the larynx were randomly assigned to receive either IC consisting of cisplatin and 5-FU followed by RT or surgery with postoperative RT. Patients who experienced no tumor response to chemotherapy or those who had locally persistent or recurrent cancer underwent salvage laryngectomy. Two-year survival for both treatment groups was 68%, and 41% of patients randomly assigned to the experimental arm were alive with a functional larynx at 2 years. Thus, the efficacy of chemotherapy followed by RT with surgical salvage was similar to that of surgery followed by RT, which established organ preservation as a realistic goal of nonsurgical treatment administered with curative intent.
Lefebvre and colleagues later reported data from a European trial that involved patients with cancers of the hypopharynx. In this randomized study that compared IC followed by RT in responding patients with surgical resection and postoperative RT, OS rates in the two arms were considered equivalent, which again demonstrated that larynx preservation could be achieved in some patients without jeopardizing OS. Pointreau and associates published more data, in 2009, comparing IC using cisplatin and 5-FU with docetaxel 75 mg/m 2 , cisplatin 75/m 2 , and 5-FU 750 mg/m 2 infusion for 5 days (TPF) in hypopharyngeal and laryngeal cancer. In 220 patients, results showed a superior overall response rate of 83% with TPF versus 61% for cisplatin and 5-FU. The rate of larynx preservation was also better: 80% of patients preserved the larynx in the TPF arm versus 58% in the cisplatin and 5-FU arm. Neutropenia was greater in the experimental arm (57% vs. 35%). On balance, TPF demonstrated a significantly superior tumor response rate, was tolerated with acceptable toxicity, and was associated with better larynx preservation.
In the VA study, trends were observed in patterns of tumor relapse: 20% of patients in the chemotherapy arm had locoregional recurrence compared with 7% in the surgery arm. Distant disease recurrence was more likely in the surgical arm and affected 17% of patients in that group, but it affected only 11% in the CRT arm. Salvage laryngectomy was required more often in patients with glottic cancers than in those with supraglottic primary sites (43% vs. 31%, respectively), in patients with fixed vocal cords than in those with mobile vocal cords (45% vs. 29%), and in patients with gross invasion of thyroid cartilage than in those without (41% vs. 35%). Notably, salvage laryngectomy was required in 56% of patients with T4 cancers but in only 29% of patients with smaller primary tumors ( P = .001).
The VA study has prompted further investigations of chemotherapy and RT in the treatment of intermediate-stage laryngeal cancer using the sequential administration of IC, consisting of cisplatin 100 mg/m 2 and a 5-FU infusion of 1000 mg/m 2 /day for 5 days, followed by RT as the control arm. In a study reported in 2003 by Forastiere and colleagues, namely the Intergroup Radiation Therapy Oncology Group (RTOG) 91-11 trial, this regimen was compared with concomitant cisplatin 100 mg/m 2 in weeks 1, 4, and 7 and RT against RT administered as a single treatment modality. For all groups, a total of 547 patients, surgical salvage was reserved for patients with persistent or locally recurrent disease. Eligible patients had stage III (64%) or IV disease (36%). Those with T1 staging were not eligible, and most T4 disease, with tumor extension beyond 1 cm of the tongue base or cartilage invasion, was also excluded. The rate of preservation of the larynx was the greatest in patients who received CRT. Acute severe-grade mucocutaneous toxic effects of treatment were also most common in patients who received RT with concomitant cisplatin.
In 2013, Forastiere and colleagues provided a 10-year analysis of the Intergroup RTOG 91-11 data ( Table 76.1 ). Most notably, laryngeal preservation was the greatest in those patients randomly assigned to CRT with cisplatin (82% vs. 64% with RT alone; P < .001). Data for patients living with preservation of the larynx were similar when contrasting the cisplatin and 5-FU induction arm with CRT. Moreover, long-term survival was 38% in the induction arm compared with 27% in the CRT arm (a trend with P = .08). Disease-free survival (DFS) was similar for the sequential and CRT strategies. Risk of systemic disease recurrence was reduced in patients who received chemotherapy relative to those in the group that received RT alone. With regard to long-term speech and swallow functions, no clear superiority was apparent among the treatment arms, and inability to swallow was reported in less than 3% of patients across all treatment groups. The ability to swallow only soft foods was evident in 13% to 14% of patients in the induction arm and in 17% to 24% of patients who received CRT.
| Therapy Protocol | % RT Compliance | % Laryngectomy-Free Survival | % Larynx Preserved |
|---|---|---|---|
| Cisplatin/fluorouracil followed by RT | 86 | 29 ( P = .02 vs. RT) | 68 |
| RT + cisplatin | 93 | 24 ( P = .03 vs. RT) | 82 ( P < .001 vs. RT) |
| RT alone | 95 | 17 | 64 |
These trials indicate that for patients with intermediate-stage SCC of the larynx, a combined treatment program with the objectives of tumor eradication and laryngeal preservation is feasible and reliable. It should be emphasized that patients with large, destructive, T4 primary laryngeal cancers were not included in the RTOG 91-11 trial. This group of patients may require total laryngectomy for optimal tumor control and preservation of swallowing without aspiration. Vengalil et al. demonstrated that a proportion of patients with T4 laryngeal cancer, mainly with low volume minimal cartilage involvement, may still benefit from an organ preservation approach followed by close surveillance with prompt salvage treatment for those with locoregional recurrence. However, the treatment planning should be multidisciplinary for accuracy in staging and the most effective decision making. Moreover, to optimize long-term function, patients should also be systematically followed by physicians experienced in the diagnosis and care of patients with laryngeal cancer and also by qualified speech pathologists. The value of multispecialty care in managing complex cancers of the head and neck cannot be overemphasized.
Over the past 15 years, CRT has become a standard-of-care treatment approach for patients not considered candidates for surgery who have locally advanced SCCs of the larynx, oropharynx, and hypopharynx. The theoretic rationale for and mechanism of the interaction between cytotoxic drugs and irradiation that results in additive or synergistic enhancement have been reviewed in detail. This biologic phenomenon relates to several mechanisms that include (1) inhibition of DNA repair, (2) redistribution of cells in sensitive phases of the cell cycle, and (3) promotion of oxygenation of anoxic tissues. The net effect is to improve cellular cytotoxicity. The benefits of adding chemotherapy delivered during irradiation are most notably demonstrated in two meta-analyses. CRT achieves better local control and a 6.5% survival advantage at 5 years over RT administered as a single modality. This is truly a clinically significant difference in patients with SCCHN, given the multiple competing causes of death: tumor recurrence, chronic general medical illness associated with tobacco and alcohol abuse, and second primary tumors. Notably, however, this approach to improved tumor control may be associated with increased acute and chronic toxicities that include overall debility, pharyngeal stenosis with gastrostomy tube dependence, and recurrent infections related to aspiration. These treatment outcomes further underscore the need for multidisciplinary care as a prerequisite for optimal patient selection, therapy planning, and execution.
The choice of the best chemotherapy regimen to be used in conjunction with irradiation has not been well addressed in prospective randomized trials, but cisplatin 100 mg/m 2 administered on days 1, 22, and 43 of a daily radiation treatment plan has been accepted as a standard control arm in clinical trials. The major drugs with efficacy for SCCHN and in vitro evidence of radiation enhancement capability have been tested as single agents since the 1960s. Most single agents used to treat patients with head and neck cancer have been combined with RT. Multi-agent CRT has also been evaluated in several studies. Data from selected randomized trials of combined therapy are cited, and in general, no convincing evidence indicates that multi-agent chemotherapy is superior to single-agent chemotherapy when given concomitantly with RT for patients able to tolerate cisplatin administration. In addition, nearly all reported trials of CRT (single-agent or multi-agent) and RT have noted enhanced acute radiation-induced toxicity, primarily mucocutaneous; this may result in dose reductions and interruptions in the radiation fractionation schedule, which violates a guiding principle of radiation therapeutics. Thus, in combining these two treatment modalities, especially when multi-agent chemotherapy regimens are used, it is essential that sensitizing drug-related toxicity should not be allowed to compromise an optimal radiation dose, schedule, and volume plan. As a result, single-agent cisplatin therapy has evolved as a predictable and effective regimen and is a standard chemoradiation program in the United States for head and neck cancers of any site. In part, this development has been due to favorable results observed in the larynx trials cited previously and the Intergroup 0099 trial for nasopharyngeal carcinomas. In this study, patients were to receive either RT alone or cisplatin (100 mg/m 2 on days 1, 22, and 43) during RT, followed by adjuvant chemotherapy with cisplatin and 5-FU (three cycles). An analysis of 147 randomly assigned patients revealed significant differences in 3-year survival time (78% vs. 47%) and PFS time (69% vs. 24%) favoring the CRT group.
An alternative approach to combined drug therapy and RT has been developed by Robbins and Homma, with rapid infusion of high-dose intra-arterial (IA) cisplatin followed by the systemic neutralizing agent sodium thiosulfate administered with concomitant irradiation, a technique known as RADPLAT . Drug is infused selectively into the tumor bed after placement of microcatheters with the intent of concentrating the cytotoxic compound within the tumor and minimizing systemic exposure in order to gain a marked therapeutic effect with reduced systemic toxicity. In a 2008 report on a series of 240 patients with T3 or T4 SCCs of the oral cavity, oropharynx, and hypopharynx in whom RADPLAT was used, local disease control ranged from 69% to 89% and was most favorable for patients with oropharyngeal lesions. It may be beneficial for patients with relatively large tumors (≥30 cm 3 ) not extending across the midline. Despite almost several decades of experience, the use of IA chemotherapy for the treatment of head and neck cancer is limited. The overall reported response rates were not substantially different from the therapeutic results obtained with systemic therapy. Laryngeal necrosis, severe mucositis, osteonecrosis, and neurologic defects may occur with its use.
Biologic agents have been studied in combination with RT as well, with EGFR-targeted agents representing the class of drugs in the most advanced stages of clinical development. Fig. 76.2 depicts signaling pathways considered to be potential targets for new drugs in development (see also Fig. 76.1 ). The overexpression of EGFR in head and neck squamous cell carcinoma is associated with a poor prognosis. The therapy based on EGFR has shown promising effects in improving OS. In the important study previously cited, Bonner and associates conducted a prospective Phase III trial in 424 treatment-naïve patients with stage III and IV SCC of the oropharynx, hypopharynx, and larynx. Patients were randomly assigned to RT as a single modality or RT with cetuximab administered on a weekly schedule at 250 mg/m 2 after an initial loading dose of 400 mg/m 2 . The experimental regimen was generally well tolerated, although 3% of patients who received the targeted agent demonstrated severe hypersensitivity reactions; notably, grades 3 and 4 “in-field” mucocutaneous toxicity was not increased in the combined-modality treatment arm. Moreover, locoregional tumor control (median 24.4 months vs. 14.9 months for RT only) and OS (hazard ratio [HR] for death 0.74; P = .03) were higher in the combined-modality arm. In a retrospective subset analysis, the survival advantage was most favorable for patients with oropharyngeal primary cancers, although the study was not sufficiently powered for a survival analysis according to primary site. With a longer follow-up period, the local disease control and OS advantages maintained over time attest to the biologic effect of combining an active EGFR-inhibiting agent with RT. A favorable tumor response and survival benefits correlated with treatment-associated folliculitis, as was observed earlier in Phase II cetuximab trials in patients with metastatic disease. Association of tumor EGFR expression or mutation with outcomes has not been demonstrated; this could be used as a selection factor for treatment with cetuximab and RT, and so, more work in this area is needed. This trial was a landmark study, because it was the first to demonstrate a survival advantage for patients who receive targeted therapy in the primary treatment of SCCHN.
The influence of HPV status on outcomes data has been striking. In a prospective trial, Fakhry and colleagues reported a significantly improved 2-year OS of 95% versus 62% ( P = .005), respectively, in patients with HPV-positive oropharyngeal cancer (OPC) treated with IC followed by CRT compared with a matched group of patients with HPV-negative cancers. In a large experience from the Princess Margaret Hospital, a retrospective look at outcomes for 505 patients treated with RT or CRT for OPCs, the subset of HPV-positive patients ( n = 382) compared with HPV-negative patients ( n = 123) had higher local (94% vs. 80%) and regional (95% vs. 82%) tumor control ( P < .01). In a retrospective analysis of outcomes data from an RTOG trial in patients with stage III/IV disease, Ang and associates compared accelerated RT with concomitant cisplatin 100 mg/m 2 for two cycles and standard fractionation radiation with cisplatin on weeks 1, 4, and 7 and identified a subset of 323 patients with OPC for whom HPV status could be determined. With median follow-up of 4.8 years, 3-year survival was greater in 206 HPV-positive patients (82.4% vs. 57.1%; P < .001). Furthermore, Rosenthal et al. have studied the association of HPV and p16 protein expression status with outcomes in OPC patients treated with RT plus cetuximab or RT alone. Of 182 patients enrolled in the study group, 41% were p16 positive. In both group, p16-positive patients had a longer OS than p16-negative patients (HR, 0.40; 95% CI, 0.21 to 0.74 vs. HR, 0.16; 95% CI, 0.07 to 0.36). The addition of cetuximab to RT was associated with better locoregional control, OS, and PFS in both patients with p16-positive and p16-negative disease. This study identified that p16 status is strongly prognostic for OPC and clearly suggests that the addition of cetuximab to RT improved clinical outcomes regardless of p16 or HPV status versus RT alone.
The influence of tobacco on prognosis was also notable. A history of tobacco use (>10 packs/year consumption) conferred a negative prognostic influence in this trial. Remarkably, HPV-positive patients with a less than 10-year smoking history had projected survival at 5 years of greater than 90%. After a recursive partitioning analysis, risk of death was found to be significantly associated with HPV status, tobacco consumption history, tumor stage, and nodal status. These and other reports of favorable survival in HPV-positive patients after RT or combined treatment programs have led to ongoing studies to address the potential for modification of treatment intensity in this patient population. In a report from the Eastern Cooperative Oncology Group (ECOG), a radiation-deintensification trial for HPV-associated OPC, a total of 77 patients (median age 57 years) with HPV16 and/or p16 positive were treated with IC. Those who responded to IC received definitive RT in a modified plan of 54 Gy radiation or intensity-modulated radiation therapy (IMRT) and concomitant cetuximab, as opposed to more usual radiation dose of 72 to 72 Gy. High rate of disease control was demonstrated with 2-year PFS and OS of 80% and 94%, respectively. The induction agents, cisplatin, paclitaxel, and cetuximab, were well tolerated among patients with HPV-positive disease, and 96% of them received all planned cycles, without major delays or increase in toxicity burden. IMRT also resulted in significant improvement in swallowing and nutritional status. Future clinical trials consisting of larger sample sizes will guide the treatment modalities separately in HPV-positive versus HPV-negative patients.
Pfister and colleagues combined cetuximab with cisplatin (100 mg/m 2 weeks 1 and 4) and concomitant boost RT in patients with locally advanced disease and observed a 3-year OS rate of 76%, with locoregional disease control in 71%. Langer and colleagues reported a treatment combination with daily radiation, concomitant cisplatin (75 mg/m 2 administered in three cycles), and weekly cetuximab, followed by maintenance antibody therapy in 61 patients and observed much severe-grade toxicity, especially neutropenia (26%), fatigue (23%), and folliculitis (28%). In a large, prospective Phase III study, the RTOG tested the value of adding concomitant cetuximab to CRT and analyzed 891 patients with locally advanced SCC of the oropharynx, hypopharynx, and larynx who received cetuximab plus cisplatin radiation, versus cisplatin radiation alone at similar cisplatin delivery (mean, 185.7 mg/m 2 vs. 191.1 mg/m 2 ). Analysis with a median follow-up of 3.8 years has shown no significant difference in locoregional disease control, PFS, and OS. Meanwhile, PFS and OS were significantly higher, and distant metastasis was significantly lower in patients with p16-positive OPC over p16-negative carcinoma, but tumor EGFR expression did not distinguish outcome. However, this study also identified more than 10 packs/year of cigarette smoking as an independent predictor of poor prognosis.
More data are coming from the trials investigating the potential benefits of combining small-molecule EGFR inhibitors, such as gefitinib or erlotinib and lapatinib. A Phase II trial was conducted to assess the efficacy and safety of gefitinib. Sixty-nine patients with locally advanced SCCHN were enrolled. Patients received combined gefitinib with IC consisting of paclitaxel and carboplatin prior to RT with concomitant 5-FU and hydroxyurea. Gefitinib was administered at 250 mg/day throughout the treatment sequence and was continued for a 2-year maintenance period. After the completion of chemotherapy and radiation, 52 of 59 evaluable patients achieved complete response status, and 60 patients continued the maintenance oral gefitinib. Considerable toxicity was reported, and 59 of 69 patients developed grade 3 mucositis during CRT; in addition, four deaths occurred, two consequent to neutropenic sepsis, one as the result of a cardiac event, and one of uncertain cause. Four-year OS was 74%, higher in the 37 patients (68% HPV positive) with oropharyngeal primary cancers (HR 1.00 vs. 3.70 in others). Gefitinib was further studied in a Phase III trial in combination with docetaxel in recurrent and metastatic SCCHN. A total of 270 patients were randomly assigned to docetaxel with either placebo group or gefitinib group until disease progression. Median OS was 6.0 months versus 7.3 months, respectively (HR, 0.93; 95% CI, 0.72 to 1.21; P = .60), indicating that addition of gefitinib to docetaxel did not have survival benefit; however, the combined regimen was well tolerated.
Erlotinib, an oral tyrosine kinase inhibitor (TKI), has been studied in combination with chemotherapy and RT in SCCHN. A Phase II RCT evaluated treatment outcome from erlotinib and cisplatin group versus cisplatin group in 205 patients with locally advanced SCCHN. Both groups also received concurrent RT. The CRR and PFS did not improve with erlotinib at a median follow-up of 26 months.
A recent study has shown favorable efficacy of lapatinib, orally administered as a dual HER1/HER2 TKI in combination with capecitabine, an oral pro-drug of 5-FU, as a first-line treatment of metastatic or recurrent SCCHN. The survival benefit was found to be comparable to that of combination of cisplatin, 5-FU, and cetuximab regimen, with overall response rate of 25%, median OS of 10.7 months, and had better toxicity profile. However, the study was done in a small sample size.
In summary, organ-preservation strategies are feasible for the treatment of SCCHN. CRT produces OS similar to that achievable with surgical approaches, while avoiding extensive resections and maintaining anatomic organ preservation. Of concern in patients receiving CRT is the level of long-term organ function and quality of life. For selected patients with oropharyngeal and hypopharyngeal SCCs, CRT has been demonstrated to be superior to RT alone and is considered a standard of care for the treatment of locally advanced disease not considered to be amenable to surgical resection. Single-agent cisplatin therapy administered every 3 weeks with RT administered once daily is the most widely accepted regimen in the United States as a concurrent chemotherapy. The three-drug combinations of taxane, cisplatin, and fluorouracil (TPF) are the preferred approach for IC, as demonstrated in several clinical trials. Biologic agents, such as cetuximab, are currently being studied for the treatment of this disease as well, although optimal application has not been well defined to date. The combination of cetuximab and RT may be a suitable treatment alternative for patients who have intermediate-stage head and neck cancers or who are at high risk for platinum-based toxicities. Intermediate-stage SCCs of the larynx may be effectively treated with sequential or CRT with objectives of achieving larynx preservation at 5 years in a majority of patients and an OS equivalent to laryngectomy with postoperative therapy. Oral cavity and locally advanced laryngeal cancers are more often treated with surgical resection as the optimal definitive local approach.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here