Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Editors' comment : A complete chapter focusing on the brain in normal pregnancy and preeclampsia appeared in Chelsley's third edition, and this is its second revision. The important contributions of previous authors of this chapter, Gerda G. Zeeman and F. Gary Cunningham, are greatly appreciated. Hemorrhagic and ischemic strokes are in addition to eclamptic fits important and feared causes of maternal morbidity and mortality in women with preeclampsia. Increasing evidence now indicates that both preeclampsia and eclampsia can impact long-term maternal cerebrovascular health. This Chapter 13 includes updated clinical, epidemiological, and mechanistic knowledge since the last edition and adds important new sections on “Stroke in Pregnancy and Preeclampsia” and “Neurocognitive Functioning.” Discussions regarding prevention and management of cerebral complications, particularly eclampsia, can be found in Chapter 17. Future basic, translational, and clinical research is urgently needed to improve our mechanistic understanding of how preeclampsia and eclampsia damage the maternal brain, hopefully leading to improved prevention and treatment strategies .
The brain plays a central role in the preeclampsia–eclampsia syndrome. For many centuries, convulsions in the pregnant woman were the most recognizable event of what we now know to be a generalized disorder affecting virtually every organ system. In his first edition of Hypertensive Disorders in Pregnancy , Chesley chronicled the historical evolution of theories concerning causes of convulsions in women with eclampsia. Since the times of Hippocrates and Galen, the two main theories were either cerebral congestion — repletion , or cerebral anemia — depletion . Beliefs concerning repletion led to the widespread practice of phlebotomy during the 1700 and 1800s. Throughout much of the last century, as therapeutic measures were aimed at either halting or preventing convulsions, evidence began to accrue leading to insights into the cerebrovascular pathophysiology of eclampsia. For example, during the renaissance of neuroanatomy and pathology, intracranial hemorrhage and generalized cerebral edema were prominently emphasized.
Neuroanatomical emphasis culminated in the work of Sheehan and Lynch and their autopsy series of eclamptic women. A unique feature of this work is that the brains studied were from autopsies performed within 2 h after death, eliminating some of the postmortem changes that rapidly occur in brain tissue and might confound interpretation. By then, it was appreciated that women with fatal eclampsia frequently had brain abnormalities. As deaths from eclampsia declined over the last half of the 20th century, interest in cerebral pathology waned also because there were few avenues from which to approach appropriate investigation. The development of computed tomography (CT) in the 1970s, allowing noninvasive brain imaging, as well as Doppler studies of cerebral blood flow velocity, reawakened interest in cerebrovascular perturbations in the preeclampsia syndrome. More recently, the use of magnetic resonance imaging (MRI) has given us new opportunities to study neuroanatomical changes, as well as to more accurately measure cerebral perfusion and white matter lesions. These technologies, combined with reproducible animal models to better study cerebral blood flow and its alterations, have allowed a heretofore unknown look at cerebrovascular pathology provoked by the preeclampsia syndrome. In addition, cognitive testing and neuroimaging in formerly preeclamptic women haves suggested that this condition may have long-term effects on the maternal brain.
This chapter is designed to specifically describe cerebral pathology and pathophysiology in preeclampsia/eclampsia, as well as their clinical consequences. Other clinical aspects of the preeclampsia syndrome are discussed in Chapters 1 (clinical spectrum), 4 (prediction and prevention), 17 (clinical management and antihypertensive treatment), and 18 (long-term effects on mothers and offspring). We review the earlier neuropathological observations of eclampsia and describe noninvasive imaging findings derived from CT scanning and MR imaging. We also describe cerebrovascular abnormalities induced by preeclampsia–eclampsia measured with direct and indirect noninvasive methods such as MRI technology and Doppler velocimetry. Hypertensive effects on cerebral perfusion in both pregnant and nonpregnant animal models, from which we draw a composite description of the effects of the preeclampsia syndrome on the brain, are presented. Finally, we review current findings on long-term cerebrovascular disease in women with a history of preeclampsia.
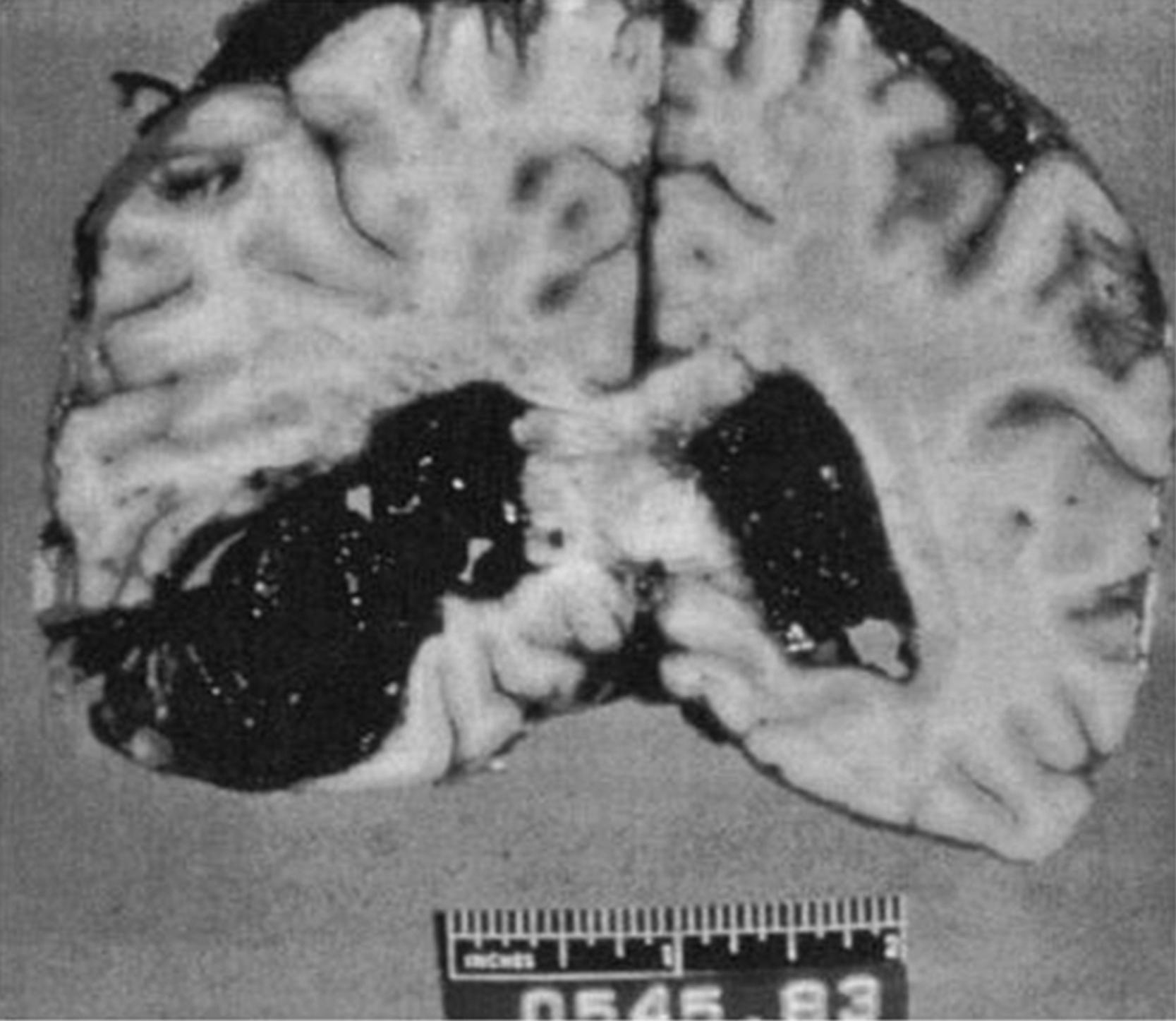
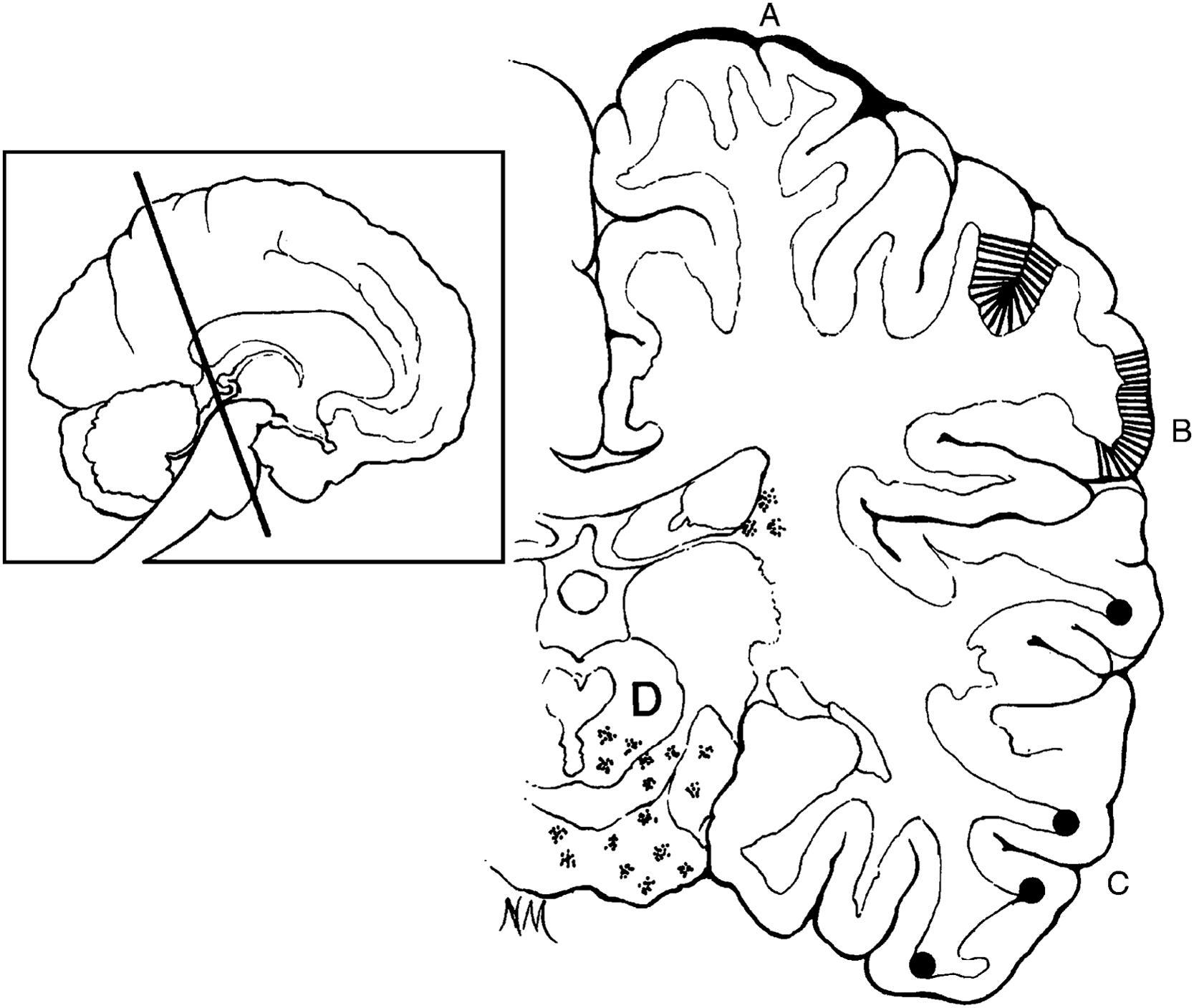
Most neuroanatomical descriptions of the brain in eclamptic women are taken from eras when mortality rates were quite high. Gross intracerebral hemorrhage was seen in up to 60% of eclamptic women and was considered the final cause of death in half ( Fig. 13.1 ). As shown in Fig. 13.2 , other principal lesions found at autopsy consisted of cortical and subcortical petechial hemorrhages. Histologically, these are composed of numerous small hemorrhages, 0.3–1.0 mm in diameter, arranged in streaks of 2–4 cm running radially in the cortex. They may appear anywhere on the gyral surface and are most common in the occipital lobes and least common in the temporal lobes. Many occur in the border zones between cerebral arterial territories. Other frequently described major macroscopic lesions include subcortical edema, multiple nonhemorrhagic areas of “softening” throughout the brain, hemorrhagic areas in the white matter, and hemorrhage in the basal ganglia or pons, often with rupture into the ventricles. In some cases, numerous small cortical infarctions are described as well. These infarcts vary from about 0.3 to 1.0 mm in diameter and are sometimes confluent. The classical microscopic vascular lesions consist of fibrinoid necrosis of the arterial wall and perivascular microinfarcts and hemorrhages.
Several neuroimaging techniques have been used to better understand the cerebrovascular mechanism(s) involved in the preeclampsia syndrome. These include both CT and MRI techniques.
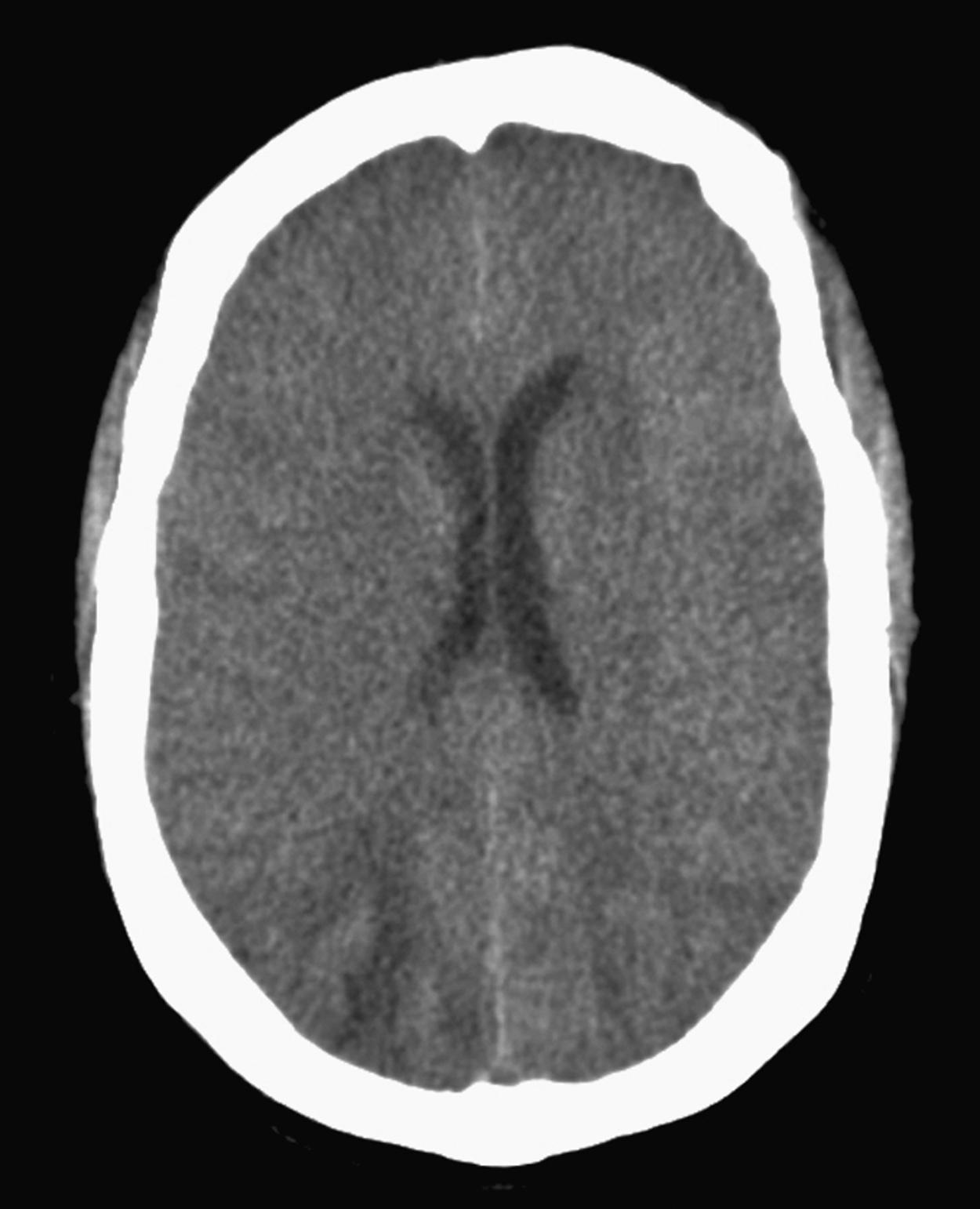
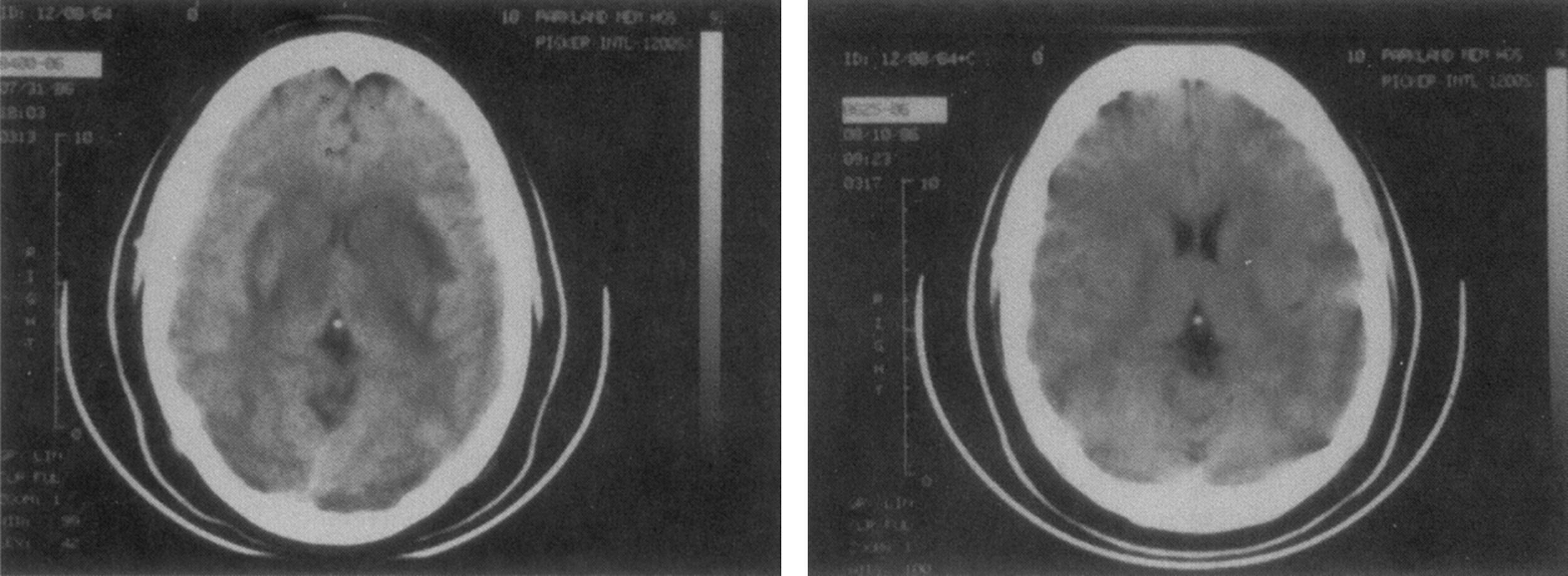
Cerebral edema. Eclampsia is typically associated with cerebral edema, which can be visualized on CT as localized, hypodense lesions at the gray–white matter junction, often in the parietooccipital lobes ( Fig. 13.3 ). Lesions may also be seen in the frontal and inferior temporal lobes, the basal ganglia, and thalamus. On MRI, this edema is visualized as hyperintense T2 lesions in subcortical and cortical regions of the parietal and occipital lobes, with occasional involvement of basal ganglia and/or brainstem. , , Some examples are shown in Figs. 13.4A and 13.5A . The spectrum of involvement is wide , and with increasing radiological involvement, either of the occipital lobes or with diffuse cerebral edema, symptoms such as lethargy, confusion, and blindness will develop. , In these cases, widespread edema shows as a marked compression or even obliteration of the cerebral ventricles ( Fig. 13.6 ). Such women may develop signs of impending life-threatening herniation. While these lesions of the posterior reversible encephalopathy syndrome (see later section) are almost universal in women with eclampsia, their incidence in women with preeclampsia is not known; however, they are more likely to be found in women who have more severe disease and who have neurological symptoms. While most reports describe reversibility of cerebral edema, , there are persistent findings in up to a fourth of eclamptic women several weeks postpartum. , , Two distinct types of cerebral edema are recognized in eclampsia: vasogenic and cytotoxic edema. Vasogenic edema is associated with increased hydrostatic pressure and ensuing capillary leak, while cytotoxic edema occurs due to ischemia and infarction with cell death. While vasogenic edema is usually reversible, ischemia may not be.
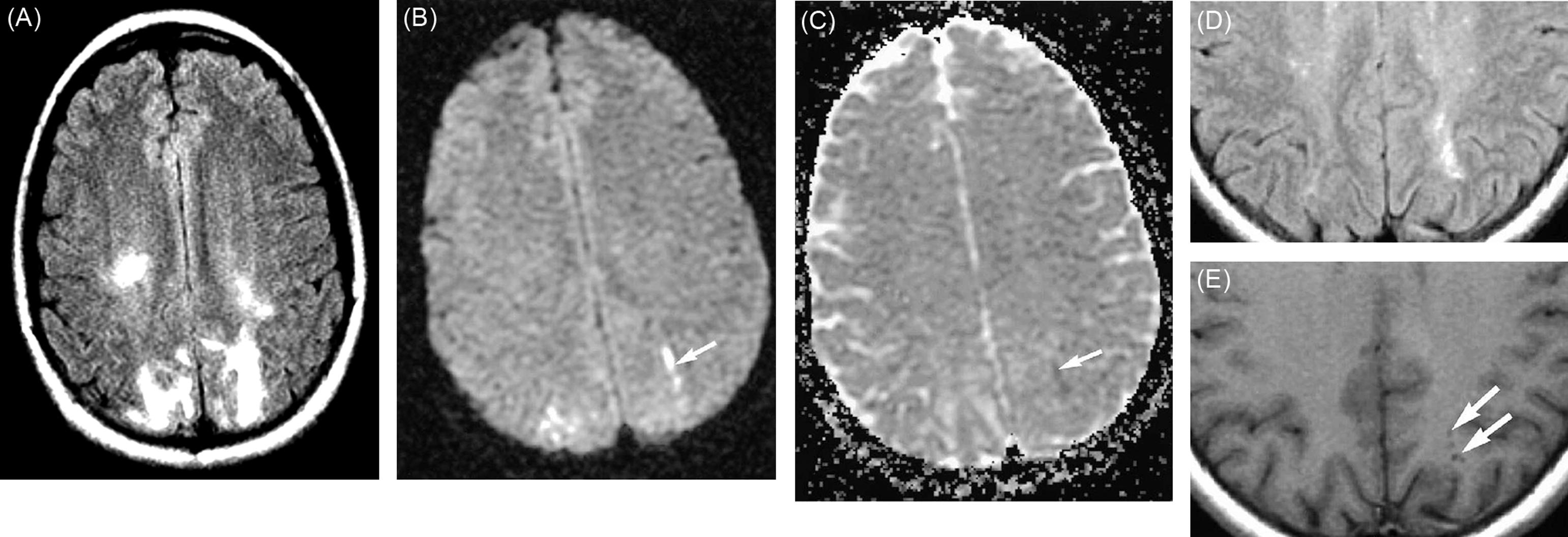
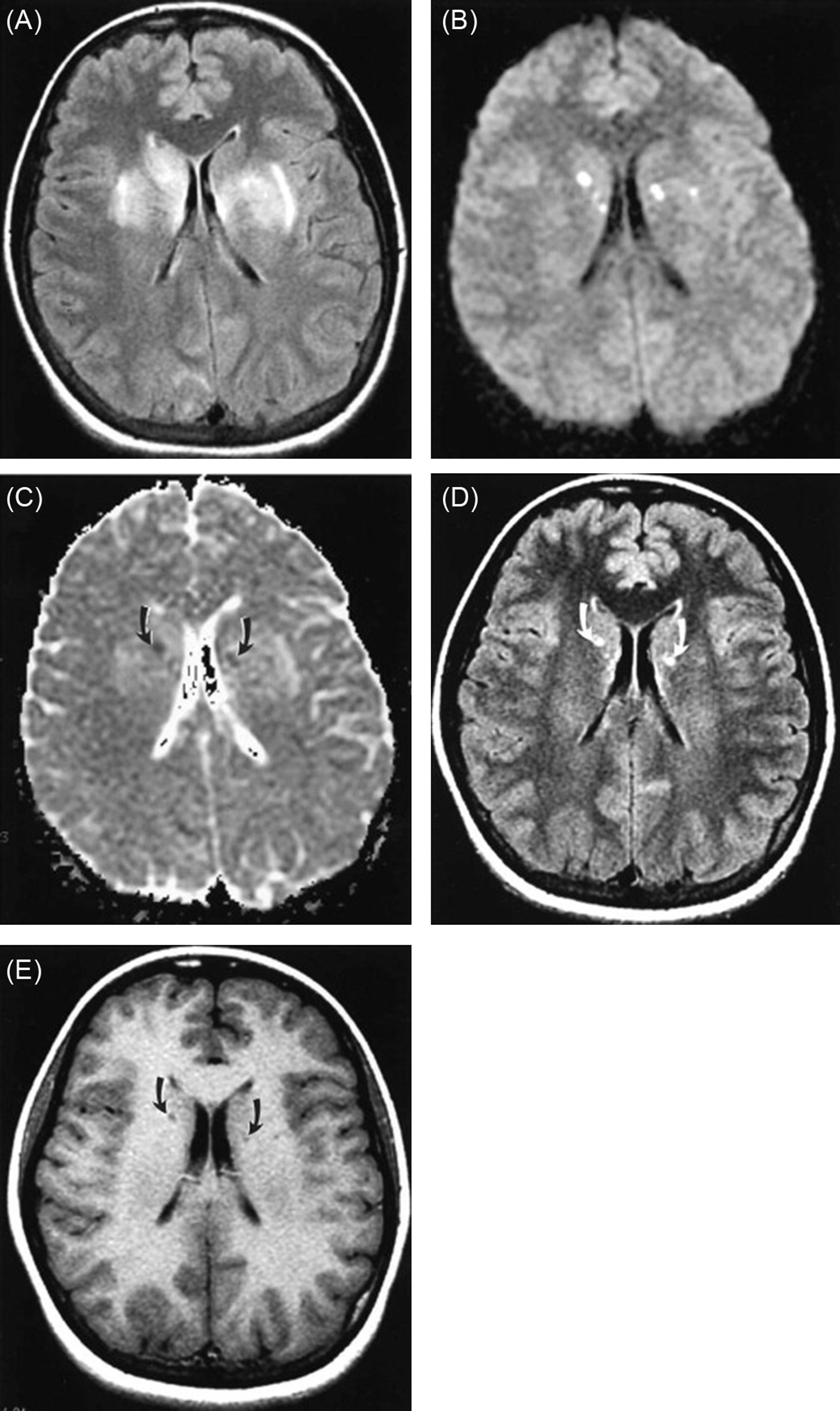
Cerebral infarction. Cerebral infarctions have been described in some women with eclampsia, sometimes with hemorrhagic transformation. , MRI findings in cerebral infarction include abnormalities on diffusion-weighted imaging (DWI) sequences and apparent diffusion coefficient (ADC) mapping. With these, it is possible to further characterize the hyperintense lesions seen on T2 imaging ( Figs. 13.4B–E and 13.5B–E ). DWI takes advantage of strong diffusion gradients that detect changes in water molecule distribution in tissue. Quantitative measurement of the diffusion property of a tissue is expressed as the ADC. Vasogenic edema is characterized by increased extracellular fluid with enhanced water diffusion and may be seen as a combination of normal DWI with hyperintense T2 signal lesions and increased apparent diffusion. , In the presence of an ischemic event, cytotoxic edema is caused by sodium pump failure, cell swelling, and eventually cell death. This causes a reduction in proton diffusion, due to a shift of water from the extracellular to the intracellular space, and it elicits a hyperintense signal on DWI but with a decreased ADC. Ischemic brain regions can be identified within minutes to hours after the onset of neurological symptoms. , , Studies in women with eclampsia using DWI sequences demonstrated primarily vasogenic cerebral edema. Less commonly, ischemic and cytotoxic changes may be seen. These latter cases have DWI hyperintense T2 lesions and decreased ADC superimposed on the pattern of vasogenic edema. , Additional MRI sequences include T2∗ susceptibility-weighted imaging (SWI) or gradient echo (GRE) for detecting hemorrhages and diffusion tensor imaging for assessing white matter structure (typically used in a research setting rather than clinically). ,
Intracerebral and subarachnoid hemorrhage. As noted by neuropathologists, both micro- and macrohemorrhage may be found in women with preeclampsia–eclampsia. On CT, acute intracranial hemorrhage is visualized as hyperdensities within the brain parenchyma or in the subarachnoid or subdural space. If acute hemorrhage is suspected, CT is the test of choice due to its rapidity and high sensitivity for acute bleeding. MRI is also highly sensitive for detection of intracranial hemorrhage, which may be visualized best on SWI or GRE as hypointense lesions.
Few studies have investigated pregnancy-induced changes of cerebrovascular hemodynamics and thus the pathogenesis of cerebral manifestations of the preeclampsia syndrome remains unclear. This is partly due to the challenges associated with in vivo studies of cerebral blood flow in human pregnancy (see below). While central nervous system histopathology is mainly based on autopsy data as discussed, most hemodynamic data are from surviving women. Although this presents some difficulty in relating histopathological with hemodynamic findings, pathological and neuroimaging data from the past few decades have led to two hypotheses to explain cerebral abnormalities associated with eclampsia. As emphasized throughout this chapter, endothelial cell dysfunction that characterizes the preeclampsia syndrome may play a key role in both hypotheses.
The first hypothesis suggests that in response to acute severe hypertension, cerebrovascular hyperreactivity leads to vasospasm. This suggestion is based on the angiographic appearance of diffuse or multifocal segmental narrowing suggestive of vasospasm of the cerebral vasculature in women with severe preeclampsia and eclampsia. , Clinically, this manifests as the reversible cerebral vasoconstriction syndrome (RCVS) , also known in this setting as Call–Fleming syndrome or postpartum angiopathy. RCVS is a well described neurological disorder characterized by recurrent “thunderclap” headaches and multifocal, reversible cerebral vasospasm. Focal neurological deficits may occur if arterial vasospasm leads to diminished CBF, hypoperfused territory, and tissue ischemia. In severe or fulminant cases, this may result in cerebral infarction, intracerebral hemorrhage, subarachnoid hemorrhage (often cortical), and seizure. The condition may occur outside of pregnancy, often triggered by drugs (particularly vasoactive or sympathomimetic substances). Postpartum angiopathy represents a subset of RCVS, occurring most often within 1 week of delivery. RCVS is more common in women with preeclampsia and other hypertensive disorders of pregnancy. However, whether RCVS causes eclampsia is not known.
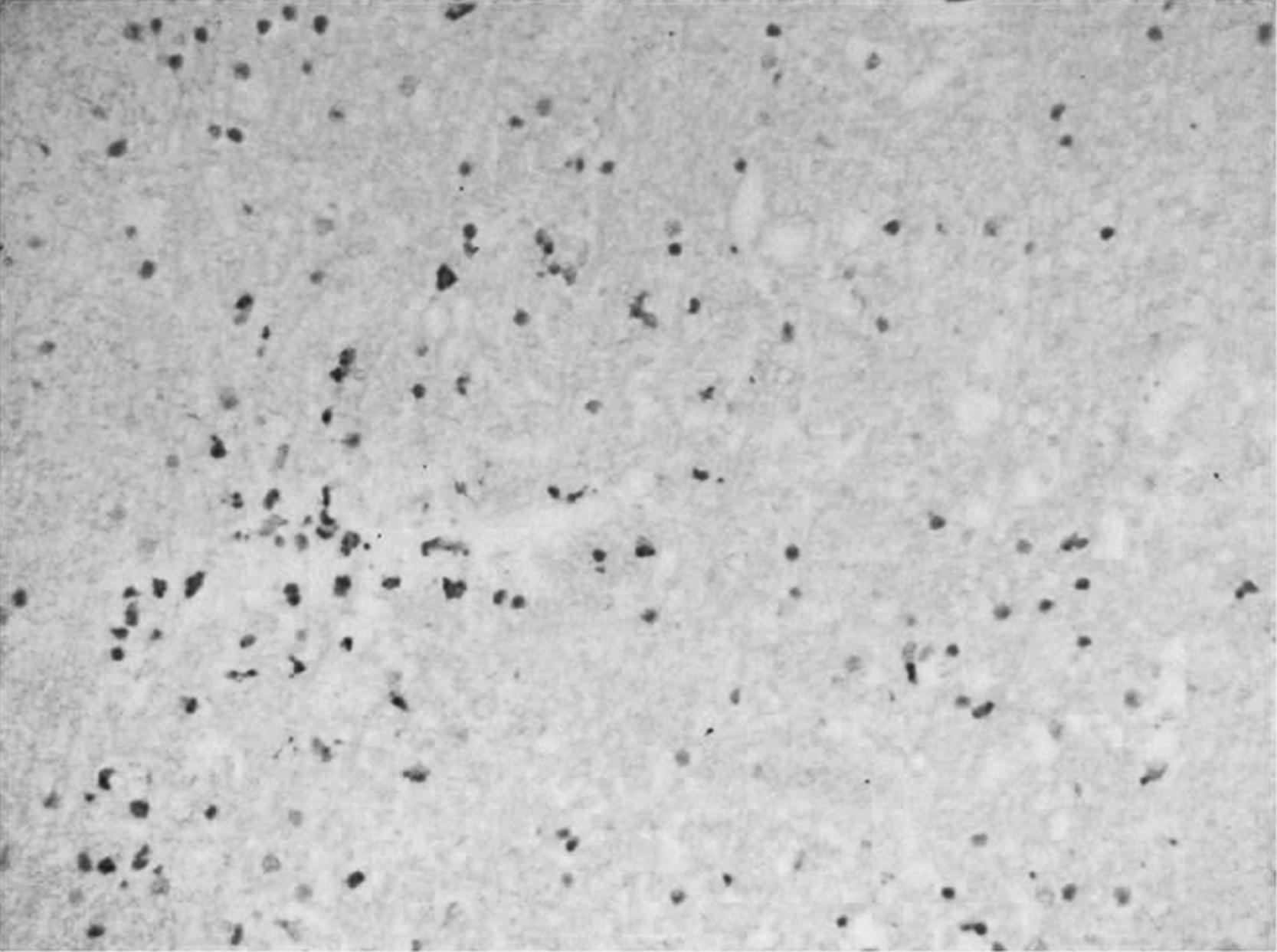
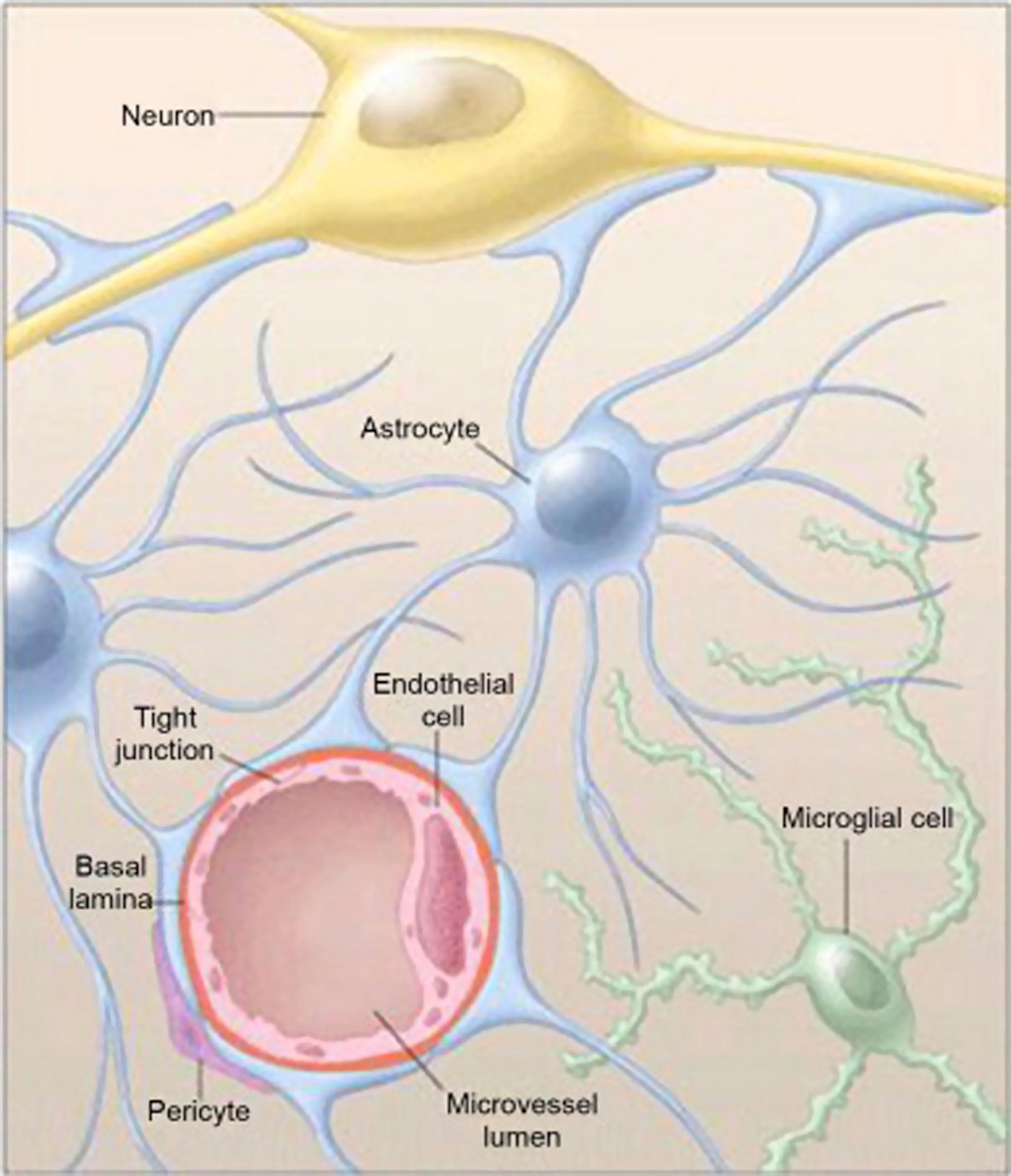
A related hypothesis is that eclampsia represents a form of hypertensive encephalopathy, in which sudden elevations in systemic blood pressure exceed the normal cerebrovascular autoregulatory capacity. , Fig. 13.7 shows a brain biopsy of a patient with hypertensive encephalopathy, a condition that may relate to preeclampsia. The decrease in cerebrovascular resistance is hypothesized to cause disruption of end-capillary hydrostatic pressure, hyperperfusion, and extravasation of plasma and red cells through opening of the endothelial tight junctions with increased pinocytosis leading to the accumulation of vasogenic edema. Regions of forced vasodilatation and vasoconstriction develop, especially in arterial boundary zones, similar to hypertensive encephalopathy. The normal structure of the neurovascular unit comprises capillary endothelial cells in close association with basal lamina, astrocytic endfeet, and pericytes ( Fig. 13.8 ). How these cells and structures are affected during preeclampsia and contribute to brain pathologies remains largely unknown. In animal studies, Tamaki et al. showed that decreased tissue perfusion and ischemia were preceded by blood–brain barrier (BBB) disruption due to marked local hydrostatic pressure. This mechanism has gained much attention over the last two decades and has been described as reversible posterior leukoencephalopathy syndrome or the posterior reversible encephalopathy syndrome (PRES). The association between PRES and eclampsia was suggested in the first published description of PRES in 1996, which included 15 patients, three of whom had eclampsia. While the condition is often predominant in posterior regions of the brain, it may involve other brain regions as well, and lesions and neurological deficits are not always reversible, particularly when they lead to intracerebral hemorrhage.
Preeclampsia and eclampsia share many features with PRES, possibly reflecting a shared pathogenesis. Its clinical, pathological, as well as neuroimaging features reflect the rapid and dynamic fluctuations in cerebral blood flow and water content. , Nearly all patients with eclampsia had PRES-like changes on MRI. , In nonpregnant and pregnant patients, PRES is usually an acute cerebral illness, which may present with headache, nausea, altered mental function, visual disturbances such as cortical blindness, and seizures. In preeclampsia–eclampsia-related PRES, headaches are more frequent than altered mental status as the initial PRES-related symptom, compared to nonpregnant PRES patients. The convulsions are commonly occipital in onset and correlate with the characteristic predominantly posterior imaging abnormalities seen with MRI in women with eclampsia. The arterial boundary zones, located at the territorial limits of the major arteries, are commonly affected sites. These zones are known as the border zone or watershed areas . In the human, the most frequently affected region in the cortex is at the parietooccipital sulci, which represent the boundary zone of the anterior, middle, and posterior cerebral arteries. Involvement of the cerebral cortex may also be seen in PRES, and lesions may extend to the brainstem, cerebellum, basal ganglia, and frontal lobes. , , However, eclampsia-related PRES cases demonstrate less frequent involvement of the thalamus, midbrain, and pons compared to nonpregnant PRES cases.
Some patients with PRES have only convulsions and do not manifest traditional prodromal signs and symptoms of hypertensive encephalopathy. In addition, particularly with extensive endothelial damage, the dramatic blood pressure increases that typify hypertensive encephalopathy are not necessarily seen, and there may be only mild to moderate blood pressure increases with PRES. , This has been described in the thrombotic microangiopathy syndromes—hemolytic uremic syndrome and thrombotic thrombocytopenic purpura—as well as with systemic lupus erythematosus, with immunosuppressive drug toxicity, or with the use of certain chemotherapeutic agents that include methotrexate and cisplatin. , Early recognition of PRES is critical, because it is usually treatable by lowering dangerously elevated blood pressure and correction of the underlying medical condition that caused endothelial cell injury. Left untreated, PRES can result in irreversible damage, including intracerebral hemorrhage and brain herniation.
Autoregulation is the process by which cerebral blood flow (CBF) remains relatively constant in the face of alterations in cerebral perfusion pressure. Put another way, when cerebral perfusion pressure declines, cerebrovascular resistance decreases due to myogenic vasodilatation of pial arteries and arterioles and hypoxic vasodilatation, thus augmenting perfusion. Alternatively, if cerebral perfusion pressure increases, the autoregulatory response stimulates vasoconstriction, resulting in relatively constant CBF. Thus, autoregulation is a physiological protective mechanism that prevents brain ischemia during drops in pressure and prevents capillary damage and edema from hyperperfusion during pressure increases. In normotensive adults, CBF is maintained at approximately 50 mL per 100 g of brain tissue per minute (mL/100 g/min), provided perfusion pressure is in the range ∼60–160 mm Hg. , Above and below these limits, autoregulation may be lost and CBF may become dependent on mean arterial pressure in a linear fashion. ,
Significant brain injury occurs when autoregulatory mechanisms are lost. For example, during acute hypertension at mean pressures above the autoregulatory limit—about 160 mm Hg in the otherwise healthy patient—the myogenic vasoconstriction of vascular smooth muscle is overcome by excessive intravascular pressure and forced dilatation of cerebral vessels occurs. , The loss of myogenic tone during forced dilatation decreases resistance and increases CBF, a result that produces hyperperfusion, BBB disruption, and acute edema formation.
The relationship between autoregulation, CBF, and BBB disruption has been extensively studied. Numerous investigators have found a positive correlation between loss of autoregulation, increased perfusion, and BBB permeability that leads to cerebral edema. , , , Importantly, mechanisms that increase resistance, such as sympathetic nerve stimulation or inward remodeling of cerebral arterioles during chronic hypertension, attenuate increases in CBF during acute hypertension and are protective of the BBB. In general, when CBF is compared in areas with and without albumin extravasation in the same brain, the regions of increased permeability have the highest blood flow, indicating loss of autoregulation and decreased cerebrovascular resistance. , , Together, these findings suggest that decreased resistance and hyperperfusion during acute hypertension may cause BBB disruption, whereas increased resistance may be protective of the microcirculation. In fact, decreased resistance that leads to hyperperfusion during acute hypertension is considered the primary cause of edema during hypertensive encephalopathy and eclampsia. , , , ,
When severe experimental hypertension is induced by intravenous infusion of vasogenic agents, arterioles develop a pattern of alternating constrictions and dilatations, giving rise to the so-called sausage-string appearance. , This vascular pattern has been demonstrated in small blood vessels in various vascular beds, including the brain. In the cerebral circulation, the development of the sausage-string pattern is linked to the development of vascular damage, specifically in the dilated regions of the vessel as they fail to maintain myogenic vasoconstriction, with resulting endothelial hyperpermeability and extravasation of macromolecules into the brain parenchyma.
The effect of pregnancy on cerebral hemodynamics and CBF autoregulation is of significant interest mostly because impaired cerebral autoregulation is thought to be a major contributor to the development of eclampsia. , , , , , , The adaptation of the cerebral circulation to pregnancy has been reviewed. From clinical observations, it is known that eclampsia can develop with only mild or even absent hypertension. While it is tempting to hypothesize that the upper limit of cerebral autoregulation is reduced with the preeclampsia syndrome, evidence for this is lacking. Alternatively, perivascular edema may develop at a lower capillary hydrostatic pressure, possibly as a function of endothelial activation and vascular permeability known to accompany the preeclampsia syndrome. Failure of autoregulatory mechanisms may also occur in response to either an acute and/or relatively large increase in blood pressure, rather than absolute blood pressure. Thus, it is possible that it is the acuteness of the blood pressure rise, or the relative change in pressure from baseline, in the setting of endothelial dysfunction, that disrupts the delicate balance between capillary and cerebral perfusion pressures in eclampsia. Understanding cerebral hemodynamic changes associated with pregnancy and preeclampsia is challenging, necessitating the use of animal models in some instances. The following sections will review both animal and clinical studies on changes in cerebral hemodynamics during pregnancy and preeclampsia.
Many women develop eclampsia at pressures that are considerably lower than those reported for PRES or hypertensive encephalopathy outside of pregnancy. , These findings suggest that the CBF autoregulatory curve might be shifted to the lower range of pressures during pregnancy. However, studies in anesthetized rats did not support this. When the upper limit of CBF autoregulation was compared between nonpregnant and late-pregnant rats, there was no difference in the pressure of autoregulatory breakthrough ( Fig. 13.9A ). Other studies in late-pregnant rats found that both the upper and lower limits of CBF autoregulation were extended, compared with nonpregnant rats. , However, only the pregnant animals developed significant edema formation in response to acute hypertension , and autoregulatory breakthrough, suggesting that the endothelium may be more susceptible to hydrostatic edema during pregnancy ( Fig. 13.9B ).
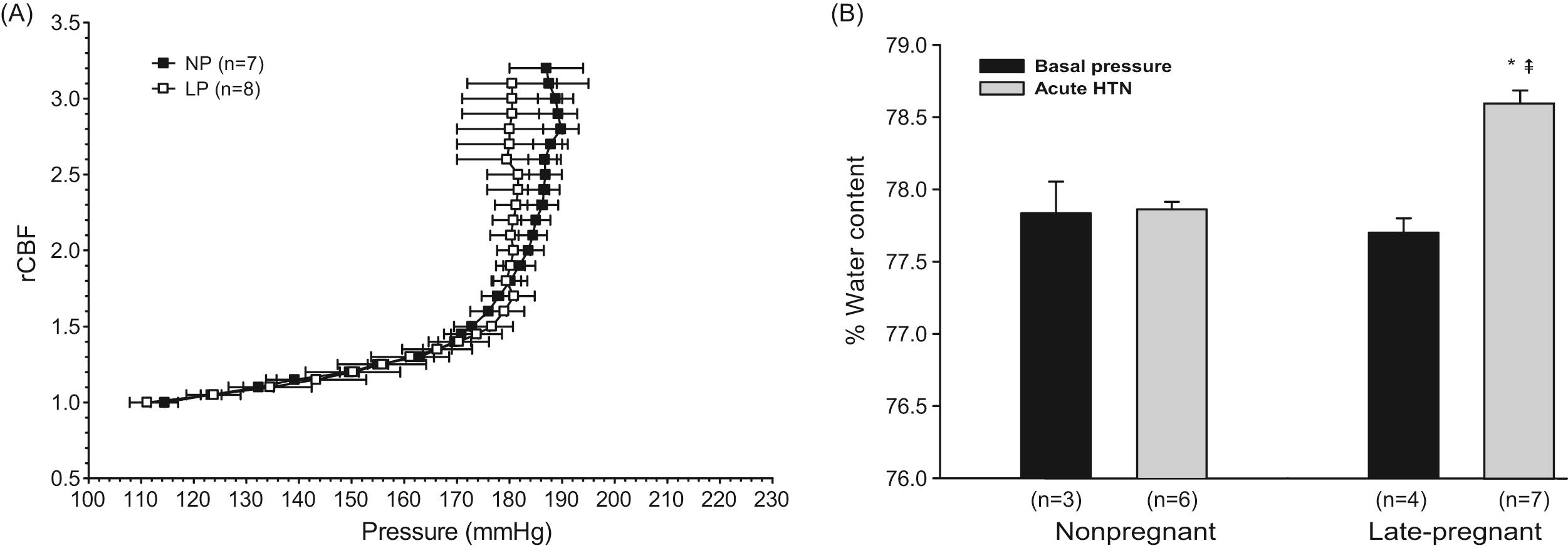
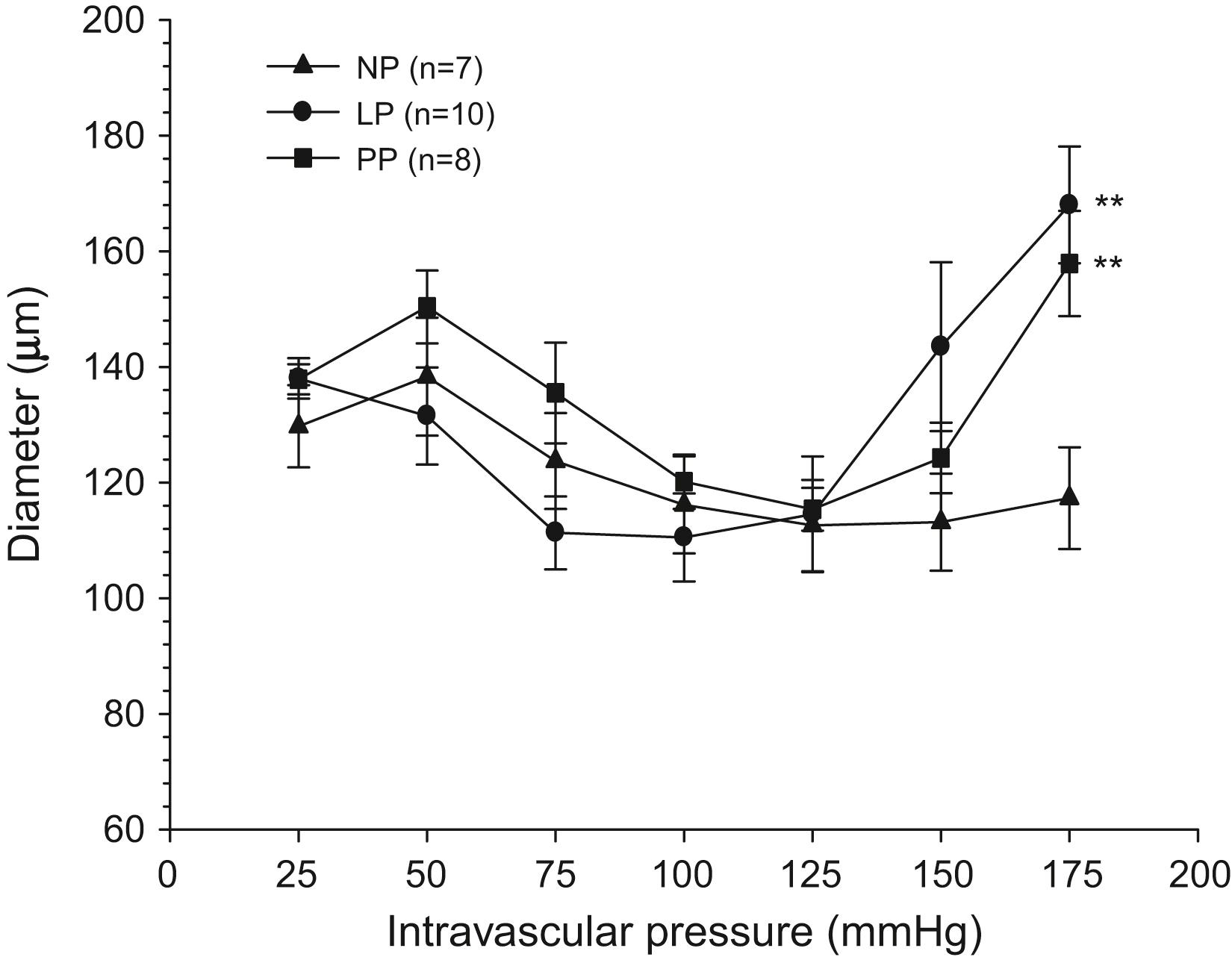
Of note, the autoregulatory curves in these studies were determined using laser Doppler methods to measure CBF and thus provide only relative changes in blood flow. , Other studies using microspheres to measure absolute CBF showed that acutely increased blood pressures in late pregnancy were associated with significantly decreased cerebrovascular resistance and increased CBF when compared with nonpregnant animals. Specifically, pregnancy was associated with a 40% decrease in cerebrovascular resistance, compared with cerebrovascular resistance in nonpregnant animals with the same change in pressure. Because increased cerebrovascular resistance in response to elevated cerebral perfusion pressure is a protective mechanism in the brain that prevents transmission of harmful hydrostatic pressure to the microcirculation, diminished cerebrovascular resistance during pregnancy in response to acute hypertension could promote BBB disruption and vasogenic edema, similar to what is seen during eclampsia. The mechanism by which pregnancy decreases cerebrovascular resistance during acute hypertension is not clear, but may be related to structural changes that affect arterial and arteriolar diameter. Resistance and flow regulation are principally determined by vessel caliber, because they are inversely related to the fourth power of vessel radius (Poiseuille's Law). The innate myogenic behavior of the cerebrovascular smooth muscle is crucial for establishment of an appropriate cerebrovascular resistance, which serves to protect downstream arterioles and capillaries in the face of changing perfusion pressures and to maintain tissue perfusion when blood pressure falls. , The cerebral circulation is a unique vascular bed, in that large extracranial and intracranial pial vessels contribute about 50% to total cerebrovascular resistance. Studies of isolated cerebral arteries from nonpregnant, late-pregnant, and postpartum animals suggest that forced dilatation occurs at lower pressures during pregnancy and postpartum ( Fig. 13.10 ). This may be a contributory mechanism by which pregnancy decreases cerebrovascular resistance during acute increases in pressure.
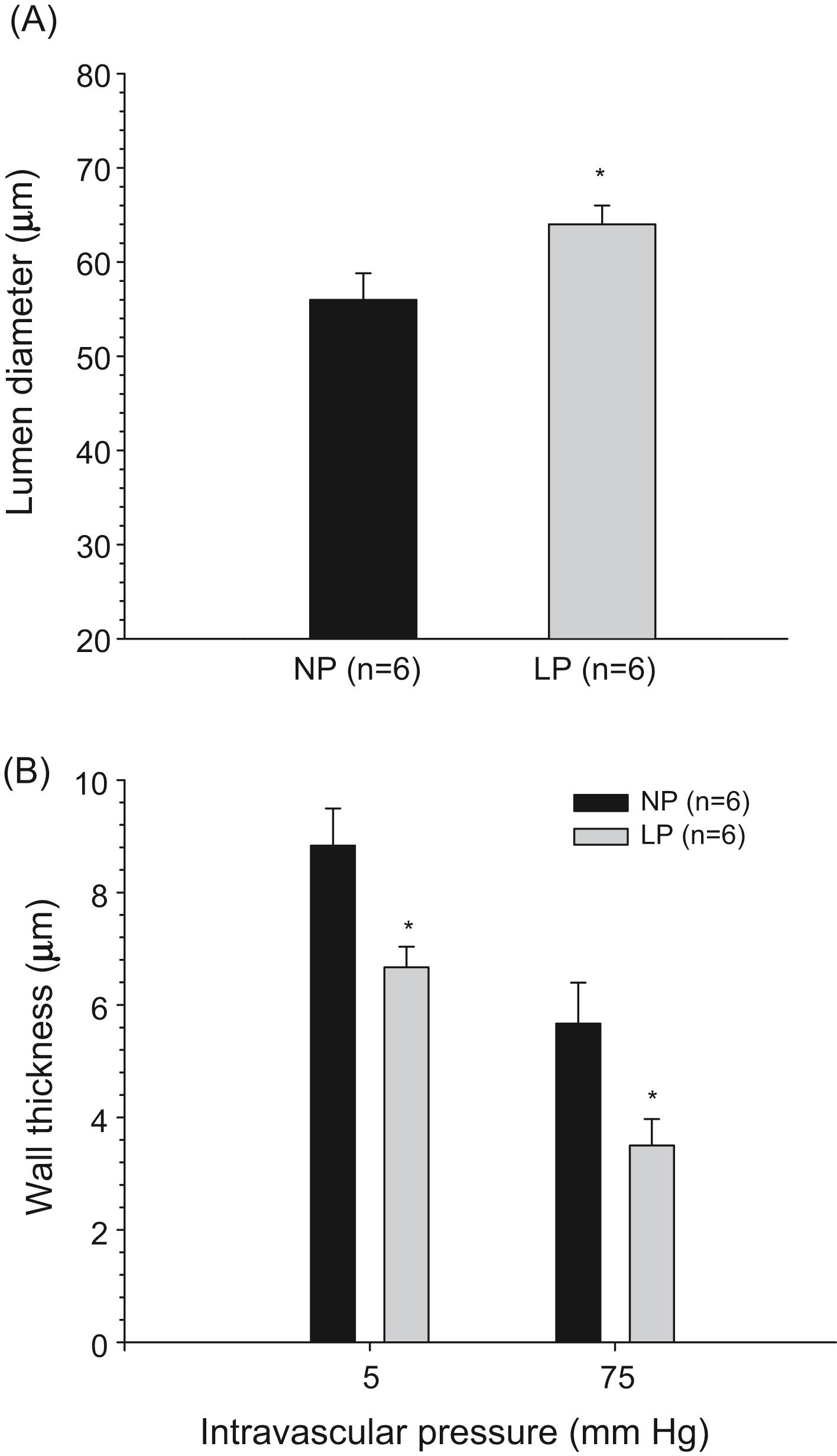
Although these changes in larger pial arteries may contribute to decreased cerebrovascular resistance and increased microvascular pressure noted in late-pregnant animals, the response of smaller parenchymal arterioles is a critical determinant of distal capillary pressure and a major determinant of BBB changes. Previous studies have shown that differences in resistance of small vessels in the brain parenchyma can account for regional differences in BBB permeability during acute hypertension. , Because late-pregnant animals developed edema in response to autoregulatory breakthrough and elevated hydrostatic pressure, it seems likely that reduced small-vessel resistance contributes to edema. In studies specifically examining brain parenchymal arterioles, vessels from late-pregnant animals were shown to have larger diameters compared with those from nonpregnant animals. Thus, there is a gestation-induced effect to cause outward remodeling of parenchymal arterioles ( Fig. 13.11A ). Subsequent studies showed that selective enlargement of brain parenchymal arterioles was due to relaxin-induced activation of the transcription factor peroxisome proliferator-activated receptor-gamma (PPARγ). Indeed, the activation of PPARγ is functionally repressed in preeclampsia. Although such structural changes may not influence resting CBF, they would have a significant impact on local hemodynamics under conditions when vessels are markedly dilated such as during breakthrough of autoregulation—and the resulting forced dilatation. Outward remodeling of parenchymal arterioles in the brain appears to be at the expense of the vascular wall, which becomes significantly thinner during pregnancy ( Fig. 13.11B ). Therefore, the significance of outward remodeling of cerebral arteries and arterioles during pregnancy may not be limited to decreased cerebrovascular resistance during acute hypertension, but may also predispose the brain to hemorrhage, another pathological finding of eclampsia, due to severely increased wall stress.
In 1949, McCall first described CBF changes in women with eclampsia using an inhalation technique of a gaseous mixture containing nitrogen, nitric oxide, and oxygen. Internal jugular arterial and venous blood was collected and the Fick principle applied by measuring serum concentrations. In eclamptic women, while CBF and the delivery of oxygen were normal, there was a 20% decrease in oxygen utilization. Other than these studies, there are none reported that used invasive methods to assess pregnancy-related CBF in humans. There are obvious major challenges encountered when assessing CBF in the human, since the most accurate methods are either invasive or require radioactive substances.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here