Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The aortic arch gives off, from right to left, the innominate, the left common carotid, and left subclavian arteries. The innominate artery passes beneath the left innominate vein before it divides into the right subclavian and the right common carotid arteries (CCA). The vertebral arteries come off the subclavian arteries 2 or 3 cm from the arch, but many variations may occur. The left CCA may arise from the innominate and crosses to a relatively normal position on the left side. The right vertebral artery may arise as part of a trifurcation of the brachiocephalic trunk into common carotid, subclavian, and vertebral arteries, and the left vertebral artery may arise directly from the aortic arch. Occasionally, an aberrant right subclavian artery may arise distal to the left subclavian artery from the aortic arch and crosses to the right side.
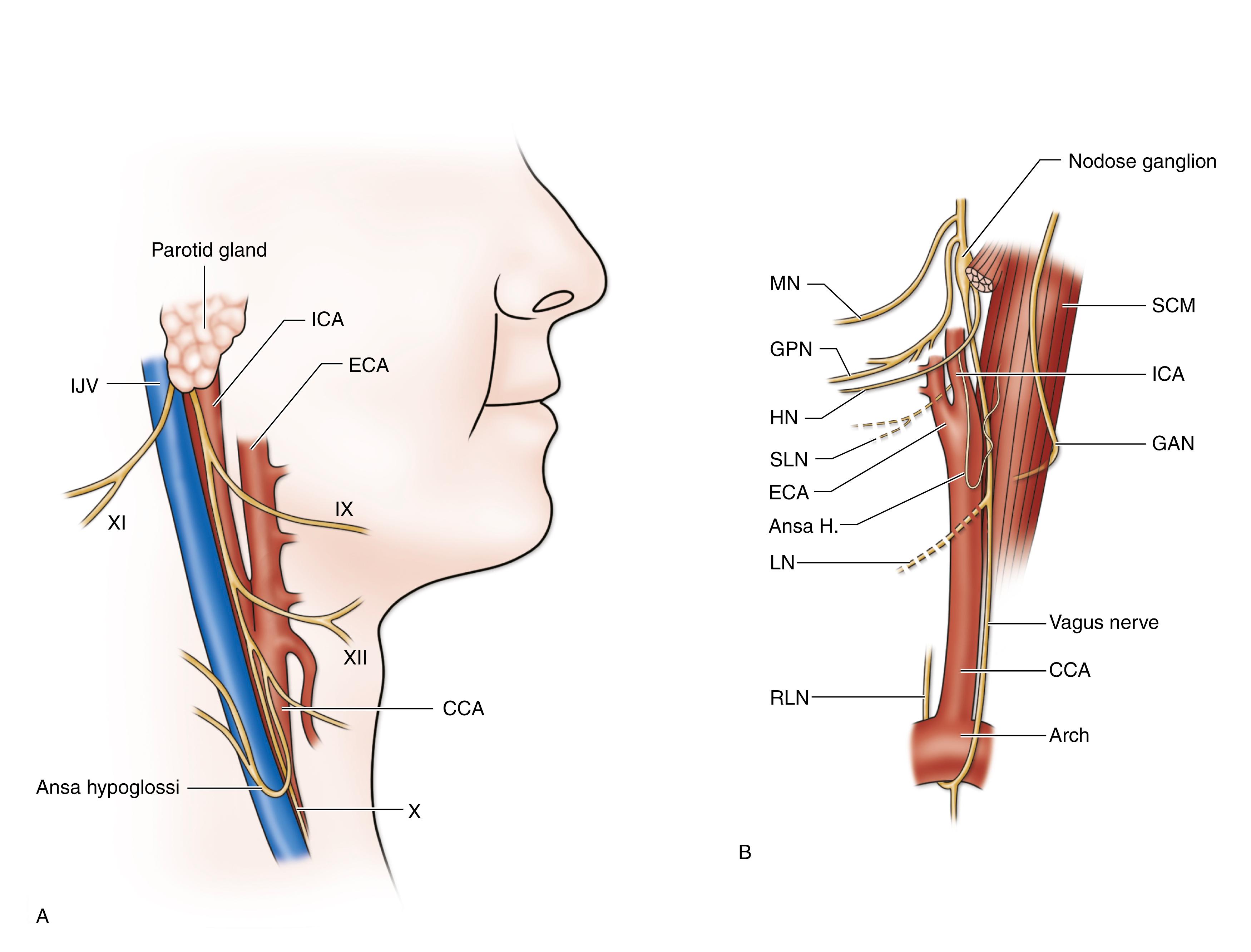
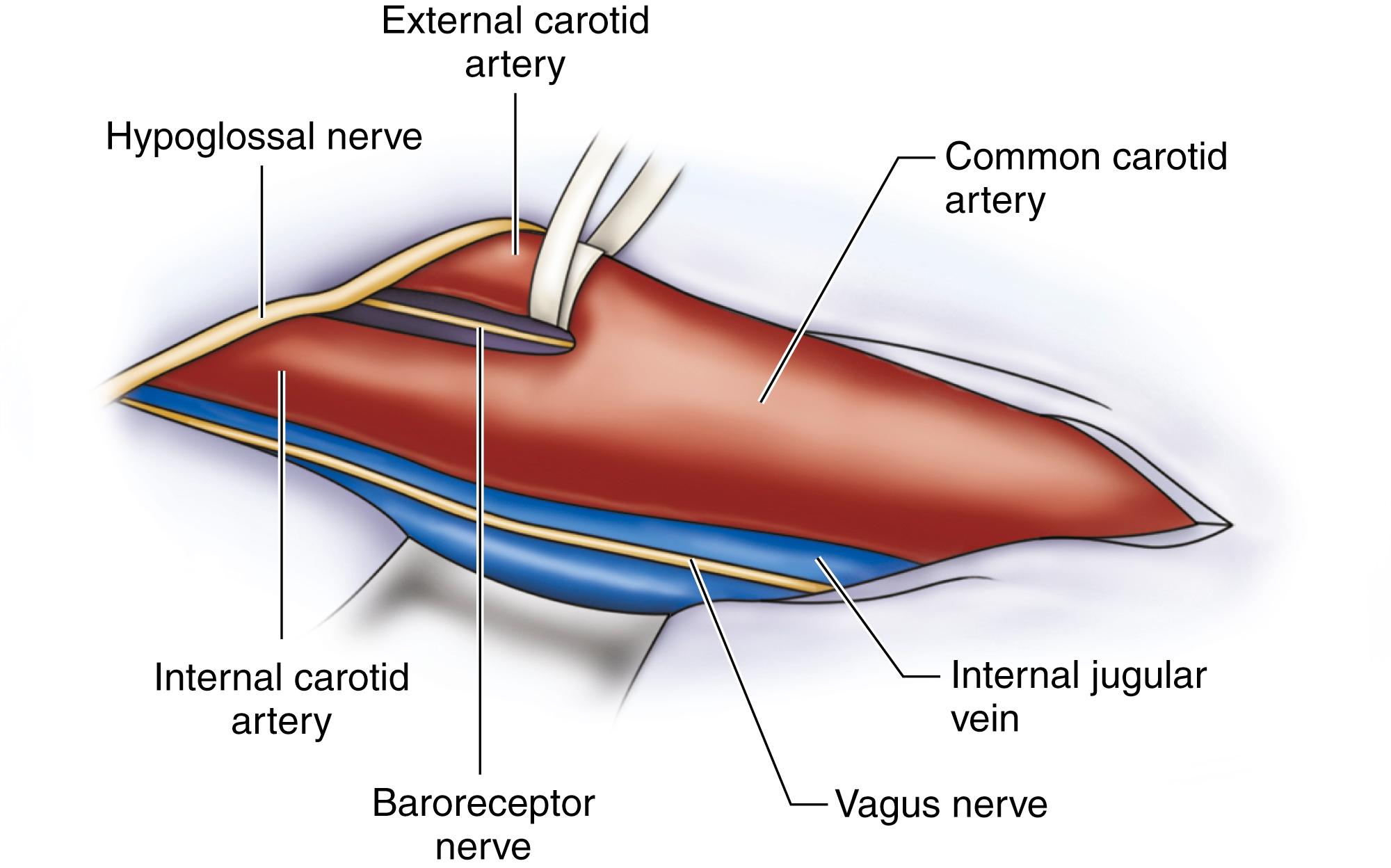
The CCAs on each side travel in the carotid sheath up to the neck before dividing into external carotid (ECA) and internal carotid arteries (ICA) just below the level of the mandible. Important branches of the ECA include the superior thyroid, which may arise from the CCA; the ascending pharyngeal, which is important in that it accompanies the superior laryngeal nerve; the lingual and occipital arteries that have a close association with the hypoglossal nerve. No branches of the ICA occur in the neck.
The carotid sinus is a baroreceptor located in the crotch of the carotid bifurcation. It is innervated by the sinus nerve of Hering (branch from the glossopharyngeal nerve). The carotid body is a very small structure lying in the crotch of the bifurcation and functions as a chemoreceptor, responding to low oxygen or high carbon dioxide levels in the blood. It is also innervated by the sinus nerve of Hering.
Most patients undergoing CEA receive general anesthesia with intra-arterial pressure monitoring. Although some surgeons prefer local or cervical block anesthesia, general anesthesia has the advantage of increasing cerebral blood flow and reducing several metabolic demands. Endotracheal intubation provides good airway control and reduces physician and patient anxiety. Nasotracheal intubation can be utilized to facilitate exposure for high carotid stenosis or in patients undergoing reoperation (see Ch. 93 , Carotid Endarterectomy).
The patient should be positioned supine, with the head averted from the operative side and slightly extended by placing a small roll behind the shoulder blades transversely. The bed should also be placed slightly in a reverse Trendelenburg position to decompress the surrounding venous structures. Both arms can be tucked to allow for the surgeon and assistant to stand across from each other or with one at the head of the bed and one at the side of the involved vessel, depending on surgeon preference. The area to be prepped should include the jawline and the inferior aspect of the ear to below the clavicle. If regional anesthesia is being performed, this is done prior to prepping and draping. It is also advantageous to place a small squeeze toy in the contralateral hand to allow for neurologic assessment throughout the procedure. This allows the patient to demonstrate function of that limb when regional blocks are being utilized.
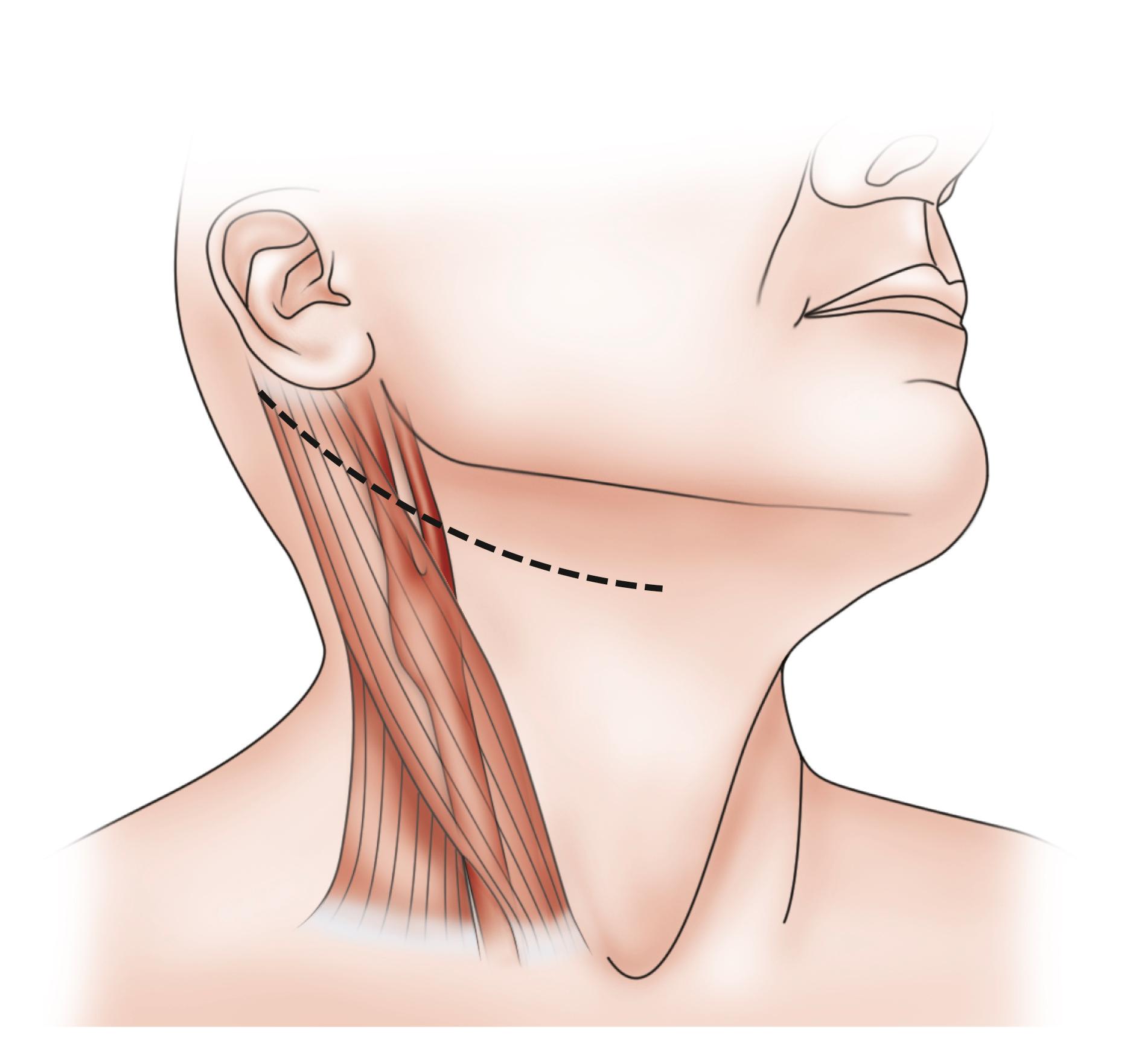
The cervical vertical incision is made parallel and somewhat anterior to the sternocleidomastoid muscle and centered over the carotid bifurcation ( Fig. 57.1 ). This can be extended proximally to the sternal notch for more proximal CCA lesions, and distally to the mastoid process for higher exposure. The upper end of the incision should be angled posterior to the earlobe, if needed, to avoid the parotid gland.
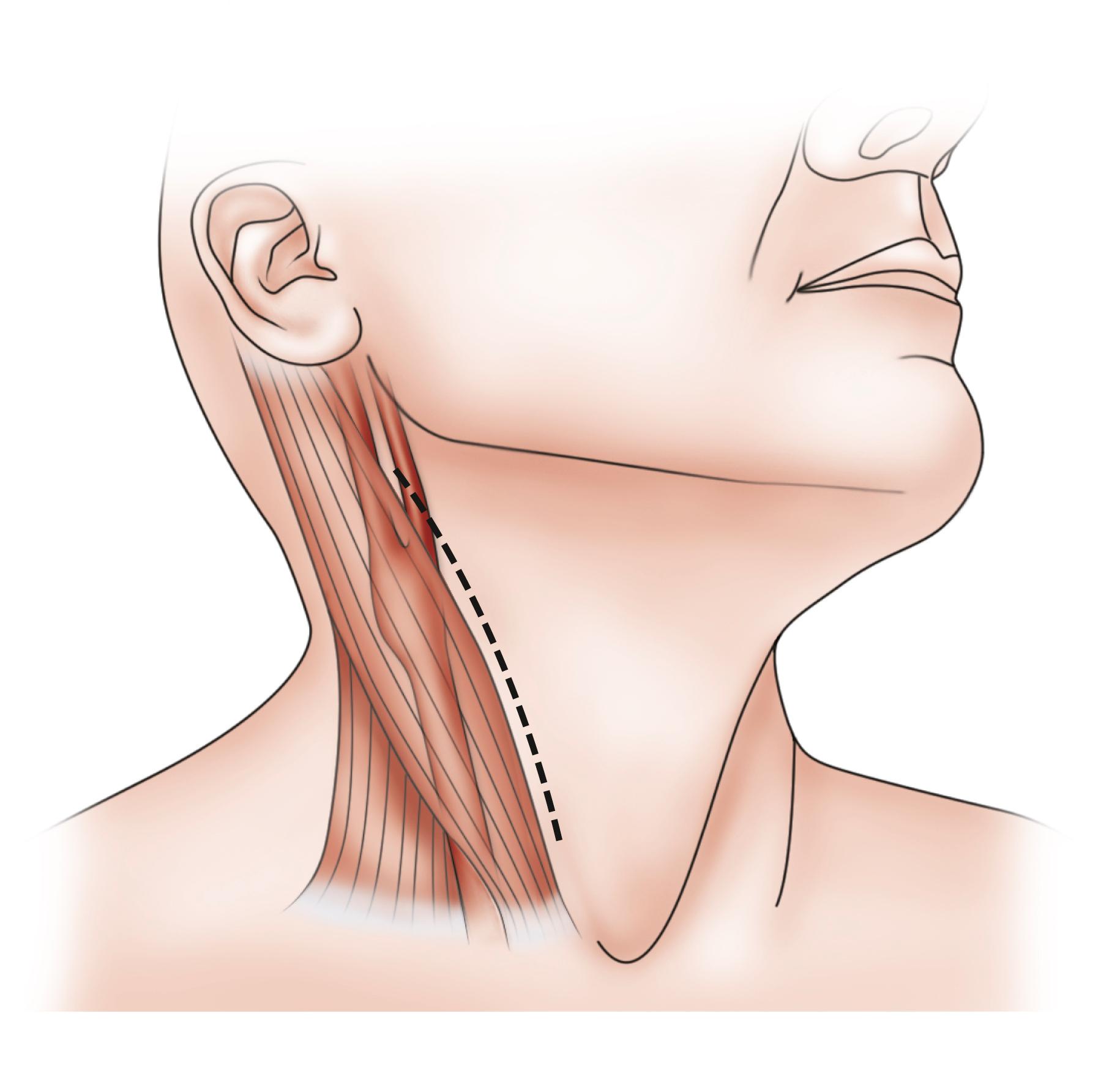
An alternative incision placed obliquely in the skin crease over the carotid bifurcation can be used ( Fig. 57.2 ). This incision has the advantage of a more cosmetically acceptable scar than the vertical incision, but has the following limitations: more difficult to gain additional proximal/distal arterial exposure and the necessity of raising skin flaps.
Dissection is continued through platysma, typically with electrocautery. The external jugular vein frequently has to be divided. Several small nerves of the superficial cervical plexus may have to be divided, which may lead to areas of hypoesthesia around the incision. The great auricular nerve may be visualized when the incision is high. The nerve should be protected if possible; if divided, it results in numbness to the ear lobe, which usually regresses within a few months. Care should be taken at the angle of the mandible to remain lateral to avoid dissection into the parotid gland. The dissection is continued through the tissues along the medial border of the sternocleidomastoid until the carotid sheath is encountered. The CCA is generally mobilized for a sufficient length proximal to the carotid lesion. More proximal control of the CCA can be obtained by division of the omohyoid muscle, and ligation of the associated vessels. Dissection is continued upward to isolate the ECA. The ICA is mobilized to a point where the vessel is completely normal. It may be necessary to inject a local anesthetic in the area of the carotid bifurcation to block the nerve to the carotid body to prevent reflex bradycardia. During the dissection, a small sternomastoid branch of the superior thyroid artery usually has to be ligated; other small perforating vessels supplying the SCM can be divided with cautery. At this point one must avoid injury to the accessory nerve, which can be found at the superior aspect of the incision. Once the sternocleidomastoid has been retracted laterally, a Weitlaner or Henle retractor should be utilized to hold the tissues in place. If regional block is utilized, it is occasionally necessary to supplement with additional lidocaine at the carotid sheath.
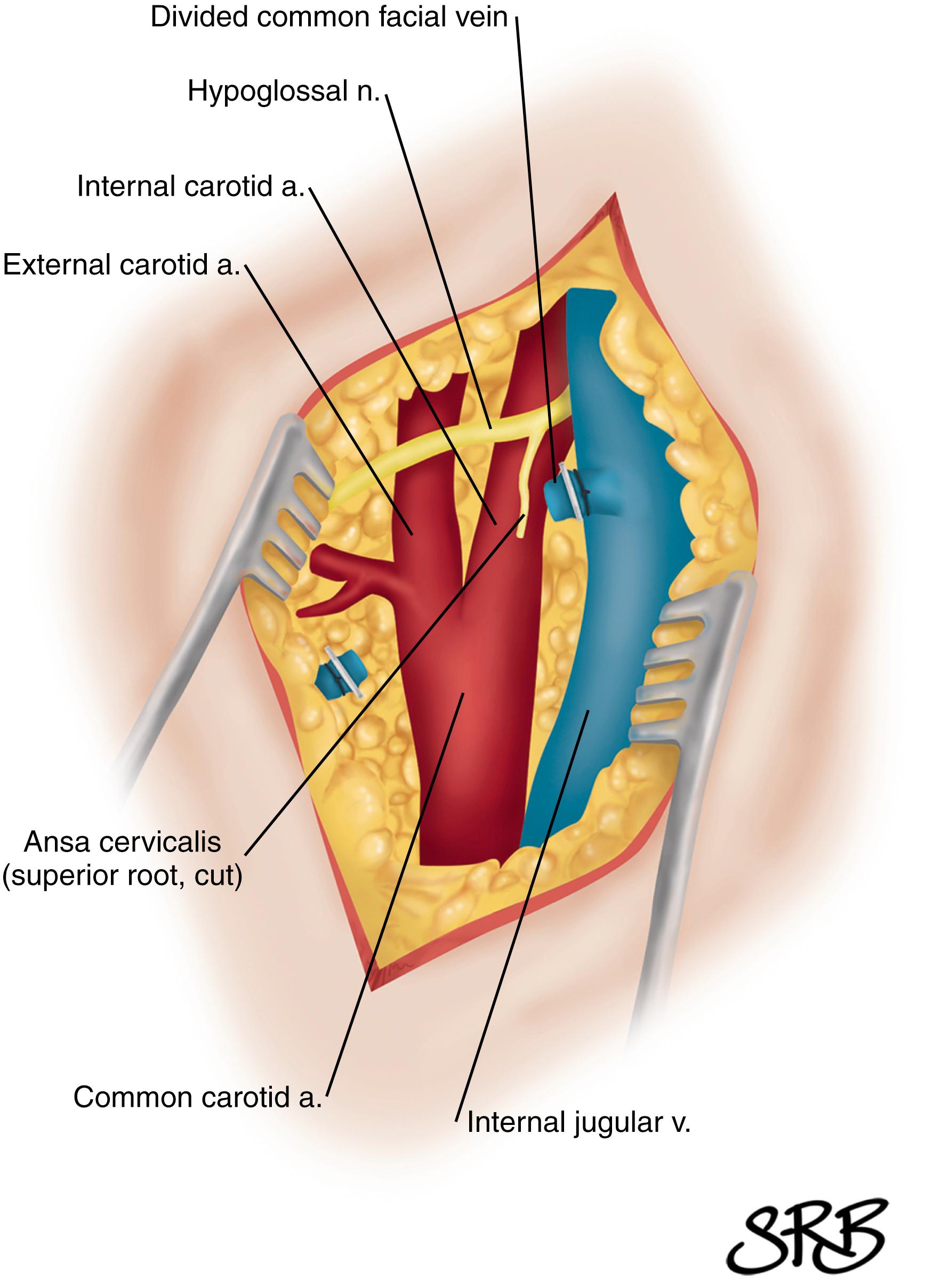
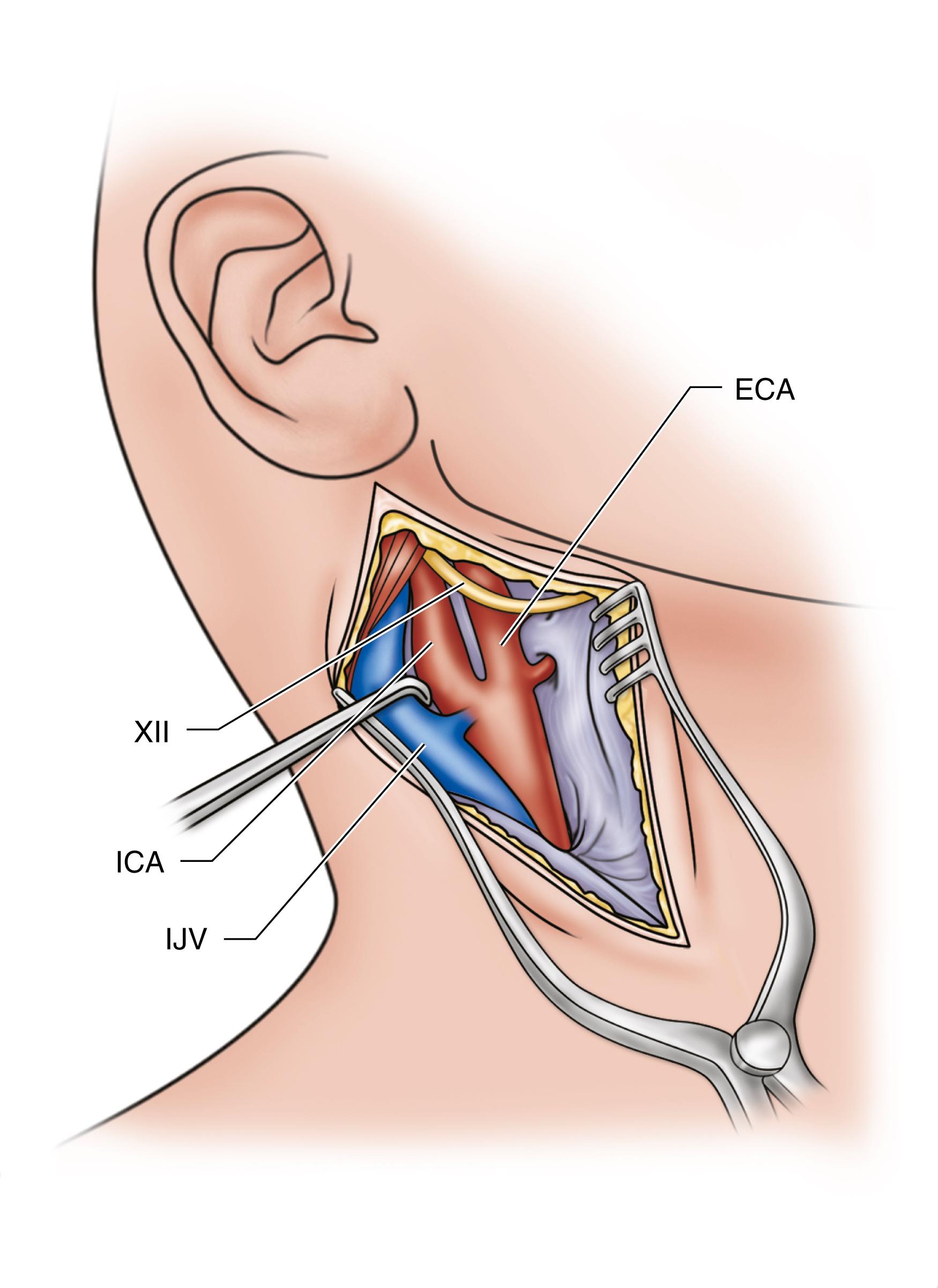
The internal jugular vein is dissected along the medial border and retracted posteriorly. This maneuver requires division of the common facial vein ( Fig. 57.3 ). Since the anatomy of the venous structures is quite variable, there may be a single vein or, alternately, two or three veins separately joining the internal jugular vein, in which case they must be separately ligated and divided. The connective tissue between the facial vein and the digastric muscle is rich in lymph nodes, which can be dissected from the vein and, if necessary, divided with cautery.
Dissection should stay anterior to the CCA to avoid injury to the vagus nerve, which usually lies in the posterior lateral position within the carotid sheath but occasionally may spiral anteriorly, particularly in the lower end of the incision. Attention should be paid to various cranial nerves, including IX, X, XI, and XII, the marginal mandibular branch of VII, and the rare nonrecurrent laryngeal nerve that comes directly off the vagus on the way to innervate the vocal cord. This nerve can cross anterior to the carotid artery and be mistaken for a part of the ansa hypoglossi, resulting in cord paralysis. This anomaly is most often noted on the right side of the neck ( Fig. 57.4 ). The vagus nerve may be closely adherent to the carotid bulb, and it becomes nearly confluent with the hypoglossal nerve near the styloid process. The hypoglossal nerve is often surrounded by small veins that should be ligated carefully. The hypoglossal nerve may be injured by retraction; therefore, the structures that tether it in place, such as the artery and vein to the sternocleidomastoid muscle, the descending hypoglossal branch of the ansa cervicalis, and the occipital artery may require division to mobilize the nerve for distal ICA exposure. Careful attention should also be given to the superior laryngeal nerve, which is usually located medial to the ICA. The superior laryngeal nerve divides into external and internal branches that pass posterior to the superior thyroid artery, and it may be harmed while controlling either of these two vessels. The glossopharyngeal nerve crosses the ICA near the base of the skull and is best protected by maintaining dissection very close to the anterior surface of the ICA. Excessive or prolonged retraction of the upper aspect of the incision may cause temporary compression injuries laterally to the greater auricular nerve or medially to the marginal mandibular branch of the facial nerve. Once exposure has been completed, the CCA, ECA, and the ICA are controlled using silastic loops ( Figs. 57.5 and 57.6 ).
With the standard approach, when bleeding occurs postoperatively, it is frequently venous, specifically related to the facial vein. The ICA is located more posteriorly with this approach, and it may be difficult to access more distal disease. The vagus nerve is also not well visualized during the standard approach, which can lead to clamp injuries. With the retrojugular approach, the ICA is anterior. Visualization of the external carotid artery (ECA) is slightly more limited, but the origin and superior thyroidal arteries are easily identified and controlled, with markedly better visualization of the ICA. There is no need for ligation or division of major venous structures, thus decreasing the potential for postoperative bleeding, and the ansa hypoglossi is also not divided.
Skin incision and initial approach are identical to the standard exposure. Once the sternocleidomastoid has been retracted and the carotid sheath exposed, the dissection diverges from the standard approach.
The sheath overlying the vessels is divided at the lateral border of the internal jugular vein. Once fully dissected, the vein is then retracted medially, using a blunt Weitlaner. Occasionally there may be small venous branches posteriorly that require ligation and division. The vagus nerve is visualized and left lateral to the carotid artery. This approach avoids division of the facial vein, ansa cervicalis, and the vascular bundle associated with the hypoglossal nerve, as all of these structures are retracted medially with the jugular vein. This approach allows greater visualization of the internal carotid artery ( Fig. 57.7 ).
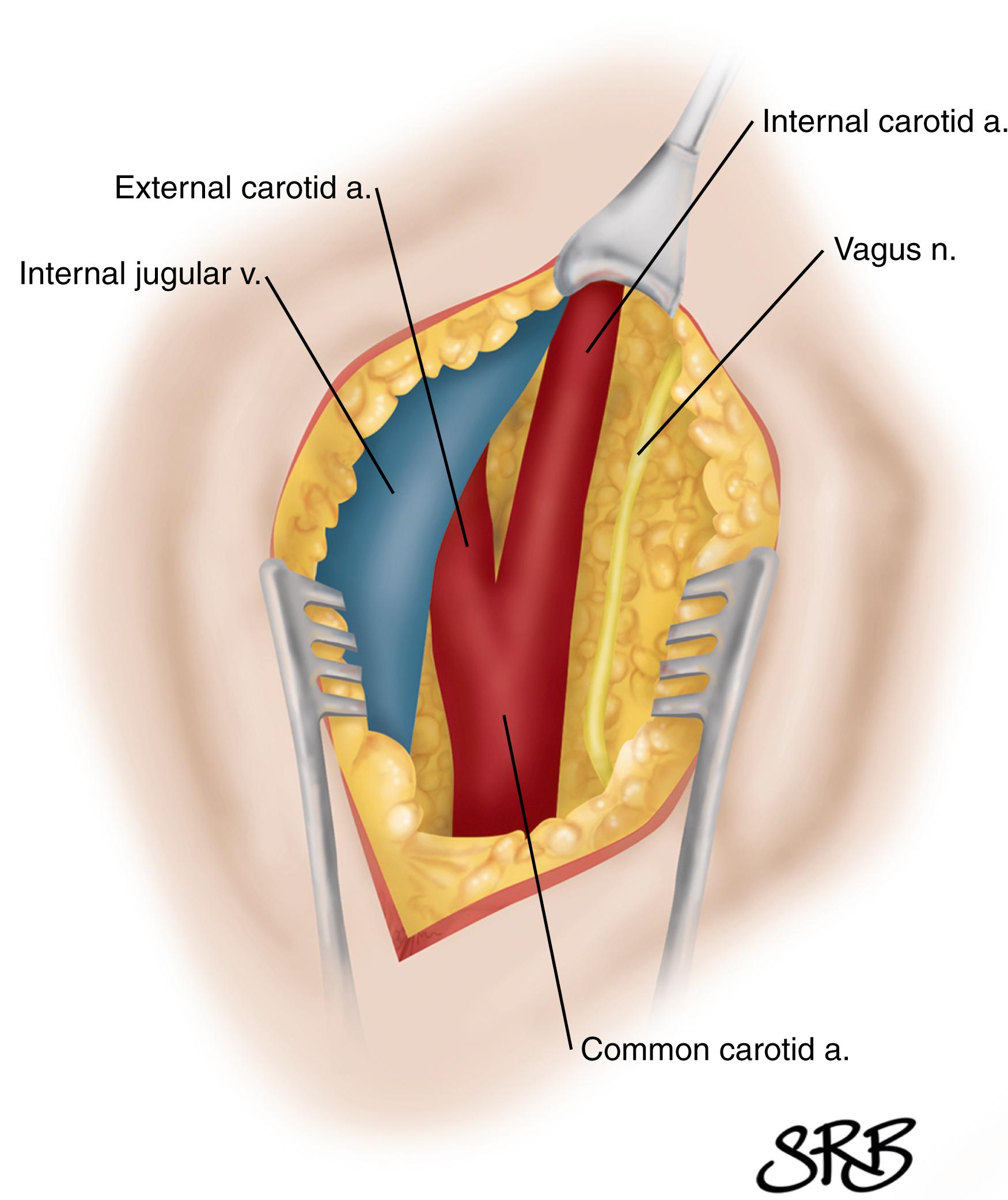
At this point, the dissection is the same as for the standard carotid approach, with mobilization of the ICA, ECA, and common carotid artery (CCA) for isolation (using silastic loops) as well as the superior thyroid artery. However, the vagus nerve has already been identified laterally and does not fall into the area of concern when encircling the CCA.
Carotid endarterectomy (CEA) is then performed in either standard fashion or with the eversion technique.
At completion of the procedure, after hemostasis has been verified, the jugular vein is allowed to return to its normal location, lateral to the artery, and the wound is closed in the standard fashion with reapproximation of the platysma and subcuticular skin closure.
Most vascular surgeons are not familiar with this approach. This technique has been described by Berguer. It allows exposure of the ICA, medial to the sternocleidomastoid, between the hypoglossal and vagus nerves.
The patient is placed prone/lateral with the contralateral arm placed under the head.
The incision is initially transverse, beginning at the occipital protuberance and extending to the mastoid process, where it is curved downward along the posterior border of the SCM for 2 to 3 cm.
The fibers of the trapezius, splenius capitis, semispinalis capitis, and longissimus capitis muscles are divided.
The greater occipital nerve, which is a dorsal ramus of C2 and courses over the semispinalis capitis muscle, may have to be divided.
At this point the internal jugular vein, carotid artery, and the accessory nerve are exposed.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here