Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Cerebral cavernous malformations (CCMs) are vascular lesions that contain a compact bundle of pathologic capillary vessels without intervening brain parenchyma. CCMs are relatively common, affecting approximately 1 in every 200 individuals and accounting for 8% to 15% of all vascular malformations of the central nervous system (CNS). The majority of lesions occur in the brain, with most being located in the supratentorial compartment and the minority infratentorially, to include the brainstem. Approximately 3% to 5% are discovered as intramedullary spinal CCM.
Despite the high prevalence of CCM, most lesions are asymptomatic, being discovered incidentally, if ever. Only 20% to 30% of CCM patients are symptomatic during their lifetimes, presenting to medical attention most commonly during their third to fifth decades of life with symptoms such as headaches, seizures, and focal neurologic deficits due to lesion expansion following events such as thromboses and hemorrhages.
Cavernous malformations can be either familial or sporadic. The familial form of the disease often manifests as multiple lesions in the setting of a family history of neurologic disease. In the sporadic form, patients rarely have more than two lesions, and family history is typically absent. Mutations in three genes, CCM1 , CCM2 , and CCM3 , have been discovered as being responsible for the familial disease, accounting for 96% of all mutations. De novo occurrence of lesions can occur and may impact long-term outcome.
Complete surgical resection of CCM is the only management strategy that is curative. Medical management is limited to seizure control and symptomatic relief of headaches. The indication for radiosurgery treatment is controversial. In contrast, successful lesion resection immediately eliminates a patient's hemorrhage risk, but up to 80% of patients achieve seizure control postoperatively. The main goal in managing CCM is to balance the risks of surgery with those of the natural history of the disease. Because both of these factors vary significantly, each CCM patient must be considered on an individual basis.
The most serious complication of CCM natural history is intracerebral hemorrhage. Patients with posterior fossa cavernomas are reported to be 6.75 times more likely to present with a bleed, and the rehemorrhage rate is higher than that for lesions in other locations. Not only were these repeat hemorrhages common, but brainstem cavernomas can result in debilitating deficits due to the high density of critical tracts and nuclei in this region.
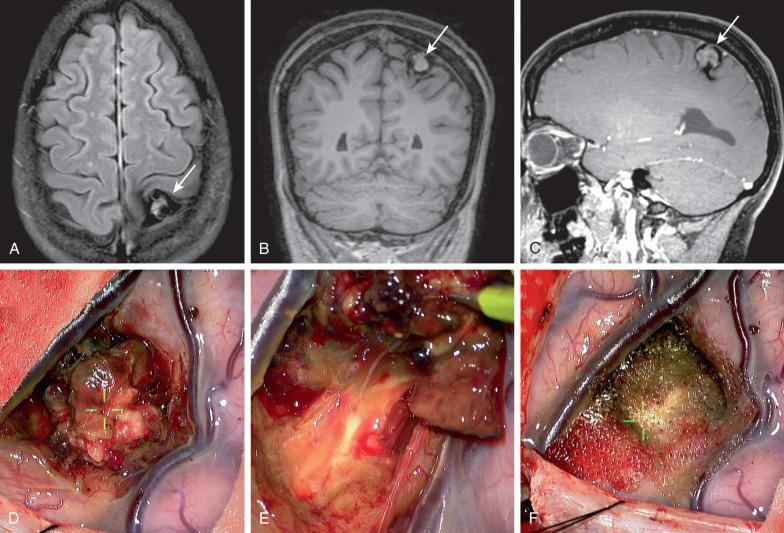
As a result of devastating outcomes with untreated cavernomas in high-risk regions, surgical treatment must always be considered for these select patients. Four major criteria assist in determining which patients with infratentorial lesions are appropriate surgical candidates: those with (1) lesions that rise to the pial surface based on T1-weighted MRI, (2) lesions with repeated hemorrhages causing progressive neurologic deficits, (3) lesions with acute hemorrhage extending outside the lesion capsule, and (4) significant mass effect produced with a large intralesional hemorrhage. Surgery is considered only when total resection can be achieved, because lesion remnants can grow and hemorrhage as well.
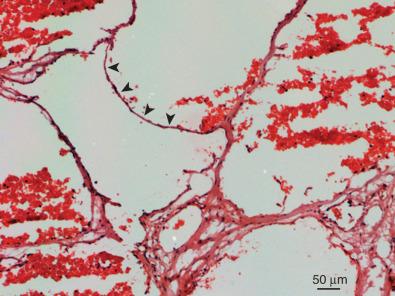
Cerebral cavernous malformations (CCMs), or cavernomas, are low-flow vascular lesions consisting of clusters of dilated, thin-walled vascular channels lacking intervening neural parenchyma. They typically range in size from 1 mm to several centimeters and can be found anywhere in the central nervous system (CNS) as well as in other organs such as the skin and eye. Histologically, the lesions are composed of a single layer of endothelial cells and lack structural elements found in mature vessels, including smooth muscle and elastin ( Fig. 21.1 ). Other elements usually found in the blood-brain barrier, including astrocytic foot processes and pericytes, are also diminished or completely absent. Macroscopically, the lesions appear reddish purple. They are often multilobulated and can be encapsulated by a variable layer of fibrous adventitia, giving them their characteristic mulberry-like appearance. Given a lack of tight junctions in cavernomas walls, they tend to be leaky, resulting in hemorrhages with blood products of various ages.
Cavernous malformations can be either familial or sporadic. The familial form of the disease usually manifests as multiple lesions in the setting of a family history of neurologic disease ( Fig. 21.2 ). In the sporadic form, patients rarely have more than two lesions, and family history is typically absent. Mutations in three genes, CCM1 , CCM2 , and CCM3 , have been discovered as being responsible for the familial disease, accounting for 96% of all mutations.
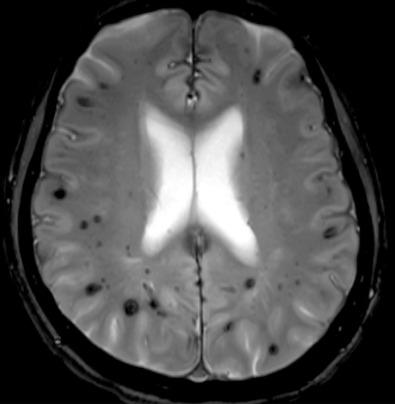
Radiographically CCMs are best detected on magnetic resonance imaging (MRI), where they appear as a mixture of high and low T1 and T2 signal intensity surrounded by hemoglobin degradation products. These different components give lesions a characteristic popcorn appearance, with a surrounding hemosiderin ring due to chronic bleeds, that appears hypointense both on T1- and T2-weighted imaging. Axial T2 gradient echo or susceptibility weighted images are most sensitive in identifying cavernous lesions but possess a significant blooming artifact due to blood products ( Figs. 21.2 and 21.3 ). Because computed tomography (CT) findings for cavernomas are nonspecific, this imaging modality is less useful for detection. Angiography is similarly of little diagnostic help because lesions are usually angiographically occult. After a hemorrhage, however, developmental venous anomalies (DVAs) can be detected on angiography and should alert the clinician to a concomitant cavernoma, which frequently coexists with DVAs.
CCMs are relatively common, affecting approximately 1 in every 200 individuals and accounting for 8% to 15% of all vascular malformations of the CNS. The majority of lesions occurs in the brain, with 63% to 90% of these being located in the supratentorial compartment and 7.8% to 35.8% infratentorially. Between 9% and 35% of infratentorial lesions are located in the brainstem.
Despite the high prevalence of CCM, most lesions are asymptomatic, being discovered incidentally, if ever. Only 20% to 30% of CCM patients are symptomatic during their lifetimes, presenting to medical attention most commonly during their third to fifth decades of life with symptoms such as headaches, seizures, and focal neurologic deficits due to lesion expansion following such events as thromboses and hemorrhages. Asymptomatic patients also occasionally present to health care providers after having one or multiple CCMs detected incidentally on imaging studies obtained for other purposes. Given this highly variable presentation and disease progression in patients with CCM, choosing the appropriate management strategy can be challenging. This chapter explores the different treatment options available for CCM and provides suggestions as to the appropriate management in different circumstances. Before doing so, however, the natural history of these lesions will be discussed, as sound understanding of the natural history of the disease is paramount in any decision-making process with regard to treatment.
The natural history of CCM can vary widely among patients. Although once believed to be congenital, it is now recognized that CCM can also occur de novo. Once present, these lesions are dynamic, expanding as lesions thrombose and hemorrhage, and regressing as they recanalize and as blood products from hemorrhages are resorbed. The most common symptom reported in CCM patients is seizures, which are especially common with frontal or temporal lobe lesions. Cavernoma lesions are typically surrounded by reactive gliosis, which, at least in certain cases, is thought to serve as an epileptogenic focus. The estimated annual seizure risk is approximately 1% to 2%, and in patients with supratentorial lesions several seizure types including simple, complex partial, and generalized have been reported.
Gross apoplectic hemorrhages are the most severe presentation of CCM. Because cavernomas are low-flow, low-pressure lesions, most bleeds are relatively small and result from blood extravasation from the leaky vascular channels of the lesion. Larger bleeds can and do occur, though, with an annual hemorrhage risk ranging between 0.25% and 6% depending on a variety of factors. Larger and deeper lesions have been reported to have an increased bleeding risk, as do lesions in older patients, pregnant patients, and patients who have suffered a previous bleed. Rehemorrhage could be as high as 30% especially with infratentorial and brainstem lesions. Asymptomatic patients or those presenting with seizures typically have the lowest risk, which usually ranges from 0.4% to 2% annually. Symptoms from a hemorrhage are typically maximal at the time of the bleed and gradually improve as the hemorrhage undergoes organization and resorption. With repeat hemorrhages, however, neurologic deficits often worsen, and the risk that such deficits will become permanent increases. Progressive neurologic deficits are usually the most common presenting symptom of infratentorial CCM. Because this region has a higher density of eloquent neural structures compared to supratentorial regions, lesions here usually become symptomatic at smaller sizes.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here