Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Cartilage and bone are both specialized connective tissues that function in supporting parts of the body. The former has a firm pliable matrix that resists mechanical stresses; the latter is one of the hardest tissues of the body, and protects vital organs such as the brain, spinal cord, bone marrow, and heart. Both cartilage and bone have cells that are specialized to secrete the matrix in which the very same cells become trapped. Most cartilage and all bones are surrounded by a connective tissue capsule, the perichondrium and the periosteum , respectively.
Cells of cartilage, known as chondrocytes , occupy small cavities called lacunae within the cartilage extracellular matrix ( ECM ). Cartilage is avascular, has no nerve supply, and does not have lymphatic vessels. Chondrocytes receive oxygen and nourishment from blood vessels of the perichondrium by diffusion through the ECM, which is composed of glycosaminoglycans (GAGs) and proteoglycans that are intimately associated with the collagen and elastic fibers embedded within the matrix. The flexibility and resistance of cartilage to compression permit it to function as a shock absorber, and its smooth surface permits almost friction-free movement of the joints of the body as it covers the articulating surfaces of the bones.
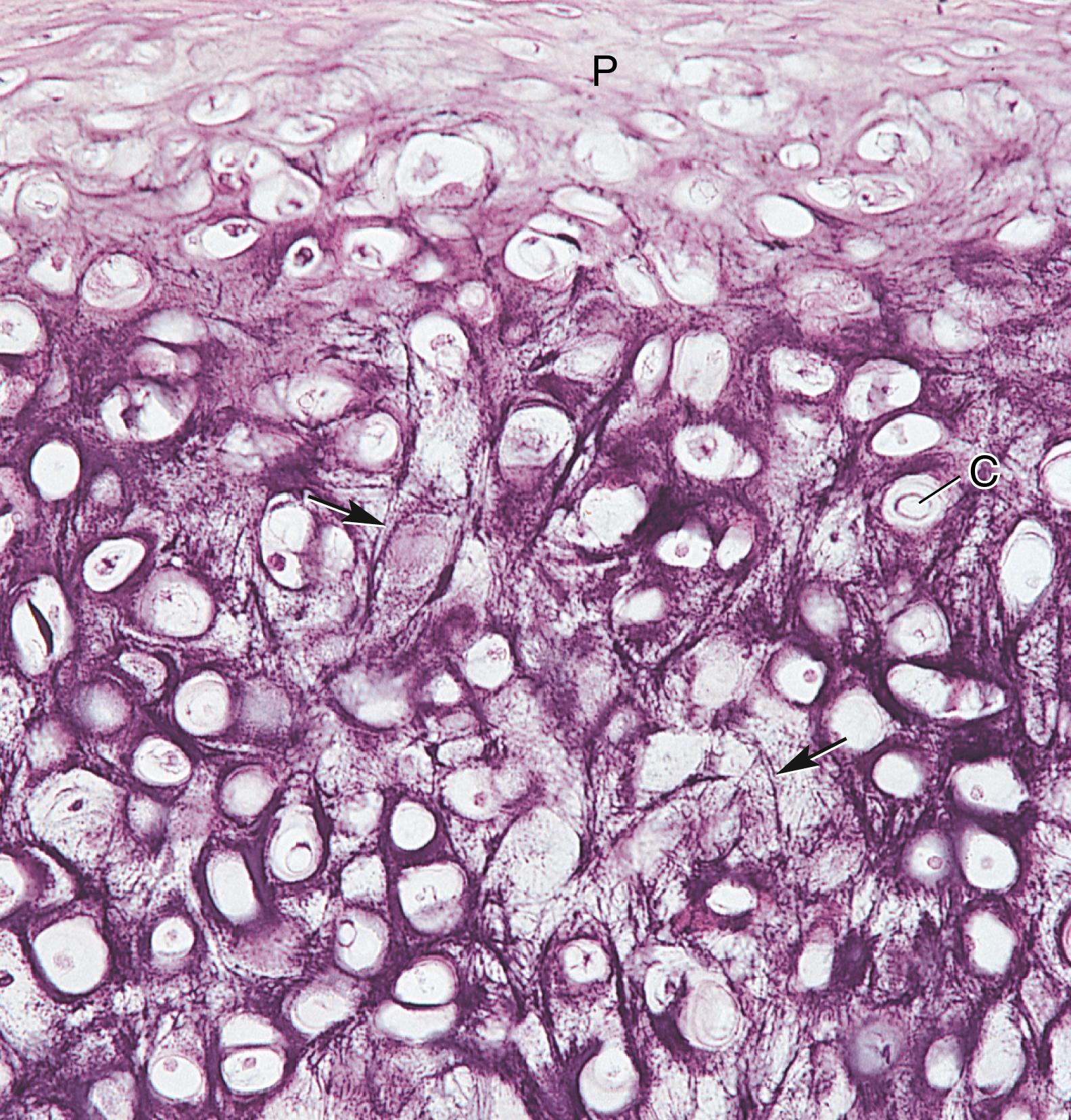
There are three types of cartilage, based on the types of fibers present in the matrix ( Fig. 7.1 and Table 7.1 ). Hyaline cartilage contains type II collagen fibers in its matrix; it is the most abundant cartilage in the body. Elastic cartilage contains, in addition to the type II collagen fibers, an abundance of elastic fibers scattered throughout its matrix, giving it more pliability. Fibrocartilage possesses dense, coarse type I collagen fibers in its matrix, which aids it in withstanding tensile forces.
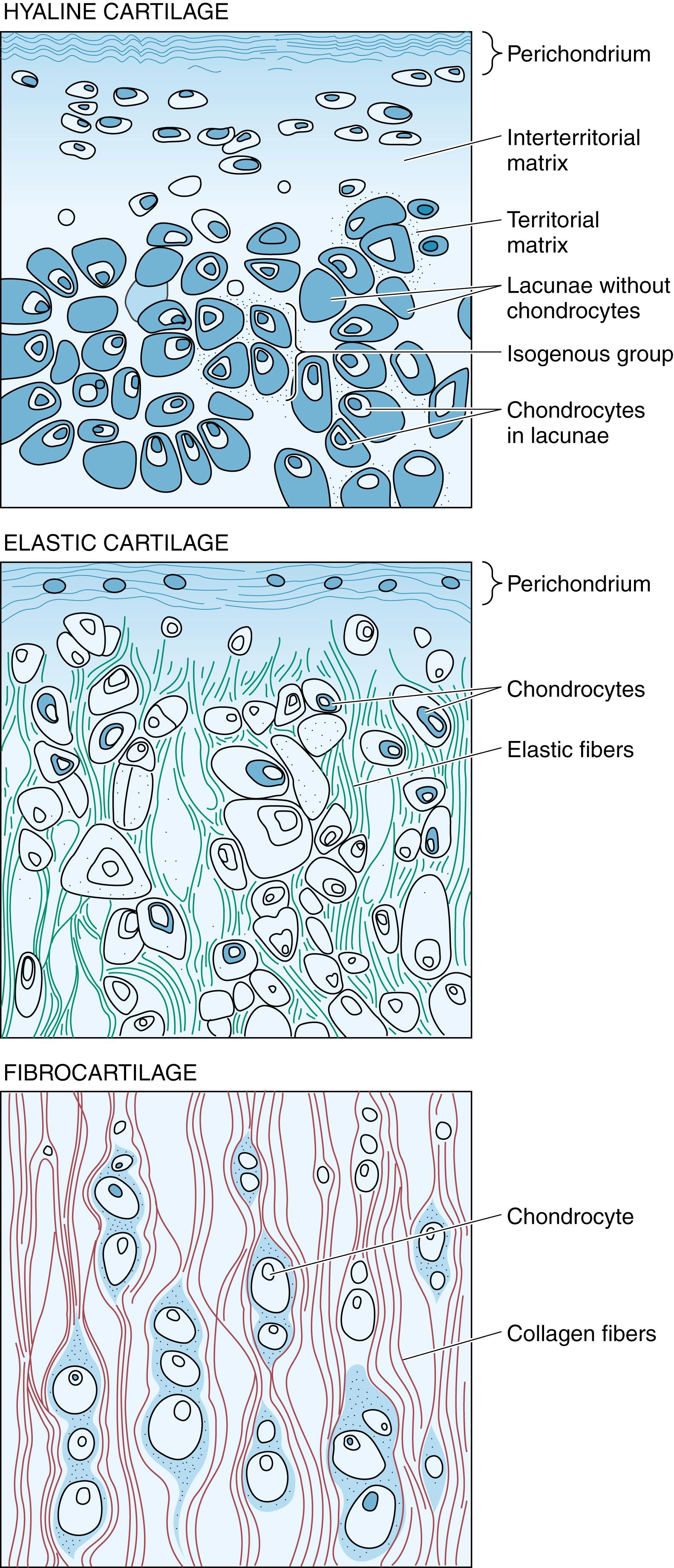
| Type of Cartilage | Identifying Characteristics | Perichondrium | Location |
|---|---|---|---|
| Hyaline | Type II collagen, basophilic matrix, chondrocytes usually arranged in groups | Perichondrium present in most places. Exceptions: articular cartilages and epiphyses | Articular ends of long bones, nose, larynx, trachea, bronchi, ventral ends of ribs |
| Elastic | Type II collagen, elastic fibers | Perichondrium present | Pinna of ear, walls of auditory canal, auditory tube, epiglottis, cuneiform cartilage of larynx |
| Fibrocartilage | Type I collagen, acidophilic matrix, chondrocytes arranged in parallel rows between bundles of collagen, always associated with dense, regular collagenous connective tissue or hyaline cartilage | Perichondrium absent | Intervertebral disks, articular disks, pubic symphysis, insertion of some tendons |
Hyaline cartilage, the most abundant cartilage in the body, forms the template for endochondral bone formation.
Hyaline cartilage , a semitranslucent, bluish-gray, pliable substance, is the most abundant cartilage of the body. It is located in the nose and larynx, on the ventral ends of the ribs where they articulate with the sternum, in the tracheal rings and bronchi, and on the articulating surfaces of the movable joints of the body. It is hyaline cartilage that forms the cartilaginous template of long bones during embryonic development and constitutes the epiphyseal plates of growing long bones (see Table 7.1 ).
Cells responsible for hyaline cartilage formation differentiate from mesenchymal cells.
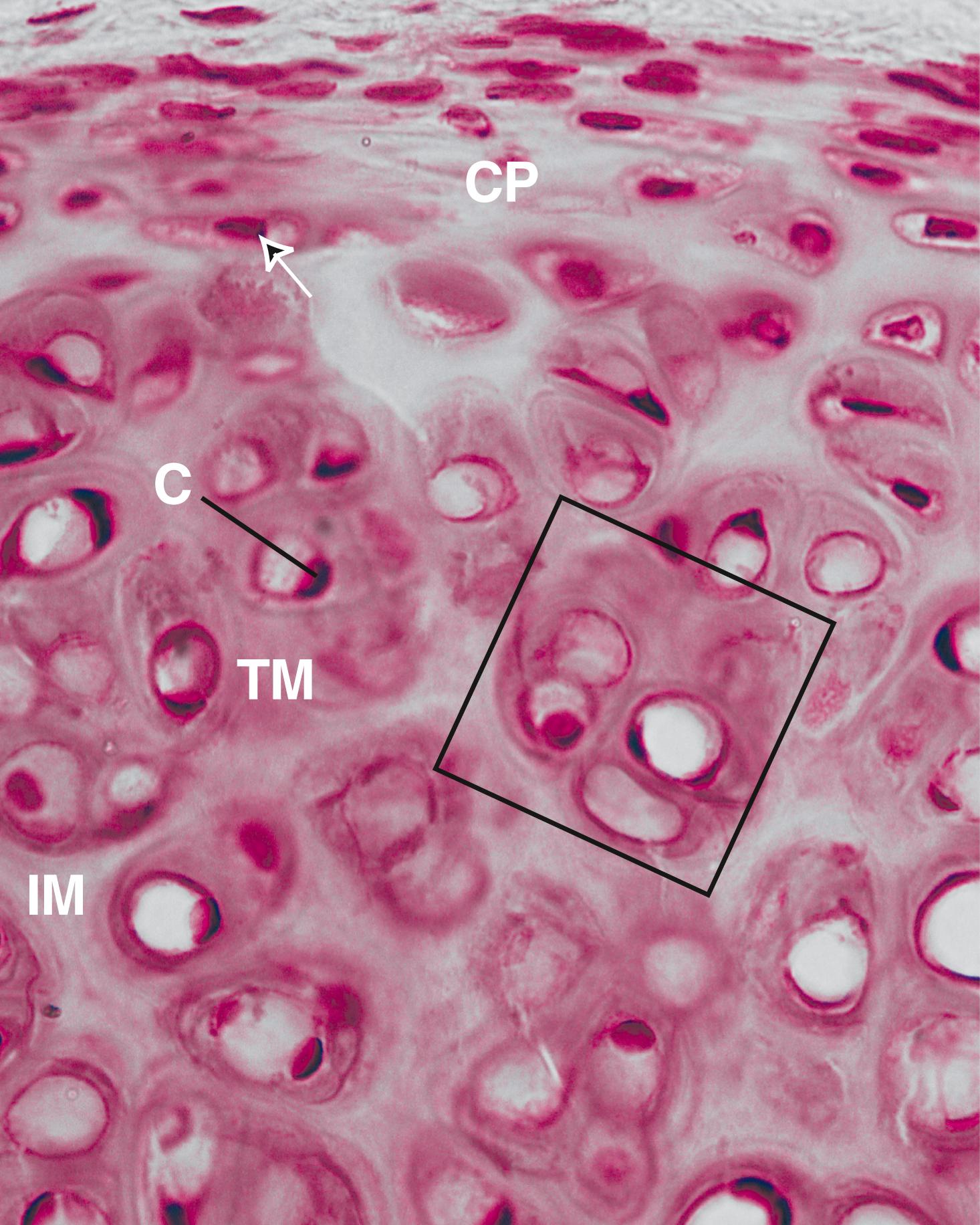
In the region where cartilage is to form, individual mesenchymal cells retract their processes and congregate in cell clusters to form chondrification centers . Under the influence of a small molecule called kartogenin , cells in the chondrification centers differentiate into chondroblasts and secrete cartilage matrix, entrapping themselves within small individual compartments called lacunae . Once surrounded by this matrix, these cells are known as chondrocytes ( Figs. 7.2 to 7.4 ). These cells are still capable of cell division, forming a cluster of two to four or more cells in a lacuna. These groups are known as isogenous groups and represent one, two, or more cell divisions from an original chondrocyte (see Fig. 7.1 ). As the cells of an isogenous group manufacture matrix, they are pushed away from each other, forming separate lacunae and, thus, enlarging the cartilage from within. This type of growth is called interstitial growth .
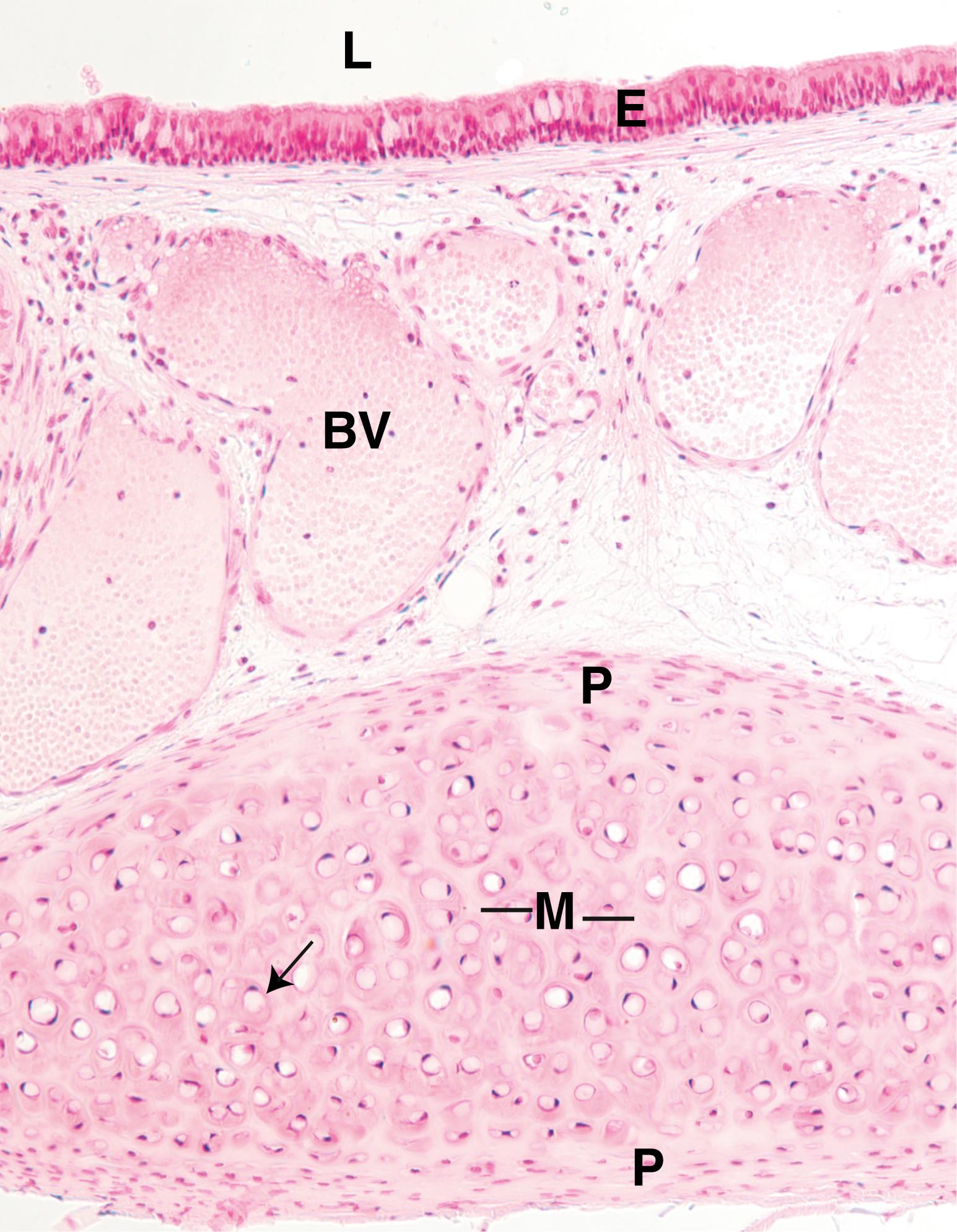
Mesenchymal cells at the periphery of developing cartilage differentiate to form fibroblasts that manufacture a dense irregular collagenous connective tissue, the perichondrium , responsible for the maintenance and growth of cartilage. The perichondrium has two layers: an outer fibrous layer composed of type I collagen, fibroblasts, and blood vessels; and an inner cellular layer composed mostly of chondrogenic cells that divide, then differentiate into chondroblasts . (Note that under increased oxygen tension, these cells become transformed into osteoprogenitor cells that give rise to bone-forming cells, known as osteoblasts .) These newly formed cells elaborate matrix; in this way, cartilage also grows by adding to its periphery a process called appositional growth .
Interstitial growth occurs only in the early phase of hyaline cartilage formation. Articular cartilage lacks a perichondrium and increases in size by interstitial growth only. This type of growth also occurs in the epiphyseal plates of long bones, where the lacunae are arranged in a longitudinal orientation parallel to the long axis of the bone; in this case, interstitial growth serves to lengthen the bone. The cartilage in the remainder of the body grows mostly by apposition, a controlled process that may continue during the life of the cartilage.
Mesenchymal cells located within the chondrification centers are induced to become secreting chondroblasts by their attachments and the chemistry of the surrounding extracellular matrix. Also, if chondroblasts are removed from their secreted cartilage matrix and are grown in a monolayer in a low-density substrate, they will cease to secrete cartilage matrix containing type II collagen. Instead, they will become fibroblast-like and start secreting type I collagen.
It has been demonstrated in animal experiments that mice with arthritic-like knee joints when treated with kartogenin developed more cartilage and were able to move their joints freely and without pain.
Because osteoarthritis does not damage bone until after the cartilage is completely worn down and bone articulates directly against bone, an artificial cartilage could be constructed to replace the damaged cartilage and assuage joint pain. Recently, a hydrogel composed of 70% to 90% water and nanofibers of aramid—the material used in bulletproof vests—has been tested to replace the damaged cartilage in animals. The hydrogel satisfied many of the requirements for artificial cartilage but clinical studies have to be conducted to see how well the material adheres to bone and how it interacts with the surrounding tissues.
The matrix of hyaline cartilage is composed of type II collagen, proteoglycans, glycoproteins, and extracellular fluid.
The semitranslucent blue-gray matrix of hyaline cartilage contains up to 40% of its dry weight in collagen. In addition, it contains proteoglycan aggregates (mostly in the form of aggrecans), glycoproteins (mostly chondronectin), and extracellular fluid. Because the refractive index of the collagen fibrils and that of the ground substance are nearly the same, the matrix appears to be an amorphous, homogeneous mass, as seen with the light microscope.
The matrix of hyaline cartilage contains primarily type II collagen , but types IX, X, and XI and other minor collagens are also present in small quantities. Type II collagen does not form large bundles, although the bundle thickness increases with distance from the lacunae. The matrix is subdivided into two regions: the territorial matrix , around each lacuna, and the interterritorial matrix (see Fig. 7.4 ). The territorial matrix, a 50-μm-wide band, is poor in collagen and rich in chondroitin sulfate, which contributes to its basophilic and intense staining. The bulk of the matrix is interterritorial matrix , which is richer in type II collagen and poorer in proteoglycans than the territorial matrix.
A small region of the matrix—1 to 3 μm thick, immediately surrounding the lacuna—is known as the pericellular capsule . It displays a fine meshwork of collagen fibers embedded in a basal lamina–like substance. These fibers may represent some of the other minor collagens present in hyaline cartilage; it has been suggested that the pericellular capsule may protect chondrocytes from mechanical stresses.
Cartilage matrix is rich in aggrecans , large proteoglycan molecules composed of protein cores to which chondroitin 4-sulfate, chondroitin 6-sulfate, and heparan sulfate are covalently linked. The abundant negative charges associated with these exceedingly large proteoglycan molecules attract cations, predominantly Na + ions, which, in turn, attract water molecules. In this way, the cartilage matrix becomes hydrated to such an extent that up to 80% of the wet weight of cartilage is water, accounting for the ability of cartilage to resist forces of compression.
Not only do hydrated proteoglycans fill the interstices among the collagen fiber bundles but also their GAG side chains form electrostatic bonds with the collagen. Thus, the ground substance and fibers of the matrix form a cross-linked molecular framework that resists tensile forces.
Cartilage matrix also contains the adhesive glycoprotein chondronectin . This large molecule, similar to fibronectin, has binding sites for type II collagen, chondroitin 4-sulfate, chondroitin 6-sulfate, hyaluronic acid, and integrins (transmembrane proteins) of chondroblasts and chondrocytes. Chondronectin thus assists these cells in maintaining their contact with the fibrous and amorphous components of the matrix.
The smoothness of hyaline cartilage and its ability to resist forces of both compression and tension are essential to its function at the articular surfaces of joints. Because cartilage is avascular, nutrients and oxygen must diffuse through the water of hydration present in the matrix. The inefficiency of such a system necessitates a limit on the width of cartilage. There is a constant turnover in the proteoglycans of cartilage that changes with age. Hormones and vitamins also exert influence over the growth, development, and function of cartilage. Many of these substances also affect skeletal formation and growth ( Table 7.2 ).
Hyaline cartilage degenerates when the chondrocytes hypertrophy and die and the matrix begins to calcify. This process is a normal and integral part of endochondral bone formation. However, it is also a natural process of aging, often resulting in less mobility and pain in the joints.
Cartilage regeneration is usually poor, except in children. Chondrogenic cells from the perichondrium enter the defect and form new cartilage. If the defect is large, the cells form dense connective tissue to repair the scar.
| Hormone | Effects |
|---|---|
| Thyroxine, testosterone, and somatotropin (via insulin-like growth factors) | Stimulate cartilage growth and matrix formation |
| Cortisone, hydrocortisone, and estradiol | Inhibit cartilage growth and matrix formation |
| Vitamin | |
| Hypovitaminosis A | Reduces width of epiphyseal plates |
| Hypervitaminosis A | Accelerates ossification of epiphyseal plates |
| Hypovitaminosis C | Inhibits matrix synthesis and deforms architecture of epiphyseal plate; leads to scurvy |
| Absence of vitamin D, resulting in deficiency in absorption of calcium and phosphorus | Proliferation of chondrocytes is normal but matrix does not become calcified properly; results in rickets |
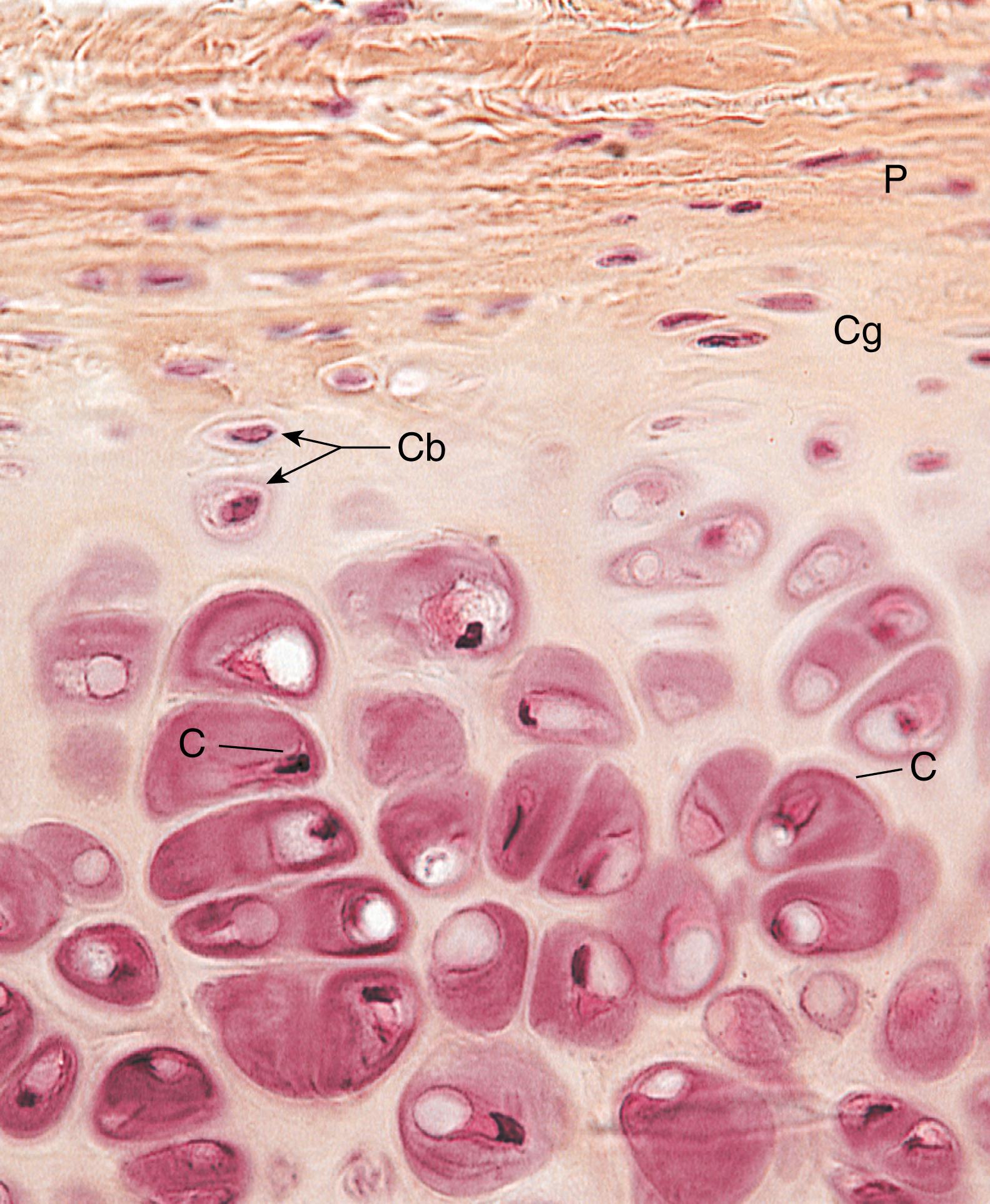
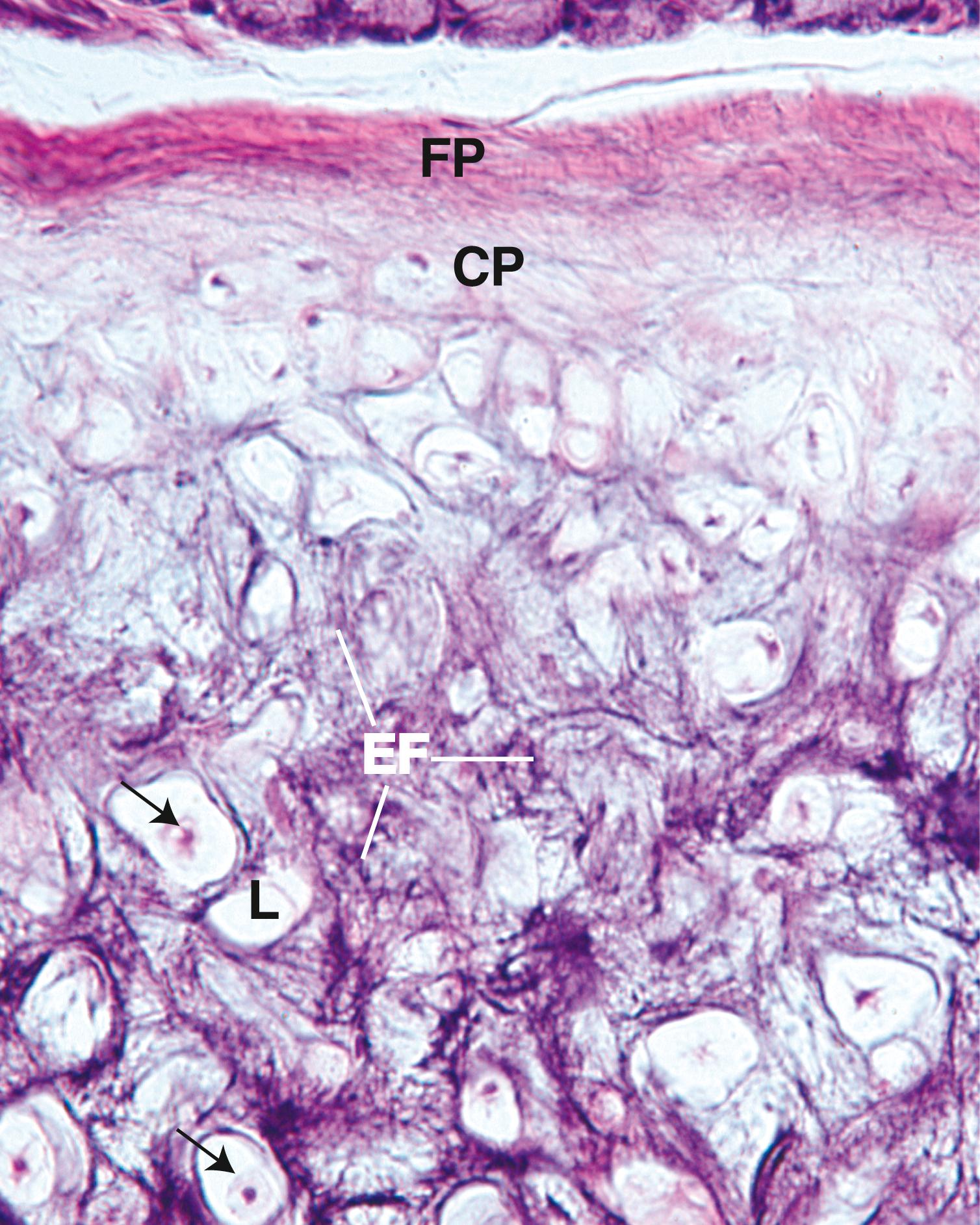
Elastic cartilage greatly resembles hyaline cartilage except that its matrix and perichondrium possess elastic fibers.
Elastic cartilage is located in the pinna of the ear, external and internal auditory tubes, epiglottis, and larynx (cuneiform cartilage). In the fresh state, owing to the presence of elastic fibers, elastic cartilage is somewhat yellow in appearance and is more opaque than hyaline cartilage (see Table 7.1 ).
The outer fibrous layer of the perichondrium is rich in elastic fibers. The matrix of elastic cartilage possesses abundant fine-to-coarse branching elastic fibers interspersed with type II collagen fiber bundles, giving it much more flexibility than the matrix of hyaline cartilage ( Figs. 7.5 and 7.6 ). Chondrocytes of elastic cartilage are more abundant and larger than those of hyaline cartilage. The matrix is not as ample as in hyaline cartilage, and the elastic fiber bundles of the territorial matrix are larger and coarser than those of the interterritorial matrix.
Fibrocartilage, unlike hyaline and elastic cartilage, does not possess a perichondrium and its matrix possesses type I collagen.
Fibrocartilage , present in intervertebral disks, in the pubic symphysis, and in articular disks, does not possess a perichondrium. It displays a scant amount of matrix (rich in chondroitin sulfate and dermatan sulfate) and exhibits bundles of type I collagen, which stain acidophilic ( Fig. 7.7 ). Chondrocytes are often aligned in alternating parallel rows with the thick, coarse bundles of collagen, which parallel the tensile forces attendant on this tissue (see Table 7.1 ).
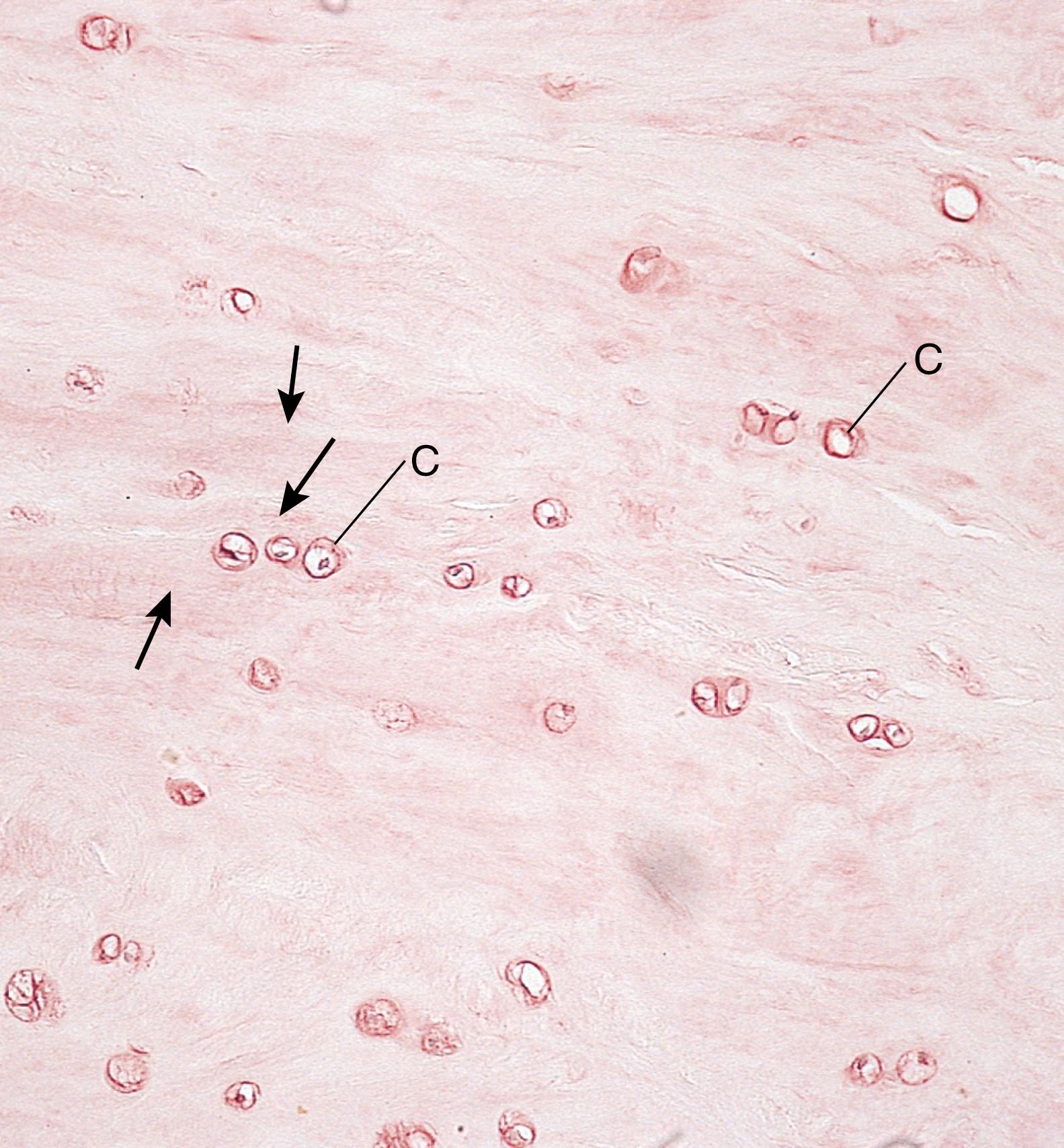
Chondrocytes of fibrocartilage usually arise from fibroblasts that experience increasing tensile forces and, therefore, begin to manufacture proteoglycans. As the ground substance surrounds the fibroblast, the cell becomes incarcerated in its own matrix and differentiates into a chondrocyte.
Intervertebral disks represent an example of the organization of fibrocartilage. They are interposed between the hyaline cartilage coverings of the articular surface of successive vertebrae. Each disk contains a gelatinous center, called the nucleus pulposus , which is composed of notochord-derived cells lying within a hyaluronic acid–rich matrix. These cells disappear by the 20th year of life. Much of the nucleus pulposus is surrounded by the annulus fibrosus , layers of fibrocartilage whose type I collagen fibers run vertically between the hyaline cartilages of the two vertebrae. The fibers of adjacent lamellae are oriented obliquely to each other, providing support to the gelatinous nucleus pulposus . The annulus fibrosus provides resistance against tensile forces, whereas the nucleus pulposus resists forces of compression.
A ruptured disk refers to a tear or break in the laminae of the annulus fibrosus through which the gel-like nucleus pulposus extrudes. This condition occurs more often on the posterior portions of the intervertebral disks, particularly in the lumbar portion of the back, where the disk may dislocate, or slip. A “slipped disk” leads to severe, intense pain in the lower back and extremities because the displaced disk compresses the lower spinal nerves.
Bone is a specialized connective tissue whose extracellular matrix is calcified, incarcerating the cells that secreted it.
Bone is the primary structural framework for support and protection of the organs of the body, including the brain and spinal cord and the structures within the thoracic cavity—the lungs and heart. It also contains a central cavity, the marrow cavity , which houses the bone marrow , a hemopoietic organ. Bones also serve as levers for the muscles attached to them, thereby multiplying the force of the muscles to attain movement. Additionally, bone is a reservoir for several minerals of the body; for example, it stores about 99% of the body’s calcium.
Although bone is one of the hardest substances of the body, it is a dynamic tissue that constantly changes shape in relation to the stresses placed on it. Thus, pressures applied to bone lead to its resorption, and tension applied to it results in development of new bone.
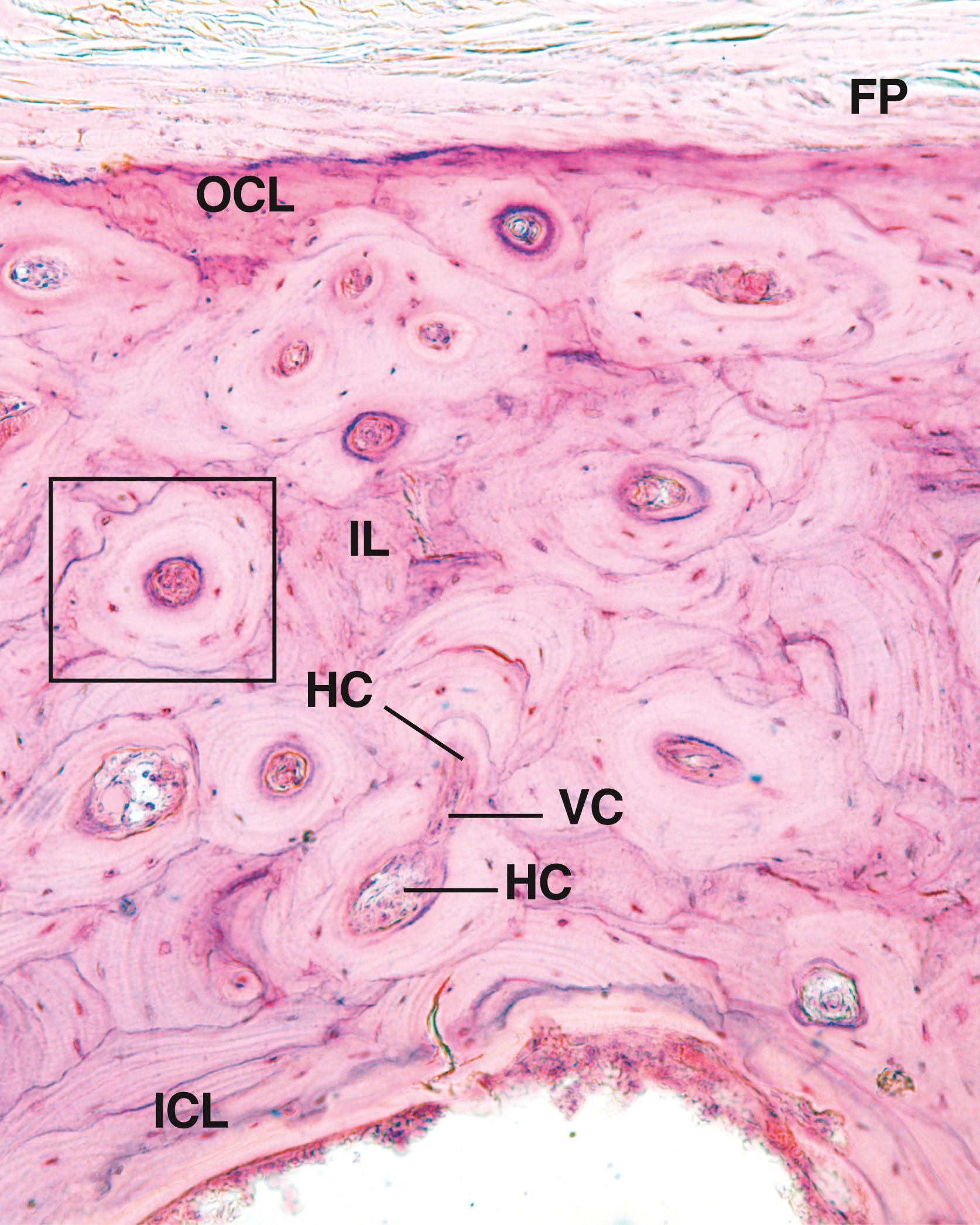
Bone is covered on its external surface, except at synovial articulations, with a periosteum , which consists of an outer layer of dense fibrous connective tissue and an inner cellular layer containing osteoprogenitor ( osteogenic ) cells as well as occasional osteoblasts . Bundles of collagen fibers from the periosteum, known as Sharpey fibers , are embedded into the outer surface of bone, thereby securing the periosteum to the bone surface. The central cavity of a bone is lined with endosteum , a specialized thin connective tissue composed of a monolayer of osteoprogenitor cells and osteoblasts .
The cells of bone include osteoprogenitor cells , which differentiate into osteoblasts . Osteoblasts are responsible for secreting and eventually calcifying bone matrix. When these cells are surrounded by that matrix, they become quiescent and are known as osteocytes , housed in spaces known as lacunae . Additional cells of bone, known as osteoclasts , are multinucleated giant cells derived from fused bone marrow precursors. Osteoclasts are responsible for bone resorption and remodeling.
Because bone is such a hard tissue, two methods are employed to prepare it for study. Decalcified sections can be prepared by decalcifying the bone in an acid solution to remove the calcium salts. The tissue can then be embedded, sectioned, and routinely stained for study. Ground sections are prepared by sawing the undecalcified bone into thin slices, followed by grinding the sections with abrasives between glass plates. When the section is sufficiently thin, it is mounted for study with light microscopy. Each system has disadvantages. In decalcified sections, osteocytes are distorted by the decalcifying acid bath; in ground sections, the cells are destroyed, and the lacunae and canaliculi are filled in with bone debris.
Bone matrix has inorganic and organic constituents.
The inorganic constituents of bone are crystals of calcium hydroxyapatite, composed mostly of calcium and phosphorus.
The inorganic portion of bone, which constitutes about 65% of its dry weight, is composed mainly of calcium and phosphorus along with other components, including bicarbonate, citrate, magnesium, sodium, and potassium. Calcium and phosphorus exist primarily in the form of hydroxyapatite crystals [Ca 10 (PO 4 ) 6 (OH) 2 ], but calcium phosphate is also present in an amorphous form. Hydroxyapatite crystals (40 nm in length by 25 nm in width and 1.5–3 nm in thickness) are arranged in an ordered fashion along the type I collagen fibers. They are deposited into the gap regions of the collagen but also are present along the overlap region. The free surface of the crystals is surrounded by amorphous ground substance. The surface ions of the crystals attract H 2 O molecules, forming a hydration shell around the crystals that permits ion exchange with the extracellular fluid.
When bone is decalcified (i.e., all mineral is removed from the bone), it still retains its original shape but becomes so flexible that it can be bent like a piece of tough rubber. If the organic component is extracted from bone, the mineralized skeleton still retains its original shape but becomes extremely brittle and can be fractured with ease.
The predominant organic component of bone is type I collagen.
The organic component of bone matrix constitutes approximately 35% of the dry weight of bone; it includes fibers that are almost exclusively type I collagen (with a small amount of type V, VII, XI, and XII collagen).
Collagen comprises about 80% to 90% of the organic component of bone. It is formed in large (50–70 nm in diameter) bundles displaying the typical 67-nm periodicity. Type I collagen in bone is highly cross-linked, which prevents it from being easily extracted.
The fact that bone matrix stains with periodic acid–Schiff (PAS) reagent and displays slight metachromasia indicates the presence of sulfated GAGs, predominantly chondroitin sulfate and keratan sulfate. These form small proteoglycan molecules with short protein cores to which the GAGs are covalently bound. The proteoglycans are noncovalently bound via link proteins to hyaluronic acid , forming very large aggrecan composites . The abundance of collagen, however, causes the matrix to be acidophilic.
Several glycoproteins are also present in the bone matrix. These appear to be restricted to bone and include osteocalcin (which binds to hydroxyapatite) and osteopontin , which also binds to hydroxyapatite but has additional binding sites for other components as well as for integrins present on osteoblasts and osteoclasts. Vitamin D stimulates the synthesis of these glycoproteins. Bone sialoprotein , another matrix protein, has binding sites for matrix components and integrins of osteoblasts and osteocytes, suggesting its involvement in the adherence of these cells to bone matrix.
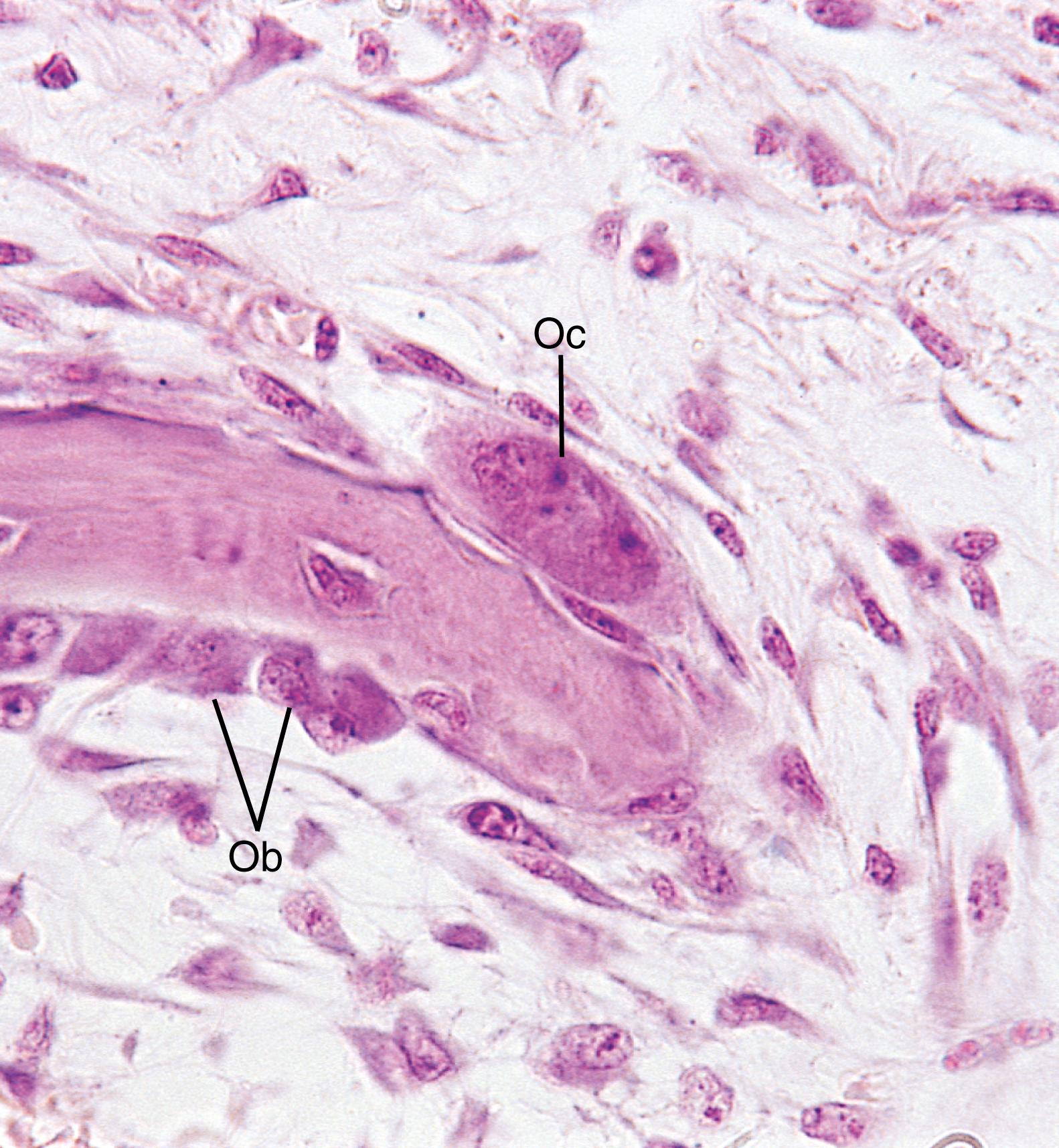
The cells of bone are osteoprogenitor cells, osteoblasts, osteocytes, and osteoclasts ( Figs. 7.8 and 7.9 ).

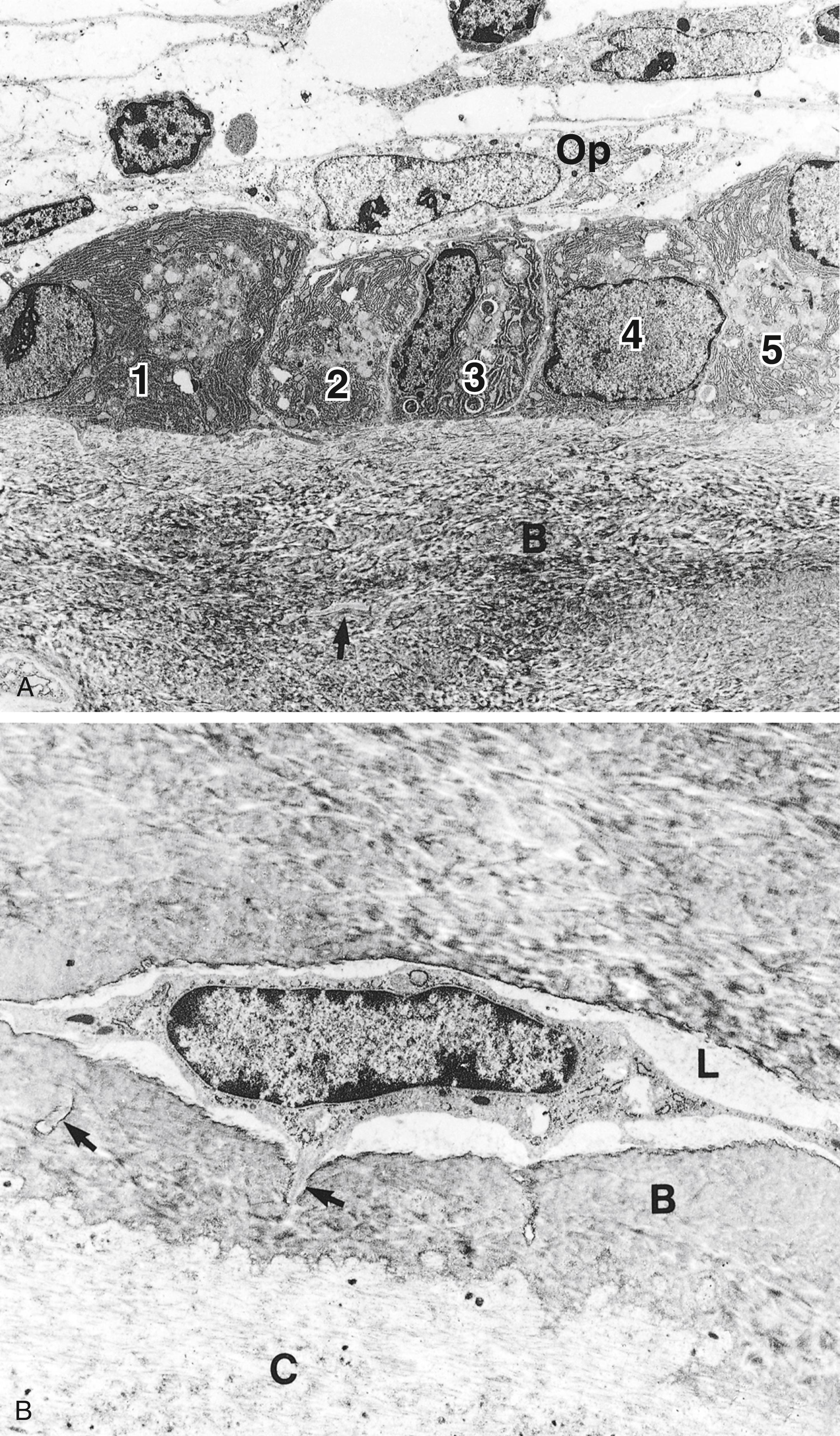
Osteoprogenitor cells are derived from embryonic mesenchymal cells and retain their ability to undergo mitosis.
Osteoprogenitor cells are located in the inner cellular layer of the periosteum, lining haversian canals, and in the endosteum (see Fig. 7.9 ). These cells, derived from embryonic mesenchyme, remain in place throughout postnatal life and can undergo mitotic division and have the potential to differentiate into osteoblasts. Moreover, under certain conditions of low oxygen tension, these cells may differentiate into chondrogenic cells. Osteoprogenitor cells are spindle shaped and have a pale-staining oval nucleus. Their scant pale-staining cytoplasm displays sparse rough endoplasmic reticulum (RER) and a poorly developed Golgi apparatus but has an abundance of free ribosomes. These cells are most active during the period of intense bone growth.
Osteoblasts not only synthesize the organic matrix of bone but also possess receptors for parathyroid hormone.
Bone morphogenic protein-6 (BMP-6) —as well as, to some extent, BMP-2 and BMP-4—and transforming growth factor-β (TGF-β) induce osteoprogenitor cells to differentiate into osteoblasts , cells that manufacture and secrete the organic components of bone matrix (osteoid) : type I collagen and some type V collagen, glycoproteins, and proteoglycans. Osteoblasts also synthesize the receptor for the activation of nuclear factor kappa Β ligand (RANKL) , macrophage colony-stimulating factor (M-CSF) , alkaline phosphatase , insulin-like growth factor-1 (IGF-1) receptors , and parathyroid hormone (PTH) receptors , all of which they place on their cell membranes. These cells also manufacture and release a number of additional macromolecules, such as
Osteocalcin , a signaling molecule responsible for mineralization of bone
Osteonectin , a glycoprotein that assists in the binding of calcium hydroxyl apatite crystals to collagen
Osteopontin , which aids in the formation of the sealing zone of osteoclasts (see section on the morphology of osteoclasts)
Bone sialoprotein , which assists osteoblasts in adhering to the bone matrix, and
Osteoprotegerin (OPG) , a glycoprotein that can bind to RANKL and, thus, interfere with osteoclast formation.
Osteoblasts are located on the surface of the bone in a sheet-like arrangement of cuboidal to columnar cells ( Fig. 7.10 ). When actively secreting matrix, they exhibit a basophilic cytoplasm.
The organelles of osteoblasts are polarized so that the nucleus is located away from the region of secretory activity, which houses secretory granules believed to contain matrix precursors. Electron micrographs exhibit abundant RER, a well-developed Golgi complex ( Fig. 7.11A ), and numerous secretory vesicles containing flocculent material. Osteoblasts extend short processes that contact those of neighboring osteoblasts and long processes that form contacts with processes of osteocytes. Although these processes form gap junctions with one another, the number of gap junctions between osteoblasts is much fewer than those between osteocytes. As osteoblasts exocytose their secretory products, each cell surrounds itself with the bone matrix that it has just produced. When this occurs, the incarcerated cell is referred to as an osteocyte , and the space it occupies is known as a lacuna . Most of the bone matrix becomes calcified; however, osteoblasts as well as osteocytes are always separated from the calcified substance by a thin, noncalcified layer known as the osteoid (uncalcified bone matrix).
Surface osteoblasts that cease to form matrix revert to a more flattened-shaped quiescent state and are called bone-lining cells . Although these cells appear to be similar to osteoprogenitor cells, they are most likely incapable of dividing but can be reactivated to the secreting form with the proper stimulus ( Table 7.3 ).
Osteoblast cell membranes are rich in the enzyme alkaline phosphatase. During active bone formation, these cells secrete high levels of alkaline phosphatase, elevating the levels of this enzyme in the blood. Thus, the clinician can monitor bone formation by measuring the blood alkaline phosphatase level.
Individuals who have the type of mutations in the genes that code for TGF-β, in which the factor is always active, have the rare autosomal-dominant inherited disorder known as Camurati-Engelmann disease . This ailment usually manifests itself in late adolescence or early adulthood, characterized by an excess of highly active osteoblasts, resulting in very thick bones of the extremities. In some patients, the bones of the skull and hip may also be involved. The individual experiences intense pain in the bones and muscles of the leg. Additionally, the muscles of the extremities may be weakened; that, with the additional factor of pain, causes many affected individuals to “waddle” as they walk.
| Cytokine | Function |
|---|---|
| Alkaline phosphatase | Encourages bone matrix mineralization |
| Bone morphogenic protein | Stimulates osteoprogenitor cells to become osteoblasts |
| Bone sialoprotein | Assists the adherence of osteoblasts to bone matrix |
| Insulin-like growth factor-1 | Encourages bone formation |
| Interleukin-1 | Stimulates osteoclast precursors to undergo mitosis |
| Interleukin-6 | Recruits and induces osteoclast precursors to become osteoclasts |
| Macrophage colony-stimulating factor | Stimulates osteoclast precursor formation and induces them to express RANK on their cell membrane |
| Osteocalcin | Stimulates mineralization of bone matrix |
| Osteoclast-stimulating factor | Stimulates osteoclast to become active and resorb bone |
| Osteonectin | Encourages calcium hydroxyapatite binding to type I collagen |
| Osteopontin | Aids osteoclasts in their formation of sealing zone |
| Osteoprotegerin | Inhibits osteoclast formation by forming bonds with RANKL |
| PTH receptor | Parathyroid hormone binding induces osteoblasts to secrete RANKL |
| RANKL | Encourages preosteoclast differentiation into osteoclast |
| TGF-β | Stimulates osteoprogenitor cells to become osteoblasts |
Osteoblasts have several factors on their cell membranes, the most significant of which are integrins and PTH receptors . When PTH binds to these receptors, it stimulates osteoblasts to secrete RANKL , a factor that induces the differentiation of preosteoclasts into osteoclasts. Also, osteoblasts secrete an osteoclast-stimulating factor , which activates osteoclasts to resorb bone. Osteoblasts also secrete enzymes responsible for removing osteoid so that osteoclasts can make contact with the mineralized bone surface.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here