Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The carotid body tumor (CBT), first described in 1743 by Von Haller, is the only known pathologic condition of the carotid body. The tumor is extremely rare. In 1971, only about 500 cases had been reported in the literature; doubling to more than 1000 by the early 1980s. Due to the infrequency of this disorder, very little is known about its etiology, clinical, and biologic behavior, or its malignant potential. In 1903, the first successful resection of a carotid body tumor was performed by Scudder in the United States. Despite over a century of literature describing surgical treatment, significant controversy remains surrounding the details in the management of carotid body tumors.
The exact incidence of CBTs is unknown. Although they may be discovered in patients of all ages, they are usually diagnosed in the third to fifth decades of life. Patients with a family history of carotid body tumors may present at an earlier age. Gender predominance has not been established, though some studies have found a higher prevalence in women. , They may be classified as sporadic, familial, or hyperplastic. , Sporadic is the most common form. Familial patterns may occur in up to 10% of cases with apparent autosomal dominant inheritance. In addition to a younger age at presentation for familial cases, rates of bilateral tumors have been reported in up to 30% of cases, in contrast to bilateral disease in 2% to 20% of nonfamilial cases. , Hyperplastic lesions, although not true neoplasms, are more prevalent in patients exposed to prolonged hypoxia, including those living at high altitudes and those suffering from chronic obstructive pulmonary disease or cyanotic heart disorders. This association has suggested chronic hypoxia as a potential etiology of CBTs. Studies of mice deficient in the SDHD (succinyl dehydrogenase – subunit D) gene have found continued activation of the carotid body cells in response to hypoxia; such that SDHD gene mutations may be associated with formation of carotid body tumors.
The carotid body is the largest mass of chemoreceptor tissue in the body. It is located within the periadventitia of the posterior surface of the carotid bifurcation. The normal carotid body is ovoid in shape and approximately 5 mm in its longest dimension. It usually receives its blood supply through branches of the external carotid artery. Blood returns through tributaries of the lingual and laryngopharyngeal veins. The carotid body derives sensory innervation through small nerve fibers from the glossopharyngeal nerve.
The embryologic origins of the carotid body are both neural crest ectoderm and mesodermal tissue from the third branchial arch. The neural crest cells migrate in close association with autonomic ganglion cells; thus, they are often referred to as paraganglioma cells. These cells differentiate into the chemoreceptors, also known as type I glomus cells. The mesoderm forms the rich vascular stroma, made up of type II glomus cells, which support the chemoreceptor cells.
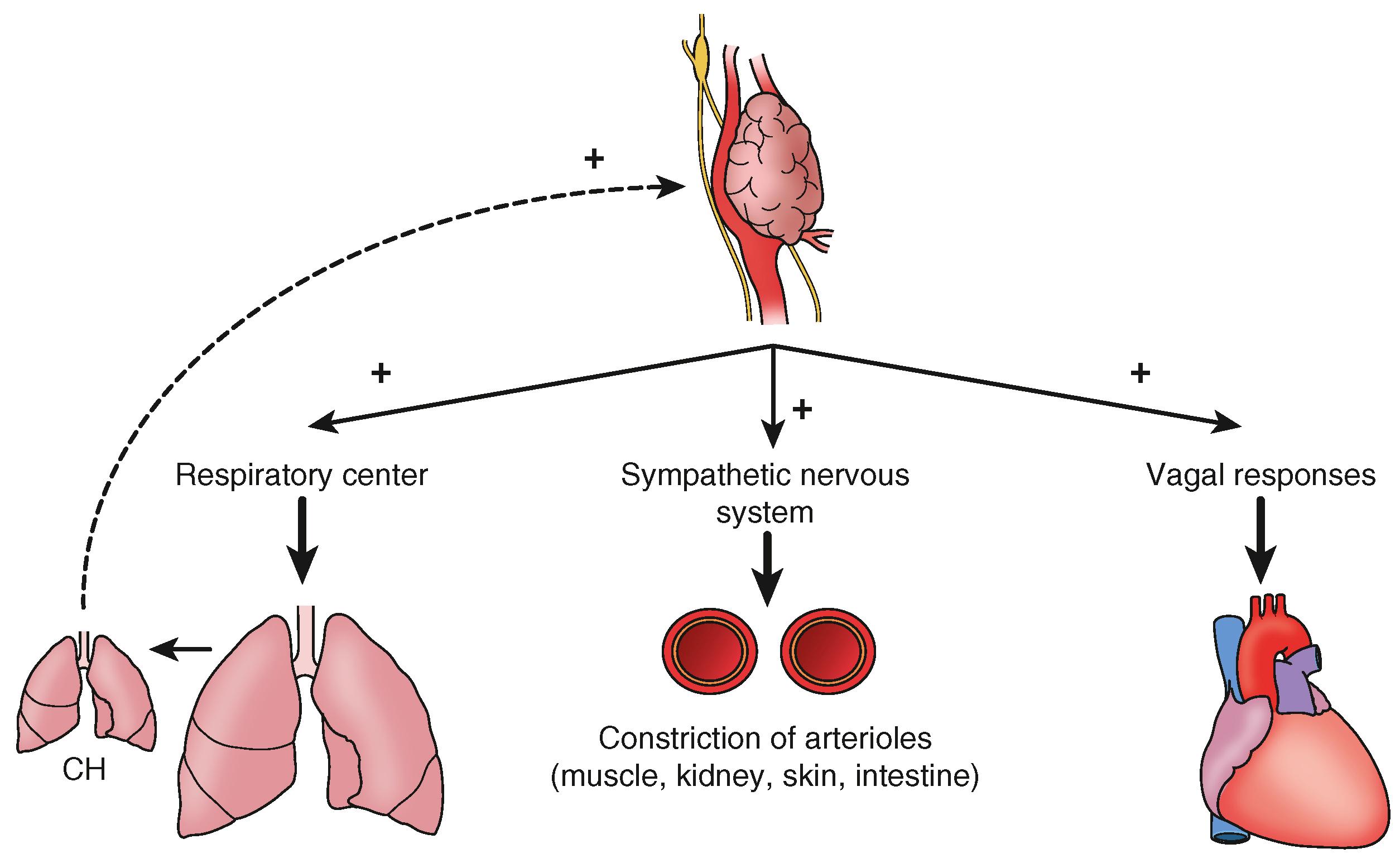
The carotid body is stimulated primarily by the partial pressure of O 2 , and to a lesser degree the partial pressure of CO 2 and arterial pH. In response, the type I glomus cells release neurotransmitters that act on the receptors of afferent nerve fibers. Signals are carried through the glossopharyngeal nerve to the medulla oblongata, affecting a number of the body’s systems ( Fig. 98.1 ). Most notable are cardiopulmonary centers in the brain that regulate breathing and blood pressure. For example, hypoxia, hypercapnia, or acidosis can stimulate the carotid body, resulting in increases in respiratory rate, tidal volume, and blood pressure with vasoconstriction.
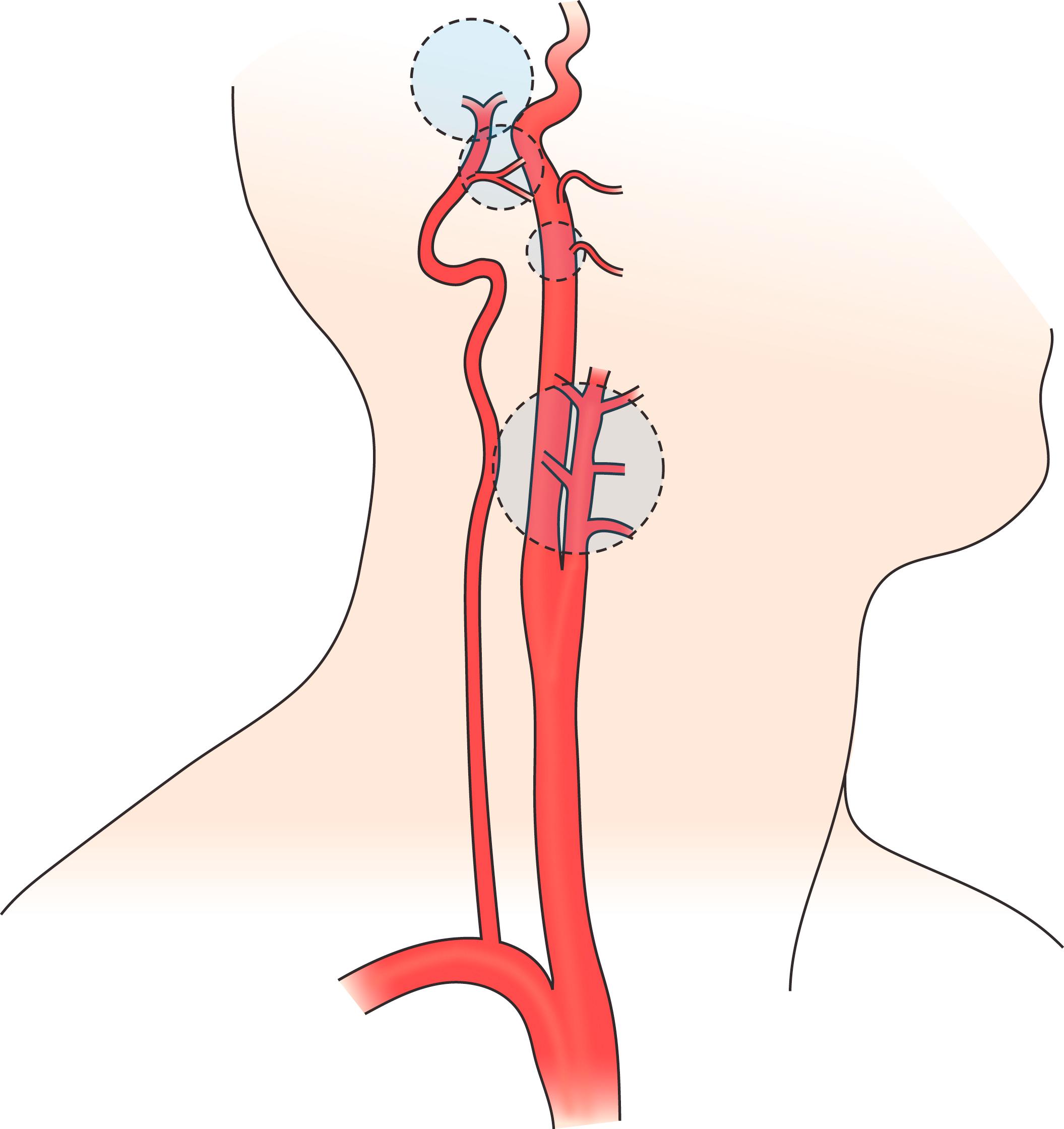
CBTs are also known as carotid chemodectomas, carotid paragangliomas, and glomus tumors. They represent neoplastic growths of the chemoreceptive tissue. These tumors belong to the family of paragangliomas, which are neoplastic tumors that occur along the autonomic ganglion chain from the head to pelvis. Within the head and neck, carotid body tumors are the most common type. Other cervical paragangliomas include the glomus tympanicum, glomus vagale, and glomus jugulare ( Fig. 98.2 ).
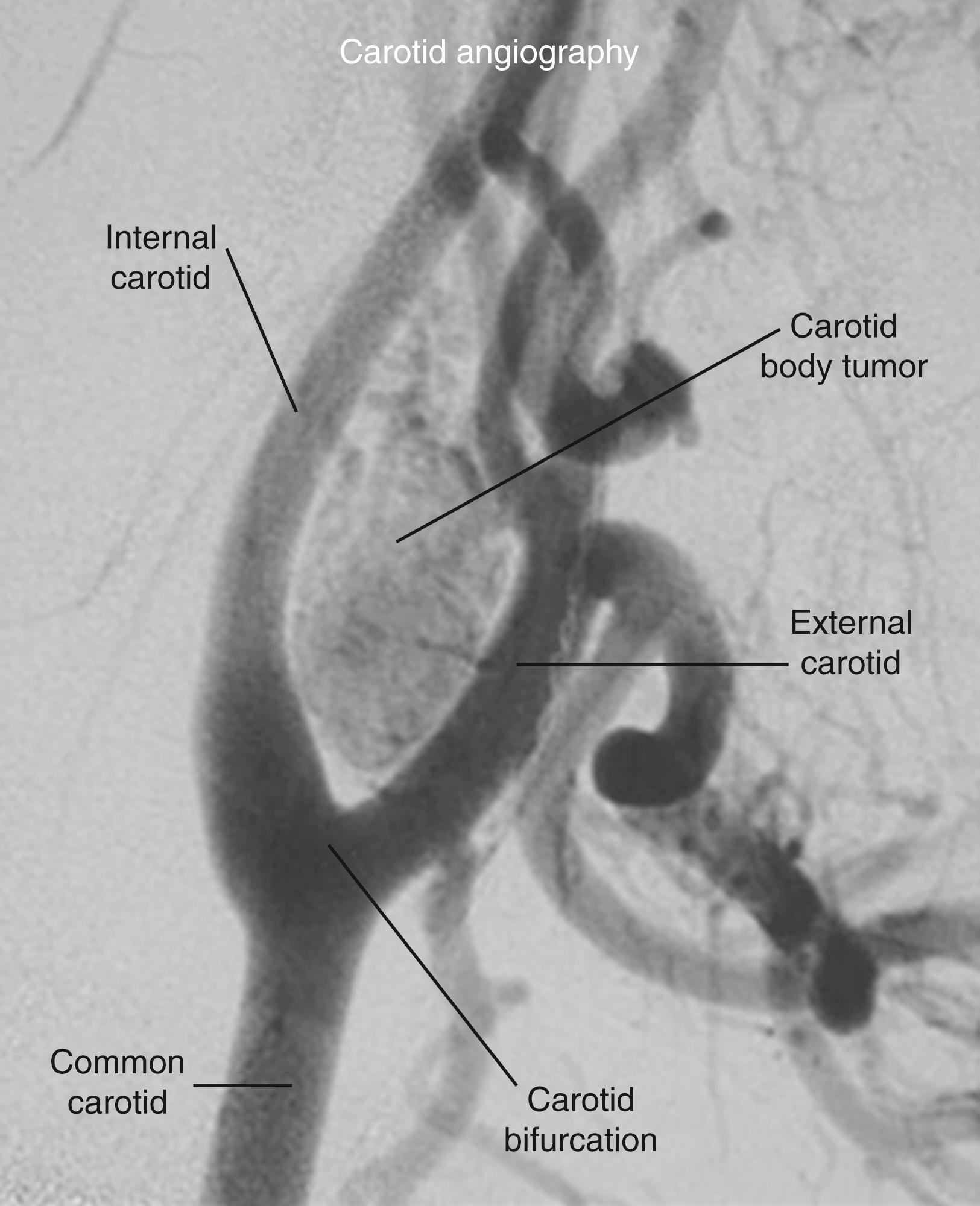
Macroscopically, CBTs resemble normal carotid body tissue. They are reddish brown, rubbery, and well circumscribed, although they lack a true capsule. They are highly vascular, and can invade the adventitia of adjacent carotid vessels. As the tumors enlarge, they distort the carotid bifurcation and splay the internal and external carotid arteries, known as the “lyre sign” seen on angiography ( Fig. 98.3 ).
Microscopically, CBTs tend to resemble normal carotid body architecture with a well-differentiated benign appearance. Only very rarely does histology demonstrate degenerative malignant characteristics, such as nuclear polymorphism, vascular invasion, increased mitotic activity, and necrosis. Malignant transformation cannot be predicted based on histologic findings. , Advanced immunohistochemical studies have revealed that carotid body tumors can produce numerous neuroendocrine substances, often with granules rich in catecholamines seen in the cytoplasm. These tumors, in contrast to retroperitoneal paragangliomas, are usually nonfunctional and stain negative for chromaffin.
Most CBTs are benign. Malignant transformation has been reported, but the exact incidence is unknown. In contrast to many other types of cancer, malignancy of CBTs and other neuroendocrine tumors is based on clinical behavior instead of histology. Even benign tumors are capable of aggressive invasion into adjacent structures, as well as nodal and distal metastatic spread. Local growth may include adherence or encasement of neurologic and vascular structures, and even extension into the skull. Metastatic disease usually spreads into regional lymph nodes. If carotid body cells are found in lymph nodes biopsied during surgery, this is diagnostic for malignancy; and an indication for completion of an ipsilateral modified radical neck dissection. However, routine biopsy of lymph nodes is not recommended, and only advised if lymph nodes appear clinically abnormal. Metastases have also been seen in the cerebellum, thyroid, brachial plexus, lungs, kidney, pancreas, bones, and breast.
CBTs most commonly present as asymptomatic neck masses located below the angle of mandible. On palpation, the lesions are firm, smooth, and lobulated, and are characteristically mobile laterally but fixed longitudinally due to their association with the carotid artery. Carotid pulsation may be transmitted through the mass, and approximately 30% to 40% of patients may have an audible bruit over the tumor. Very large carotid tumors may cause compression or local invasion, leading patients to present with nonspecific symptoms, such as localized tenderness, fullness, numbness, dysphagia, hoarseness, chronic cough, and tinnitus. Tumors rarely produce cranial nerve dysfunction, and if there is involvement, symptoms are typically associated with the vagal, hypoglossal, and cervical sympathetic nerves. Occasionally, Horner syndrome has been reported in patients with this tumor. Patients may complain of dizziness, but lateralizing neurologic signs are uncommon.
Despite possessing apparatus to synthesize and secrete catecholamines and hormones, CBTs are almost never functional. In extremely rare cases, tumors demonstrate neuroendocrine activity and patients may complain of headaches, dizziness, palpitations, tachycardia, arrhythmias, flushing, diaphoresis, and photophobia. , Some cases have been reported of patients with hypertension that resolves after tumor resection, which may be caused by tumor-related catecholamine release.
These neoplasms tend to grow slowly over several years, although occasional cases of rapid growth have been reported. Although the risk of malignancy is believed to be relatively low, these tumors do progress in size and become locally invasive. Patients may live many years without treatment; however, due to the morbidity and mortality associated with progressively enlarging tumors, the low but unpredictable risk of malignancy, and the ease of excising small tumors, most surgeons recommend early diagnosis and surgical resection.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here