Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Cardiac output is the quantity of blood pumped into the aorta each minute by the heart. This is also the quantity of blood that flows through the circulation. Because cardiac output is the sum of the blood flow to all the tissues of the body, it is one of the most important factors to consider in relation to function of the cardiovascular system.
Venous return is equally important because it is the quantity of blood flowing from the veins into the right atrium each minute. The venous return and the cardiac output must equal each other except for a few heartbeats when blood is temporarily stored in or removed from the heart and lungs.
Cardiac output varies widely with the level of activity of the body. The following factors, among others, directly affect cardiac output: (1) the basic level of body metabolism; (2) whether the person is exercising; (3) the person’s age; and (4) the size of the body.
For young healthy men , resting cardiac output averages about 5.6 L/min. For women , this value is about 4.9 L/min. When one considers the factor of age as well—because with increasing age, body activity and mass of some tissues (e.g., skeletal muscle) diminish—the average cardiac output for the resting adult, in round numbers, is often stated to be about 5 L/min. However, cardiac output varies considerably among healthy men and women depending on muscle mass, adiposity, physical activity, and other factors that influence metabolic rate and nutritional needs of the tissues.
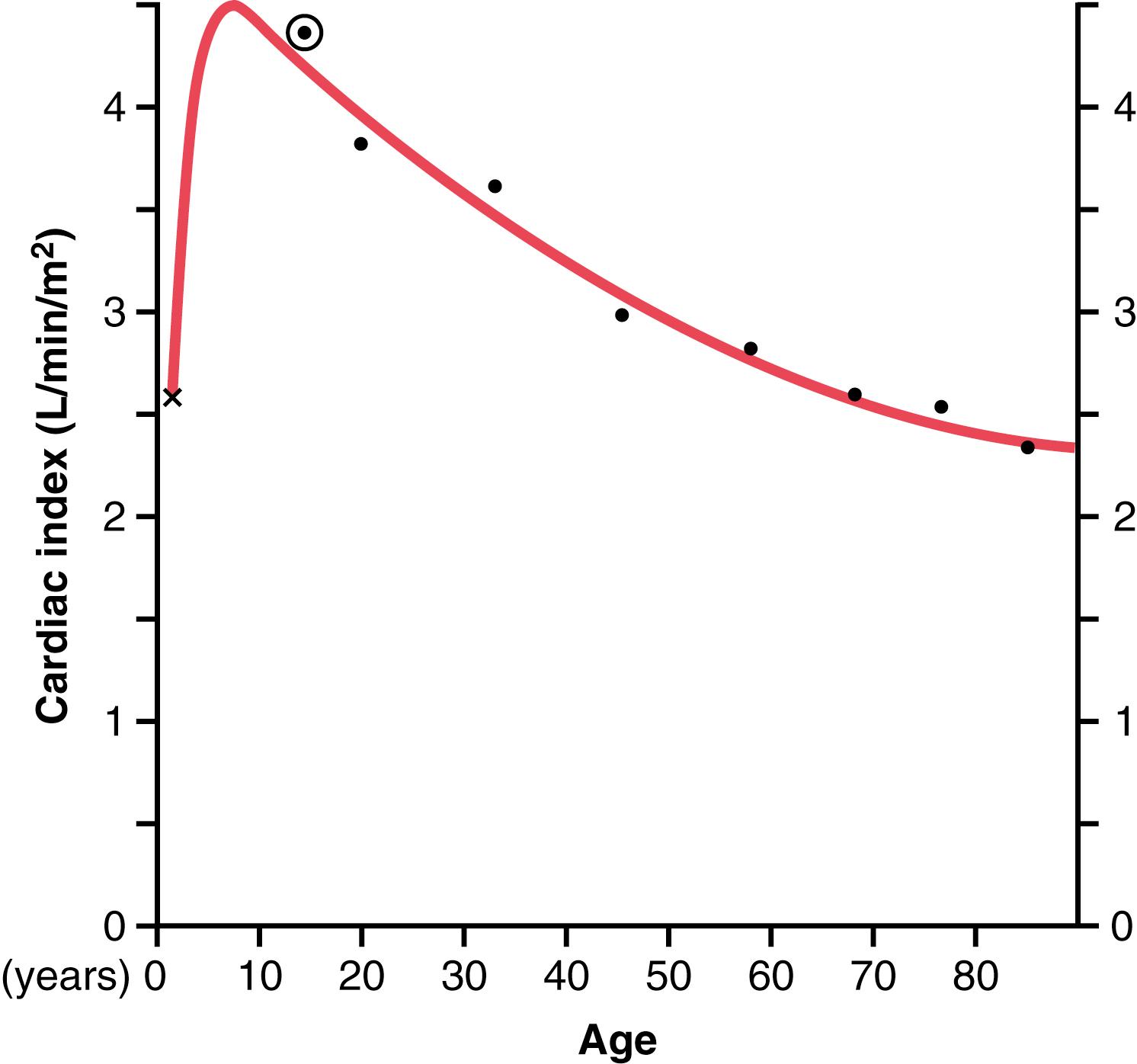
Experiments have shown that the cardiac output increases approximately in proportion to the surface area of the body. Therefore, cardiac output is frequently stated in terms of the cardiac index , which is the cardiac output per square meter of body surface area . The average person who weighs 70 kilograms has a body surface area of about 1.7 square meters, which means that the normal average cardiac index for adults is about 3 L/min/m 2 of body surface area.
Figure 20-1 shows the cardiac output, expressed as cardiac index, at different ages. The cardiac index rises rapidly to a level greater than 4 L/min/m 2 at age 10 years and declines to about 2.4 L/min/m 2 at age 80 years. We explain later in this chapter that the cardiac output is regulated throughout life almost directly in proportion to overall metabolic activity. Therefore, the declining cardiac index is indicative of declining activity and/or declining muscle mass with age.
Although heart function is obviously crucial in determining cardiac output, the various factors of the peripheral circulation that affect flow of blood into the heart from the veins, called venous return , are normally the primary controllers of cardiac output.
The main reason why peripheral factors are usually so important in controlling cardiac output is that the heart has a built-in mechanism that normally allows it to pump automatically the amount of blood that flows from the veins into the right atrium. This mechanism, called the Frank-Starling law of the heart , was discussed in Chapter 9 . Basically, this law states that when increased quantities of blood flow into the heart, the increased volume of blood stretches the walls of the heart chambers. As a result of the stretch, the cardiac muscle contracts with increased force, and this action ejects the extra blood that has entered from the systemic circulation. Therefore, the blood that flows into the heart is automatically pumped without delay into the aorta and flows again through the circulation.
Another important factor, discussed in Chapter 10, Chapter 18 , is that stretching the heart causes an increased heart rate. Stretch of the sinus node in the wall of the right atrium has a direct effect on the rhythmicity of the node to increase the heart rate as much as 10% to 15%. In addition, the stretched right atrium initiates a nervous reflex called the Bainbridge reflex , passing first to the vasomotor center of the brain and then back to the heart by way of the sympathetic nerves and vagi, which also increases the heart rate.
Under most normal unstressed conditions , the cardiac output is controlled mainly by peripheral factors that determine venous return. However, as we discuss later in the chapter, if the returning blood does become more than the heart can pump, then the heart becomes the limiting factor that determines cardiac output.
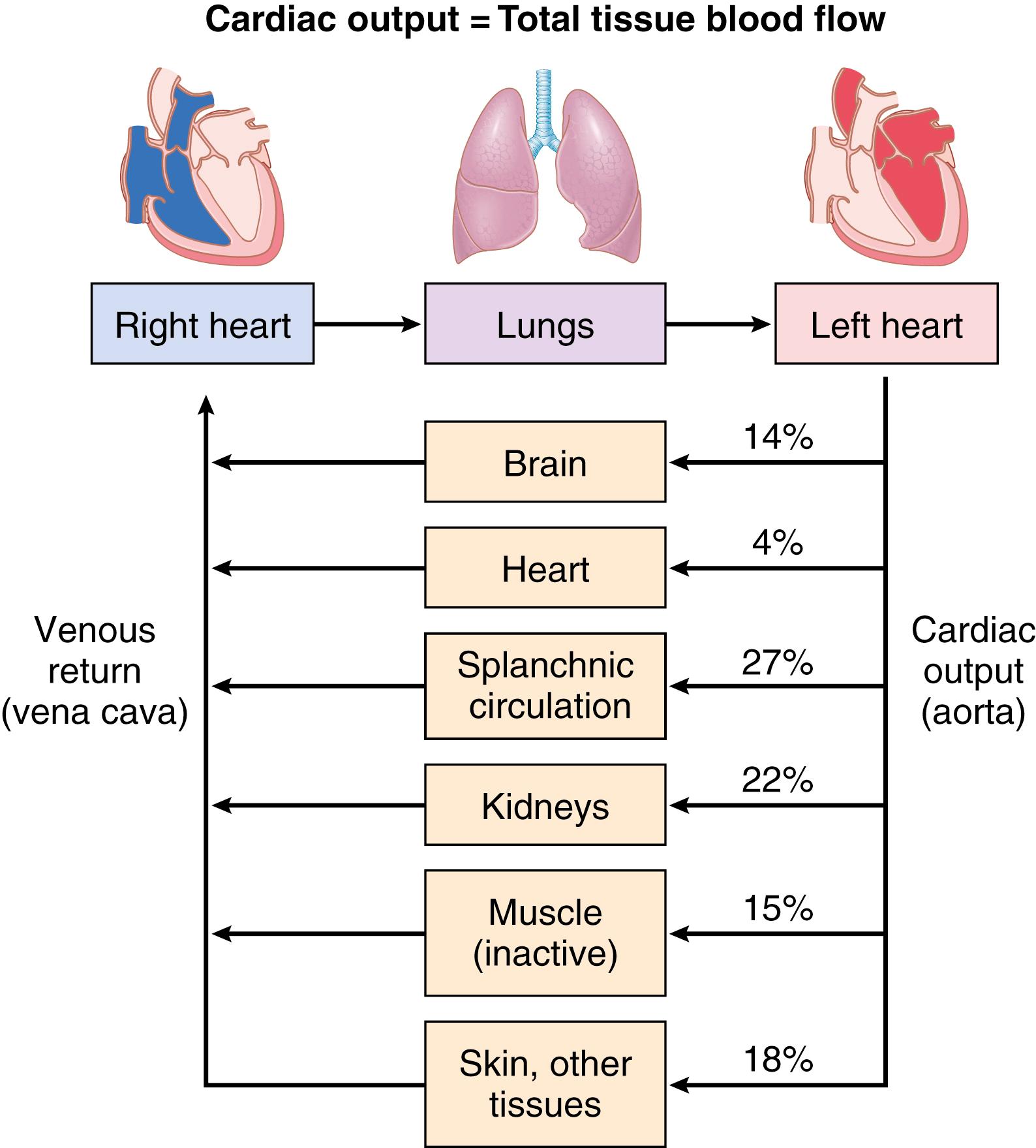
The venous return to the heart is the sum of all the local blood flow through all the individual tissue segments of the peripheral circulation ( Figure 20-2 ). Therefore, it follows that cardiac output regulation is normally the sum of all the local blood flow regulations.
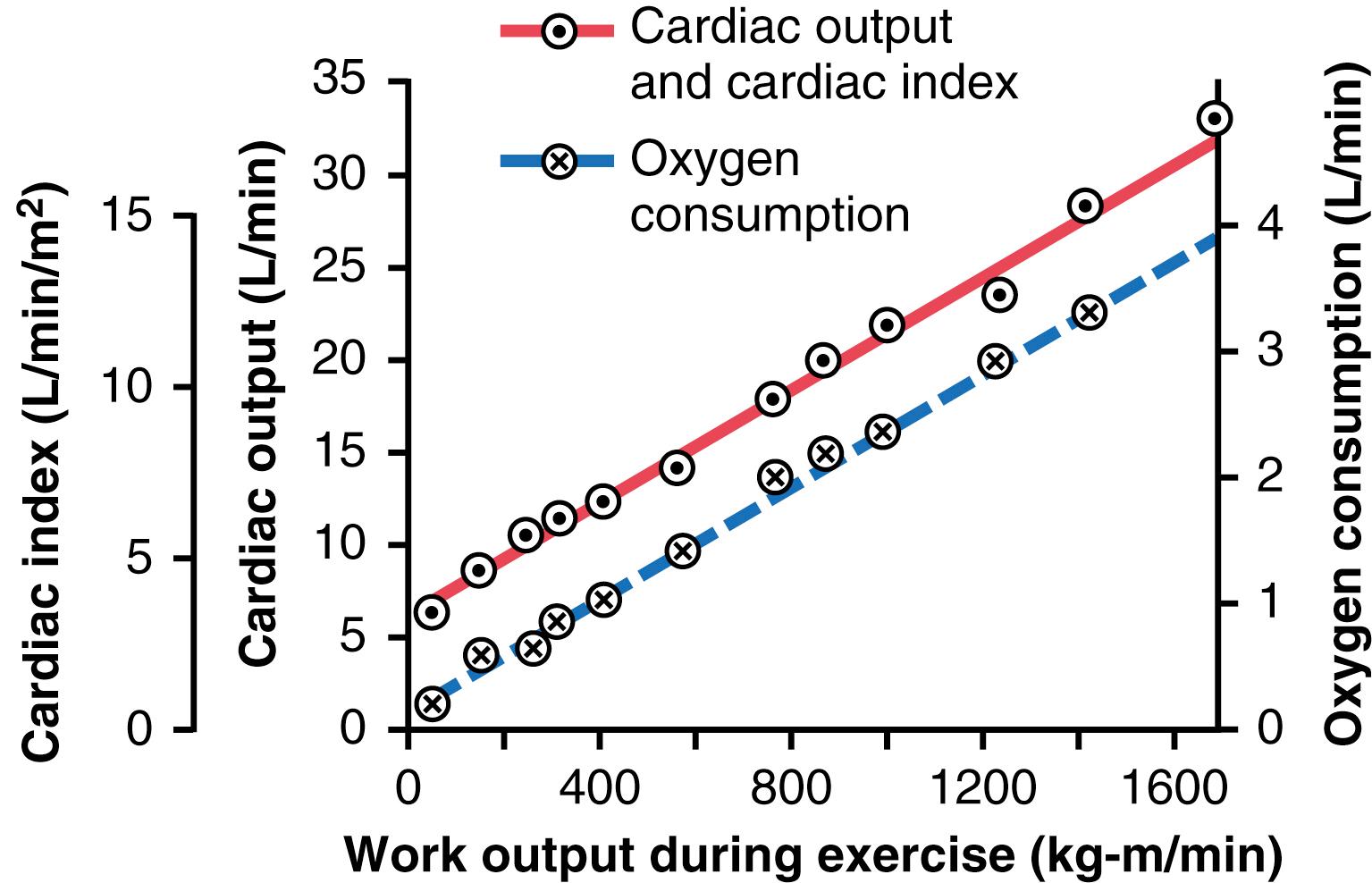
The mechanisms of local blood flow regulation were discussed in Chapter 17 . In most tissues, blood flow increases mainly in proportion to each tissue’s metabolism. For example, local blood flow almost always increases when tissue oxygen consumption increases; this effect is demonstrated in Figure 20-3 for different levels of exercise. Note that at each increasing level of work output during exercise, oxygen consumption and cardiac output increase in parallel to each other.
To summarize, cardiac output is usually determined by the sum of all the various factors throughout the body that control local blood flow. All the local blood flows summate to form the venous return, and the heart automatically pumps this returning blood back into the arteries to flow around the system again.
Figure 20-3 is the same as Figure 19-5 . It is repeated here to illustrate an extremely important principle in cardiac output control: Under many conditions, the long-term cardiac output level varies reciprocally with changes in total peripheral vascular resistance as long as the arterial pressure is unchanged. Note in Figure 20-4 that when the total peripheral resistance is exactly normal (at the 100% mark in the figure), the cardiac output is also normal. Then, when the total peripheral resistance increases above normal, the cardiac output falls; conversely, when the total peripheral resistance decreases, the cardiac output increases. One can easily understand this phenomenon by reconsidering one of the forms of Ohm’s law, as expressed in Chapter 14 :
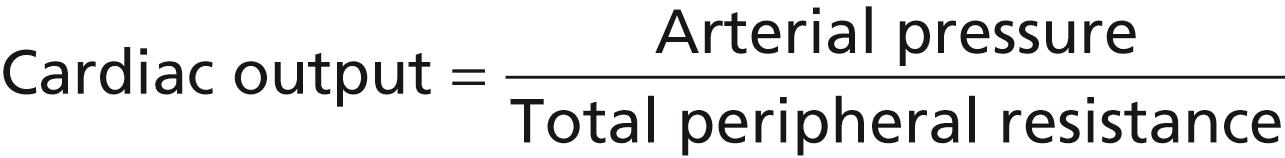
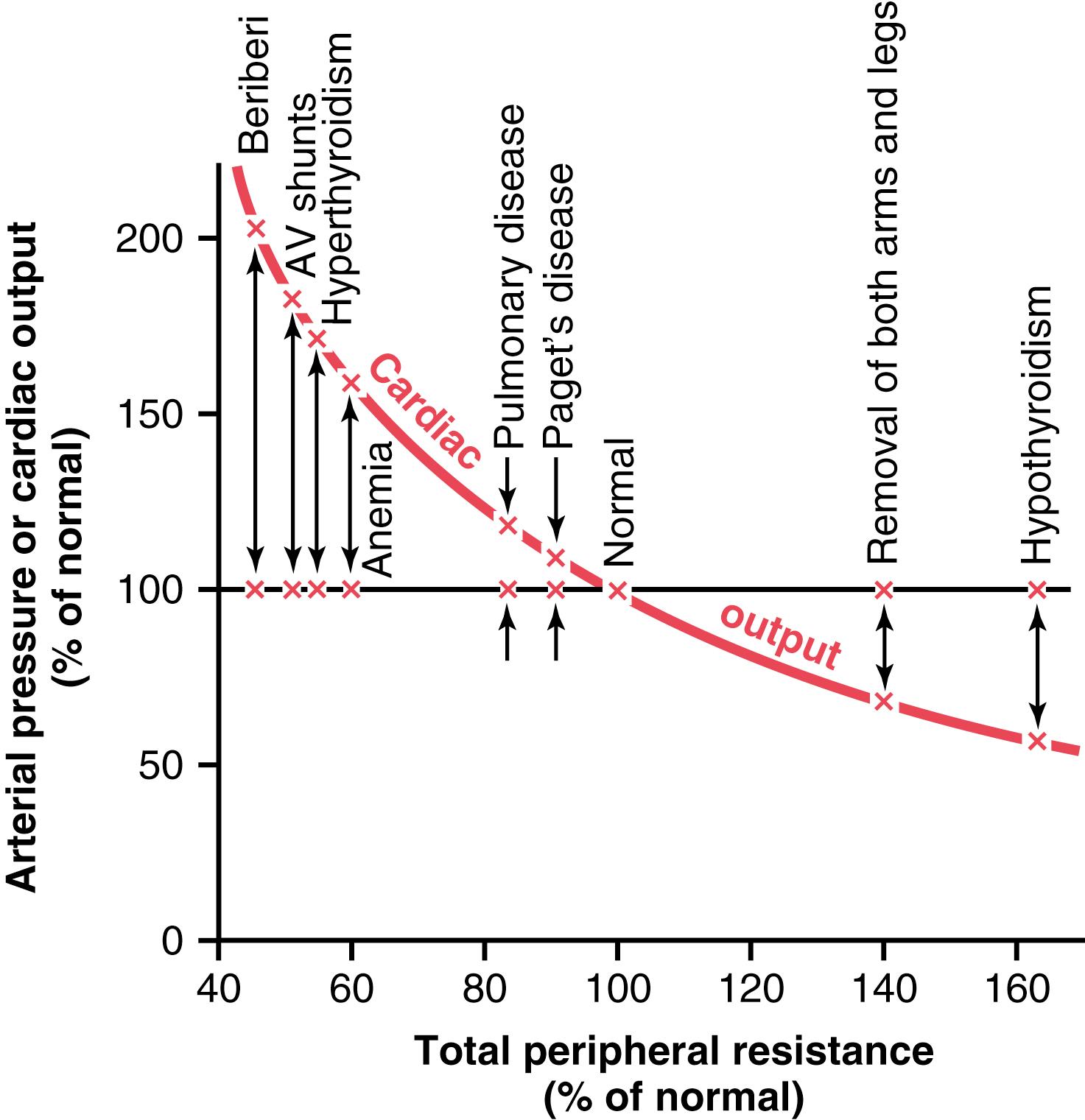
Thus, any time the long-term level of total peripheral resistance changes (but no other functions of the circulation change), the cardiac output changes quantitatively in exactly the opposite direction.
There are definite limits to the amount of blood that the heart can pump, which can be expressed quantitatively in the form of cardiac output curves .
Figure 20-5 demonstrates the normal cardiac output curve , showing the cardiac output per minute at each level of right atrial pressure. This is one type of cardiac function curve , which was discussed in Chapter 9 . Note that the plateau level of this normal cardiac output curve is about 13 L/min, 2.5 times the normal cardiac output of about 5 L/min. This means that the normal human heart, functioning without any special stimulation, can pump a venous return up to about 2.5 times the normal venous return before the heart becomes a limiting factor in the control of cardiac output.
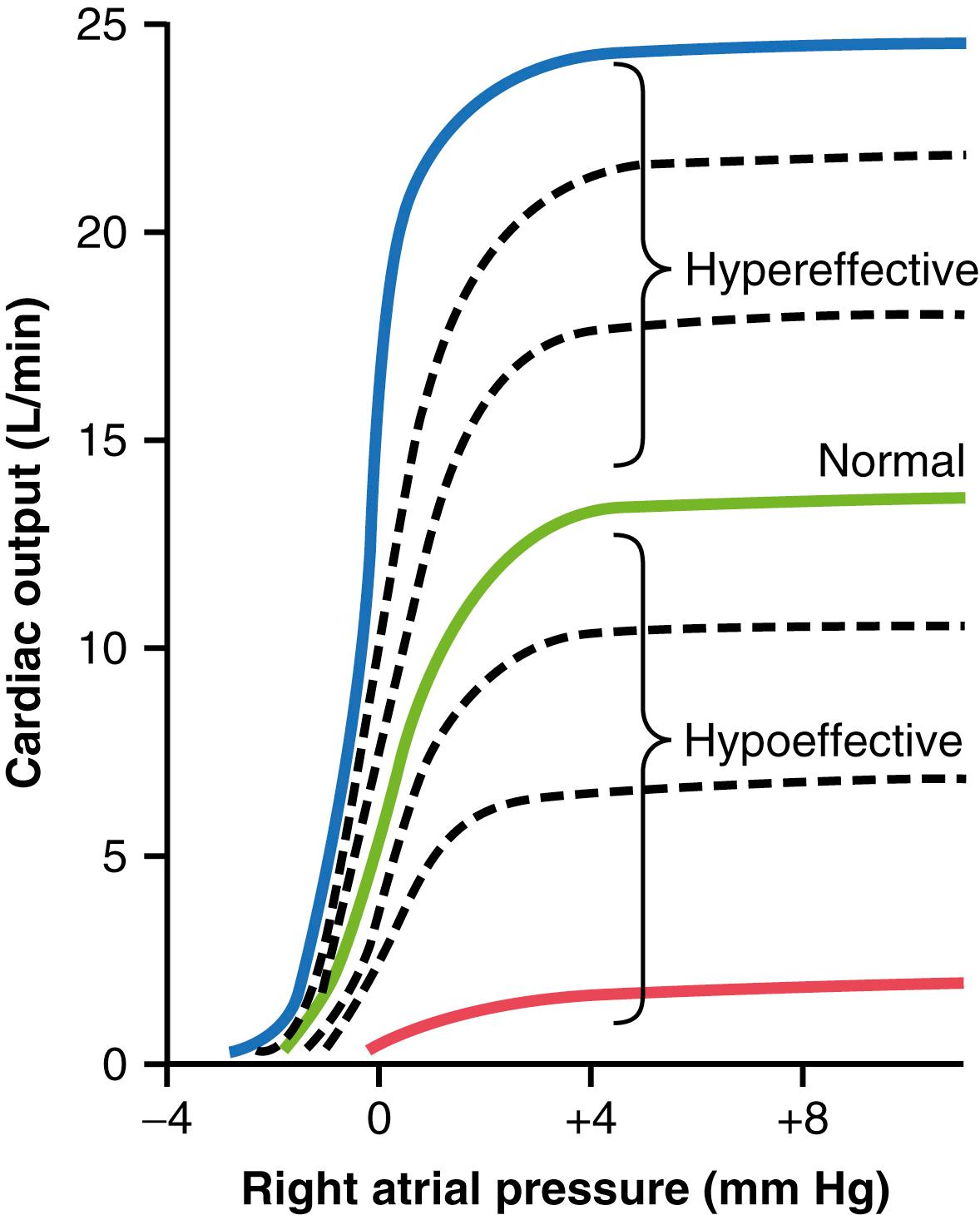
Shown in Figure 20-5 are several other cardiac output curves for hearts that are not pumping normally. The uppermost curves are for hypereffective hearts that are pumping better than normal. The lowermost curves are for hypoeffective hearts that are pumping at levels below normal.
Two general types of factors that can make the heart a stronger pump than normal are nervous stimulation and hypertrophy of the heart muscle.
In Chapter 9 , we saw that a combination of sympathetic stimulation and parasympathetic inhibition does two things to increase the pumping effectiveness of the heart: (1) it greatly increases the heart rate—sometimes, in young people, from the normal level of 72 beats/min up to 180 to 200 beats/min—and (2) it increases the strength of heart contraction (called increased contractility ) to twice its normal strength. Combining these two effects, maximal nervous excitation of the heart can raise the plateau level of the cardiac output curve to almost twice the plateau of the normal curve, as shown by the 25-L/min level of the uppermost curve in Figure 20-5 .
A long-term increased workload, but not so much excess load that it damages the heart, causes the heart muscle to increase in mass and contractile strength in the same way that heavy exercise causes skeletal muscles to hypertrophy. For example, the hearts of marathon runners may be increased in mass by 50% to 75%. This factor increases the plateau level of the cardiac output curve, sometimes 60% to 100%, and therefore allows the heart to pump much greater than the usual amounts of cardiac output.
When one combines nervous excitation of the heart and hypertrophy, as occurs in marathon runners, the total effect can allow the heart to pump as much 30 to 40 L/min, about 2.5 times the level that can be achieved in the average person. This increased level of pumping is one of the most important factors in determining the runner’s running time.
Any factor that decreases the heart’s ability to pump blood causes hypoeffectivity. Some of the factors that can decrease the heart’s ability to pump blood are the following:
Increased arterial pressure against which the heart must pump, such as in severe hypertension
Inhibition of nervous excitation of the heart
Pathological factors that cause abnormal heart rhythm or rate of heartbeat
Coronary artery blockage, causing a heart attack
Valvular heart disease
Congenital heart disease
Myocarditis, an inflammation of the heart muscle
Cardiac hypoxia
Figure 20-6 shows an important difference in cardiac output control with and without a functioning autonomic nervous system. The solid curves demonstrate the effect in the normal dog of intense dilation of the peripheral blood vessels caused by administering the drug dinitrophenol, which increased the metabolism of virtually all tissues of the body about fourfold. With nervous control mechanisms intact, dilating all the peripheral blood vessels caused almost no change in arterial pressure but increased the cardiac output almost fourfold. However, after autonomic control of the nervous system was blocked, vasodilation of the blood vessels with dinitrophenol (dashed curves) then caused a profound fall in arterial pressure to about one-half normal, and the cardiac output increased only 1.6-fold instead of fourfold.
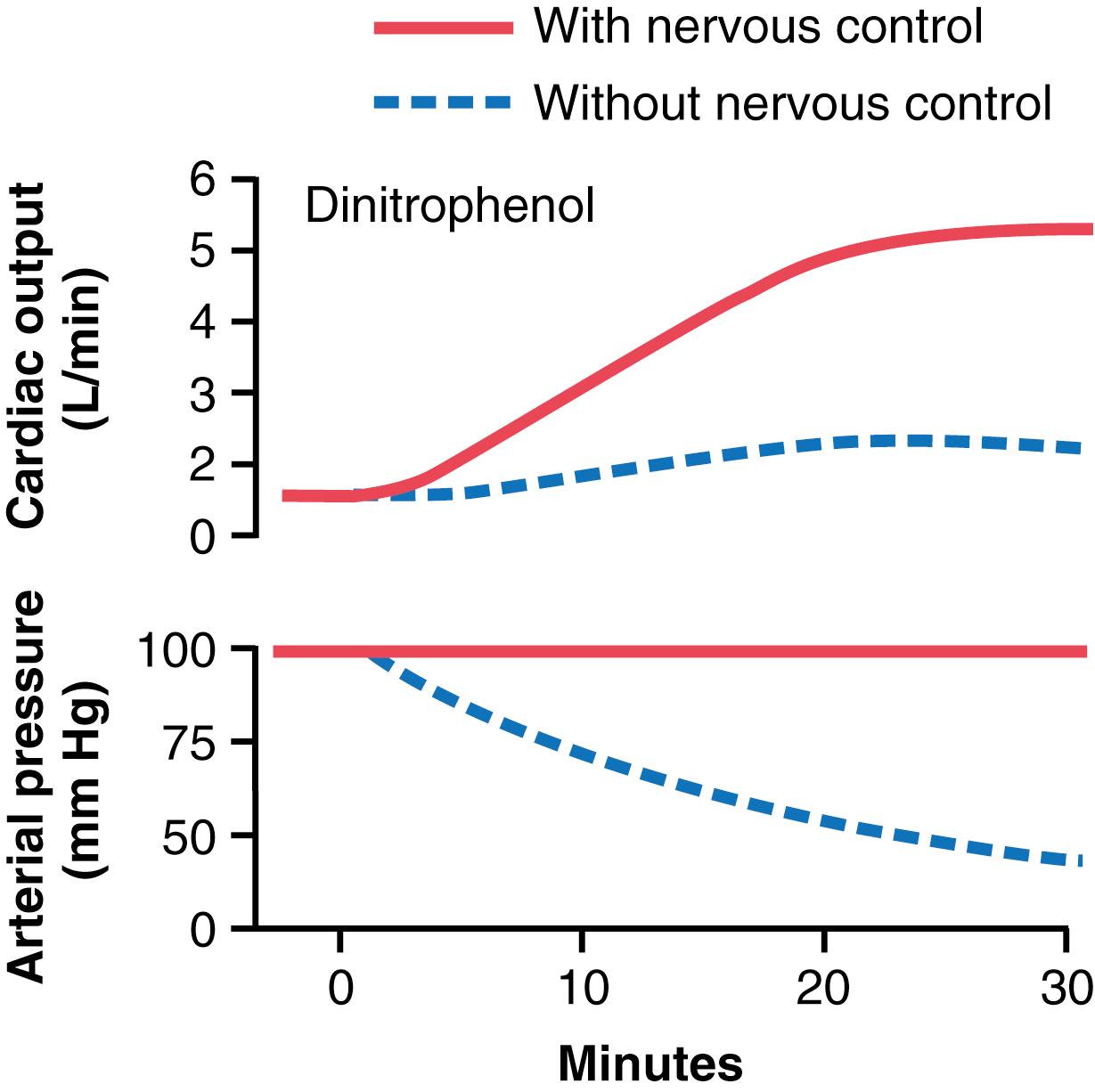
Thus, maintenance of a normal arterial pressure by the nervous system reflexes, by mechanisms explained in Chapter 18 , is essential to achieve high cardiac outputs when the peripheral tissues dilate their blood vessels to increase the venous return.
During exercise, intense increases in metabolism in active skeletal muscles cause relaxation of muscle arterioles to allow adequate oxygen and other nutrients needed to sustain muscle contraction. This greatly decreases the total peripheral resistance, which normally would decrease the arterial pressure as well. However, the nervous system immediately compensates. The same brain activity that sends motor signals to the muscles sends simultaneous signals into the autonomic nervous centers of the brain to excite circulatory activity, causing large vein constriction, increased heart rate, and increased contractility of the heart. All these changes acting together increase the arterial pressure above normal, which in turn forces still more blood flow through the active muscles.
In summary, when local tissue blood vessels dilate and increase venous return and cardiac output above normal, the nervous system plays a key role in preventing the arterial pressure from falling to disastrously low levels. During exercise, the nervous system goes even further, providing additional signals to raise the arterial pressure above normal, which serves to increase the cardiac output an extra 30% to 100%.
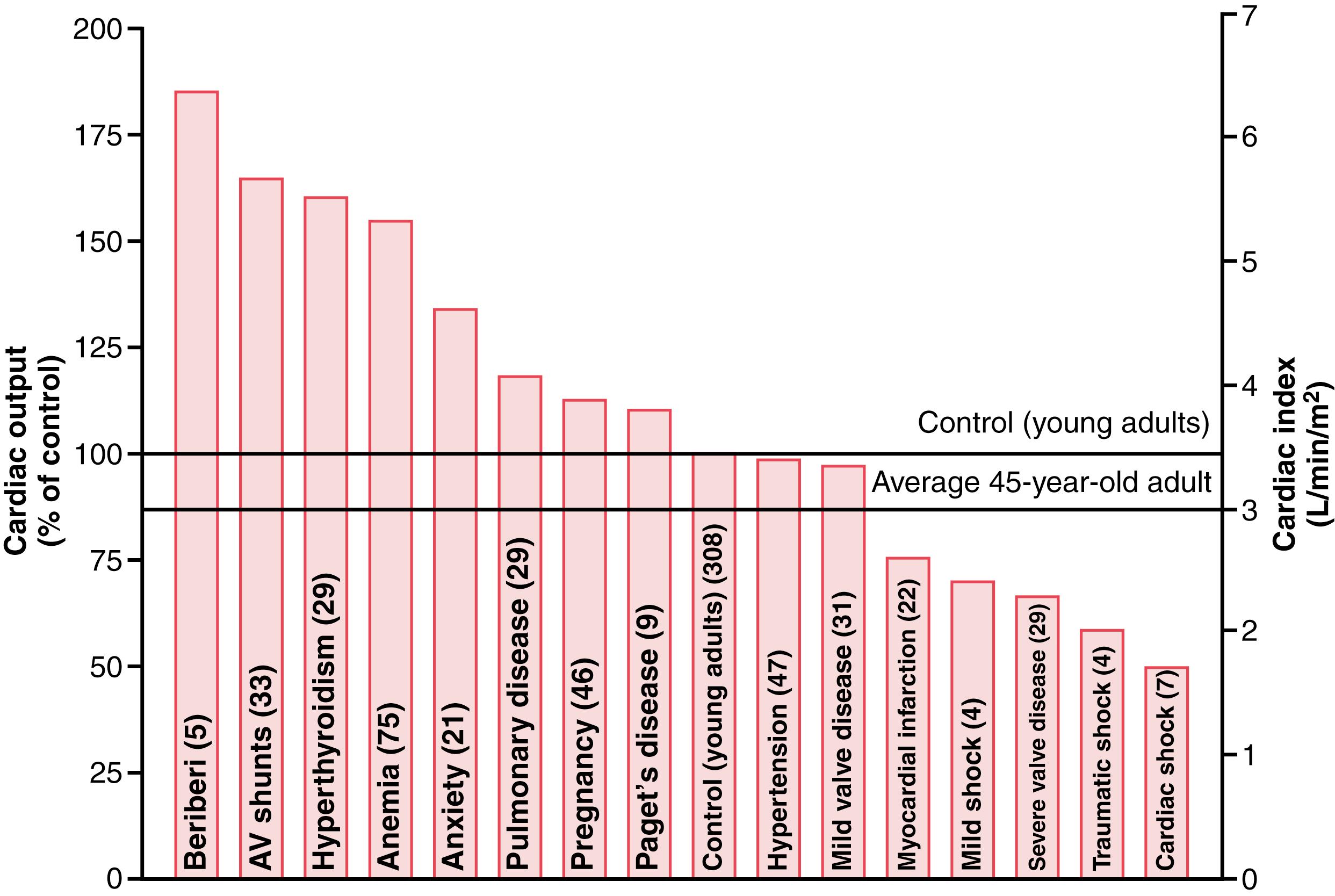
Multiple clinical abnormalities can cause either high or low cardiac outputs. Some of the more important of these abnormal cardiac outputs are shown in Figure 20-7 .
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here