Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Pancreatic adenocarcinoma is the fourth leading cause of cancer-related death.
The overall 5-year survival rate for all patients is less than 5%: 15% to 20% of patients present with resectable or borderline resectable disease with a median survival period of 20 to 24 months, 25% to 30% present with locally advanced or unresectable disease with a median survival period of 8 to 14 months, and 50% to 60% present with metastatic disease with median survival period of 6 to 12 months.
An estimated 10% to 15% of pancreatic adenocarcinomas are attributable to genetic causes. Pancreatic cancer aggregates in some families, and approximately 5% to 10% of individuals with pancreatic cancer have a family history of the disease. Familial atypical multiple-mole melanoma syndrome, hereditary pancreatitis, Peutz-Jeghers syndrome, and a strong family history of pancreatic cancer are the strongest risk factors, and these patients should undergo genetic testing and screening. Risk factors also include smoking, heavy alcohol consumption, chronic pancreatitis, obesity, and diabetes.
Screening of the general population is not indicated at this time.
Mutations in the KRAS oncogene and the CDKN2A tumor suppressor gene are found in more than 80% of pancreatic tumors and are thought to be early mutations. Inactivation of tumor suppressor genes TP53 and SMAD4 are thought to occur later in the tumorigenesis process.
Pancreatic intraepithelial neoplasms (PanINs) are microscopic precursor lesions. PanIN-3 lesions should be fully resected when found. Intraductal papillary mucinous neoplasms (IPMNs) and mucinous cystic neoplasms (MCNs) are noninflammatory cysts that can lead to pancreatic cancer. All MCNs, main duct IPMNs, and symptomatic branch duct IPMNs should be resected.
Jaundice, abdominal pain, malabsorption, weight loss, back pain, and nausea and vomiting are common manifesting symptoms.
Computed tomography with three-dimensional reconstruction (or magnetic resonance imaging) should be used for diagnosing and staging. Endoscopic ultrasonography may offer additional staging information. It is critical to determine resectability on imaging because it will determine the course of treatment.
All patients should be evaluated in a multidisciplinary setting when possible.
Surgery should be considered upfront in patients with resectable disease unless treated on a neoadjuvant clinical trial.
Patients should receive adjuvant 5-fluorouracil (5-FU)– or gemcitabine-based chemotherapy with 5-FU– or gemcitabine-based chemoradiation when appropriate as adjuvant therapy leads to longer survivals.
Neoadjuvant chemotherapy followed by chemoradiation can be given in patients with borderline resectable disease to increase the likelihood of R0 resections, treat micrometastatic disease earlier, and avoid surgery in patients who demonstrate early progression.
Locally advanced and metastatic disease patients can be treated with the same systemic chemotherapy regimens.
Chemoradiation or stereotactic body radiotherapy can be considered for locally advanced patients with good performance status if there is no disease progression after initial systemic chemotherapy.
Palliative measures should be introduced early for advanced patients and focus on relieving pain, biliary obstruction, gastric outlet obstruction, and malnutrition.
Additional studies are needed to evaluate the ability of novel biomarkers to guide pancreatic cancer management.
Pancreatic adenocarcinoma (PC) has one of the highest incidence-to-mortality ratios of any disease. Although it represents the 10th leading cause of cancer in the United States, it is the 4th leading cause of cancer-related death because the vast majority of patients die from their disease. The overall 5-year survival rate for all patients with PC is less than 5%. This is in part because there is no appropriate screening test for the general population, and manifesting symptoms are vague. After patients are diagnosed, only 15% to 20% of patients present with resectable, potentially curable, disease. Even when detected at an early resectable stage, the median survival period is 20 to 24 months with a 5-year survival rate of 15% to 20%. The majority of patients have disease that eventually recurs despite surgery and chemotherapy. PC demonstrates complex biological features, presents with aggressive growth, and is poorly responsive to chemotherapy. Patients with locally advanced (25% to 30% at presentation) and metastatic disease (50%–60% at presentation) have median survival times of 8 to 14 months and 4 to 6 months, respectively. Some of the more recent trials with combination chemotherapy regimens provide some promise with improved survival in selected patients. Because many patients develop biliary obstruction, diarrhea, pain, and malnutrition, palliative care can provide great benefit. Although there has been improved understanding in the biology of PC, translating in some modest survival improvements, there are still significant gaps of understanding that must be identified to advance the treatment of this disease. This chapter reviews carcinoma of the exocrine pancreas, the most common form of cancers of the pancreas.
Pancreatic adenocarcinoma is the fourth most common cause of cancer-related death among US men and women. In 2017, it was predicted that there would be an estimated 53,670 new cases of exocrine PC and 43,090 deaths from PC in the United States. Worldwide, there are more than 278,600 new cases and more than 266,600 deaths per year, with an average of 4.1 new cases per year per 100,000 people. This rate does vary according to location, with more developed regions having a higher rate of 13.5 on average (Japan, Czech Republic, Hungary, and Finland have the highest rate of 18) compared with an average rate of 2 for less developed regions (Africa and South-Central Asia have the lowest with <1 new case). These numbers are expected to increase as the world's population grows and ages. The male-to-female ratio is virtually identical, with only a slight male predominance. The median age at diagnosis is 72 years in the United States, with more than 66% of cases being diagnosed at an age older than 65 years. Only 2.6% of cases are diagnosed in individuals younger than the age of 45 years, and it is virtually never found in children. There are some racial disparities in the United States because there is a slightly higher incidence in African Americans (17.5 new cases/year per 100,000 people) compared with whites (13.5 new cases), Hispanics (11.4 new cases), and Asians (10.6 new cases; all incidences reported for men), and the age of diagnosis is younger in the African American and Hispanic groups.
Numerous risk factors have been identified that aid in preventive measures ( Table 78.1 ). Cigarette smoking is the most preventable risk factor. The risk increases with longer duration and higher number of cigarettes smoked but can return to normal after 10 years of cessation. Cigarette smoke includes more than 50 carcinogens, the most important being nitrosamines, which promote tumor growth via various pathways, including activating the KRAS oncogene, and cause inflammation in the pancreas. It also contributes to local immune inhibitory environment. It is believed to cause 15% to 25% of cases of PC, with a relative risk of 1.5- to 3-fold in smokers compared with nonsmokers. The risk is particularly high in heavy smokers who also have homozygous deletions of the gene for the carcinogen-metabolizing enzyme glutathione S-transferase T1 (GSTT1). Chronic pancreatitis, often the result of chronic and heavy alcohol consumption or biliary duct blockages, leads to an increased risk of 2- to 16-fold, although fewer than 5% of patients with chronic pancreatitis will develop PC. Chronic inflammation is thought to activate macrophages that produce cytokines that induce cell proliferation, angiogenesis, and inhibit apoptosis. Chronic pancreatitis may also be a manifesting symptom of PC from biliary obstruction caused by the tumor. Consequently, PC should be in the differential for a person who develops pancreatitis without any known risk factor. Hereditary pancreatitis is caused by an autosomal dominant mutation in PRSS1 leading to premature activation of trypsin while still in the pancreas or a mutation in SPINK1 or CFTR in the autosomal-recessive form. These patients have a 40- to 85-fold increased risk and a cumulative risk of 30% to 55% of developing PC in their lifetime. Alcohol is a clear risk factor for cancers of the upper aerodigestive tract, including PC; however, it appears that only heavy alcohol use, defined as three or more alcoholic drinks per day, has a slightly increased relative risk of 1.2, but mild or moderate intake poses no increased risk. Obesity, defined as body mass index equal to or greater than 30 and accounting for 33% of adults in the United States, may lead to an increased risk of 1.2- to 1.7-fold and possibly higher in severely obese individuals. This may result from increased circulating insulin and insulin growth factors, lower amounts of antiinflammatory cytokines, and a chronic low-grade inflammatory state throughout the bodies of obese people.
| Risk Factor | Relative Increase in Risk |
|---|---|
| HIGH RISK (>10-FOLD) | |
| FAMMM | 13- to 47-fold |
| Hereditary pancreatitis | 50- to 83-fold |
| Peutz-Jeghers syndrome | 132-fold |
| Three or more first-degree relatives with PC | 14- to 32-fold |
| MODERATE RISK (5- TO 10-FOLD) | |
| Two first-degree relatives with PC | 4- to 6.4-fold |
| Cystic fibrosis | 5.3-fold |
| Chronic pancreatitis | 2- to 19-fold |
| BRCA2 mutation carrier | 3.5- to 10-fold |
| PALB2 mutation carrier | 6-fold |
| LOW RISK (<5-FOLD) | |
| Cigarette smoking | 1.5- to 3-fold |
| Alcohol consumption | None to 1.2-fold |
| Obesity | None to 1.7-fold |
| Diabetes mellitus | 1.3- to 2.6-fold |
| One first-degree relative with PC | 3-fold |
| BRCA1 mutation carrier | None to 2-fold |
| Familial adenomatous polyposis | 4-fold |
| Li-Fraumeni syndrome | 2-fold |
| Lynch syndrome | 2- to 8-fold |
The relationship between diabetes mellitus and PC is difficult to ascertain because type 2 diabetes can be both an early sign of PC and a risk factor. PC is thought to lead to diabetes through destruction of glands causing decreased production of insulin; however, the presence of diabetes does not appear to correlate with the size or stage of the tumor. Long-term diabetes is thought to increase the risk for PC because the increased secretion of insulin and insulinlike growth factors promote cell growth and the heightened state of inflammation leads to proinflammatory cytokines that contribute to angiogenesis and tumorigenesis. Studies have demonstrated that 55% to 85% of patients with PC are diagnosed with glucose intolerance or diabetes either concurrently or within the 2 years preceding their cancer diagnosis. But given the very high incidence of diabetes in the population, the relative risk of developing PC is still only 1.3- to 2.6-fold above normal, when considered independently of obesity, and does not imply that all newly diagnosed diabetic patients warrant screening for PC. However, it should be considered in the atypical patient with newly diagnosed diabetes who has a steady or decreased weight, no change in activity, and no family history of diabetes. Diets high in animal protein, history of gallstones, Helicobacter pylori infection, and some occupational exposures may lead to an increased risk. ABO blood type has also been associated with a risk of several gastrointestinal (GI) malignancies, including PC Compared with blood group O, individuals with non-O blood group (type A, AB, or B) were significantly more likely to develop PC. These findings are supported by the results of a genome-wide association study that identified variants in the ABO locus that were associated with susceptibility to PC.
Allergies such as hay fever; increased vitamin D intake; and diets high in fruits, vegetables, and citrus fruits may have a protective effect. Patients with intraductal papillary mucinous neoplasm of the pancreas (IPMN), which is the most common type of neoplastic pancreatic cyst, are at risk for malignant degeneration, and are commonly managed with surveillance. When an IPMN develops invasive malignancy, it is usually referred as IPMN-associated adenocarcinoma. These patients are also at risk of developing PC (concurrent or distinct ductal adenocarcinoma), which arises away from the cyst, suggesting the existence of a pancreatic field defect. This phenomenon has been described in 2% to 9% of patients who are being followed for IPMN.
Although the majority of PC are sporadic, 5% to 10% of patients have a family history. Familial PCs are defined as two or more first-degree relatives with the disease. Having one first-degree relative with PC gives a person a 3-fold increased risk, two first-degree relatives has a 4- to 6.4-fold increase risk, and three or more first-degree relatives poses a 14- to 32-fold increased risk. Although some patients with familial PC do not have identifiable genes, many syndromes have been described. Carriers of the BRCA2 gene (associated with breast, ovarian, and pancreatic cancers) have a 3.5- to 10-fold increased risk and account for 5% to 17% of families with familial PC. Mutations in PALB2 (binds to BRCA2 ) carry a sixfold increased risk, and BRCA1 carriers may have a twofold increased risk. Germline mutations in STK11 cause the autosomal dominant Peutz-Jeghers syndrome, characterized by hamartomatous polyps, pigmented macules, and a more than 90% chance of developing some form of cancer, including a 132-fold increased risk for PC. Familial atypical mole-multiple melanoma patients typically have a mutation in CDKN2A and carry a 13- to 47-fold increased risk of PC. Germline mutations in DNA mismatch repair genes causing Lynch syndrome carry a two- to eightfold increased risk. Cystic fibrosis, characterized by a mutation in CFTR that produces viscous mucus that obstructs pancreatic ducts, carries an increased risk of 5.3-fold, and those with familial adenomatous polyposis (germline mutation in APC gene) have a 4-fold increased risk. Mutations in the tumor suppressor gene TP53 causing Li-Fraumeni syndrome result in a doubling of the risk.
Pancreatic adenocarcinoma is a genetic disease that is caused by inherited and acquired mutations in specific cancer-associated genes. The sequencing of the protein-coding exons from 20,661 genes in 24 advanced PC provided understanding of the key signaling pathways that are dysregulated in pancreatic tumorigenesis. Several oncogenes and tumor suppressor genes are involved in the development of PC both by contributing to the growth of the tumor itself as well as to the support cells.
Oncogenes, typically inactive in the normal cell, cause uncontrolled cell proliferation by inhibiting apoptosis and activating the cell cycle when mutations make them constitutively active. The KRAS gene, located on chromosome 12p, is one of the most frequent oncogene mutated in PC. KRAS mutation occur in more than 90% of PC tumors and encodes a membrane-bound protein that has guanosine triphosphatase activity and is involved in signal transduction. When mutated, it becomes constitutively active, independent of growth factors, leading to chronic activation of its downstream pathways PI3K, MAPK , and RAF , causing inhibition of apoptosis, activation of the cell cycle, migration, angiogenesis, cytoskeleton remodeling, and unchecked proliferation. When the AKT1 oncogene is activated through phosphorylation in the PTEN/PI3K/AKT pathway, it helps the cancer cells overcome cell-cycle arrest, blocks apoptosis, and promotes angiogenesis. Other oncogenes that are mutated in some PCs include BRAF (in KRAS wild-type tumors), MYC, MYB, and AKT2 .
Tumor suppressor genes, normally active, act in the opposite manner by activating apoptosis and inhibiting cell proliferation. Tumor suppressor genes can be silenced when mutations make them inactive. CDKN2A , a cell-cycle control gene, is the most commonly inactivated tumor suppressor gene in PC (lost in 80% to 95% of cases), leading to increased cell-cycle progression. TP53 is activated when there is DNA damage to either stop the cell cycle and repair the DNA or initiate apoptosis. Mutations in this tumor suppressor gene are found in 50% to 75% of tumors. Inactivation of SMAD4 ( DPC4 ), involved in regulating cell cycle progression through the TGFB pathway, is seen in more than 50% of PC and is associated with worse prognosis and the development of metastases. Inactivation of RB1, in less than 10% of PC, and STK11, responsible for Peutz-Jeghers syndrome, is also seen. Other genes that have been demonstrated to be abnormal include the overexpression of insulin-like growth factor 1 (IGF1), which leads to the abnormal activation of many downstream pathways, CDKN1A and CDKN1B mutations that cause loss of regulation at G1 checkpoint, EGFR TGFB mutations causing activation of MAPK pathway, and overexpression of ERBB2 (HER2/neu) .
DNA mismatch repair genes such as hMLH1 and hMSH2 play an important role in the pathogenesis of Lynch syndrome (hereditary nonpolyposis colorectal cancer syndrome). Patients with Lynch syndrome have inherited (germline) mutations in one of several DNA mismatch repair genes and an elevated risk of several GI cancers, including PC. DNA mismatch repair genes are mutated in approximately 4% of cases of PC. Early studies suggested patients with DNA mismatch repair genes mutations may be more susceptible to immunotherapy.
Epigenetic modification, the process by which gene expression is silenced by aberrant promoter methylation, also has a role in PC tumorigenesis. DNA methylation and histone modification are two examples of this. Among the genes that can be silenced in this manner in PC are UCHL1 , NPTX2, SARP2, CLDN5 , REPRIMO (RPRM), LHX1, WNT7A, FOXE1, TJP2, CDH3, ST14, and p16/CDKN2A. Conversely, some of the genes that are overexpressed in PC are hypomethylated.
Telomere shortening and overexpression of microRNAs lead to chromosomal instability and dysregulation of gene expression, respectively. In addition to the tumor cells, the tumor microenvironment, composed of stromal cells, inflammatory cells, and endothelial cells, can play a role in PC tumorigenesis. The cancer cells secrete growth factors IGF1, fibroblast growth factor, transforming growth factor–β (TGF-β), vascular endothelial growth factor (VEGF), and platelet-derived growth factor that stimulate the pancreatic stellate cells (also called myofibroblasts) to secrete excess amounts of extracellular matrix. The matrix and its stromal cells in turn secrete cytokines and growth factors that promote cancer cell growth, invasion, and dissemination and protect the cancer cells from apoptosis. TGF-β also leads to a decrease in activity of helper T cells, which suppresses the body's immune system reaction against the abnormal cancer cells.
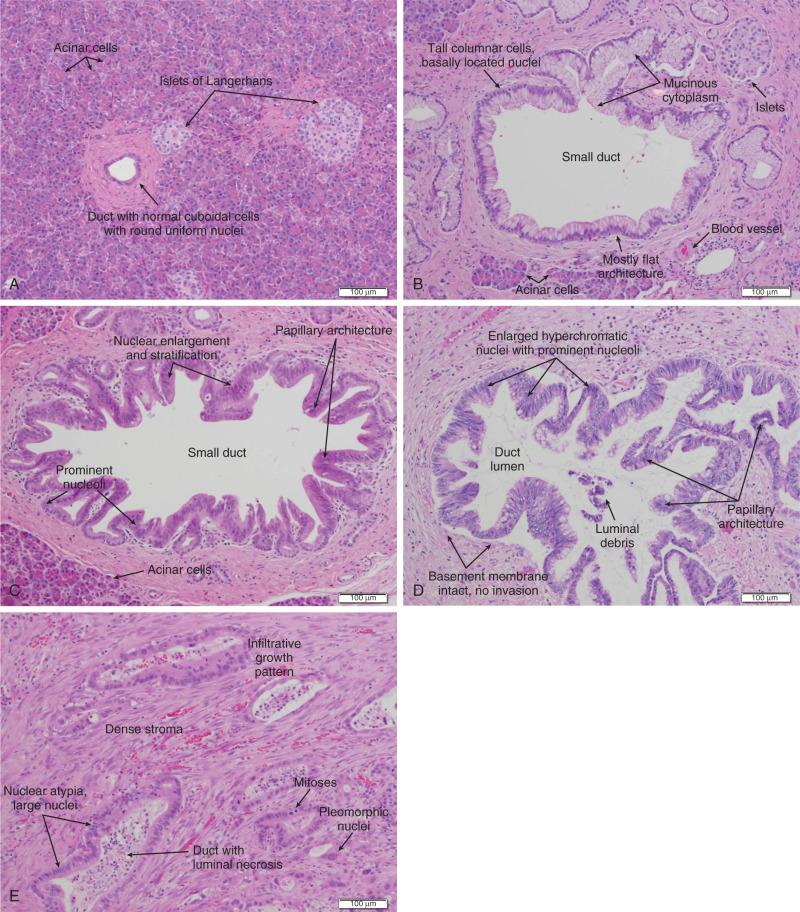
Approximately 85% of PC develops from the ductal epithelial, termed pancreatic ductal adenocarcinoma (PDAC) . PDACs are thought to arise from precursor lesions that include pancreatic intraepithelial neoplasms (PanINs), intraductal papillary mucinous neoplasms (IPMNs), and mucinous cystic neoplasms (MCNs). PanINs, the most common precursor lesions, are grossly visible (typically >10 mm) and are composed of mucin-producing columnar cells. The lesions show papillary proliferation, cyst formation, and varying degrees of cellular atypia. IPMNs may involve the main pancreatic duct, the branch ducts, or both. Whereas patients with branch-duct lesions are at lower risk for developing malignancy (~20% at 10 years), patients with IPMNs involving the main duct are at high risk (~70%). PanINs, are classified from low-grade atypical lesions (PanIN-1A or -1B) to high-grade atypical lesions (PanIN-2 or -3) as molecular alterations accumulate and more dysplasia appears ( Fig. 78.1 ). Over time, these precursor lesions accumulate similar mutations as compared with invasive carcinoma. Activating mutations of the KRAS oncogene are one of the earliest abnormalities in the development of PC because they appear in 30% to 45% of PanIN-1 lesions and more than 90% of PanIN-3 lesions. BRAF mutations are also found in the early precursor lesions in 5% of patients that are wild-type KRAS. Telomere shortening also occurs early and is present in 90% of PanIN-1 lesions and leads to chromosomal instability, making further mutations more likely. Inactivating mutations of CDKN2A begin to occur in PanIN-2 lesions and inactivation of TP53, BRCA2, and SMAD4 are seen in PanIN-3 lesions. Low-grade PanIN lesions are common in older individuals; however, higher grade PanINs are typically seen in association with invasive cancer, especially in those with familial PC. Although all precursor lesions have a risk of progressing to invasive carcinoma, the risk is low for PanIN-1 lesions and increases for PanIN-3 lesions.
Intraductal papillary mucinous neoplasms and MCNs are two types of noninflammatory cysts in the pancreas that are diagnosed secondary to symptoms or from incidental findings on imaging. Cysts are found incidentally on 1.2% to 2.6% of the more than 50 million computed tomography (CT) scans done annually in the United States. Given their malignant potential, recommendations have been developed for their management. IPMNs are grossly visible, mucin-producing, epithelial neoplasms, typically with papillary architecture, that arise from either the main pancreatic duct or branch ducts and are graded according to degree of dysplasia. They range from 5 to 150 mm; are more commonly located in the pancreatic head; and can manifest with abdominal or back pain, weight loss, anorexia, or ductal obstruction from the mucin or the tumor itself. The average age at onset is 65 years, and they have a 2 : 1 male-to-female predominance. Endoscopic ultrasonography (EUS) and endoscopic retrograde cholangiopancreatography (ERCP) can visualize the degree of dilation of the main pancreatic duct to help determine the place of origin. They are less frequent precursors to PC than PanINs but share some of the same molecular aberrations. Whereas KRAS mutations are seen in 50% of low-grade IPMNs, inactivating mutations of CDKN2A and TP53 are seen in high-grade lesions. Whereas loss of SMAD4 is rarely seen in high-grade lesions, mutations of GNAS are commonly seen. IPMNs arising from the branch ducts are less aggressive than those arising from the main duct with rates of malignancy and invasive malignancy (either mucinous noncystic carcinoma/colloid carcinoma or PDAC) of 25% and 15% for branch duct origin and 70% and 43% for main duct origin. Patients with main duct IPMNs should undergo resection. Their 5-year survival rates are 77% to 96% for the noninvasive neoplasms and 40% to 70% in the invasive lesions. Symptomatic patients with branch duct IPMNs have a higher risk of malignancy and should undergo resection. Asymptomatic branch duct IPMNs can be monitored with imaging (every 3 to 12 months depending on size) because they have a 0% to 5% chance of malignancy, especially if there is no main duct dilation and no mural nodules and the neoplasm is smaller than 30 mm. They should be removed if they cause symptoms or increase in size. Patients should be followed even after resection, on a yearly basis for benign IPMNs and twice yearly for invasive IPMNs, to detect recurrence.
Mucinous cystic neoplasms also produce mucin and are characterized by ovarian-type stroma. They are found almost exclusively in women, typically in the fourth and fifth decades of life, and 95% occur in the pancreatic body and tail. They tend to be slow growing, with an average size of 5 to 12.5 cm. They have an orange-like gross appearance and only rarely communicate with the pancreatic duct. All MCNs should be resected because they may progress to mucinous cystadenocarcinomas, which have a poor prognosis. Patients with benign MCNs do not need to be followed after resection because these MCNs do not recur; however, patients with malignant MCNs (6% to 36%) should be followed by imaging every 6 months.
Given the poor outcomes for patients diagnosed with PC, risk factor reduction and early detection are critical. Smoking cessation is the most important preventive measure and is strongly encouraged. Avoidance of heavy alcohol consumption can both reduce the risk of chronic pancreatitis, which is itself a risk factor, and reduce the carcinogens delivered to the pancreas from alcohol. Decreasing the incidence of diabetes by maintaining a healthy weight, a diet high in fruits and vegetables, and regular exercise will lower the risk.
Screening the general population is not indicated given the relatively low incidence of PC and the lack of an inexpensive, accurate, and noninvasive test. To date, there are no biomarkers that have been shown to be appropriate for screening the general population. CA19-9, a sialylated Lewis A blood group antigen, is the most studied biomarker that is expressed and shed in pancreatic and hepatobiliary diseases. Its sensitivity ranges from 80% to 100% and specificity from 68% to 98.5%. Although the positive predictive value is higher in symptomatic individuals, especially when combined with imaging, it cannot be used alone for screening. In patients diagnosed with PC, CA19-9 is often used to predict prognosis and chance of recurrence. It is not a reliable screening tool because it can be elevated from other causes, such as cholestasis, cholangitis, pancreatitis, neuroendocrine tumors, and other GI cancers, and 5% to 10% of people are nonsecretors because they do not express Lewis A antigen. Obstructive jaundice can falsely raise the CA19-9 value.
Individuals who are at high risk for developing PC, on the other hand, are recommended to undergo screening to detect premalignant lesions earlier. The American Cancer of the Pancreas Screening (CAPS) Consortium did a prospective trial screening of high-risk individuals, defined as patients with Peutz-Jeghers syndrome, patients with familial breast–ovarian cancer with at least one affected first- or second-degree relative with PC, and relatives of patients with familial PC with at least one affected first-degree relative. They screened 225 high-risk individuals using CT, magnetic resonance imaging (MRI), and EUS, of which 82 had proven or suspected IPMNs and 3 had pancreatic endocrine tumors. Surgery was offered for suspected pancreatic neoplasms if there were solid masses, main duct or mixed duct IPMNs, or branch duct IPMNs 2 cm or larger or if there were concerning features. MRI and EUS were repeated in 6 to 12 months if lesions were found but no surgery was done and repeated in 1 to 3 years if no mass was found. In the five patients who underwent pancreatectomy, all had high-grade dysplastic IPMN, PanIN, or both but no invasive PC. The CAPS group considered this rate of identifying premalignant conditions adequate and recommended screening for this population starting at age 50 years, 10 years before the earliest incidence in the family, or age 30 years for Peutz-Jeghers syndrome patients. Based on these results, individuals should be considered to be at high risk for hereditary PC if they have any of the following: known genetic syndrome associated with PC, including hereditary breast–ovarian cancer syndrome, familial atypical multiple melanoma and mole syndrome, Peutz-Jeghers syndrome, Lynch syndrome, or other gene mutations associated with an increased risk of PC; two relatives with PC, with one being a first-degree relative; three or more relatives with PC; and hereditary pancreatitis. However, only a subset of high-risk individuals are candidates for screening. Guidelines for screening for PC have been published by several guidelines. The Fourth International Symposium of Inherited Diseases of the Pancreas recommends screening high-risk individuals, defined as patients with greater than a 10-fold risk as per Table 78.1 , as well as patients with three or more PC cases among first-, second-, and third-degree relatives, with at least one being a first-degree relative, and known BRCA1 , BRCA2 , and PALB2 mutation carriers who have at least one first- or second-degree relative with PC. Screening should start at age 45 years or 15 years before the earliest relative's cancer onset and should be done with EUS given its ability to detect pancreatic lesions smaller than 1 cm. Although MRI may be better, it has not been directly compared with EUS, and CT is less reliable for detecting small lesions. Several smaller studies have also demonstrated benefit of screening by finding precursor lesions in 8 of 72 high-risk individuals and 12 of 46 high-risk individuals, but others have shown only minimal yield. Therefore it is first recommended to test affected individuals in kindreds with familial PC for a causative mutation to properly test the unaffected individuals. Second, it is reasonable to screen high-risk individuals as defined per the studies discussed. Table 78.2 summarizes screening recommendations.
| HRIS TO CONSIDER FOR SCREENING |
| FAMMM patients with CDKN2A Patients with hereditary pancreatitis Patients with hereditary PJS Three or more first-, second-, or third-degree relatives with PC with at least one being a first-degree relative Two or more first-degree relatives with PC BRCA1, BRCA2, or PALB2 mutation carriers with at least one first- or second-degree relative with PC |
| AGE TO START SCREENING |
| Age 45–50 years or 15 years before age of earliest occurrence of PC in the family (whichever is earliest) Consider age 30 years for patients with PJS |
The pancreas is composed of both exocrine and endocrine cells. The endocrine cells account for 1% to 2% of the pancreas and form the islets of Langerhans, where they secrete insulin, glucagon, and somatostatin. The exocrine pancreas includes the acinar cells that produce and secrete digestive enzymes in their inactive forms, the cuboidal cells that line the smaller ducts, and the mucin-producing columnar cells that line the larger ducts that carry these enzymes to the duodenum. Fibroblasts, pancreatic stellate cells, endothelial cells, nerves, and inflammatory cells create the stroma surrounding the endocrine and exocrine pancreas.
The commonly used terms “carcinoma of the pancreas” or PC usually refer to ductal adenocarcinoma (including its subtypes), which represents approximately 85% of all pancreatic epithelial neoplasms. Ductal adenocarcinomas arise from the pancreatic head in 60% of cases, the pancreatic body in 15% of cases, the tail in 5%, and diffusely in 20%. Carcinomas arising in the head of the pancreas tend to be diagnosed earlier when they are smaller and less advanced than do tumors in the body and tail because even small neoplasms near the common bile duct or ampulla of Vater can cause biliary obstruction and painless jaundice. Tubular adenocarcinoma subtype is the most common histology; adenosquamous carcinoma, colloid carcinoma, hepatoid carcinoma, medullary carcinoma, signet ring cell carcinoma, undifferentiated carcinoma, and undifferentiated carcinoma with osteoclast-like giant cells are less common variants. Medullary and colloid variants have a better prognosis than the typical tubular adenocarcinoma; adenosquamous and undifferentiated have the worse prognosis. The remaining 15% of pancreatic epithelial neoplasms are composed of serous cystadenomas (1% to 2%), mucinous cystic neoplasms (1% to 2%), IPMNs (3% to 5%), acinar cell carcinomas (1% to 2%), pancreatoblastomas (<1%), pancreatic endocrine neoplasms (3% to 4%), and solid-pseudopapillary neoplasms (1% to 2%). Most PCs are moderately to poorly differentiated, with varying degrees of duct-like structures and mucin production. Histologic grading, which is based on the degree of differentiation and the prevalence of mitotic cells, typically uses three grade levels (grade 1, well differentiated; grade 2, moderately differentiated; and grade 3, poorly differentiated), although highly anaplastic tumors are sometimes designated grade 4.
Invasive PC can spread through local invasion or through perineural, lymphatic, or vascular invasion, producing sites of distant metastasis. Given its location in the retroperitoneum, the most common sites of direct local invasion are to the stomach, duodenum, liver, common bile duct, gallbladder, spleen, superior mesenteric vein (SMV), superior mesenteric artery (SMA), and other surrounding arteries, veins, and lymph nodes. Perineural invasion is defined as the presence of cancer cells along nerves or within the neuronal sheath. Whereas neurotrophins that are secreted by both the cancer cells and the nerve cells help support the survival and growth of these cells and promote neurogenesis, chemokines like CX3CR1 appear to increase the cancer cells’ migration toward the nerve. The head of the pancreas is innervated by the superior mesenteric ganglion, the celiac plexus, and its branches, which are the main routes for perineural invasion by the cancer cells. The main route of spread for cancers of the body and tail is through the celiac plexus and the splenic plexus. Intrapancreatic or extrapancreatic neural invasion is seen in virtually all advanced stage tumors and even in more than 70% to 75% of stage I tumors, implying that this is an early event in the tumor's progression. Given that some studies have reported worse prognosis for patients with perineural invasion, pathologists are now recommended to report the tumor's perineural invasion status. In a retrospective analysis of 193 patients with resected PDACs, those without nodal metastases or perineural invasion had a 5-year survival rate of 75% as compared with 29% of those with perineural invasion. In patients with nodal metastases, the 5-year survival rate was 17% when there was no perineural invasion and only 10% when there was invasion. Perineural invasion is one reason that many PC patients experience difficult-to-control abdominal and back pain.
Vascular invasion is critical for both resectability and prognosis. The head and neck of the pancreas are supplied from superior pancreaticoduodenal arteries arising from the celiac trunk and the inferior pancreaticoduodenal arteries arising from the SMA. These areas drain into the SMV, inferior vena cava (IVC), portal vein, and inferior mesenteric vein. The body and tail are supplied by the splenic artery arising from the celiac trunk and from pancreatic branches off the SMA and mostly drain into the splenic vein. Given their proximity to the pancreas, the SMV and SMA are the most commonly involved artery and vein by the tumor. The celiac artery, splenic artery, portal vein, hepatic artery, and, more rarely, the IVC and aorta can also be involved. On pathologic review of more than 1100 resections, 53% had evidence of vascular invasion.
Lymphatic invasion, specifically nodal involvement, is the strongest predictor for survival. Lymphangiogenesis occurs during embryonic development and again during regeneration after a trauma and is thought to also occur during tumor growth. Tumor cells enter the lymphatic system by either migration through the interendothelial valves or by destroying the vessel walls. They will enter the smaller intralobular lymphatic vessels located within the pancreas and subsequently drain into the four main lymphatic branches of the pancreas: anterior, posterior, inferior, and superior pancreaticoduodenal lymphatic vessels. These then drain into regional lymph nodes that are typically located near larger blood vessels: the celiac artery, common hepatic artery, SMA, and aorta for head or neck tumors and the splenic artery for body or tail tumors. At least 75% of all resections have positive lymph nodes.
Tumor cells travel through the nerves, lymphatics, or vasculature to form distant metastases. The liver is the most common site of metastasis, possibly because tumor cells travel through the portal vein followed by the peritoneal cavity. Lung metastases are the next most common, especially in long-term survivors. In a phase III trial for first-line metastatic PC, 88% of the patients had liver metastases, 24% had lung, 19% had peritoneal, and 14% had other sites. In a second-line therapy trial, 70% had liver disease, 30% had peritoneal, and 17% had lung involvement. Brain and skeletal metastases are quite uncommon, and there have only been case reports of metastases to the appendix, kidneys, skin, prostate, stomach, heart, thyroid, and muscles.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here