Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Metabolism supports biosynthesis, energetics, and cell signaling including chromatin state and epigenetics.
A common feature of each element of malignancy is the necessity to adapt metabolic functions.
Altered metabolism in key metabolic pathways and networks is being exploited clinically for diagnostics and therapeutics.
Old and new therapies target cancer metabolism, and the repurposing of metabolic drugs for cancer therapy is attractive and ongoing.
Future work in the area of cancer metabolism will incorporate the interaction between tumor cells and their environment, germline genetics, liver physiology, the microbiome, and other influences including diet and exercise.
Cancers are diseases in which cells acquire mutations that result in proliferation that occurs outside the context of normal tissue development. These somatic mutations interact with their environment to result in cell transformation. This environment is determined by numerous factors including, but not exclusively, host genetics, lifestyle including diet, host physiology, the state of the immune system, and the microenvironment of the tumor cells. At the nexus of this interaction between genes and environment is cellular metabolism.
Metabolism involves a set of interconnected chemical reactions mediated by enzymes. At the cellular level, nutrients including glucose, lipids, and amino acids that are derived from their constituent dietary macronutrients—carbohydrates, fats, and proteins—are taken up and then transformed through a series of interconnected chemical reactions that comprise the metabolic network ( Fig. 9.1 ). These nutrients are stored in their electron-rich reduced forms and through a process known as catabolism are oxidized. The release of the electrons from these oxidative processes generates energy that is used to sustain all elements of life. Metabolism also allows for the conversion of intermediate products of catabolism to materials used as structural components or building blocks for the production of proteins, nucleic acids, and cell membranes. This is termed anabolism or anabolic metabolism. Metabolism also can communicate directly to other elements of cellular machinery by generating molecules that directly react with and alter the activity of proteins and nucleic acids.
A common feature of each element of malignancy is the necessity to adapt each of these metabolic functions to support the demands of uncontrolled proliferation. Indeed, differential metabolic requirements manifest during each cancer-associated process such as anoikis, invasion, and metastasis. This metabolic programming comes from both the oncogenic signaling that drives distinct metabolic processes and the environmental factors such as the tissue vasculature and the nutrient content of serum. Furthermore, metabolic enzymes, by virtue of their design and particularly their binding pocket, which encapsulates small molecules, are readily druggable. In addition, metabolism may be manipulated by lifestyle factors such as diet and exercise. Thus there is tremendous opportunity to exploit metabolism for cancer prevention and therapy.
This chapter discusses the fundamentals of metabolic reprogramming and adaptation in cancer cells and outlines both the principles that lead to this altered metabolism and the specific requirements that result. Particular attention will be paid to key metabolic pathways and networks and to areas that have direct clinical application such as current antimetabolite chemotherapy agents and ongoing drug development efforts. Our hope is to give the reader a broad overview of this rapidly progressing area of cancer biology and medical oncology.
In conditions with sufficient oxygen, terminally differentiated cells usually metabolize glucose through three highly regulated sequences of enzymatic processes: glycolysis, the tricarboxylic acid (TCA) cycle, and the electron transport chain (ETC). On complete oxidation, one molecule of glucose can ultimately generate approximately 36 units of the energy-storing molecule adenosine 5′-triphosphate (ATP) and other energy-rich metabolic currency such as reduced nicotinamide adenine dinucleotide (NADH). These processes are compartmentalized: glycolysis in the cytosol, and the TCA cycle and ETC in the mitochondria. Under conditions of oxygen limitation such as exercise in muscle, the end product of glycolysis (pyruvate) is diverted away from the mitochondria to produce the fermentation product lactate. This is known as anaerobic glycolysis and generates only two net ATP molecules per molecule of glucose while consuming NADH (produces oxidized nicotinamide adenine dinucleotide [NAD + ]), and is a common form of glucose metabolism for unicellular organisms such as certain yeasts and parasites. Although this may seem less efficient for mammalian cells, the rate of ATP production via glycolysis can be much faster than the time it takes for mitochondrial respiration; therefore in some cases greater amounts of ATP can be generated from glycolysis in a given amount of time in the presence of abundant glucose.
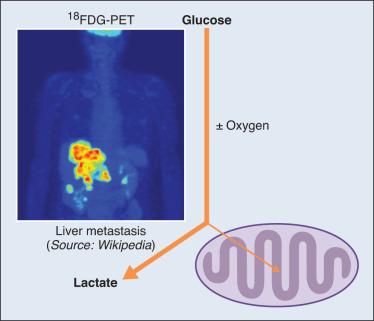
One of the first documented points of evidence for an altered molecular property in tumors was the seminal observation made by Otto Warburg and colleagues in 1924 regarding the tumor cell–specific fate of glucose ( Fig. 9.2 ). The essential features of what came to be defined as the “Warburg effect” were the observations that neoplastic cells consumed large amounts of glucose and fermented it into lactate. It was also found that this occurred even in the presence of abundant oxygen; thus this phenomenon is commonly referred to as aerobic glycolysis, and Warburg hypothesized that killing cancer cells would require depleting both glucose and oxygen. These initial findings have been conclusively validated by genetic and pharmacologic studies, but not all cancers undergo or require aerobic glycolysis. Moreover, nontransformed proliferative cell types such as lymphocytes and fibroblasts use aerobic glycolysis for normal function. Nonetheless, the Warburg effect in tumors is generally broad and has been exploited clinically for many years through imaging of glucose uptake (discussed later in further detail) for diagnosis and monitoring of treatment progress in numerous cancers including lymphomas, breast cancer, non–small cell lung cancer (NSCLC), esophageal cancer, and colorectal cancer.
Several hypotheses as to why cancer cells favor what seems like a wasteful process have been proposed. Warburg and colleagues eventually concluded it was due to defective mitochondria, but many cancer cells in fact use diverse mitochondrial metabolic functions for growth advantages, which are discussed in detail later. One proposal for why cancer cells undergo the Warburg effect is the need for rapid production of ATP, and as mentioned previously this can be achieved by enhanced glycolysis. In support of this, it has been demonstrated that cells upregulate aerobic glycolysis when challenged with conditions that require generation of large amounts of ATP while oxidative phosphorylation remains constant. However, mathematical calculations indicate that the amount of ATP required for cell growth and division may be less than the amount required for normal cell survival, suggesting that ATP may not be a limiting factor in cancer cell proliferation. Another model hypothesizes that the Warburg effect is important for generating biomass in the form of donating carbons for biosynthetic processes. For example, the enzyme phosphoglycerate dehydrogenase (PHGDH) diverts glucose carbons away from glycolysis into the serine biosynthetic pathway, which is important for one-carbon metabolism and nucleotide synthesis (discussed later), but it remains unclear if or how this would promote biomass production because the majority of glucose carbons are excreted as lactate during the Warburg effect. An intriguing hypothesis suggests that the acidic microenvironment created by lactate secretion promotes tumorigenesis. This is supported by studies showing that increased acidity promotes cancer cell invasiveness, but the Warburg effect occurs at an early time point during tumorigenesis before invasion, which calls into question whether this can be the main function. Another model reasons that cancer cells undergo aerobic glycolysis for the purpose of cellular signaling such as the opening of chromatin, although it is difficult to conduct experiments that conclusively demonstrate this.
Although the exact reason why cells favor the Warburg effect remains elusive, there has been considerable effort toward exploiting it for cancer treatment by generating new therapeutic targets. It is clearly required for certain tumors, and furthermore, glucose uptake and catabolism are driven by enzymes encoded by oncogenes commonly mutated or overexpressed in many tumor types such as PI3K, KRas, and HIF1α, suggesting that tumors select for aerobic glycolysis. Future work will focus on elucidating exactly how the Warburg effect promotes tumorigenesis and better defining the specificity of targetable nodes for new cancer therapeutic strategies.
In addition to glucose, cancer cells rely on other nutrients to meet increased metabolic demands. Several amino acids have been shown to play important roles for various cancer cell functions. Similar to glucose, amino acid uptake through cell membrane transport channels and catabolism can be driven by oncogenes. Cancer cells can also obtain amino acids via de novo synthesis, breakdown of the serum peptide albumin after micropinocytosis, and autophagic digestion of cellular proteins. Of the 20 common amino acids, nine are essential—meaning that they are obtained from dietary sources. However, certain nonessential amino acids are considered to be conditionally essential in cases in which rapid catabolism outcompetes the local rate of generation.
There have been substantial efforts in studying cancer cell glutamine metabolism as both a carbon and a nitrogen source. Glutamine levels in serum are the highest of all amino acids, and glutamine is important for several cellular functions. Glutamine maintains redox balance by contributing to glutathione (GSH) synthesis and participates in anabolic metabolism such as lipid biosynthesis through reductive carboxylation. Glutamine also maintains nitrogen pools for the synthesis of nonessential amino acids and nucleotides. Of particular importance is that glutamine-derived glutamate is converted into α-ketoglutarate (αKG), which can maintain the flow of the TCA cycle leading to ATP production via the ETC. This is known as anaplerosis and is critical for continuing mitochondrial respiration. There is strong evidence that this occurs in cell culture, but reports using stable isotope labeling in mice have indicated that glutamine may not be a major source of αKG in all tumors. However, numerous studies have demonstrated the importance of glutamine in certain tumors; inhibition of glutamine metabolism prevents tumor growth in models of breast cancer, liver cancer, kidney cancer, and T-cell acute lymphoblastic leukemia.
Another fundamental metabolic process is one-carbon metabolism, which involves the amino acids serine, glycine, and methionine. One-carbon metabolism that consists of the folate and methionine cycles is a master integrator of nutritional status. Conversion of serine to glycine via serine hydroxymethyltransferase (SHMT) generates one-carbon molecules that are passed to folate moieties. These folate moieties undergo further chemical reactions that lead to the transfer of carbon atoms to downstream metabolic pathways. A major output of the folate cycle is the generation of nucleotides, which are essential for proliferating cells. Serine can be taken up by cells through transporters or synthesized de novo from glucose or gluconeogenic intermediates. In addition to contributing to the generation of nucleotides, serine coupled to the folate cycle is necessary for other biomass such as phospholipids and the generation of redox factors such as NADPH, a molecule used for reductive biosynthesis and restoration of glutathionine, which is used to protect against oxidative stress. Serine further contributes to redox balance by ligating with homocysteine to begin the transsulfuration pathway for cysteine synthesis, which is required for GSH production. Highlighting the importance of serine biosynthesis for certain cancers was the discovery that PHGDH, the gene encoding the enzyme that catalyzes the committed step, is amplified in melanoma and breast cancer. Moreover, PHGDH inhibitors have shown promise in reducing tumor growth in mouse models. Also of note, one-carbon units are used to methylate homocysteine to generate methionine, which can have a major effect on protein regulation and epigenetics (discussed in more detail later). In many cases, the majority of one-carbon units used to recycle methionine come from serine. In all, carbon units derived from serine, glycine, and other one-carbon donors such as choline, betaine, sarcosine, and histidine are used to produce biosynthetic components, maintain redox status, and provide the substrates for methylation reactions.
Other amino acids important for tumorigenesis include arginine, tryptophan, and the branched-chain amino acids leucine, isoleucine, and valine. Arginine can act as nitrogen donor for nitric oxide (NO) signaling, as a fuel for the urea cycle, or to maintain pools of nonessential amino acids, and tumors lacking the argininosuccinate synthase enzyme highly depend on exogenous arginine for growth. Tryptophan catabolism by tumors has been shown to create an immunosuppressive tumor microenvironment. Branched-chain amino acids contribute to biosynthesis of alanine and glutamine, and high levels are found in the serum of patients with early-stage pancreatic cancer. In addition, leucine and arginine are potent activators of mammalian target of rapamycin (mTOR), which is a regulator of protein translation and metabolism and cell growth and often dysregulated in cancers.
Mitochondria are organelles that play an important role in cell survival and proliferation. Mitochondrial metabolism is important for the function of the TCA cycle; ETC, fatty acid oxidation (FAO); synthesis of amino acids, lipids, and nucleotides; and production of ATP and antioxidants. One consequence of mitochondrial metabolism is the generation of reactive oxygen species (ROS). This led to the proposal that mitochondria may promote DNA damage via high amounts of ROS accumulation, which could contribute to genome instability. Although potentially damaging to cells at high levels, at lower concentrations ROS have been shown to act as signaling molecules that can promote proliferation and may be essential for tumorigenicity. In all, mitochondria promote cell growth through generation of energy, biomass, and signaling cascades ( Fig. 9.3 ).
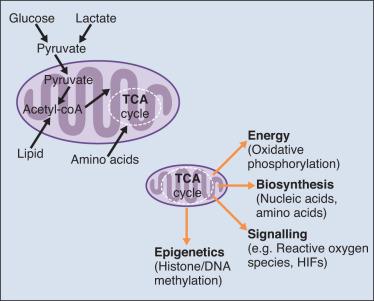
Warburg and others originally hypothesized that tumor cells harbored dysfunctional mitochondria, which is how it was reasoned that the TCA cycle and ETC were not used for tumor cell glucose metabolism. However, subsequent studies found that tumor cells could undergo oxidative metabolism, and in fact the mitochondria play a critical role in cancer cell metabolism. For example, it was reported in the 1950s that oxidation of the fatty acid (FA) palmitate occurred in a manner similar to that in healthy liver cells. In addition, enzymes of the TCA cycle such as isocitrate dehydrogenase (IDH) have similar expression levels in cancer cell and normal cell mitochondria. Numerous studies have corroborated these findings, and several reports have provided genetic evidence that mitochondrial metabolism is necessary for tumorigenesis. Indeed, the current paradigm in the cancer metabolism field is that cancer cells actively use and require both glycolysis and mitochondrial metabolism.
There is developing interest in targeting tumor mitochondrial processes for cancer therapy. As mentioned, the Warburg effect can generate sufficient amounts of ATP to fuel cancer cells in the absence of mitochondrial metabolism. Thus targeting mitochondrial ATP production may not be a viable therapeutic strategy. However, certain subtypes of cancer have been shown to be highly reliant on mitochondrial-dependent ATP production via oxidative phosphorylation. Moreover, the tumor microenvironment may have limited glucose availability, which would reduce the glycolytic capacity of the cell and make it more dependent on mitochondrial metabolism (discussed later in detail). A major pitfall for targeting these processes is the fact that a majority of normal cells require functional mitochondrial metabolism for survival. Thus tumor-specific delivery and uptake of therapeutics or the targeting of biosynthetic precursors selectively required in cancer cells would be essential for reducing healthy cell toxicity. Potential candidates include the antidiabetes drug metformin and certain glutaminase inhibitors (discussed later in detail).
Although given less attention than glucose or amino acids, lipid metabolism provides important signaling intermediates and biomass and energy resources to cancer cells. There are numerous species of lipids, or FAs, and all contain a hydrocarbon chain and terminal carboxyl group. The synthesis and oxidation of FAs contribute to numerous cellular growth and survival functions such as membrane formation, signaling molecules, and energy sources. Similar to other nutrients that support proliferation, lipid metabolism is upregulated in cancer cells. This is largely because cells must double their lipid membrane in order to divide, resulting in a massive demand for lipid and phospholipid precursors. Building blocks for membrane production and lipid energy sources come from exogenous sources such as diet and/or are synthesized de novo by cells. Cancer cells preferentially synthesize lipids locally, and early studies revealed a shift toward FA synthesis in neoplastic cells.
De novo synthesis of FAs is coupled to glucose and glutamine metabolism. The TCA cycle intermediate citrate is the starting material for a majority of local FA production. As mentioned, citrate can be generated by glucose-derived pyruvate or, in high–Warburg effect cells, glutamine-derived αKG. Several enzymes including ATP citrate lyase (ACLY), acetyl-coenzyme A (CoA) carboxylase (ACC), and fatty acid synthase (FASN) are required to metabolize citrate into bioactive FAs. ACLY converts citrate to oxaloacetate and acetyl-CoA, and acetyl-CoA is the major precursor for all lipids in the cell. The importance of ACLY for tumor growth is demonstrated by studies showing that loss of ACLY reduced tumor growth in mouse models. ACC catalyzes the committed step in FA synthesis via carboxylation of acetyl-CoA to malonyl-CoA. ACC is a highly regulated enzyme, and its activity is negatively regulated by the tumor suppressor LKB1 via AMPK-dependent phosphorylation. ACC has been shown to be required for cancer cell growth and survival, but additional complexity comes from other studies that have indicated a tumor suppressive role for ACC. FASN is commonly upregulated in several cancer types, and its expression correlates with poor prognosis. FASN condensates one acetyl-CoA and seven malonyl-CoA molecules to generate the initial product of FA synthesis, palmitate, which is then chemically altered to fuel pools of a diverse array of lipids including those involved in membrane formation and signaling molecules.
In addition to relying on lipids for biomass, cancer cells can oxidize FAs for energy production. The synthesis and oxidation of FAs are mutually exclusive, and several mechanisms for this regulation have been described in cancer cells. In a process known as β-oxidation, cellular FAs such as palmitate are catabolized in peroxisomes and mitochondria to generate energy and reducing molecules. Carnitine palmitoyltransferase 1 (CPT1) catalyzes the rate-limiting step for importing FAs into the mitochondria, where it is catabolized to generate acetyl-CoA. The 16-carbon palmitate ultimately generates eight acetyl-CoA molecules, which condense with oxaloacetate to drive the TCA cycle. Thus one molecule of palmitate can produce more energy than fully oxidized glucose. The brain isoform of CPT1 (CPT1C) was identified as a potential oncogene for its role in promoting cancer cell survival under metabolic stress. β-Oxidation has been shown to be particularly important for cancer cells that have lost attachment to the basal membrane, and targeting β-oxidation was sufficient to reduce tumor growth in a patient-derived triple-negative breast cancer (TNBC) xenograft model.
Because cancer cells may selectively rely on de novo FA synthesis, many efforts have been made toward targeting these pathways. Owing to its upregulation in numerous cancers, FASN in particular has been a popular target for drug development efforts, with several inhibitors evaluated in preclinical studies showing strong antitumor efficacy. Unfortunately, harsh side effects such as detrimental weight loss have been observed in preclinical models. Other enzymes of targetable interest include CPT1, ACLY, and ACC, with results similar to those with FASN inhibition. An interesting strategy for using cancer cell lipid dependence against tumors is loading drugs into liposomal nanoparticles, which has been shown to increase tumor-specific drug delivery. As is the case with targeting most metabolic processes, the inherent challenge is overcoming toxic side effects to normal cells.
Epigenetics, or more specifically chromatin state, encompasses changes in gene expression that are not the result of mutations in DNA sequences. Chromatin accessibility can in part determine gene expression and is regulated by posttranslational modifications of the chromatin-bound histone proteins including methylation, acetylation, ubiquitination, and phosphorylation in addition to methylation of the DNA base cytosine. Changes in epigenetics and chromatin have emerged as drivers of cancer initiation and progression and can function similarly to the amplification of oncogenes or the deletion of tumor suppressor genes. From a therapeutic perspective, targeting epigenetics is appealing for several reasons, including the druggability of the enzymes that carry out modifications to chromatin and DNA and the fact that many of the effects are reversible, as opposed to the irreversible changes of genetic mutations.
Histone acetylation and DNA and histone methylation are among the best studied modifications. DNA methylation occurs at the fifth position of cytosine bases and is commonly observed in promoter regions of genes. Histone acetylation and methylation occur on lysine (K) residues. Acetylation generally leads to active chromatin, whereas histone methylation is associated with both active and inactive chromatin. For example, methylation of histone H3K4 leads to enhanced gene expression, whereas methylation of H3K9 or H3K27 is associated with gene suppression. Underlying many epigenetic states is cellular metabolism because certain metabolites provide substrates for posttranslational modifications and essential cofactors for epigenetic machinery.
Methionine-derived S -adenosyl methionine (SAM) is a methyl donor for several methyl transferase enzymes, including DNA and histone methyl transferases ( Fig. 9.4A ). Therefore changes in one-carbon metabolism can have dramatic effects on epigenetics. Indeed, dietary restriction of methionine reduces levels of H3K4 methylation. Moreover, limiting glycine input reduces SAM levels and has a similar effect on H3K4 methylation. Similarly, SAM levels also affect DNA methylation during osteoclast differentiation. Acetyl-CoA derived from glycolysis and β-oxidation is the primary acetyl donor for histone acetylation reactions carried out by histone acetyltransferases ( Fig. 9.4B ). Previous studies have demonstrated that acetyl-CoA availability largely regulates histone acetylation, and histone acetylation depends on ACLY activity. Histone deacetylases remove acetyl groups from histones, and some require NAD + as a cofactor. Therefore the NAD + /NADH ratio in addition to the levels of acetyl-CoA, and NAD + , which can be increased in high Warburg cells, may have an effect on epigenetics and gene expression.
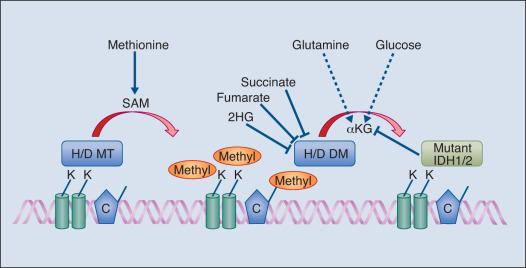
A major breakthrough in understanding of the connection between cancer metabolism and epigenetics was the discovery of mutations in the IDH genes IDH1 and IDH2 in leukemias and gliomas. The enzymes IDH1 and IDH2 normally convert citrate to αKG in the mitochondria and cytosol, respectively. Mutations in IDH1 and IHD2 occur in the active site, and loss of αKG production by IDH-mutant enzymes was originally attributed to loss-of-function. Subsequent studies found the IDH mutants to be gain-of-function mutations, where αKG was converted to 2-hydroxyglutarate (2HG) at high levels, resulting in a neomorphic enzymatic activity. Because αKG is an essential cofactor and 2HG is an inhibitor of many DNA and histone demethylases, IDH-mutant cells show broad DNA and histone hypermethylation, and supplementation with αKG attenuates these changes. Of note, pharmaceutical targeting of IDH1 and IDH2 has shown promising results in leukemia and glioma models. Similarly, the loss of glutamine, which can produce αKG, results in increased histone methylation of stem cells and alters drug responses in tumors; targeting the methyltransferases or supplementing with αKG resensitized cancer cells to the drug. Other metabolites besides mutant IDH–derived 2HG can inhibit demethylase activity. Cancer cells with loss-of-function mutations in the TCA cycle enzymes succinate dehydrogenase and fumarate hydratase accumulate succinate and fumarate, respectively, and display global DNA and histone hypermethylation ( Fig. 9.4A ). Thus future cancer treatments may target epigenetic machinery or use dietary supplements in combination with establish chemotherapeutics and new agents that target cancer metabolism.
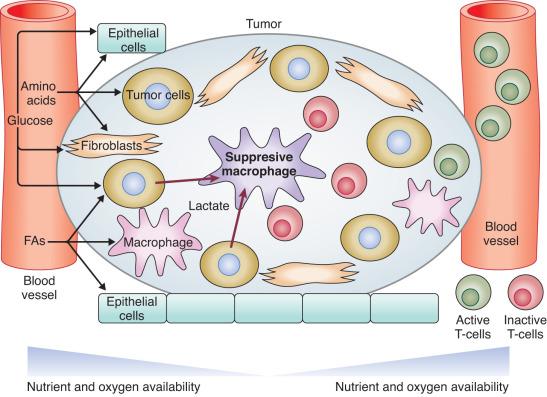
Many studies conducted in cell culture are performed on single cell types in the presence of abundant nutrients. In physiologic environments, tumor cells are surrounded by numerous other cell types including fibroblasts, endothelial cells, and lymphocytes, resulting in competition for local nutrients ( Fig. 9.5 ). In addition, tumors often contain incomplete and unorganized vasculature, which can lead to regions of nutrient and oxygen limitation. Although tumor cells require an abundance of nutrients to maintain rapid growth and proliferation, they paradoxically persist in these harsh environments. Consequently, cells that adapted to low nutrients and oxygen are among the most difficult to kill and present major challenges for many current cancer therapies. Thus in order to develop better therapeutic strategies, it is important to understand the tumor microenvironment and mechanisms of cellular adaptation to nutrient-deficient environments.
Hypoxia, or low oxygen, is one of the most studied properties of the tumor microenvironment. Oxygen levels in healthy tissue are around 5%, whereas regions of solid tumors can have oxygen levels below 0.5%. The ETC can function in oxygen levels as low as 0.5%, allowing tumor cells to mostly undergo normal cellular functions, but they may gain survival advantages based on signaling changes in response to oxygen stress due to changes in redox balance. For example, the hypoxia-inducible factor (HIF) proteins are activated by hypoxia and promote downstream transcriptional events to adapt to limited oxygen availability. This promotes survival in response to therapeutically induced stress such as radiation, and targeting HIF in combination with radiation therapy has shown promise. HIF proteins have also been implicated in maintaining cancer initiating or cancer stem cells that can repopulate tumors, and these cells are commonly found in hypoxic niches.
In addition to oxygen, tumor cells often encounter low levels of nutrients in the microenvironment (see Fig. 9.5 ). A study conducted with paired pancreatic cancer biopsies found pancreatic tumors are generally nutrient poor compared with adjacent normal tissues. It was shown that many amino acids were depleted, including glutamine and serine. Studies have found that cancer cells can survive glutamine limitation through induction of cell cycle arrest or alteration in glucose usage. Similarly, cells adapt to serine deprivation by inhibiting cell division. In addition, a subtype of breast and melanoma cells with amplifications of PHGDH can compensate for the loss of exogenous serine by upregulating de novo serine biosynthesis from glucose. Yet glucose availability itself is reduced in the microenvironment of some tumors. Further research will undoubtedly identify other survival pathways and redundancies used by tumors to survive. One goal of understanding these mechanisms is to target them in combination with established therapeutics.
The tumor microenvironment can play a major role in metabolism of tumors, depending on the tissue of origin. Highlighting this is a study that showed metabolism within the same tumor types was drastically different depending on the surrounding tissue. Heterogeneity of nutrient availability and use can occur within a single tumor. For example, nutrient availability drastically differs in core regions of solid tumors compared with the peripheral regions. Furthermore, a study of a non–small cell lung carcinoma patient cohort in which stable-isotope labeling was used found evidence of Warburg and non-Warburg utilizing cells within a single tumor, and these metabolic phenotypes largely differed from patient to patient. These results indicate that multiple types of therapeutics targeting metabolism may be necessary for treatment of a single tumor.
Tumor cell metabolism can alter the microenvironment to promote tumorigenesis and reduce immune activity. As mentioned previously, highly glycolytic cells convert the majority of their glucose carbons to lactate and secrete those carbons out of the cells. Lactate secretion is coupled to the cotransport of H + , and CO 2 generated by the ETC perfuses out of the cell before conversion to H + and HCO 3 − in the extracellular space. Consequently, the accumulation of H + reduces the local pH, creating an acidic microenvironment around tumors. Furthermore, studies have shown that acidified environments activate matrix metalloproteases, which degrade the extracellular matrix and promote tumor invasiveness. Moreover, lactate polarizes tumor-associated macrophages into an immunosuppressive state. In addition to innate immune cells, adaptive immune cells such as T cells require specific metabolic functions in order to facilitate their protective effects. The ability of T cells to transition from a naïve (inactive) state to an effector (active) state to a memory state is determined by their metabolism. Circulating T cells are normally in nutrient- and oxygen-rich environments. Upon entering tumors, T cells are met with challenging metabolic conditions that can affect their activity (see Fig. 9.5 ). T cells require large amounts of glucose for activation, and undergo the Warburg effect to a similar degree as many cancer cells. The absence of abundant glucose can lead to T-cell inaction or death. Indeed, much of the immunosuppression found in the tumor microenvironment is attributed to the inability of T cells to obtain sufficient nutrients. In addition, tumor cells upregulate indolamine 2′3′-dioxygenase (IDO) to promote tryptophan catabolism, which induces cell death in effector T cells. In addition to nutrient stress, oxygen availability also plays a major role in affecting T-cell function. Hypoxia-induced HIF activation transcriptionally upregulates PD-1 and CTLA4, which act to suppress immune activity. HIF also promotes expression of T regulatory cells (Tregs), which downregulate the immune response. Because of this, T cells can be tumor suppressive or tumor promoting. Immunotherapy focusing on ex vivo and in vivo stimulation of T cells is a promising avenue for management of tumors, but overcoming the tumor microenvironment will be critical to its success.
Obesity is a health crisis in the developed world, with estimates of over 30% of adults in the United States classified as obese. This is thought to be a major if not the leading source of human mortality. Although associated more commonly with type II diabetes and cardiovascular disease, accumulating evidence demonstrates that obese individuals are more likely to develop cancer. Obesity has been shown to increase risk of numerous cancers including breast, prostate, pancreatic, and colon cancers, with some estimates concluding that up to one in five cancers are directly attributable to obesity. Obesity is characterized by excessive amounts of adipose tissue resulting in excessive nutrient storage in the form of lipids. Adipose tissue is important for energy storage, cell signaling through hormone secretion, and inflammatory responses through cytokine secretion, all of which are altered in the obese state. It has also been shown in ovarian cancer that FAs produced by local adipose tissue fueled tumor cell metastasis. Thus it is likely that fat depots in themselves can promote tumorigenesis.
The major regulator of glucose homeostasis is the hormone insulin, which mediates insulin receptor (IR)–initiated cell signaling cascades. Insulin is released by pancreatic β-cells in response to higher blood glucose levels and signals the uptake of glucose by peripheral tissues. On activation, IR promotes the activation of signaling pathways including PI3K, AKT, and mTOR, which promote glucose uptake, anabolic metabolism, and cell growth. Because increased insulin levels and insulin resistance are hallmarks of obesity and the PI3K/AKT/mTOR signaling axis is the most frequently altered signaling cascade, it is possible that tumor cells may use insulin signaling resulting from obesity-associated hyperinsulinemia to enhance their own glucose uptake and growth. In support of this are studies demonstrating increased IR expression in certain liver, breast, and lung cancers. Similar yet distinct hormones upregulated during obesity are insulin-like growth factors 1 and 2 (IGF1 and IGF2). IGF1 binds the insulin-like growth factor receptor (IGFR), leading to similar downstream signaling cascades as insulin and IR. High levels of IGF1 have been shown to increase the risk of breast cancer. On the other hand, IGF2 can bind both IR and IGFR and reportedly promotes tumor growth in models of breast cancer. Other secreted factors altered in response to obesity that may contribute to tumorigenesis include adiponectin and leptin. Overall, obesity can lead to changes in circulating signaling molecules that directly enhance the tumorigenic capabilities of neoplastic tissues. The mechanisms, however, remain controversial and complicated, with multifactorial effects occurring through signaling, inflammation, and likely changes in tumor cell autonomous metabolism, although this effect has not yet been well established.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here