Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
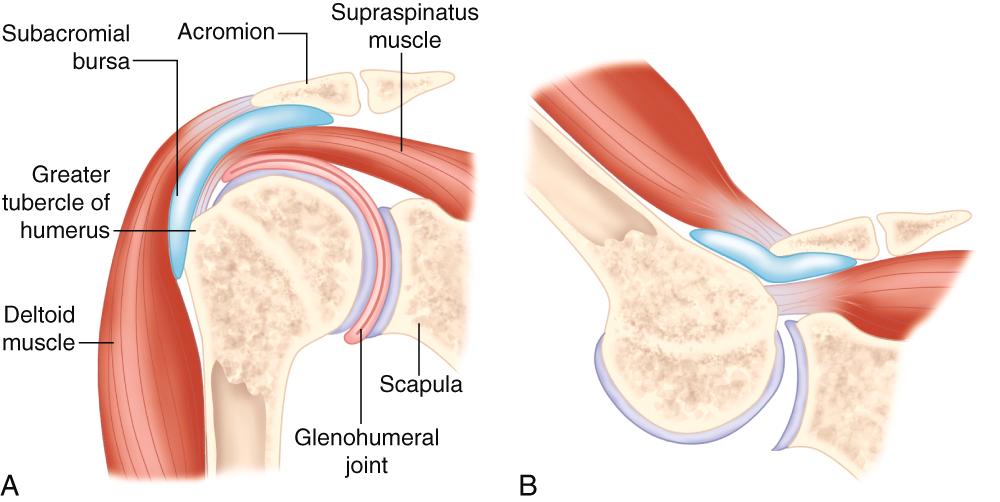
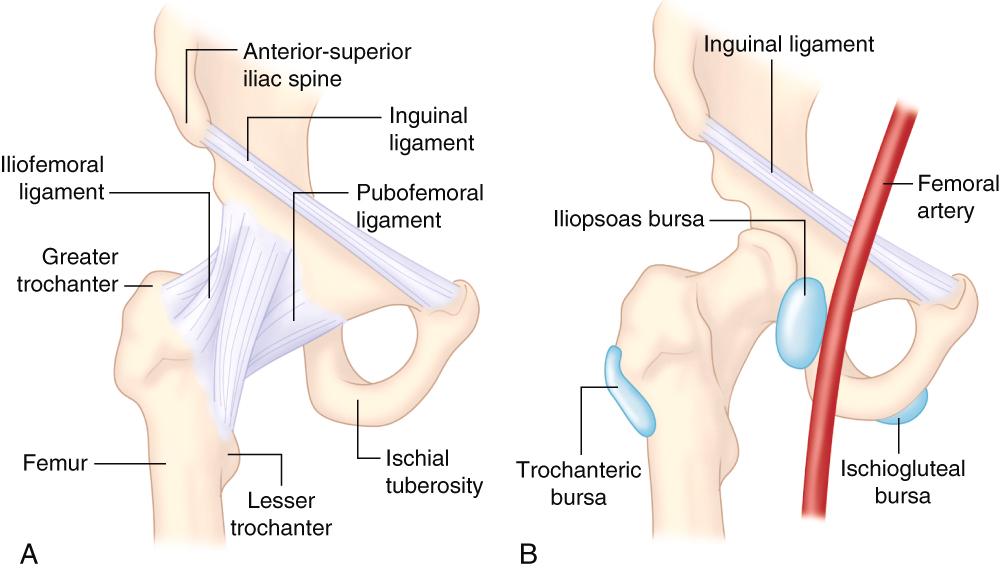
An array of painful and sometimes disabling musculoskeletal syndromes exist that are not articular in origin but arise from tendons, ligaments, enthesis, and bursae. These conditions are referred to by various names, in addition to tendinosis, enthesopathy, and bursitis, including the terms nonarticular rheumatism, soft tissue diseases, regional rheumatic pain syndromes, and repetitive use syndromes ( Table 242-1 ). These entities are often ignored, misdiagnosed as arthritis, or attributed to the aging process. Awareness of the existence of these conditions and knowledge of basic musculoskeletal anatomy ( Figs. 242-1 and 242-2 ) are the fundamental requirements for diagnosis. This knowledge is coupled with brief but specific physical diagnosis techniques. The accurate diagnosis and successful treatment of these conditions is gratifying to the clinician because many people can be relieved of their chronic painful syndromes.
| SHOULDER |
| Rotator cuff tendinosis; rotator cuff tear Bicipital tendinosis; biceps tendon tear Subacromial bursitis Adhesive capsulitis (frozen shoulder) |
| ELBOW |
| Olecranon bursitis Medial epicondylalgia Lateral epicondylalgia |
| WRIST AND HAND |
| De Quervain tenosinovitis Trigger finger Digital flexor tenosynovitis Ganglia (dorsal and volar wrist, finger, etc.) |
| HIP |
| Greater trochanter pain syndrome (gluteus medius and minimus tendinosis and tear; trochanteric bursitis) Iliopsoas bursitis Ischial bursitis Coccydynia |
| KNEE |
| Prepatellar bursitis Infrapatellar bursitis Pes anserine syndrome Iliotibial band syndrome Popliteal (Baker) cyst Quadriceps tendon tear Patellar tendinosis and tear Hoffa syndrome |
| ANKLE AND FOOT |
| Achilles tendinosis, insertional and mid-tendon Achilles tendon tear Retrocalcaneal bursitis Posterior tibial tendinosis and tenosynovitis Posterior tibial tendon tear Plantar fasciopathy (fasciitis) Morton neuroma |
Various terms regarding tendon injuries are used and may be confusing. The main term used is tendinitis, but tendinosis is the correct terminology because there are degenerative changes in the tendon but very few inflammatory cells. In addition, fatty mucoid degeneration and hyaline features occur in these tendon syndromes. Also, tendons may rupture or tear, partially or completely. The terms tenosynovitis and peritendinitis refer to an inflammatory response of the tenosynovium, such as in rheumatoid arthritis. However, tenovaginosis and peritendinosis are more appropriate terms in oversuse conditions. Tendinosis may occur when the tendon repeatedly bears more load than it can withstand. This may result from excessively high loads across normal tendons or from normal loads across degenerated tendons. In addition to load and repetitiveness, tendon changes resulting from immobility and from aging may play a role, as may the use of certain medications such as fluoroquinolones and corticosteroids.
Bursae are closed sacs lined by a synovial membrane, often discontinuous, and serve to promote smooth tissue gliding between tendon and bone, tendon and tendon, or bone and skin. A bursa can become inflamed from trauma or overuse or become infected, thereby producing a bursitis. Bursitis is typically associated with pain and swelling of the bursa.
The incidence and prevalence of the nonarticular syndromes are high. They are more common than rheumatoid arthritis and systemic lupus erythematosus combined. For example, the incidence of shoulder pain, largely a result of rotator cuff tendinosis and rotator cuff tear, is approximately 20% in a population older than 70 years of age.
A precise history is needed to identify the conditions present, and more than one syndrome can occur concomitantly. A working knowledge of regional anatomy and an approach that uses a regional differential diagnosis will help in obtaining a specific diagnosis. A complete neuromusculoskeletal examination should be performed, emphasizing careful palpation, passive range of motion (ROM), and active ROM alone or sometimes with resistance. Systemic and infectious causes must be considered. Diagnostic ultrasonography is very useful in confirming a musculoskeletal diagnosis. Magnetic resonance imaging (MRI) is also sometimes useful in confirming a diagnosis.
The causative aspects of symptoms should be evaluated, and activity should be modified as needed. Provided that the excessive load that caused the condition is reduced, most tendinopathies tend to improve with conservative therapy such as nonsteroidal anti-inflammatory drugs (NSAIDs; Table 26-4 ), relative rest of the injured site, stretching and strengthening exercises, friction massage, and use of modalities such as heat, ice, and ultrasound. The goals of therapeutic exercise are to increase flexibility by stretching, increase muscle strength by resistive exercises, and improve muscle endurance by some repetitive regimen.
Splinting, corticosteroid injections (given as the equivalent of 40 mg/mL of methylprednisolone acetate), and even surgery are options for more severe or recalcitrant symptoms. , Caution should be exerted in performing corticosteroid injections; the injections should not be placed into the tendon proper, but rather into the peritendinous sheath. The injected solution should be placed beneath the subcutaneous tissue, to avoid skin and subcutaneous fat atrophy and skin depigmentation, and injections should not be given too frequently, to avoid the possibility of weakening and rupture of the tendon. The accuracy of injections may be improved with concomitant use of diagnostic ultrasonography to assist with determining the correct needle site.
An overlap exists between commonly occurring conditions (e.g., tendinosis, enthesopathy, bursitis) and conditions attributed to specific sports injuries ( Table 242-2 ). For example, lateral epicondylalgia, frequently referred to as tennis elbow, occurs more commonly secondary to non–sports-related causes. In contradistinction, iliotibial band syndrome is usually related to sports. Other entities that occur more often in relation to sports include ligamentous knee injuries, patellar tendinosis, ankle sprains, turf toe, and acromioclavicular separations. It is important in both categories to know the anatomy and biomechanics of the condition so the problem can be diagnosed and treated appropriately. Sports-related injuries are helped with the classic RICE treatment, consisting of r est, i ce, c ompression, and e levation. Often, anti-inflammatory and analgesic drugs are used. However, corticosteroid injections are less often used for athletic injuries than in routine cases of tendinosis and bursitis because of fear of weakening the involved structures.
| SHOULDER |
| Acromioclavicular separation Glenoid labial tear (SLAP lesion) Glenohumeral instability with dislocation |
| ELBOW |
| Triceps tendinopathy Little League elbow (apophysitis) Distal biceps tendinosis |
| WRIST AND HAND |
| Gamekeeper’s thumb (skier’s thumb) Mallet finger (baseball finger) Extensor carpi ulnaris tendinitis Rupture of flexor digitorum profundus tendon Injury to triangular fibrocartilage |
| HIP |
| Adductor strain (groin pull) Hip pointer Hamstring strain |
| KNEE |
| Anterior cruciate tear Posterior cruciate tear Medial collateral ligament tear/strain Lateral collateral ligament tear/strain Popliteal tendinitis Medial and lateral meniscal tears Patellar tendinitis Iliotibial band syndrome |
| ANKLE AND FOOT |
| Ankle sprain Turf toe Stress fracture |
Shoulder pain is one of the most common musculoskeletal complaints in people older than 40 years of age. In younger people, athletic injuries are a frequent source of such pain.
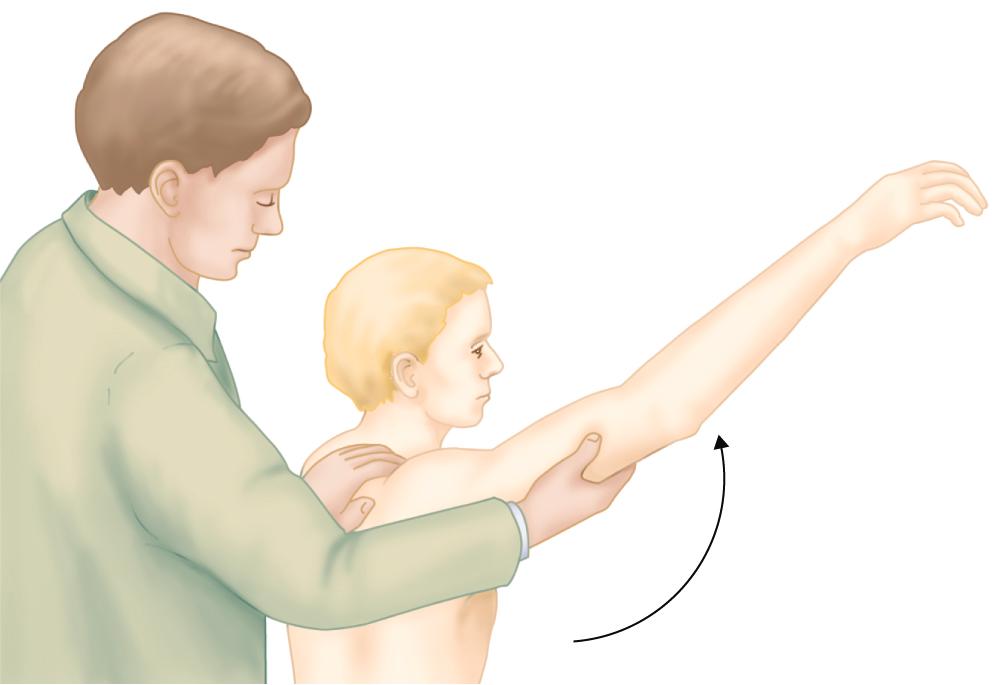
Rotator cuff tendinosis, or impingement syndrome, is the most common cause of shoulder pain. Tendinosis (and not bursitis) is the primary cause of pain, but secondary involvement of the subacromial bursa occurs in some cases. The condition may be acute or chronic and may or may not be associated with calcific deposits within the tendon. The key finding is pain in the rotator cuff on active abduction, especially between 60 and 120 degrees, and sometimes when lowering the arm. In more severe cases, pain may begin on initial abduction and continue throughout the ROM. Typically, chronic rotator cuff tendinosis manifests as an ache in the shoulder, usually over the lateral deltoid, and occurs with various movements, especially abduction, internal rotation, and the resisted action of the involved muscle(s). Other symptoms include difficulty in dressing oneself and night pain because of difficulty in positioning the shoulders. The physical findings include pain and loss of active abduction and internal rotation, less pain on passive motion, tenderness of the area of supraspinatus insertion, and a positive impingement (Neer) sign ( Fig. 242-3 ), which is pain occurring in forced flexion. The causes of rotator cuff tendinosis are multifactorial, but normal wear and relative overuse, especially from overhead activity that causes impingement of the rotator cuff, are commonly implicated.
Treatment consists of rest and modalities such as hot packs, ultrasound, or cold applications, with specific range of motion exercises as soon as tolerated. NSAIDs ( Table 26-4 ) are often beneficial. Injection of a depot corticosteroid, such as 1 mL of a 40 mg/mL concentration of methylprednisolone acetate into the subacromial bursa, the floor of which is contiguous with the rotator cuff, can provide improvement for up to 8 weeks but probably not long-term benefit. Extracorporeal shock wave therapy can be beneficial for chronic calcific tendinitis, but surgery is of limited benefit.
In a rotator cuff tear, an acute tear after trauma is usually easily recognized. The trauma may be superimposed on an already degenerative and possibly even partially torn cuff. In cases of trauma resulting in a ruptured cuff, fracture of the humeral head and dislocation of the joint also should be considered. However, most patients with a tear recall no trauma. In these cases, degeneration of the rotator cuff occurs gradually, resulting ultimately in a complete tear.
MR is the preferred imaging test. Rotator cuff tears are classified as small (≤1 cm), medium (1 to 3 cm), large (3 to 5 cm), or massive (>5 cm). Shoulder pain, weakness on abduction, and loss of motion occur in varying degrees, ranging from severe pain and mild weakness to no pain and marked weakness. A positive drop-arm sign with inability to maintain actively 90 degrees of passive shoulder abduction may be present in patients with large or massive tears.
Small complete tears and incomplete tears of the rotator cuff are treated conservatively with rest, physical therapy, and NSAIDs. Although its role has not yet been established by careful studies, a subacromial injection of a corticosteroid, such as 1 mL of a 40 mg/mL concentration of methylprednisolone acetate, may relieve pain. Surgical repair may be indicated in younger patients.
Bicipital tendinosis is manifested by pain, most often in the anterior region of the shoulder and occasionally more diffusely. The pain may be acute but is usually chronic and is related to impingement of the biceps tendon by the acromion. Tenosynovitis of the long head of the biceps is present, and the tendon may be frayed and fibrotic. Palpation over the bicipital groove reveals localized tenderness. The patient’s response should be compared with the response to palpation of the opposite side (i.e., tendon with normal tenderness). Pain may be reproduced over the bicipital tendon in some cases by supination of the forearm against resistance (Yergason sign), shoulder flexion against resistance (Speeds test), or extension of the shoulder. Rupture of the biceps tendon can occur at the superior edge of the bicipital groove, thereby producing a characteristic bulbous enlargement of the lateral half of the muscle.
Treatment of bicipital tendinitis consists of rest, hot packs, ultrasound, and, as pain subsides, passive and then active ROM exercises. NSAIDs ( Table 26-4 ) may be helpful, and occasionally a small amount of corticosteroid, such as 0.5 mL of a 40 mg/mL concentration of methylprednisolone acetate, carefully injected into the tendon sheath or 1 mL of a 40 mg/mL concentration of methylprednisolone acetate intra-articularly in the shoulder may be of benefit.
Adhesive capsulitis (frozen shoulder) is associated with generalized pain and tenderness and severe loss of active and passive motion in all planes. It is rare before 40 years of age but may occur secondary to any type of shoulder problem. However, not every stiff and painful shoulder is necessarily adhesive capsulitis. Inflammatory arthritis and diabetes can cause adhesive capsulitis. Additional factors such as immobility and neglect or improper initial treatment also favor the development of a frozen shoulder. Symptoms and function are adversely affected by depression and anxiety ( Chapter 362 ). Many cases, however, are idiopathic. The joint capsule adheres to the anatomic neck, and the axillary fold binds to itself, causing restricted motion. The capsule becomes thickened and contracted. Arthrography may help confirm this diagnosis by showing a decrease in volume of the shoulder joint capsule but is usually not needed.
Oral steroids improve pain and range of motion in the short term, but a frozen shoulder is probably best treated with a comprehensive program involving NSAIDs and corticosteroid injections of 1 mL of a 40 mg/mL concentration of methylprednisolone acetate into the glenohumeral joint and the subacromial bursa. Physical therapy consists of ice packs, ultrasound, transcutaneous electrical nerve stimulation, and gentle range of motion exercises, beginning with pendulum exercises and wall climbing with the fingers and progressing to active range of motion and strengthening exercises. Depression and anxiety may require attention ( Chapter 362 ). In a randomized trial, manipulation under general anaesthesia supplemented by a steroid injection, arthroscopic capsular release, and structured physiotherapy were equivalently effective, but arthroscopic capsular release carried the highest risks. The duration of a frozen shoulder may last up to 9 to 12 months. In prolonged duration, manipulation of the shoulder under anesthesia can be considered.
Olecranon bursitis occurs frequently and involves the subcutaneous olecranon bursa, either secondary to trauma or as an idiopathic condition. The bursa is characteristically swollen and tender on pressure ( Fig 242-4 ), but pain may be minimal, and usually no motion is lost. Aspiration may yield clear or blood-tinged fluid with low viscosity or grossly hemorrhagic fluid. Inflammatory olecranon bursitis may be caused by bacterial infection, gout, rheumatoid arthritis, or calcium pyrophosphate deposition disease. Localized erythema, a scab, fissure, or previous puncture at the tip of the elbow, surrounding edema, and local tenderness all suggest septic bursitis ( Chapter 251 ). Unlike septic arthritis, in which the elbow must be kept in semiflexion, the elbow may be brought into full passive extension in septic bursitis.
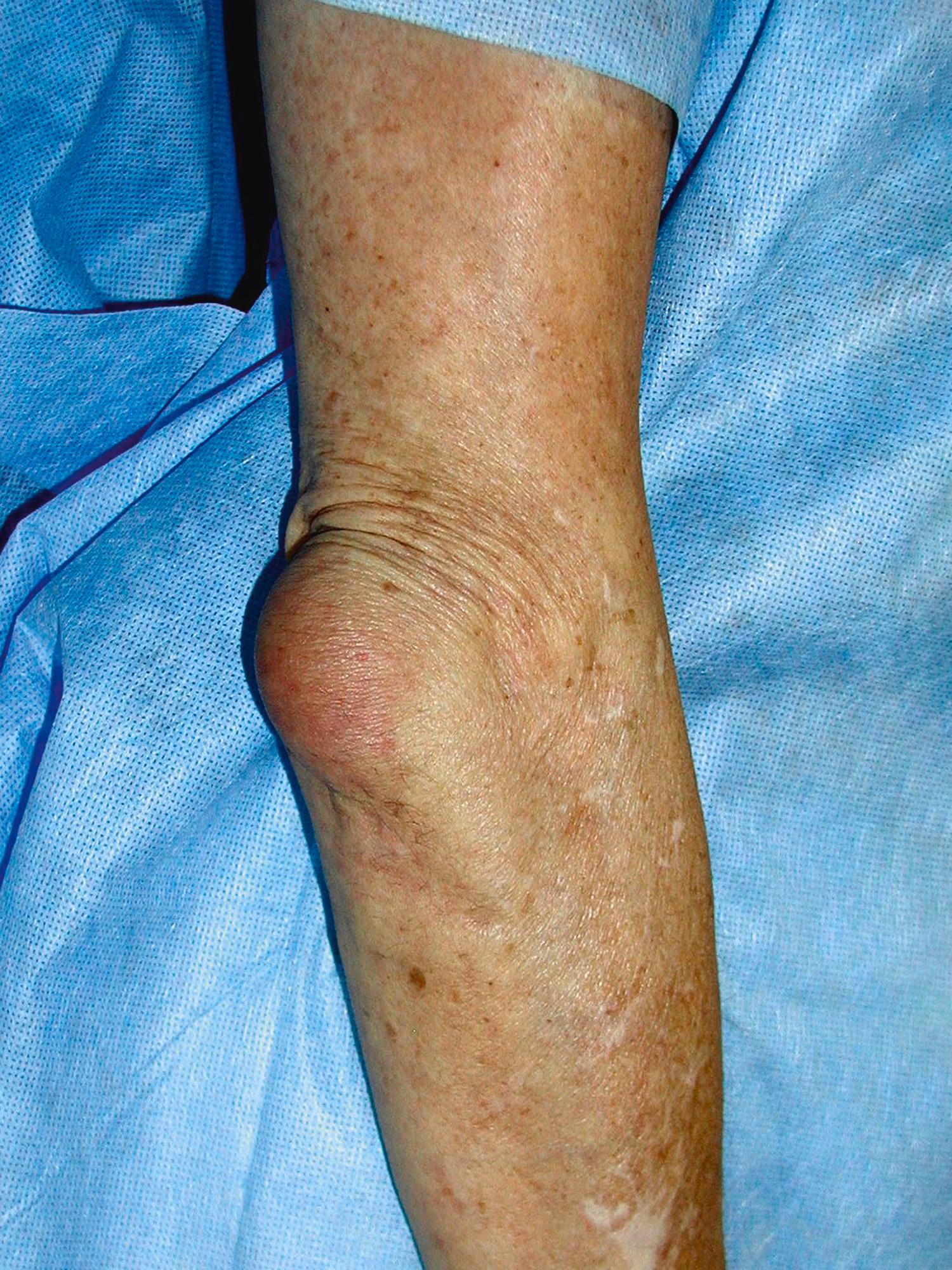
In aseptic bursitis, aspiration alone and protection from trauma are usually sufficient to resolve the condition. A small dose of a corticosteroid, such as 0.5 mL of a 40 mg/mL concentration of methylprednisolone acetate, may be injected into the bursa. Septic olecranon bursitis is treated with the appropriate antibiotics ( Chapter 251 ) and usually one or two additional needle aspirations.
Lateral epicondylalgia, or tennis elbow, is a common condition in those who overuse their arms. Localized tenderness directly over or slightly anterior to the lateral epicondyle is the hallmark of this disorder. Pain may occur during handshakes, while lifting a briefcase, or with other similar activities. Probably less than 10% of patients actually acquire lateral epicondylitis through playing tennis. Job and recreational activities, including gardening and athletics, are the usual causes. Pathologically, the condition consists of degeneration of the common extensor tendon, particularly of the extensor carpi radialis brevis tendon.
Medial epicondylitis, or golfer’s elbow, which mainly involves the flexor carpi radialis, is less common and less disabling than lateral epicondylitis. Local pain and tenderness over the medial epicondyle are present, and resistance to wrist flexion exacerbates the pain.
Treatment is aimed at altering activities and preventing overuse of the forearm musculature. Ice packs, heat, and NSAIDs are of some benefit. A forearm brace also can be used. A local corticosteroid injection, such as 1 mL of a 40 mg/mL concentration of methylprednisolone acetate with a 25-gauge needle over the epicondyle, often produces satisfactory initial relief. Isometric strengthening is important as an initial part of a rehabilitation program. Occasionally, surgery may be required for sports-related medial epicondylitis.
A ganglion is a cystic swelling that arises from a joint or tendon sheath and occurs most commonly over the dorsum or volar aspect of the wrist. A ganglion has a focal lining, does not have a synovial derivation, and contains thick, jelly-like fluid. Ganglia apparently develop secondary to trauma or prolonged wrist extension. Usually, the only symptom is swelling, but occasionally a large ganglion produces discomfort on wrist extension or compresses a neighboring nerve. Ultrasonography is useful for making the diagnosis.
Temporary immobilization with a splint or brace may be helpful. Percutaneous drainage is commonly successful, but surgery is sometimes required.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here