Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Mammographic screening of asymptomatic women after the age of 40 years decreases the mortality of breast cancer. About 40% of cancers detected by mammographic screening are not clinically apparent.
Hyperplasia is the most common benign breast disorder. When associated with cellular atypia, there is an increased risk of subsequent malignant transformation.
About 5-10% of breast cancers are hereditary and result from a germline mutation in the BRCA1 or BRCA2 gene. These genetic mutations also confer an increased risk of ovarian cancer.
The modern approach to breast cancer management requires a multidisciplinary approach with breast-conserving surgery and adjuvant radiation to the breast. Most patients are offered adjuvant chemotherapy and/or hormonal therapy, depending on the pathological features of the cancer and risk factors for recurrence.
Although the single most important prognostic factor for breast cancer is the status of the axillary lymph nodes, this is an oversimplification, as it is now clear that breast cancer is a very heterogeneous disease. The patient's estrogen receptor status is an independent prognostic factor.
Breast cancer is not treated by gynecologists in most parts of the United States, but it is important that gynecologists be expert in breast examination, diligent about recommending screening asymptomatic women for breast cancer, familiar with common benign and malignant disorders of the breast, and conversant with the various therapeutic options available.
Most breast cancers are detected by using medical screening techniques. Occasionally, a breast cancer is discovered by a woman during self-examination of her breasts. Because there is little scientific evidence that routine breast self-examination reduces mortality of breast cancer and may in fact lead to anxiety and unnecessary procedures, the United States Preventive Services Task Force (USPSTF) does not recommend routine breast self-examination. It seems reasonable, however, to encourage women to be aware of any changes in their breasts and for them to seek professional evaluation of any noted changes.
A complete breast examination should be performed by a physician at least every 3 years, especially for women older than 35 years of age. The breasts are first inspected with the patient in an upright position. The contour and symmetry are observed, and any skin changes or nipple retraction is noted. Skin retraction, because of tethering to an underlying malignancy, may be highlighted by having the patient extend her arms over her head.
Palpation of the breast, areola, and nipple is performed with the flat of the hand. If any mass is palpated, its fixation to deep tissues should be determined by asking the patient to place her hands over her hips and contract her pectoral muscles. Each axilla is then carefully examined while the patient's arm is supported. The supraclavicular fossae are also palpated for lymphadenopathy. Following palpation with the woman in the upright position, the examination is repeated with her in the supine position.
Several randomized controlled trials have demonstrated that mammographic screening of asymptomatic women older than 40 years of age can decrease the mortality of breast cancer. Densities and fine calcifications constitute suspicious findings, and clinically inapparent malignancies of less than 1 cm in diameter may be detected.
Mammograms of high quality can be made with about 0.3 cGy or less of radiation, so there is little, if any, risk of this technique causing breast cancer.
In 2009, the USPSTF estimated that screening was associated with 15%, 14%, and 32% reductions in breast cancer mortality for women 39 to 49, 50 to 59, and 60 to 69 years of age, respectively. The American Cancer Society recommends annual mammograms starting at age 40 years for women at normal risk.
Ultrasonography can differentiate cystic from solid masses and may demonstrate solid tissue that is potentially malignant within or adjacent to a cyst. It is also useful for imaging palpable focal masses in women younger than 30 years of age and in pregnant women, reducing the need for x-ray studies in this population.
Magnetic resonance imaging is a useful adjunct in breast imaging. Reported advantages include improved staging and treatment planning, enhanced evaluation of the augmented breast, better detection of recurrences, and improved screening of high-risk women, including those with BRCA gene mutations.
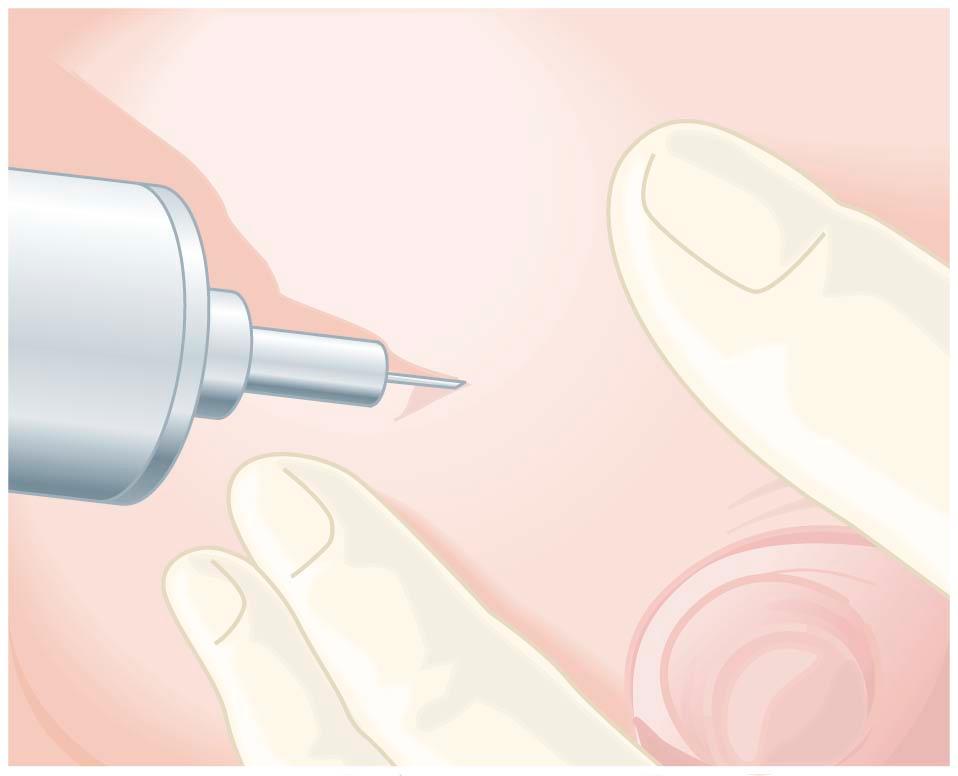
Physiologic nodularity and cyclic tenderness caused by the changing hormonal milieu must be distinguished from benign or malignant pathologic changes. Definitive diagnosis of breast neoplasms may be made by open biopsy, by fine-needle (22-gauge) aspiration cytology, or by core biopsy.
Fine-needle aspiration biopsy of a small, palpably suspicious lump in the breast can be performed in the outpatient clinic. Smears are prepared from the aspirate to allow cytologic evaluation. In experienced hands, the test is both sensitive and specific. A negative result should never be accepted as definitive when there are clinical or mammographic and/or ultrasonic suspicions that the lesion may be malignant, and a core or open biopsy should be done. In the presence of a large palpable lump, a core biopsy should make it possible to diagnose breast cancer without a formal excisional biopsy in at least 90% of cases, allowing the definitive management of the patient to be discussed preoperatively.
Relative indications for breast biopsy include those women with a clinically benign mass but a positive family or personal history of breast or ovarian cancer, a history of atypical hyperplasia, or an equivocal finding based on mammography or cytology.
The earlier term fibrocystic disease has little clinical value, and the term was abandoned by the College of American Pathologists in 1985. Lesions formerly grouped together under the designation of fibrocystic disease represent a pathologically heterogeneous group of diseases that can be divided into three separate histologic categories: nonproliferative lesions, proliferative lesions (hyperplasia) without atypia, and atypical hyperplasias.
Hyperplasia is the most common benign breast disorder and is present in about 50% of women. Histologically, the hyperplastic changes may involve any or all of the breast tissues (lobular epithelium, ductal epithelium, and connective tissue). When the hyperplastic changes are associated with cellular atypia, there is an increased risk for subsequent malignant transformation.
It is postulated that the hyperplastic changes are caused by a relative or absolute decrease in production of progesterone or an increase in the amount of estrogen. Estrogen promotes the growth of mammary ducts and the periductal stroma, whereas progesterone is responsible for the development of lobular and alveolar structures. Patients with hyperplasia improve dramatically during pregnancy and lactation because of the large amount of progesterone produced by the corpus luteum and placenta and the increased production of estriol, which blocks the hyperplastic changes produced by estradiol and estrone.
The disorder usually occurs in the premenopausal years. Clinically, the lesions are usually multiple and bilateral and are characterized by pain and tenderness, particularly premenstrually.
Treatment depends on the age of the patient, the severity of the symptoms, and the relative risk of the development of breast cancer. Women older than 25 years of age should undergo baseline mammography to exclude carcinoma. Cysts may be aspirated to relieve pain ( Figure 30-1 ). If the fluid is clear and the lump disappears, careful follow-up alone is indicated. Open biopsy is required if the fluid is bloody or if there is any residual mass following aspiration.
Composed of both fibrous and glandular tissue, the fibroadenoma is the most common benign tumor found in the female breast. Clinically, these tumors are sharply circumscribed, freely mobile nodules that may occur at any age but are common before the age of 30 years. They usually are solitary and generally are removed when they reach 2 to 4 cm in diameter, although giant forms up to 15 cm in diameter occasionally occur and have malignant potential. Pregnancy may stimulate their growth, and regression and calcification usually eventuate postmenopausally. These larger tumors require surgical excision for definitive diagnosis and cure.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here