Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Access video content for this chapter online at Elsevier eBooks+ ![]()
Gender dysphoria refers to the significant distress that results from an incongruence between the sex assigned at birth and the individual’s gender identity. Social transition, hormones, and gender-affirming surgery (GAS) can be effective in the medical treatment of gender dysphoria. Transgender and gender non-binary individuals may choose to undergo one or more surgical procedures depending on their individual goals. Gender-affirming surgeries can be divided into genital surgery (phalloplasty, metoidioplasty, oophorectomy, vaginoplasty, and orchiectomy) and non-genital surgeries. The aim of this article is to provide an overview of this latter group of gender-affirming surgeries, specifically chest surgery and facial surgery.
The World Professional Association for Transgender Health (WPATH) sets forth Standards of Care for surgical and non-surgical treatment of the transgender and gender non-binary individual. The SOC proposes the following criteria for gender-affirming chest/breast surgeries: (I) persistent well-documented gender dysphoria; (II) capacity to make fully informed decisions and to consent for treatment; (III) age of majority (although there is a separate pathway for adolescent patients); and (IV) well-controlled medical or mental health concerns. Hormone therapy is not a prerequisite, though may be recommended to maximize pectoralis hypertrophy and breast tissue atrophy prior to chest masculinization, or breast growth prior to breast augmentation, which improves cosmetic outcomes. WPATH does not provide guidelines for facial feminization surgery, though similar criteria should be followed.
Chest masculinization, often referred to as “top surgery”, is the most common surgical procedure for the transmasculine individual. Many of these patients bind their breasts daily with tight wraps and restrictive garments to conceal them. Binding is universally understood to be cumbersome, uncomfortable, and can lead to rashes, acne, and difficulty breathing. A growing body of literature definitively demonstrates improved quality of life, improved self-esteem and body image, and reduction in gender dysphoria in individuals who have undergone chest masculinization.
In accordance with WPATH Standards of Care , the initial consultation includes a complete history documenting the nature and extent of gender dysphoria, a complete medical history, and a discussion of the goals and expectations of surgery. Identifying postoperative social supports is also an important part of this visit. A thorough personal and family history of breast cancer is taken in all patients. Prior to mastectomy, the Endocrine Society and American Cancer Society recommend breast cancer screening in the form of mammography, starting at the age of 45, or as early as 40 if preferred by the patient. Preoperative breast imaging is obtained for any patient who meets criteria based on age, family history, or physical exam. The risk of occult breast cancer in the mastectomy specimen warrants discussion at the time of consultation. Studies have demonstrated diagnosis of breast cancer and high-risk lesions in gender-affirming mastectomy pathology specimens, although most lesions have been found in patients older than 40 years of age. In very young patients without risk factors, the cost–benefit of sending tissue can be discussed individually, but the general recommendation should be to send all breast tissue to pathology.
Current guidelines for breast cancer screening after gender-affirming mastectomy vary significantly and lack an evidence-based foundation. Chest mammography is typically not technically feasible after most techniques, given the flat contour of the chest wall. Alternative imaging modalities include the use of ultrasound or magnetic resonance imaging for screening; however, no data exist on the utility of these techniques for postmastectomy screening in the transmasculine population. Particular attention should be paid to the type of mastectomy. Inferior pedicle, periareolar, and circumareolar techniques result in more breast tissue left behind, but with all techniques the amount left will vary between surgeons. Patients should be counseled on lifetime monitoring of residual breast tissue with regular clinical breast exams of the chest wall, skin, and incisions.
Obese patients are encouraged to lose weight to lower BMI, although current literature does not link BMI to major complications. Smoking cessation is highly recommended, as there are known risks of wound healing complications. All nicotine products should be stopped a minimum of 4 weeks prior to surgery, and not started until at least 4 weeks postoperatively. The risk of venous thromboembolism is not well studied in patients on testosterone supplementation, although with the aromatization of testosterone to estradiol, some surgeons have advocated discontinuing testosterone for a period of time before surgery. Due to the known elevation of hematocrit levels with testosterone treatment, evaluation for polycythemia is advisable prior to surgery. However, a recent systematic review did not demonstrate any association of increased VTE or other complications after surgery with perioperative testosterone use.
A variety of surgical techniques for mastectomy in the transmasculine individual have been described, with the common goals of providing smooth masculine chest contours, minimizing and camouflaging scars along anatomic lines, and creating an aesthetic male nipple–areolar complex (NAC). Choice of technique is based on multiple factors including breast size, degree of skin laxity, degree of ptosis, skin quality, and the size and position of the NAC. In technique selection, one must balance the desire to limit the extent of the scar with obtaining an optimal chest contour. The preferences of the patient regarding scars, willingness to undergo revision surgeries, and maintenance of NAC sensitivity are factored into the technique selected.
In a landmark study published in 2008, Monstrey et al . presented an algorithm that emphasized skin elasticity and breast size as key factors in determining the optimal technique. A modification of this algorithm is presented in Algorithm 14.4.1 which, in addition to the factors presented by Monstrey, introduces the critical issue of nipple height to help guide in selecting optimal technique. The nipple height is considered high if the upper border of the areola sits above the inferior border of the pectoralis muscle with the breast pulled down on stretch. Skin laxity is best thought of as excess of the skin envelope. A convenient measure is the angle created between the lower pole of the breast and the chest wall. As a general guide, breasts that create an obtuse angle have minimal laxity, those that create a right angle have moderate laxity, and those that create an acute angle have significant laxity (see Algorithm 14.4.1 ).
Algorithm for technique selection in chest masculinization surgery. Nipple height is defined by the relationship between the upper border of the areola relative to the inferior border of the pectoralis when pulled down on stretch. The nipple is considered high if the upper border of the areola sits above the inferior border of the pectoralis muscle. Skin laxity can be estimated using the angle of the chest wall, inframammary fold (IMF), and breast tissue hanging below the IMF. An obtuse angle corresponds to minimal laxity, while an acute angle corresponds to significant laxity. Patients with low nipples and moderate or significant skin laxity should undergo a double incision procedure with free nipple grafts or with an inferior pedicle. For those with low nipples and minimal breast tissue, a periareolar or circumareolar technique can be offered, assuming the patient does not mind the low nipple position. For patients with nipples in a high position, short scar options are best, including periareolar, circumareolar, or extended circumareolar, depending on the size of the NAC and the degree of skin laxity that requires removal for flat contours. DI, double incision; FNG, free nipple graft; Inf, inferior.
Techniques can be broken down into five basic categories: (1) the periareolar technique, (2) the circumareolar technique, (3) the extended circumareolar technique with several common skin excision patterns, (4) the double incision with free nipple graft technique, and (5) the inferior pedicle technique. A process of shared decision-making is key to arrive at the appropriate surgical plan based on a combination of anatomical considerations and patient goals and wishes. Adjunct procedures frequently performed include nipple reduction and liposuction.
The periareolar technique involves mastectomies via a small incision along the inferior border of the areola. While the periareolar mastectomy technique results in a small, well-hidden scar and typically maintains NAC sensation, its success relies on minimal skin laxity, small and high NACs, and good skin quality that will contract to the chest wall. Only a minority of patients are candidates for this technique, approximately 8% as shown in a systematic review by Wilson et al .
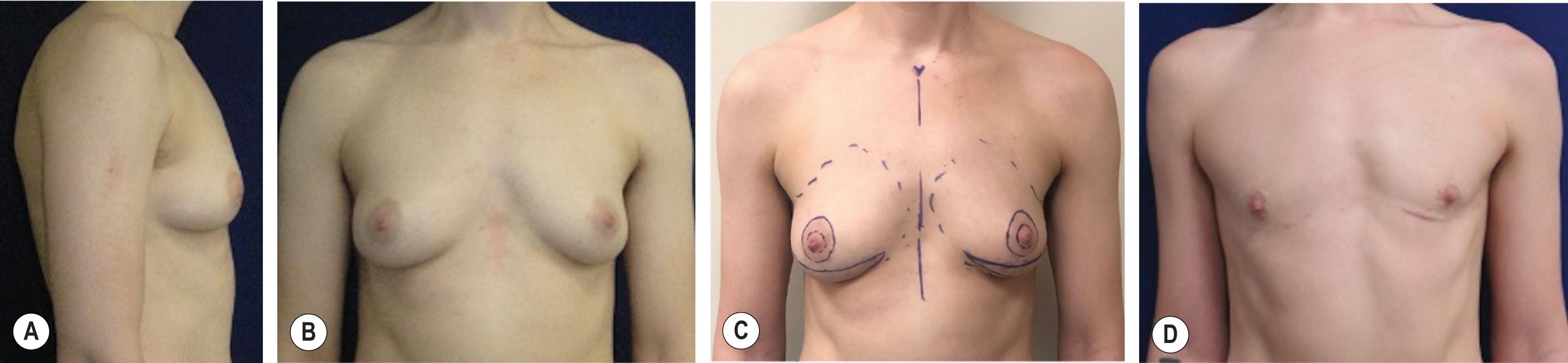
Preoperative markings, performed in a standing position, include the sternal midline and the entire footprint of the entire breast. The inferior periareolar marking is incised and the parenchyma is incised to a depth of about 1 cm. The NAC and the preserved underlying parenchyma are then elevated to the superior aspect of the NAC before transitioning to the outer breast capsule. It is important to maintain the sub-NAC parenchyma for perfusion as well as to support the NAC and prevent central contour depression. Headlamps are employed and lighted retractors are used to obtain adequate visualization. Ideally, nonconductive retractors are utilized to avoid thermal injury to the incision edges. Skin and subcutaneous flaps are elevated off the breast capsule in all directions to the extent of the breast footprint down to the chest wall. The breast gland is separated from the pectoralis muscle with preservation of the overlying fascia. After irrigation and careful hemostasis, a 15 F round closed suction drain is placed in the mastectomy cavity and secured. The incisions are closed in layers followed by placement of Steri-Strips, gauze, and a compression vest. Drains remain for 1 week, and compression is continued for 4–6 weeks. For the right patients, the periareolar technique can result in a masculine chest with nearly imperceptible scars under the areola ( Fig. 14.4.1 ).
In cases where the superior border of the areola is high relative to the pectoralis muscle and where there is a small to moderate amount of skin laxity, a concentric circular, or circumareolar technique allows for excision of a small amount of skin and areolar reduction along with the mastectomy ( Fig. 14.4.2 ). The circumareolar technique can be combined with additional skin excision patterns, of which the most commonly used are a lateral extension ( Fig. 14.4.3 ), or a wedge excision along the pectoralis border ( Fig. 14.4.4 ). In all of these techniques, the NAC is perfused on a dermal pedicle, allowing for improved projection and the possibility of preserved sensation. In the review by Wilson et al ., surgeons performed either a circumareolar or an extended circumareolar technique 34% of the time, although in our practice we utilize this technique less often, about 5% of the time.
The markings include the midline and breast footprint markings, plus an inner circle within the existing NAC, usually about 2.5 cm, and an outer circle drawn while the patient is standing while using clinical judgment to determine the amount of skin to be excised. This is often marked just outside of the existing areola border. The surgery is initiated with de-epithelialization of the intervening skin between the two circles. A full-thickness incision is then made through the lower half of the dermal pedicle, and the mastectomy is carried out identically to the periareolar technique. If an extended circumareolar technique is planned with a lateral dart, the anticipated skin excision patterns are drawn preoperatively, but typically not committed to until after the mastectomy is completed. At this point, the outer circle with or without the lateral extension is tailor-tacked to the inner circle, and the patient is sat upright in the operating room to assess contours. In the case where an inferior wedge technique is planned, our preferred method is to perform the mastectomy through the inferior incision along the lower border of the pectoralis muscle, preserving a disc of breast parenchyma beneath the NAC in the process. Once the mastectomy is completed and tailor-tacked, the circumareolar skin excision is performed and completely closed before tailor-tacking and completing the inframammary fold (IMF) wedge excision.
For patients with larger breasts, moderate or significant skin laxity, low positioned NACs, and/or poor skin quality, the best choice is the “double incision” mastectomy technique with free nipple grafting. This technique allows for the most reliable creation of flat contours and optimal control over size and position of the NAC on the chest wall. The primary disadvantage is the length of the scars and the loss of NAC sensation. In Wilson’s review he found this technique utilized in 42.2% of top surgeries, although in our practice it is much more frequent, about 85% of the time.
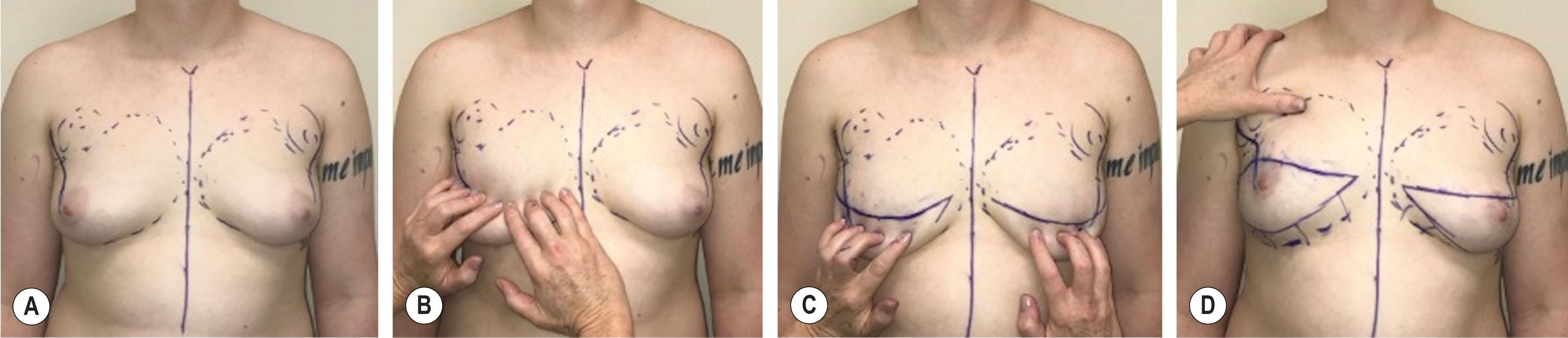
Markings of the midline and breast footprint are performed as in the other techniques. The lateral border of the pectoralis is marked symmetrically ( Fig. 14.4.5A ). Next, with downward manual tension on the overlying breast and skin meant to simulate the tension during skin closure, the projected inferior border of the pectoralis muscle is marked in a gentle curve ( Fig. 14.4.5B,C ). The line is transposed symmetrically to the opposite side using a ruler from the sternal notch. This becomes the superior line of the skin ellipse and will dictate final scar position ( Fig. 14.4.5D ). Non-anatomic scar position will result if this line is placed too high or too low relative to the muscle insertion and requires careful attention. The inferior line is then drawn by a simple pinch technique determining the amount of skin that can be removed and still close without tension. This line is typically 1–2 cm above the IMF (see Fig. 14.4.5D ).
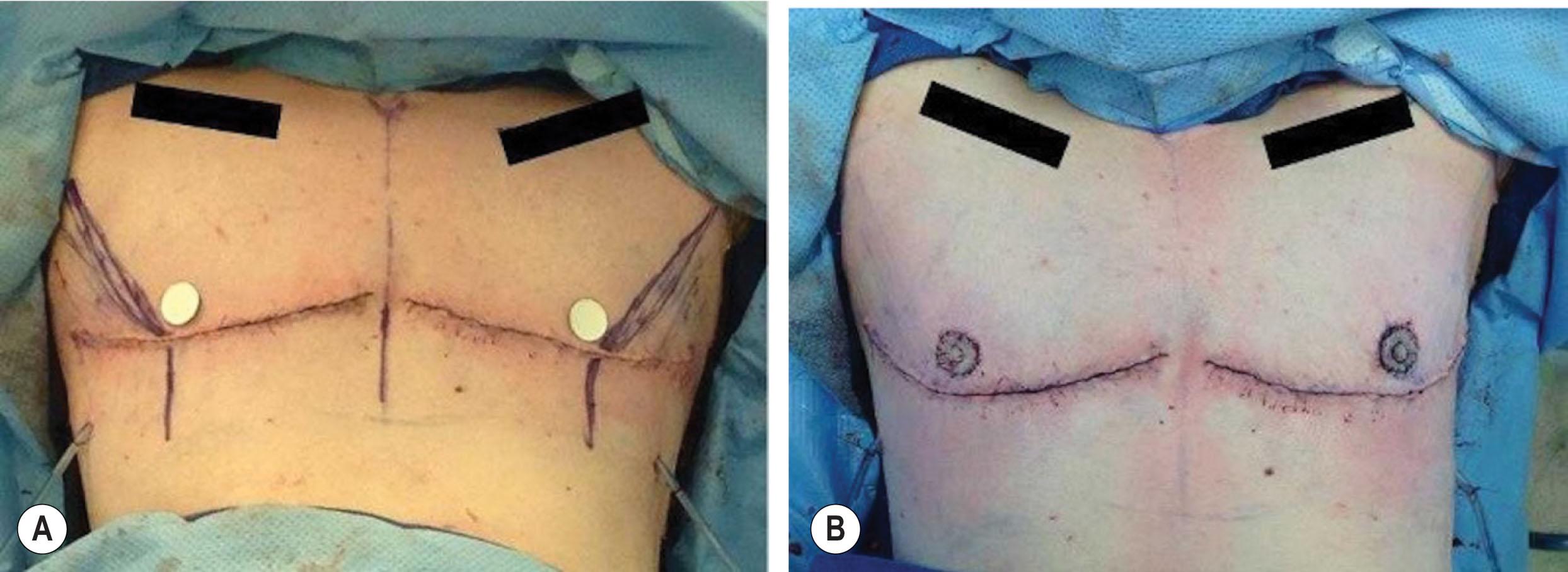
The surgery begins with marking of the NAC with a 2.2 cm circular marker with the breast held on tension. In those with large papilla (>1 cm), we will utilize a composite technique and harvest a 2.2 cm section of areola and a separate portion of the papilla. The grafts are placed on a moistened gauze on the back table for later use. The previously drawn mastectomy ellipses are then incised and carried down to the breast capsule. Skin flaps are raised in the plane separating the breast capsule and overlying the skin and subcutaneous tissue. As with the previous techniques, it is essential that the subcutaneous tissue is preserved, and that the dissection plane follows the breast capsule precisely to avoid overthinning of the skin flap and a hollowed-out appearance. Firm counter-traction of the breast tissue facilitates the dissection. These flaps are elevated to the extent of the pre-marked breast footprint, with care to remove all breast tissue in the axillary tail to prevent unwanted fullness. It is important that the inferior skin flaps are thinned adequately, and that the dissection is carried out past the marked IMF. As with the other techniques, the breast mound is elevated from the pectoralis fascia; this is thought to decrease postoperative pain, bleeding, and seroma formation. After the mastectomy is completed, the skin flaps are temporarily stapled closed, and the patient is then sat up to assess scar position, shape, and symmetry. Adjustments are made with the patient sitting up through a combination of tailor-tacking and staples until optimal scar position is obtained. The patient is returned to a supine position, skin is trimmed, and hemostasis is ensured. A 15 F round drain is placed in the mastectomy cavity and secured in place. The wound is then closed in layers. At this point we proceed with free nipple grafting.
After the mastectomy is completed and closed, the position for the NAC is determined. The patient is sat upright on the operating table and the lateral border of the pectoralis muscle is palpated and marked. Paper templates are used to determine the NAC position. The templates are placed approximately 1.5–2.5 cm above and medial to the pectoralis borders, with final position based on body habitus and surgeon aesthetic judgment ( Fig. 14.4.6 ). The most common error is leaving the NACs too high and too medial, and it is important to avoid this and position the NAC near the inferior insertion and lateral border of the pectoralis for optimal aesthetics. Once the appropriate position has been determined, the patient is returned to a supine position. Because of the tendency for the grafted NACs to elongate in a vertical direction over time along the lines of tension, we have found that modification of the recipient site to a horizontal oval shape has been an effective method to create a final round shape. We begin by drawing the 2.2 cm circle at the optimally determined location of the NAC as described above. In order to orient the oval, a line is drawn through the circle perpendicular to the incision in the direction of greatest tension ( Fig. 14.4.7 ). The circle is then converted to a horizontally oriented oval with the vertical height along this line. Through experience, we have found that oval dimensions of 1.5 cm in height × 2.5 cm in width yield a nearly round NAC in most cases, but these dimensions may need to be adjusted as deemed necessary based on skin tension. This oval is then de-epithelialized for graft placement. The oval recipient site compensates for nipple graft distortion due to the direction of skin tension, with the end result being an NAC that will be more circular over time (see Fig. 14.4.7C ). After securing the graft, pressure bolsters are placed and left in place for one week. As for other mastectomy techniques, gauze and a compression vest are placed. The compression vest, drains, and, if applicable, the nipple graft pressure bolster are left in place for one week. At the first postoperative visit, the bolsters are removed, and grafts and incisions inspected. Drains are removed once they are draining less than 30 mL per day. Patients continue to wear their compression vest for a total of 2–4 weeks. The scars for the double incision technique are well camouflaged if placed along the inferior border of the pectoralis muscle ( Fig. 14.4.8 ).


Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here