Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Blood is a suspension of cells in fluid. It is circulated around the body by the heart and, as a result of this circulation, blood serves as the transport vehicle for gases, nutrients, waste products, cells and hormones.
The fluid is known as plasma and a typical sample is composed of 90% water, 8% protein, 1% inorganic salts, 0.5% lipids, 0.1% glucose and other minor components. The proteins are numerous and diverse, including albumin, blood coagulation factors, anti-proteases, transport proteins and antibodies (immunoglobulins). Collectively, these proteins exert a water-binding effect known as colloidal osmotic pressure which helps regulate the distribution of fluid between the plasma and the extracellular space, serving to keep the fluid in the circulation.
Plasma components, including hormones, lipids, salts, water molecules and small proteins, are constantly exchanged with the extracellular fluid of body tissues in accordance with the blood’s transport functions. Proteins and plasma are not demonstrated by light microscopy except as a background colour.
The cellular components of the blood are:
Red blood cells ( erythrocytes ) are specialised cells containing the red pigment haemoglobin . They provide most of the oxygen transport from the lungs and much of the return carbon dioxide carriage. They are immotile and serve their function only as the result of being passively circulated around the vascular system. The fraction of blood (by volume) occupied by erythrocytes is called the haematocrit and is in the range of 0.35 to 0.50 in adults.
White blood cells ( leukocytes ) constitute an important part of the defence and immune systems of the body but undertake these functions mainly in the tissues; leukocytes in circulating blood are in transit or are simply waiting in reserve. There are five main subtypes of leukocytes.
Platelets ( thrombocytes ) are specialised cells which bind to and coat damaged vessel walls, plug small defects in blood vessel walls and help activate the blood-clotting cascade. They are essential for haemostasis , the system that controls bleeding.
In adults these cells are formed in the bone marrow, a process known as haemopoiesis or haematopoiesis .
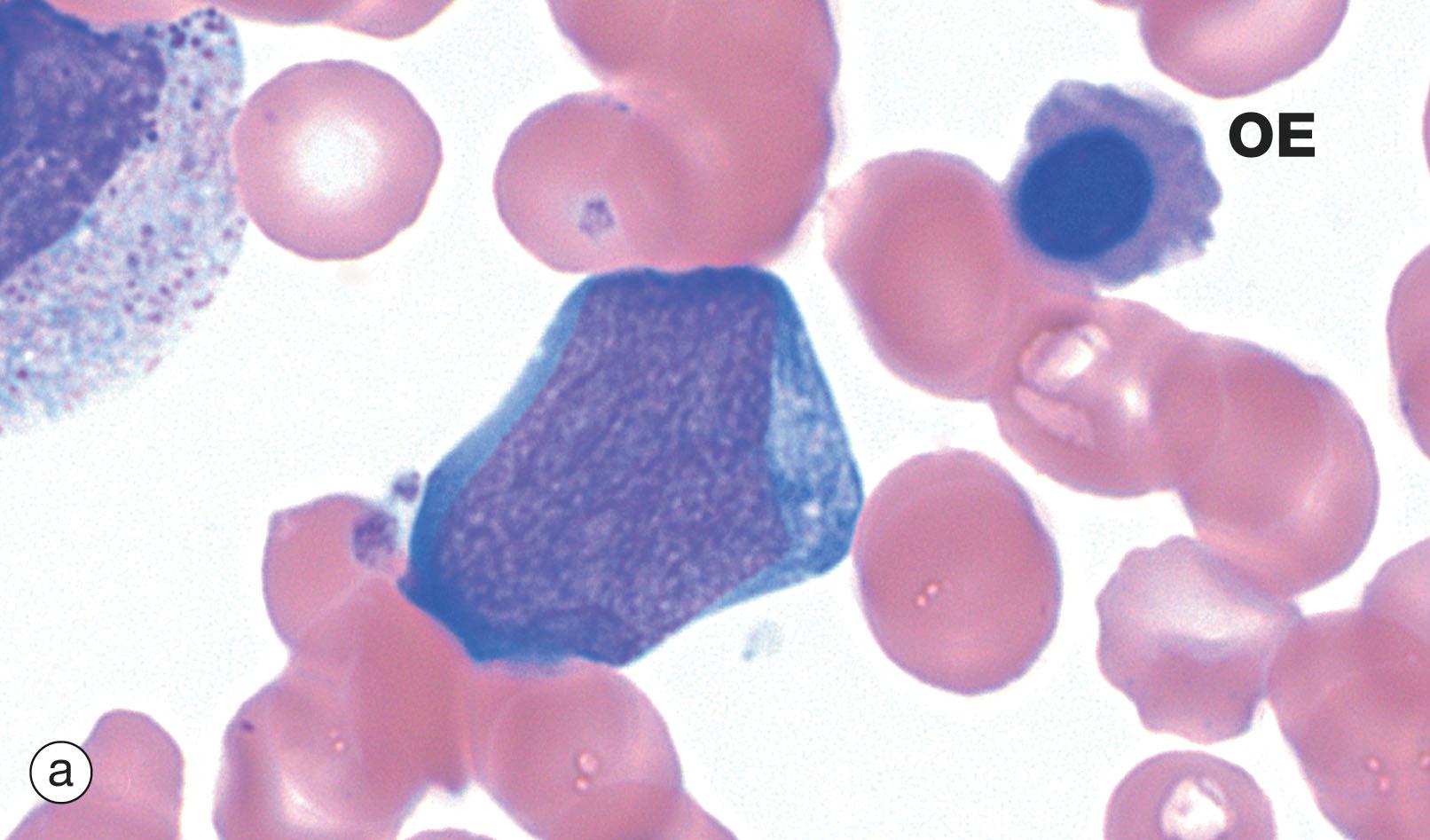
Blood cell numbers are now usually counted by sophisticated laboratory analysers. Blood cell morphology is examined by microscopy using cytological methods. A standard method is to place a drop of blood on a glass slide and spread (smear) it into a very thin layer one cell thick. This smear is then air dried, which results in the cells spreading like fried eggs, making the cells appear larger and giving a clear view into the thinned cytoplasm. These smears are alcohol fixed and stained with Romanowsky-type stains which use polychromatic dyes containing multiple molecular variants to give subtle complexity in the staining. These are the best stains for morphology of blood and bone marrow; common examples are Giemsa and Wright. Distinctive staining characteristics are easily identified and reflect the affinity of the various cellular organelles for different stain components:
Basophilia (deep blue) – affinity for the basic dye methylene blue; DNA in nuclei and RNA in ribosomes.
Azurophilia (purple) – affinity for azure dyes; typically lysosomes, one of the granule types in leukocytes.
Eosinophilia (pink/red) – affinity for the acidic dye eosin, thus also described as acidophilia .
Neutrophilia (salmon pink/lilac) – affinity for a dye once erroneously believed to be of neutral pH; characteristic of the specific cytoplasmic granules of neutrophil leukocytes.
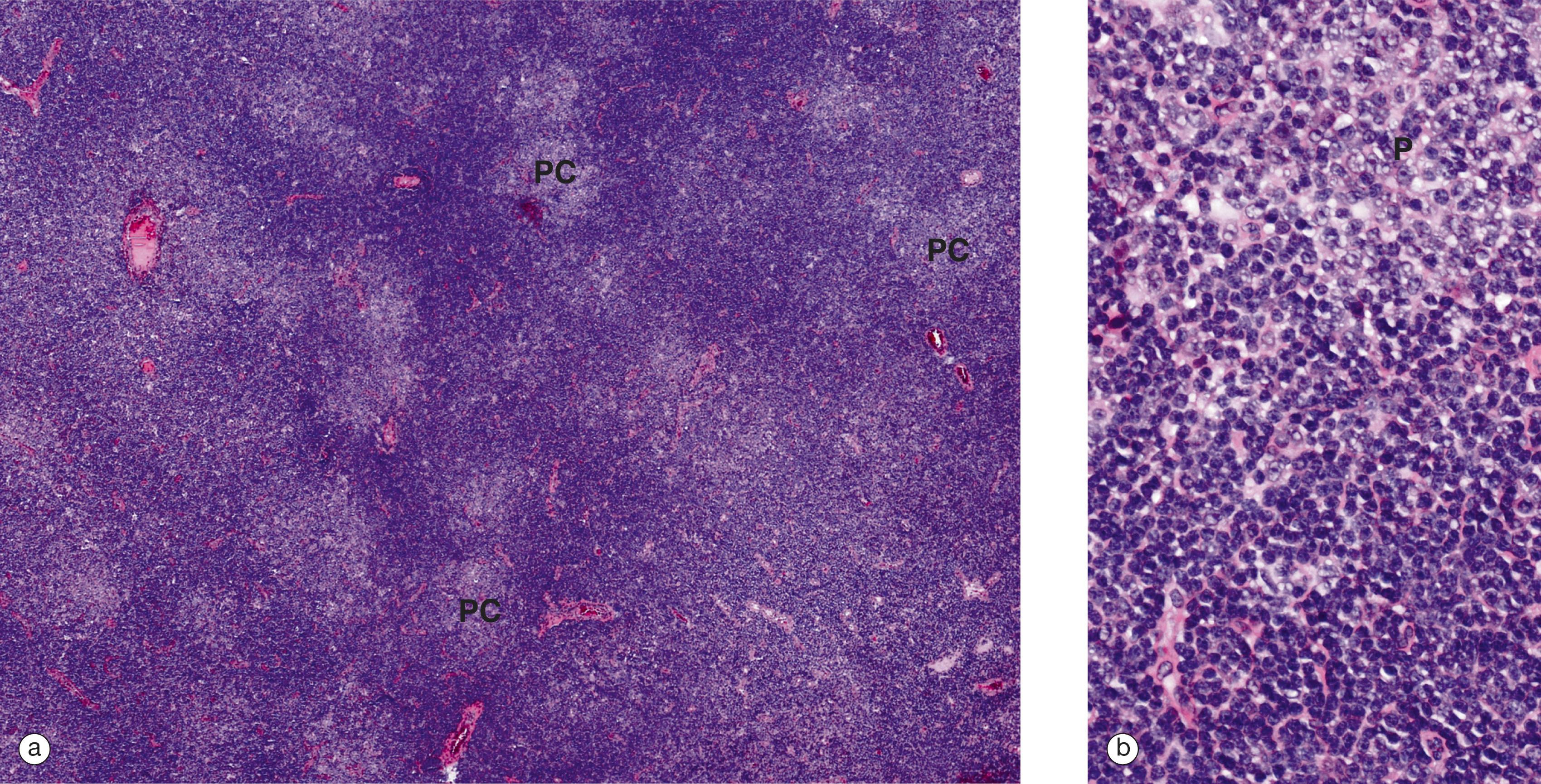
Examination of haematopoietic bone marrow in adults involves sampling from the axial skeleton, usually the iliac crest in the pelvis, with an aspiration sample and often a bone core (also called a trephine). Aspiration samples can also be obtained from the sternum. Aspirated tissue fragments are smeared and stained like blood. Larger tissue pieces and cores of bone are examined as histology preparations, requiring decalcification and often stained with haematoxylin and eosin.
Laboratory analysis of many components of blood, including cells, salts, various proteins, hormones, etc., are a convenient way of examining many body functions. ‘Blood tests’ have a large role in diagnosis and management of disease.
For example, a build-up of creatinine , a breakdown product of wear and tear on muscle, can indicate renal failure. The HbA1c test gives an average blood glucose level to monitor compliance in patents with diabetes mellitus.
Five types of leukocytes are normally present in human blood and are classified into two groups:
Granulocytes
Neutrophils
Eosinophils
Basophils
Mononuclear leukocytes
Lymphocytes
Monocytes
Granulocyte types are named for the staining characteristics of their prominent type-specific cytoplasmic granules: neutrophil (lilac), eosinophil (red) and basophil (blue). Granulocytes have a single nucleus segmented into multiple lobes, assuming variable shapes that led to the use of the term polymorphonuclear leukocytes or polymorphs , mainly because early microscopists mistook the multi-lobed nuclei for multiple nuclei. The term polymorph is sometimes used as a synonym for granulocyte. To confound matters further, polymorph is often used specifically for neutrophils as they are the commonest granulocyte. Granulocytes are also referred to as myeloid cells due to their origin from bone marrow, but they are not the only white blood cells to be formed in bone marrow.
Granulocytes are important components of the innate (non-learned) defences against infection (see Ch. 11 ); however, this role usually takes place in the tissues, not in blood . All leukocytes carry surface proteins which can bind to receptors on the endothelial cells of blood vessels (see Ch. 8 ) and, via this binding, granulocytes actively adhere to vessel walls and then migrate into the tissues using pseudopodial movement .
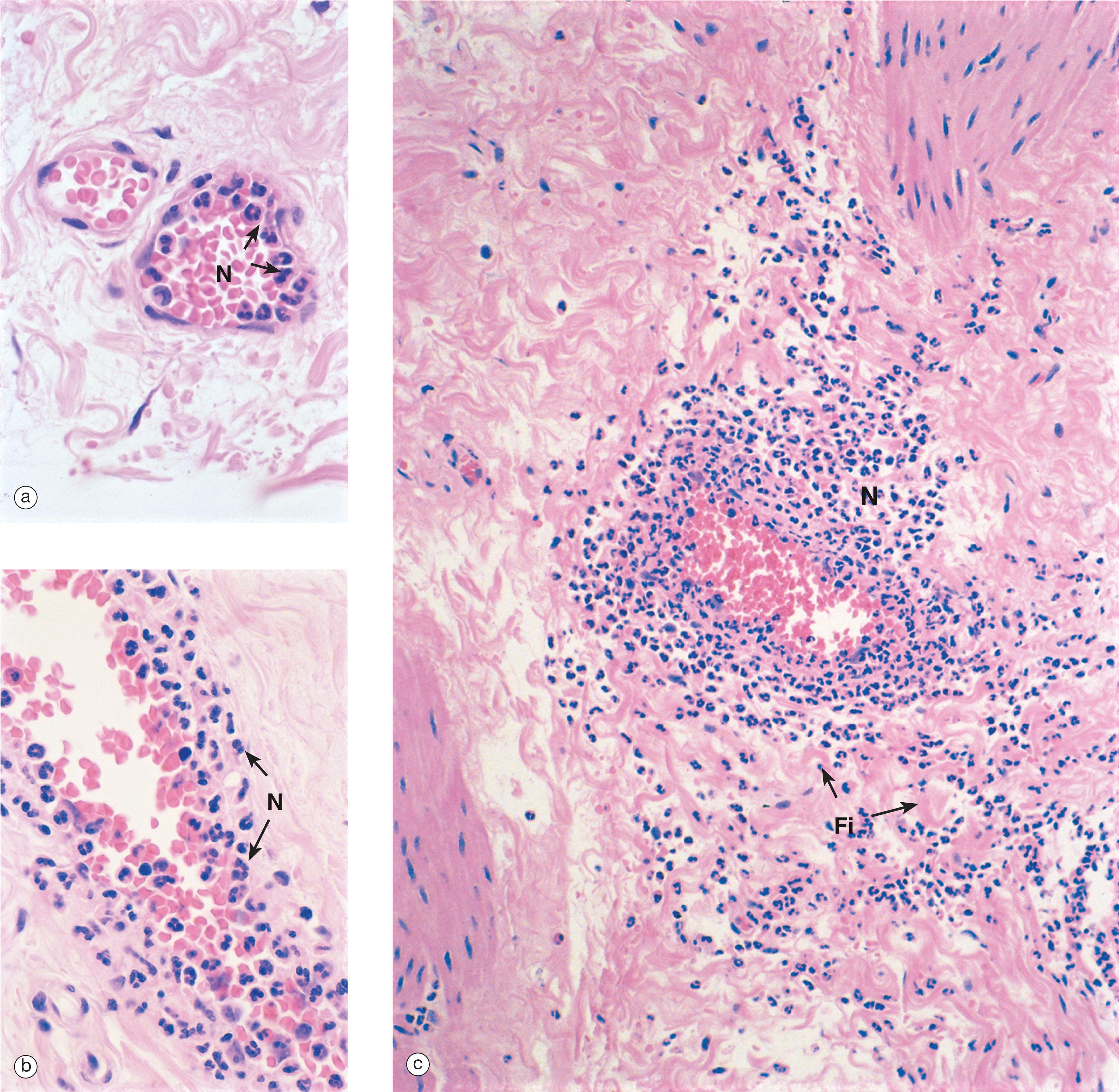
With the exception of eosinophils entering intestinal mucosa, granulocytes do not normally enter tissues in any number; they simply circulate. They enter tissues in response to chemotactic signals and due to changes in the expression of endothelial cell surface receptors, induced by mediators of acute inflammation .
Neutrophils are highly phagocytic . They engulf and kill micro-organisms and ingest cell debris and particulate matter . These cells release multiple important proinflammatory chemical signals and regulators contributing to the overall inflammatory process. Granulocytes have a short functional life; having left the circulation they apoptose in the tissues and do not re-enter the blood.
Lymphocytes and monocytes have non-lobulated nuclei and were described as mononuclear leukocytes by early microscopists to distinguish them from the polymorphs.
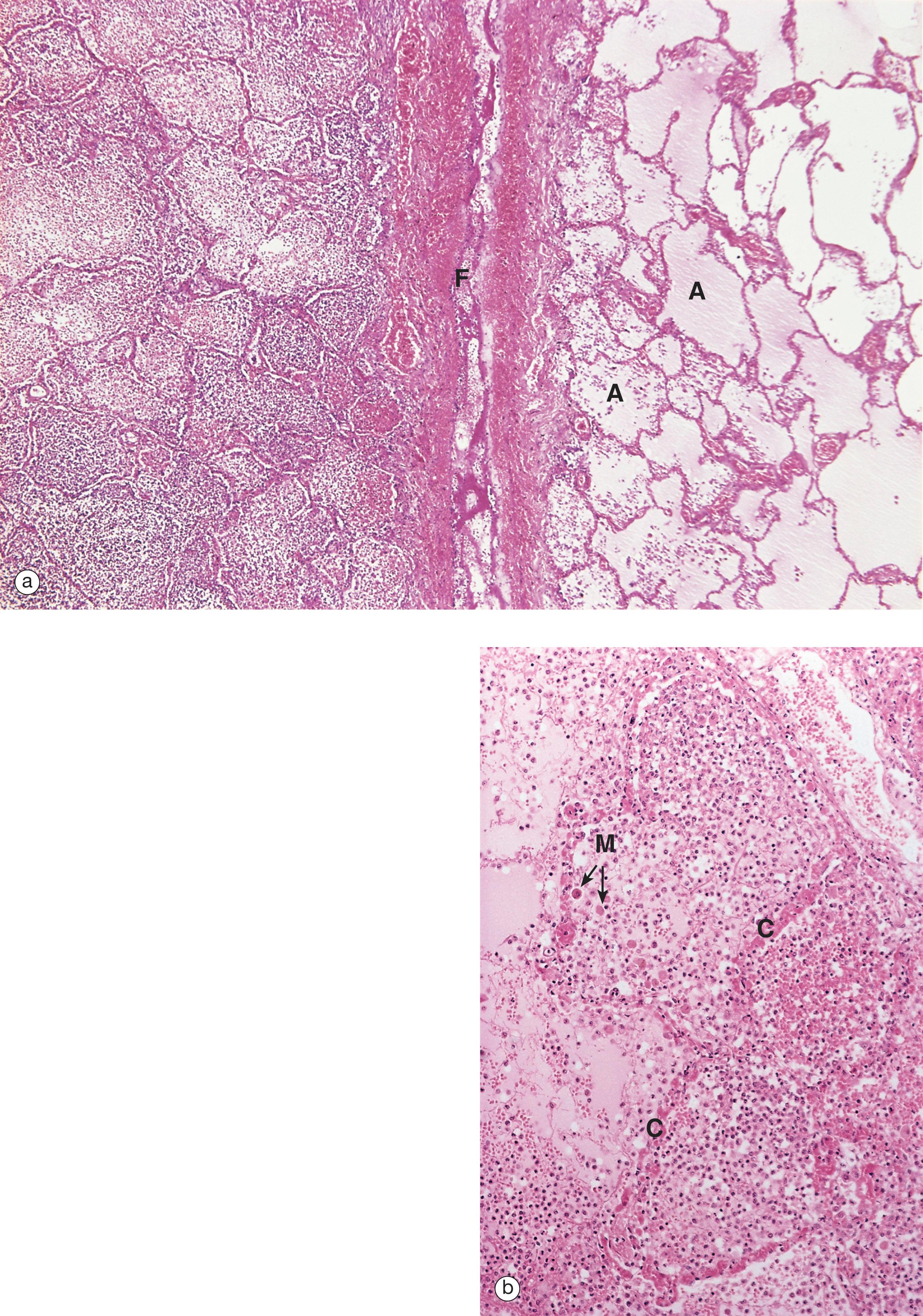
Lymphocytes play a key role in all immune responses, facilitating and regulating inflammation. In contrast to other leukocytes, their activity is directed toward specific foreign agents (antigens), providing a learned and targeted response, both antibody- and cell-mediated. Lymphocytes routinely traffic through tissues, then through lymphatics and lymph nodes and finally re-enter the circulation, providing routine surveillance against foreign antigens. They have an indefinite lifespan and are capable of proliferation.
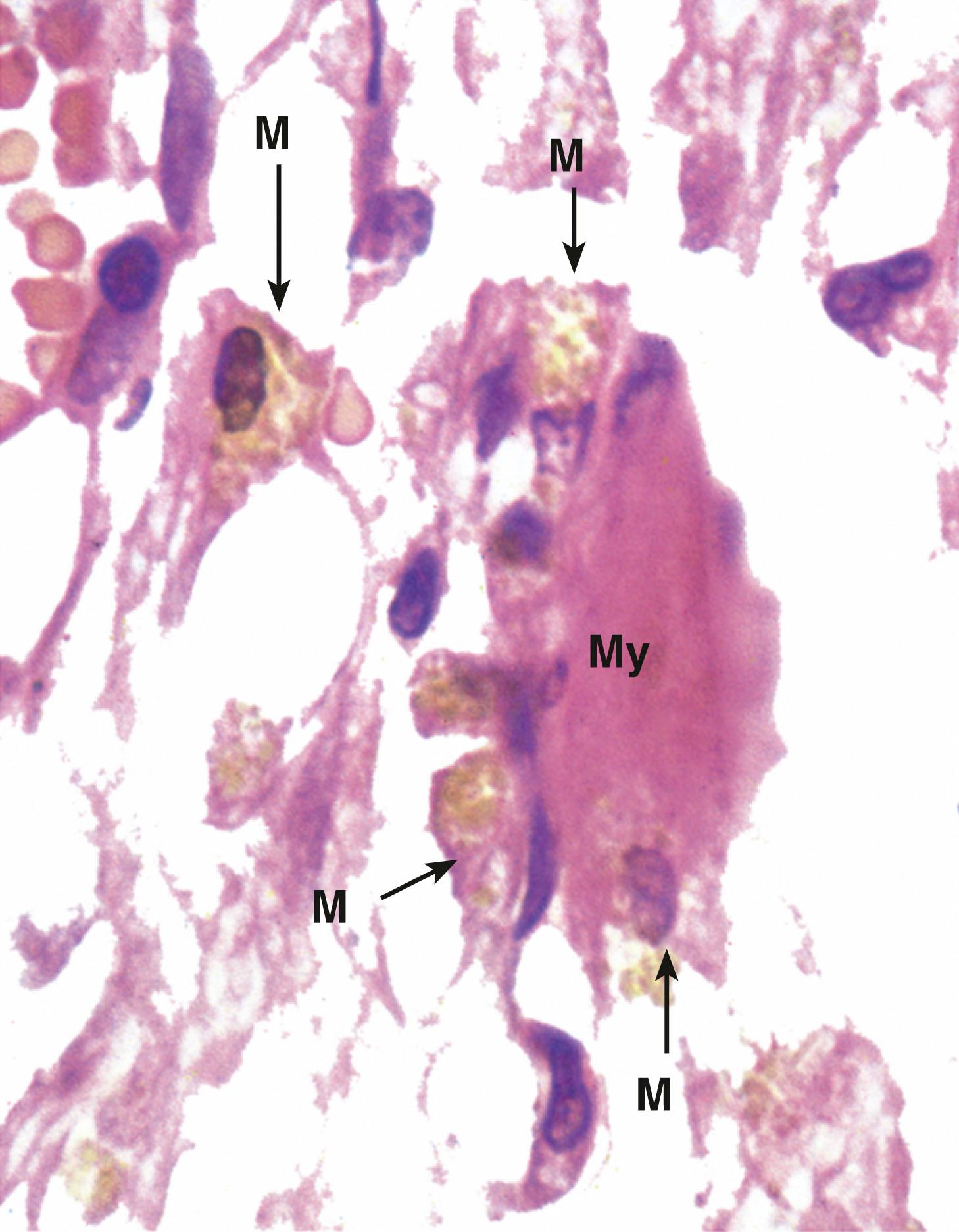
Monocytes are highly phagocytic cells, ingesting micro-organisms, cell debris and particulate matter . They routinely enter some tissues, can mature into macrophages (including becoming resident tissue macrophages ) and can have extended tissue survival.
Monocytes and lymphoid cells produce, secrete and have receptors for a large number of inflammation-related chemical mediators.
The white cells in blood are a cell population in waiting, a reserve pool. When stimulated by chemotaxins and aided by expression of leukocyte receptors on the endothelial cells, the blood leukocytes exit into tissue and become part of the inflammatory process. Numbers in blood might be expected to fall as a result, but a number of mature granulocytes are ready to respond, attached to the lining of small vessels. These form a functional reserve, not included in the blood count, but rapidly mobilised by the chemotaxins and cytokine signals of inflammation.
The same chemical signals stimulate movement of mature and almost mature cells in bone marrow into the circulating blood, forming an additional functional reserve. These signals will also stimulate faster maturation of the existing immature granulocytes in the marrow, which forms yet another reserve, and stimulate increased cell production in marrow from stem cells but this is a slower process.
In most cases of inflammation or infection, the granulocyte blood count will rise. Examples include:
A raised neutrophil count ( neutrophilia ) indicating acute inflammation, especially seen in bacterial infections.
Increased eosinophils ( eosinophilia ) – associated with allergy and parasitic infections.
High lymphocyte counts ( lymphocytosis ) are particularly seen in viral infections.
Transient reduction in neutrophils in the blood ( neutropenia ) can occur due to cytokines produced in early viral infections.
Continued reduction in numbers ( cytopenia ), however, implies that the demand is greater than the supply. This can arise from either increased utilisation or disrupted marrow production.
In very sudden and extremely severe infections, the blood count may fall as the reserve granulocytes are drained faster than increased production can replace them. In these circumstances, immature granulocyte precursors such as band forms, metamyelocytes and myelocytes (see Fig. 3.8 ) may be mobilised to enter the circulation. This is a phenomenon called left shift . A low neutrophil count ( neutropenia ) can be a blood count finding in overwhelming or severe sepsis, especially if there is left shift or in the setting of chemotherapy.
Malignant and pre-malignant diseases of white cell precursors can lead to circulating abnormal white cells ( leukaemia s ) , or the disruption of normal white cell production, leading to cytopenias . In both settings, the normal homeostasis is lost and there are clinical features relating to loss of white cell function, such as repeated infections or an enlarged spleen ( splenomegaly ).
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here