Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Pediatric liver transplantation (LT) has expanded since 1980 because of the broad utilization of segmental grafts including split, living donor, and, occasionally, also reduced grafts. This currently allows achievement of a timely transplant in virtually all the children on the waiting list. As a drawback, the pediatric population is exposed to the specific morbidity related to these kinds of grafts and particularly to biliary complications (BCs).
BCs can occur early or late, with a cutoff ranging, according to different authors, between 1 and 3 months, with early ones being generally considered more as the consequence of technical issues (see Fig. 21.1 ).
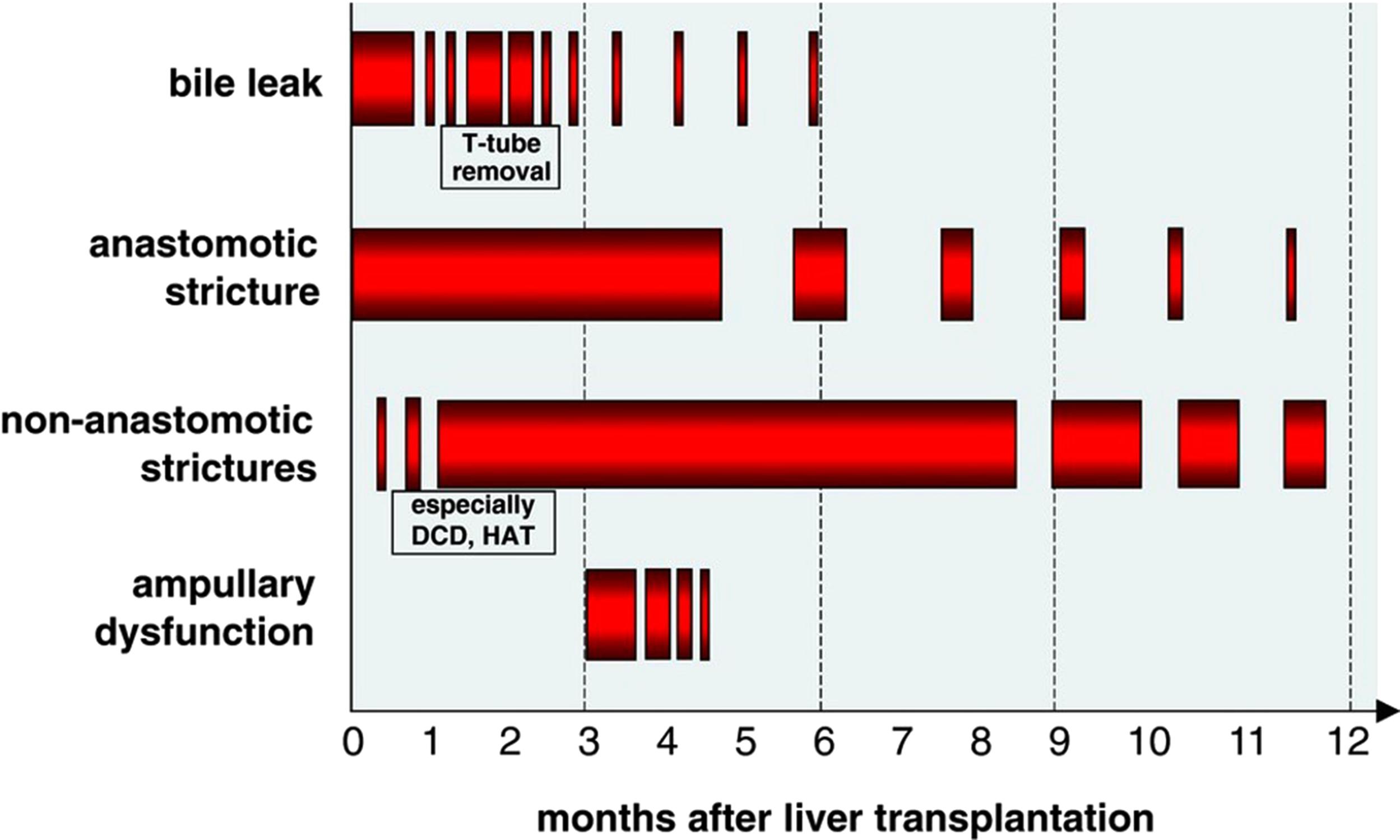
They are classified into biliary strictures (BS), which can be anastomotic or intrahepatic, bile leaks (BL), bilomas, missing or excluded ducts, and stones and cast formation, among others (see Box 21.1 )
The overall BCs incidence in transplanted children varies from 15% to 40%. The type of graft, number of bile ducts, and type of biliary reconstruction performed surely influence the variability in the incidence of BCs, but an important factor is indeed a difference, among centers, in the diagnostic capacity. In fact, the diagnosis, especially in cases of BS, requires a high index of suspicion because, in the initial phases, the clinical picture can be confused with rejection, infection, and primary disease recurrence. Only with early diagnosis and prompt management can high success rates be expected.
Because in children the majority of biliary reconstruction is a bilioenteric anastomosis performed by Roux-en-Y, the preferred method to access the biliary anastomosis in the case of BCs is using a percutaneous transhepatic cholangiography (PTC) to perform the percutaneous biliary intervention (PBI). PTC and PBI represent the mainstay of diagnosis and treatment in pediatric LT, with a success rate between 70% and 90%. However, the duration of these procedures is long, and they are not without complications, both of which lead to higher costs. Surgery is reserved for patients who have failed PBI.
Ischemic injury is crucial. The vascular supply is the most vulnerable point of the biliary system. Whereas the liver parenchyma is nourished via a dual vascular supply (portal vein and hepatic artery), the blood supply to the wall of the biliary ducts relies only on the hepatic arterial flow and is provided by thin periductal arterial plexuses (see Fig. 21.2 ).
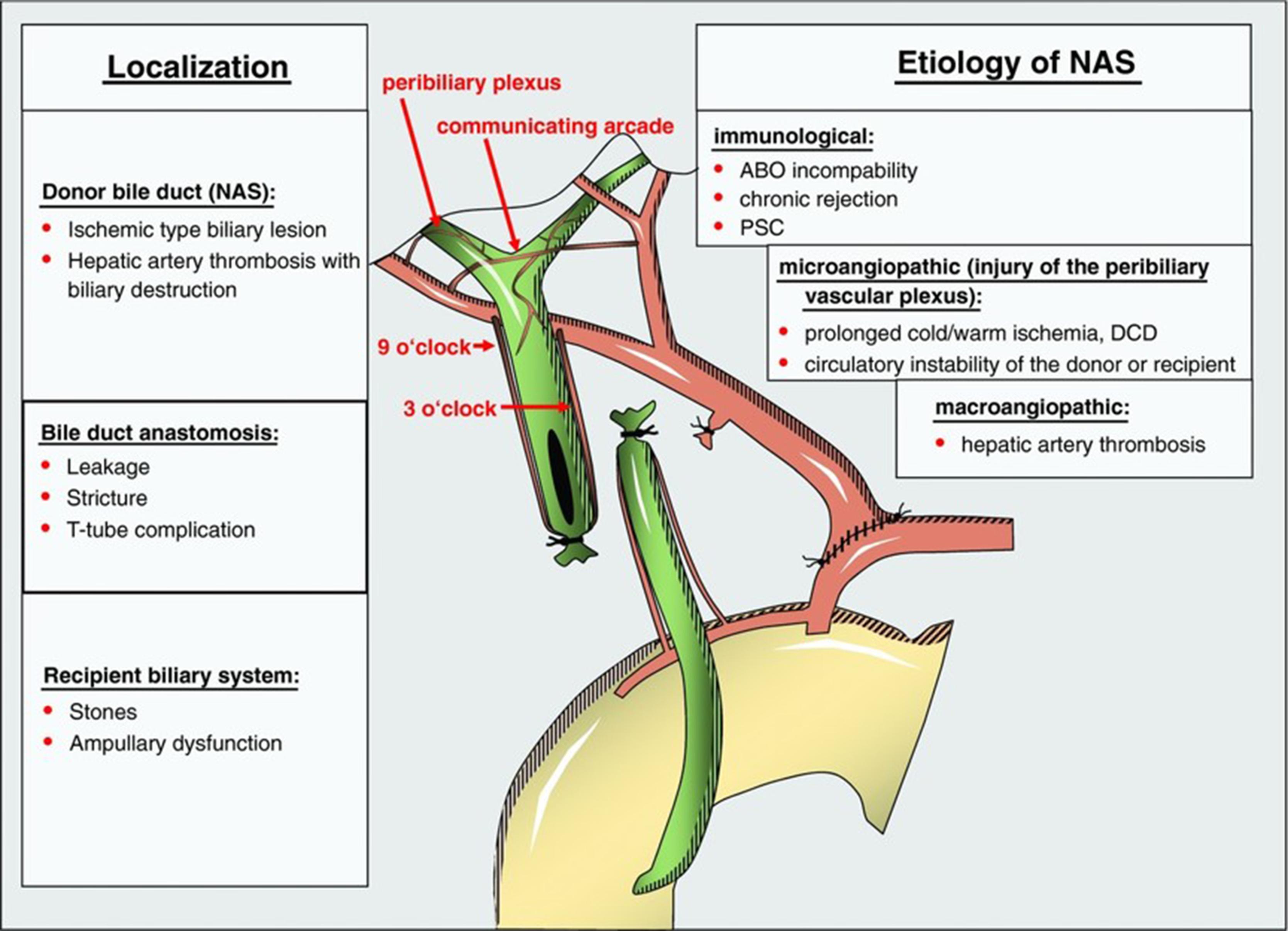
Furthermore, the plexus for the left hepatic duct, which is the anastomotic site for left segmental grafts, most commonly used in children, arises generally from the right branch of the hepatic artery, which is typically not included with the graft itself but left with the right liver. Vascularization is therefore always precarious.
Any added arterial abnormality, such as stenosis or thrombosis, always has a further detrimental effect on the integrity of the biliary tree and represents a significant risk factor, along with cytomegalovirus (CMV) infection and chronic rejection (see Box 21.2 ).
Risk factors for biliary complications
Contradictory data about:
Type of anastomosis: bilioenteric/duct to duct
Graft type: segmental grafts
Multiple ducts?
Technical factors:
Ductoplasty?
Microsurgery?
Sutures (running/interrupted)
Stenting?
Ischemic (arterial or other)
Microangiopathic injury (donor factors)
Preservation injury
Prolonged ischemia times
DCD
Immunogenetic injury (ABO incompatibility, rejection, autoimmune disease, CMV infection)
A second relevant element is the aggressive effect of bile salts on the biliary epithelium, which is enhanced by ischemia. The biliary tree is therefore more exposed to ischemic damage than liver parenchyma during the phases of organ procurement, preservation, and implantation, and both total and warm ischemia time are significant risk factors. Thorough rinsing of bile from the biliary lumen during these phases is also extremely important.
Other technical issues are probably relevant, too, although supporting data are controversially reported in the literature.
As for the type of biliary anastomosis, for several reasons, in children, this is more commonly bilioenteric than duct to duct. However, a choice between the techniques is sometimes possible. In these cases, the preference more frequently goes to the former, although contradictory results are reported favoring either option.
The presence of multiple bile ducts was found to be an independent risk factor for the development of BCs after pediatric LT and has a higher incidence of BL compared with single duct (21% vs. 9%, respectively), particularly when a ductoplasty with single anastomosis, rather than two distinct anastomoses, is performed.
The use of wide-interval interrupted sutures has been reported to decrease the incidence of BCs, whereas the use and the effect of biliary stents are also controversial.
Finally, the use of magnification, be it with operative microscopes or with loupes, and microsurgical techniques may be helpful in preventing complications.
Last but not least, consider that, in most pediatric cases, the biliary anastomosis is performed on the left hepatic duct of a left lateral segment graft. This site is exposed to the development of nonanastomotic strictures (NAS), even in whole-sized liver grafts in adults (see later), corresponding to zone “B” or “C” of the classification of these complications. It seems therefore reasonable to consider that a combination of technical and nontechnical factors may justify the high incidence of complications of anastomoses performed at a site that is at risk even when left intact.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here