Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The bile ducts and vascular conduits of the harvested grafts from living donors are incomplete, thin, and short. The biliary and vascular reconstruction of living donor transplantation is therefore too technically demanding to perform by simple extrapolation of the techniques on whole-liver transplantation.
Hepatic veins are often multiple (middle hepatic vein tributaries and inferior right hepatic veins of the right liver grafts or short hepatic veins of left liver grafts), which requires the plasty for all to one in the bench procedure. Special attention must be paid to ensure that the anastomosis is not causing outflow block in the recipient operation. The portal vein orifices can be multiple (caudate vein for left and caudate lobe graft or anterior and posterior for right liver graft). The diameter of the graft artery is usually 3 mm or smaller, which requires the procedure to be performed using microscopy for secure anastomosis. The bile duct orifices are often multiple, short, and small. Duct-to-duct anastomosis for multiple orifices especially may be impossible when they are located far from each other without the hilar plate of the recipient.
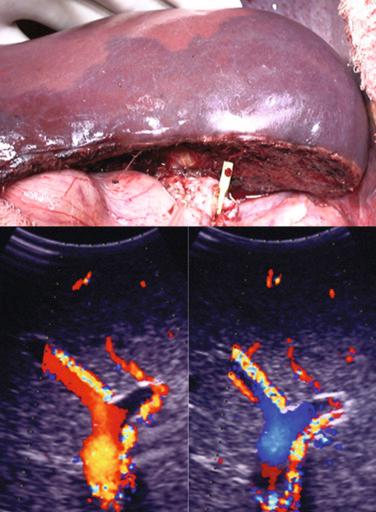
In general the hepatic vein stump should be prepared to be widely opened for outflow reconstruction (except in the double inferior vena cava (IVC) method described later). The IVC is cross-clamped, then the confluence of the left and middle hepatic veins (MHVs) for the left liver or three hepatic veins are opened ( Fig. 54-1 ).When the three hepatic veins are open, the orifice can be shortened by suturing the end of the orifice (right side for left side graft and vice versa). To secure a good and safe surgical field, the cross-clamp on the suprahepatic vena cava should be placed as far cranial as possible. Ligating and dividing the phrenic veins on both sides, as performed in the donor operation, allows the IVC to be safely cross-clamped on the cranial side ( Fig. 54-2 ).
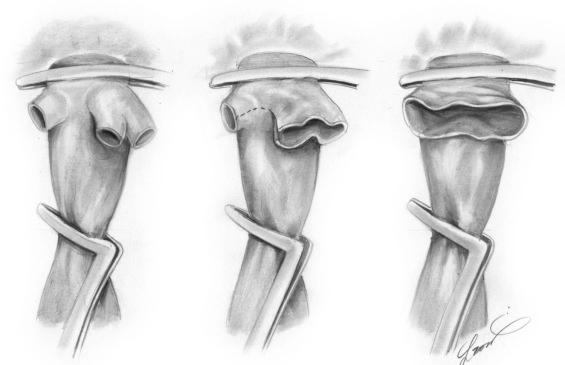
The orifice of the recipient right hepatic vein is maximally extended onto the IVC caudally and to the left to provide for optimal graft outflow. It is important to recognize that regeneration causes the right liver graft to rotate axially from right to left ( Fig. 54-3 ).
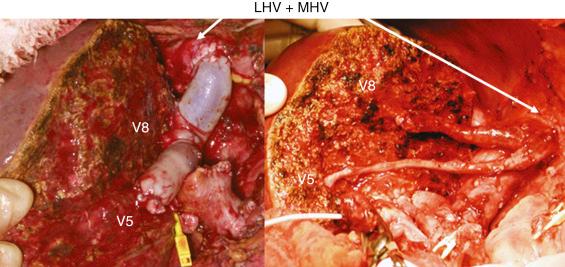
When the right liver graft is harvested without an MHV graft, the venous tributaries must be considered. Without reconstruction, the part will be congested and will not function well after reperfusion, causing poor regeneration and resulting in small-for-size syndrome.
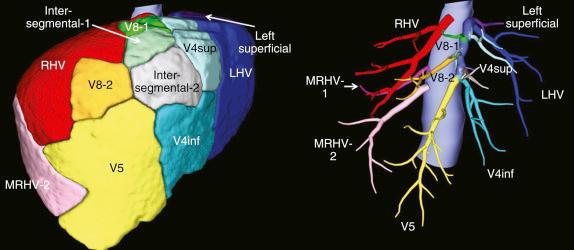
The indication for MHV tributary reconstruction should be determined preoperatively by measuring the drainage area volume of the major tributaries of the MHV. If the uncongested area (i.e., area drained by the right hepatic vein) is sufficient for the metabolic demands of the recipient (usually 35% to 40% of the recipient standard liver volume), reconstruction of the MHV tributaries is not necessary and vice versa ( Fig. 54-4 ).
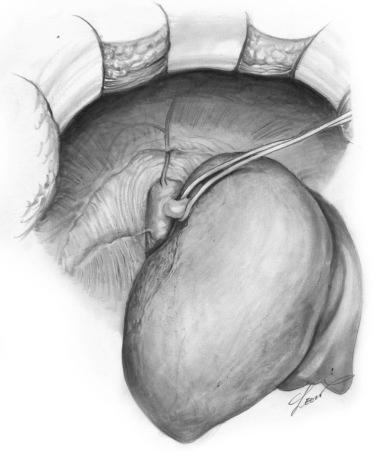
The drainage area can be confirmed during the donor hepatectomy and in the recipient operation after reperfusion. In the donor operation the examination must be performed after dissecting the parenchyma and cutting the MHV tributaries, and before cutting the inflow vessels. There are two possible methods ( Fig. 54-5 ). The first is to check the flow of the anterior branch of the portal vein by Doppler ultrasonography. If the area is congested, the portal vein flow is hepatofugal. The second is to temporarily clamp the right hepatic artery. The congested area will have a dark red surface because the area has no inflow. In the recipient operation the congested area will be seen as the area with a dark red surface just after portal vein reconstruction and reperfusion. The color difference between the congested and uncongested areas should disappear after the hepatic arterial reconstruction because the ischemia will be alleviated. Confirmation is important because there can be communication veins between the right hepatic vein and MHVs (20% to 30% in healthy donors), which sometimes cannot be diagnosed preoperatively. When communication veins are present, reconstruction of the MHV tributaries is not necessary.
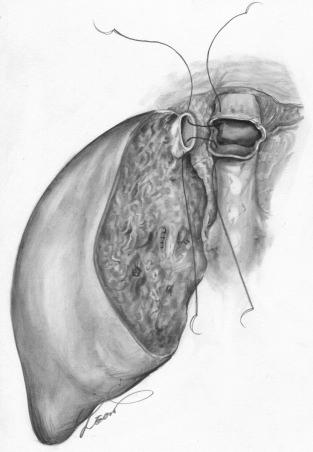
MHV tributaries are usually reconstructed at the bench. A vein graft will require interposition. Autografts (recipient’s jugular vein or iliac vein), cryopreserved vein, or arterial grafts ( Fig. 54-6 ) and artificial grafts (polytetrafluoroethylene) may be used.
When the area drained by the inferior right hepatic vein is predicted to be wide based on the preoperative evaluation, reconstruction should be considered. Direct anastomosis between the inferior right hepatic vein and the recipient IVC is sometimes technically demanding. Because determining the optimal anastomotic site and direction is difficult and requires time, this may increase the warm ischemic time. In such cases, if the IVC graft is available, the right inferior vein can be reconstructed at the bench, which is called the double IVC method . If the IVC graft is not available, but a thinner vein graft such as the femoral vein is available, similar reconstruction is possible ( Fig. 54-7 ). We must note that, in this case, extensive dissection of the IVC around the hepatic vein branches, including the phrenic veins, is unnecessary.
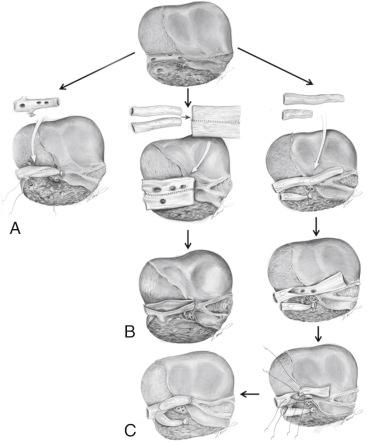
A rooflike venous patch around the graft’s left hepatic vein and MHVs at the bench simplifies the reconstruction in the recipient operation. When the left-sided caudate lobe is included with the left liver graft, venous drainage of the caudate lobe should be considered for comparable regeneration between the left liver and caudate lobe.
Direct anastomosis between the short hepatic vein and the recipient IVC can be performed. When a short hepatic vein, left hepatic vein, and MHVs are located close to each other, simple venoplasty at the bench is possible. Another option includes venoplasty using vein grafts at the bench. On the graft side a wide venous orifice with a long cuff is formed by gathering the left, middle, and short hepatic veins using a conduit vein graft and patch vein grafts.
Caval drainage is one of the most important techniques in partial graft implantation. Not only the anastomosis, but also the graft positioning can be important for the outflow. The graft should be placed in an orthotopic position, and care should be taken to consider the final position of the graft once the abdomen is closed. Especially for left liver grafts, it is important to fix the falciform ligament to the midline of the abdominal wall to prevent graft rotation to the right side.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here