Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
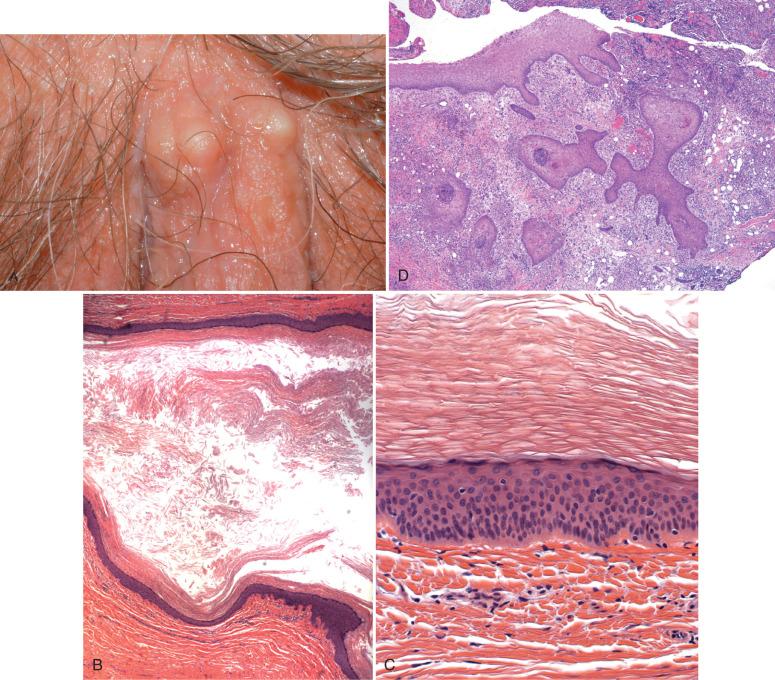
The clinician and pathologist must recognize benign cysts and adnexal lesions of the vulva to exclude more serious conditions and avoid misclassifying them as malignancies ( Table 5.1 ). They typically do not pose a diagnostic problem with the exception of (1) ectopic breast tissue, particularly when containing fibroadenomas; (2) endometriosis, particularly if it is gland-poor (stromatosis); and (3) hidradenoma papilliferum (HP), which may be interpreted as a malignancy by the uninitiated.
| Entity | Notes |
|---|---|
| Bartholin duct cysts and abscesses | Posterior introitus; transitional epithelium |
| Skene duct cyst | Near distal urethra; transitional epithelium |
| Epidermal inclusion cyst (EIC) | Associated with prior trauma or circumcision; pseudoepitheliomatous change may mimic neoplasia |
| Mucinous and ciliated cysts | Vulvar vestibule; urogenital sinus origin most plausible; mucinous with squamous metaplasia |
| Gartner duct cyst | Rare in vulva, uncommon in vagina (see Chapter 11 ) |
| Cyst of the canal of Nuck | Unilateral labial swelling; cyst on labium majus and femoral region; derived from processus vaginalis |
| Syringoma | Proliferations of adnexal eccrine epithelium separated by fibrous stroma; frequently multiple |
| Hidradenoma papilliferum (HP) | Well-circumscribed painless discrete nodule usually <2 cm; papillary glandular epithelium with myoepithelial cells; may be confused with malignancies |
| Syringocystadenoma papilliferum | Rare benign hamartomatous adnexal tumor of uncertain origin |
| Anogenital mammary-like glands and associated lesions | Rare; may be misdiagnosed as neoplastic with ducts and lobules, but well-circumscribed mass; rarely contains fibroadenoma and phyllodes tumor |
| Endometriosis | May be associated with prior trauma; rarely gives rise to carcinoma |
| Lymphangioma circumscriptum | Numerous small cutaneous vesicles or blebs; dilated lymphatics |
| Cavernous lymphangioma | Presents as a cystic mass |
| Angiokeratoma | Multiple cysts of the vulva |
These are covered in recent reviews as well.
Benign vulvar cysts generally fall into four categories: Bartholin duct cysts, epidermal inclusion cysts (EICs), mesonephric remnants, and mucous cysts. Additional rare cysts include Skene duct and prolapsed urethral tissue.
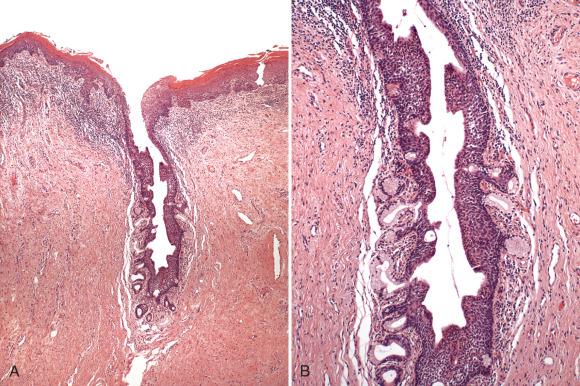
Cysts in the region of the Bartholin gland often involve the duct and are termed Bartholin duct cysts . The orifices of the ducts draining the Bartholin glands are typically located in the posterior introitus (5 o'clock and 7 o'clock positions in lithotomy). Bartholin duct cysts presumably follow obstruction of the duct and may be accompanied by infection and an abscess formation ( Fig. 5.1 ). Rarely these lesions may be detected on imaging.

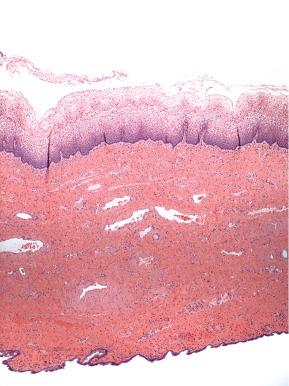
Histologically, a Bartholin duct cyst is lined by a transitional or squamous epithelium and the specimen often contains associated Bartholin gland ( Fig. 5.2 ). The diagnosis is made by identification of the transitional epithelium and gland (if obtained). Its distinction from a Skene duct cyst is based principally on its posterior rather than periurethral location ( Fig. 5.3 ). The clinical differential diagnosis also includes mucous cysts, EICs, benign adnexal tumors (hidradenoma), and soft tissue tumors, such as lipomas.

Traditionally, the management of a Bartholin duct cyst/abscess consisted of insertion of a Word catheter. Another option is marsupialization for Bartholin duct cysts/abscesses. Antibiotic therapy is recommended in the setting of cellulitis. If a cyst recurs after marsupialization, removal of the entire cyst, duct, and gland (if possible) is recommended. As with all cysts, other vulvar neoplasms must be excluded, specifically carcinomas arising in the Bartholin gland or duct (see Chapter 7 ). The latter, however, are extremely rare.
The Skene glands (also known as the periurethral glands, lesser vestibular glands, or paraurethral glands ) are located on the anterior wall of the vagina, around the distal part of the urethra (see Fig. 5.3 ). They secrete a viscous lubricating fluid upon sexual arousal, which drains into the urethra and periurethral openings. Skene duct cysts are rare and may occur in newborns, where they present as discrete periurethral pea-size swellings. In adults, they are occasionally reported in association with dyspareunia.
Like Bartholin duct cysts, Skene duct cysts are lined by transitional epithelium and in some cases squamous epithelium if sampled near the surface. A variable amount of chronic inflammation is typically encountered.
The most important distinction is a clinical one between Skene duct cysts and similar entities, such as ectopic ureterocele, urethrocele, urethral diverticula, and benign or malignant urethral and paraurethral tumors.
Management consists of marsupialization or removal of the cyst.
Mucous cysts occur over a wide age range but are usually seen in multiparous women in the third and fourth decades. They present exclusively in the region of the vulvar vestibule and in the majority are solitary lesions of 1 to 2 cm in diameter. They are usually asymptomatic, but patients may complain of pain if the cysts have recently enlarged or impinge on the urethra, where they may cause dysuria.
The origin of mucous cysts has been debated in the past. Theories of origin include invagination of overlying squamous epithelium with mucinous metaplasia, para-mesonephric (müllerian) origin, and origin from urogenital sinus epithelium. The first is unlikely, because most mucous cysts do not communicate with the overlying squamous epithelium, and the squamous differentiation in these cysts is of a metaplastic nature. The paramesonephric origin has been challenged by others who emphasize that the müllerian ducts terminate in the region of the hymen and play no part in the development of the vulvar vestibule. Moreover, the most caudal extension of müllerian epithelium seen in diethylstilbestrol exposure is cephalad to the hymen. Finally, clear cell carcinoma, a tumor arising in müllerian epithelium, has not been reported in the vulvar vestibule. Urogenital sinus epithelium remains the most plausible, inasmuch as both ciliated and mucous cells have been observed in derived epithelium, including the Bartholin gland.
The development of mucous cysts appears to be hormone related in that the lesions occur most frequently in the reproductive years, including during pregnancy.
Histologically, mucous cysts contain mucinous epithelium identical in appearance to that lining the endocervix or vaginal adenosis ( Fig. 5.4 ). Less commonly, they contain squamous metaplasia ( Fig. 5.5 ). Ciliated cells have been reported in some cases and may be mixed with the mucinous epithelium.
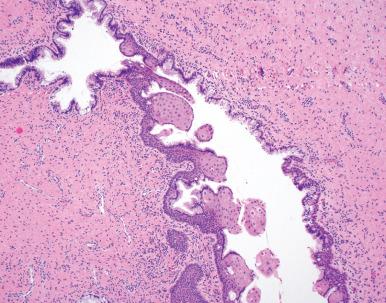
The differential diagnosis of mucous cysts includes mesonephric remnants (cuboidal epithelium and a fibromuscular wall) and Bartholin duct cysts (transitional epithelium). The labium minus transverses over the middle of the Bartholin cyst.
Mucous cysts are managed by local excision, which is typically for diagnostic purposes.
EICs occasionally occur in the vulvar region and are most commonly associated with prior trauma or circumcision. Vulvar EICs may become infected and management is similar to that of cutaneous EICs ( Fig. 5.6A ).
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here