Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
A cyst can be defined as a pathologic cavity having fluid, semifluid, or gaseous contents, and not created by accumulation of pus. It does not necessarily have an epithelial or endothelial lining; inclusion of lining in the definition results in a somewhat artificial distinction between pseudocysts and “true” cysts.
Benign cystic lesions of salivary glands may be developmental, degenerative, or neoplastic. In Sections 9.1 and 9.2 , we focus on degenerative lesions that include mucoceles, mucous retention cysts, salivary duct cysts, and the specific entity of ranula.
Ranula presents as a translucent submucosal swelling in the floor of mouth, arising from collection of saliva extravasated from a sublingual salivary gland (SLG). Wiseman stated in 1676 that ranulas could cause a croaking speech, and this, together with the resemblance of the oral ranula to the belly or air sac of a frog, justified the term ranula, meaning little frog (Latin: rana = “frog”; ulus = “small”). If extravasated saliva tracks inferior to the floor of mouth formed by the pair of mylohyoid muscles, the term diving, plunging, or cervical ranula is applied.
The anatomy of the sublingual space dictates the pathogenesis of ranula and the rationale behind its definitive treatment. The SLG consists of unencapsulated mucinogenic glandular tissue lying within areolar tissue between the mylohyoid muscle and oral mucosa. Several lesser sublingual glands commonly drain through individual ducts of Rivinus into plica sublingualis. Greater SLG, if present, lies posteromedial to the lesser glands and drains via Bartholin's duct into either Wharton's duct or directly into the caruncula sublingualis.
Over 40% of cadavers have a dehiscence in the mylohyoid muscle that can allow herniation of the SLG or saliva extravasation into the neck.
Harrison has proposed two theories for pathologenesis: extravasation of mucus through damaged duct of Rivinus or from herniated SLG, secondary to trauma or obstruction. The SLG secretes mucinous saliva spontaneously without the need of neurological stimulus. Outside the confines of the sublingual gland and duct system, extravasated saliva is only limited by either the space between mylohyoid and mucosa in the oral cavity or by inflammatory fibrosis within tissues in the neck and removal of mucin by macrophages. The former process forms a simple ranula and the latter forms a plunging ranula, both bounded by inflammatory granulation tissue, not epithelium. Epidemiologic study has revealed a high risk of plunging ranula among Maori and Pacific Islanders.
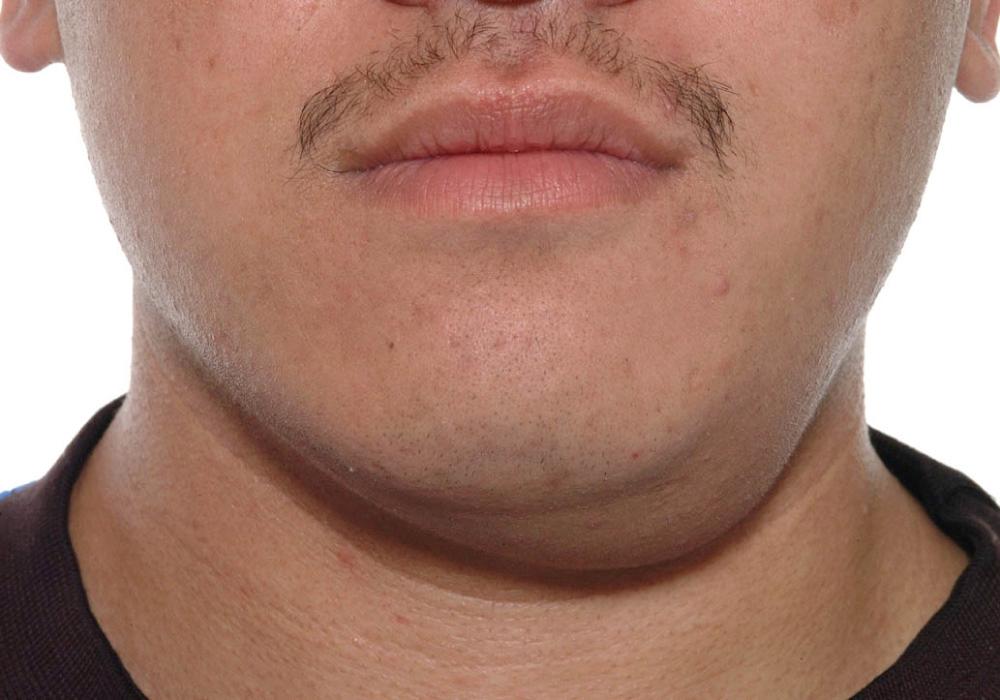
Most ranulas appear within the first three decades of life. Common presenting features are disruption to normal oral function from floor of mouth swelling ( Fig. 9.1.1 ), and cosmetic concerns in cases of plunging ranula ( Fig. 9.1.2 ). Specific history of trauma is usually absent. Episodes of increase in swelling associated with pain and tenderness secondary to inflammation may occur. Indeed, many misdiagnosed cases of plunging ranula may undergo incision and drainage for a presumed (dental) abscess that turns out to be an inflamed pseudocyst.

Differential diagnosis for this clinical presentation includes abscess, simple (e.g., dermoid) cyst, thyroglossal duct cyst, cystic hygroma, lymphangioma, and lipoma. Clinical diagnosis of ranula is usually straightforward. However, diagnostic errors may still arise. Atypical presentation may confound, as described by Abt et al., who reported a case of plunging ranula with direct extension to the prestyloid parapharyngeal space, masticator space, and parotid gland without involving the submandibular space.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here