Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Advances in ultrasound technology continue to enhance its diagnostic applications in daily medical practice. Constantly evolving, this tool has become invaluable for properly trained cardiologists, anesthesiologists, intensivists, surgeons, obstetricians, and emergency department physicians. Ultrasound can enable rapid, accurate, and noninvasive diagnosis of a broad range of medical conditions. Patients in the intensive care unit (ICU) present daily diagnostic and therapeutic challenges to the medical team. The availability of ultrasound instrumentation in critical care units has facilitated greatly the rapid evaluation and treatment of patients with a wide spectrum of conditions. Although transthoracic and transesophageal echocardiography (TEE) have been generally available for years for evaluating ICU patients, advances in ultrasound imaging, including harmonic imaging, digital acquisition, and contrast for endocardial enhancement, have improved the diagnostic yield. Modern techniques are simple and safe to use. Ultrasound devices continue to become even more portable than in the past, and hand-carried devices now are readily available for everyday clinical use (point-of-care ultrasound [POCUS]). The spectrum of POCUS is quite broad, and many of its key imaging applications are discussed elsewhere. In this chapter we place emphasis on echocardiography and cardiovascular diagnostics. The use of bedside ultrasound to facilitate central line placement and to aid in the care of patients with pleural effusions and intraabdominal fluid collections also is addressed.
Ultrasonography has become an invaluable tool for managing critically ill patients. Its safety and portability allow for use at the bedside to provide rapid, detailed information regarding the cardiopulmonary system and to assess the function and anatomy of certain internal organs. It also can be used by the clinician to interrogate the pleural and intraabdominal spaces and to perform some invasive procedures safely. General indications for the performance of echocardiography in the ICU are listed in Box E2.1 . Box E2.2 lists major indications for performance of primary TEE in the ICU. Other indications for the use of bedside ultrasonography by the intensivist in critically ill patients are listed in Box E2.3 .
Hemodynamic instability
Ventricular failure
Hypovolemia
Pulmonary embolism
Acute valvular dysfunction
Cardiac tamponade
Complications after cardiothoracic surgery
Infective endocarditis
Aortic dissection and rupture
Unexplained hypoxemia
Source of embolus
Diagnosis of conditions in which the superior image quality is vital (e.g., aortic dissection, assessment of endocarditis and its complications, intracardiac thrombus)
Imaging of structures that may be inadequately seen by TTE (e.g., thoracic aorta, left atrial appendage, prosthetic valves)
Echocardiographic examinations of patients with conditions that prevent image clarity with TTE (e.g., severe obesity, emphysema, mechanical ventilation with high level of PEEP, presence of tubes, surgical incisions, dressings)
Acute perioperative hemodynamic derangements
Central line placement
Assessment of pleural effusions and intraabdominal fluid collections
Urinary bladder scan
FAST
Intraaortic balloon counterpulsation
Ventricular assist devices
The practical value of bedside ultrasonography in the management of critically ill patients is now widely accepted, despite the inherent limitations of the technique. These limitations arise primarily from the suboptimal imaging conditions commonly encountered when performing studies of the critically ill. The constrained physical environment of the ICU also can compromise the quality of the images obtained. For an ultrasound study to be deemed adequate, a good acoustic “window” is required to allow accurate analysis. Ultrasonography uses the physical principle that sound is reflected from tissue interfaces, allowing a two-dimensional (2D) image of the anatomic structure studied to be constructed. Anything hindering the reflection of this acoustic signal—air, bone, calcium, foreign body, or other interposed structure—interferes with ultrasound transmission and diminishes the overall quality of the examination. In the ICU, many patients are mechanically ventilated. In these patients, adequate imaging can be limited by complications such as pneumothorax, pneumomediastinum, or subcutaneous emphysema. Other important factors limiting quality data acquisition in critically ill patients are related to surgical wounds and dressings, tapes, tubing, obesity, and chronic obstructive pulmonary disease. In addition, lack of patient cooperation and the impossibility of moving some patients into the optimal position for the desired examination contribute to a high prevalence of technically inadequate studies.
Although ultrasonography permits evaluation of the structure and function of the heart and other important organs and structures, acquisition of data and interpretation of results are fraught with potential traps. Performing an ultrasound examination requires a thorough knowledge of anatomy and instrumentation, including attention to gain control, grayscale settings, Doppler velocity settings, and transducer placement.
Before starting an ultrasound examination at the bedside in the ICU, certain important criteria should be met. The criteria vary, depending on the type of examination being performed (transthoracic echocardiography [TTE]; TEE; vascular, abdominal, or thoracic ultrasound) and on certain patient-related factors (e.g., presence or absence of mechanical ventilation, nasogastric tube, or surgical dressings).
An awake patient should be informed about the importance of the ultrasound investigation and should be provided with an explanation of how the clinician will perform the examination. These steps are especially important when the examination uses the transesophageal route.
Proper positioning of the patient is important for obtaining an adequate image. For performance of TTE and TEE in patients who are not mechanically ventilated, optimal imaging usually is obtained by having the patient in the left lateral decubitus position. Taking the extra 5 minutes to position the patient on his or her left side for TTE often results in much improved image quality and minimizes aspiration risk. Adequate positioning of the patient depends on the structures being assessed (e.g., pleural space, peritoneal cavity, vascular structures, or bladder). Care must be taken when positioning a critically ill patient in bed, because these patients often have multiple vascular catheters, an endotracheal tube, drains, and other tubes or devices connected to them. When the ultrasound examination is performed to localize and mark pleural or abdominal fluid collections for subsequent drainage, it is crucial that the patient be placed in the same position used during the actual drainage of the collection. Risks of perforating surrounding organs (e.g., heart, spleen, liver, lungs, or bowel) and inducing significant morbidity are increased if the drainage is performed in a position different from the one used during marking.
To optimize the ultrasound examination, the patient must be cooperative and nonagitated. Noninvasive procedures such as TTE and abdominal ultrasound usually are well tolerated, and additional sedation rarely is needed to perform them. When performing TEE, however, certain precautions need to be taken. Patients should fast (or have their tube feeds stopped) for at least 4 hours before the procedure. Topical anesthesia of the oropharynx also is helpful before insertion of the TEE probe, especially in patients who are not endotracheally intubated. Even if adequate topical anesthesia is provided, insertion of the TEE probe still can cause significant discomfort and anxiety, so providing adequate sedation and analgesia is important. Frequently used sedative or analgesic agents include intravenous (IV) midazolam, fentanyl, and propofol. Dosing should be titrated according to clinical parameters, including arterial blood pressure, minute ventilation, and arterial oxygen saturation. Sedative-induced hypotension is a frequent problem in patients with depressed ventricular function or decreased systemic vascular resistance, and occasionally patients may require transient support with IV volume infusion or vasopressor agent. If the patient is extremely uncooperative and biting, increased sedation, transient paralysis, and mechanical ventilation may be required to perform TEE safely.
Most ICU patients are monitored continuously for key respiratory, cardiac, or hemodynamic parameters. At a minimum, it is essential that patients undergoing an ultrasound examination in the ICU be monitored with noninvasive recording of blood pressure, pulse oximetry, and electrocardiogram. Even TTE or abdominal ultrasound examinations can be associated with inadvertent pulling of tubes or drains, and anxiety can be encountered during the procedure. Because of its more invasive nature, insertion of the TEE probe may induce discomfort and complications such as increased agitation and respiratory distress. These effects can be associated with substantial changes in blood pressure and ventilatory status. Administration of sedatives and sometimes paralytic agents can further alter hemodynamic and respiratory status. ,
Performance of ultrasound examinations in the ICU provides data that previously required transport to the radiology suite. This is an important advantage for the critically ill patient, because transport out of and back to the ICU is known to be associated with an increased risk of complications. Performance of bedside TTE ultrasound and of other noninvasive ultrasound examinations is safe and not associated with significant risks to the patient. Performance of the semiinvasive bedside TEE also is associated with a low incidence of serious complications (<0.5% in the general population and the elderly). The reported mortality rate associated with TEE is 0.01%–0.03%. Most patients undergoing TEE examinations in the ICU are receiving mechanical ventilation and have continuous monitoring of arterial blood pressure, electrocardiogram, and oxygen saturation. Transient hypotension, typically attributable to administration of sedative medications, usually can be treated with vasopressors or IV fluids or both. The risk of injury to the pharynx or esophagus is greater in anesthetized and endotracheally intubated critically ill patients than in awake patients, because anesthetized patients cannot assist with probe insertion by swallowing and do not resist when insertion proves difficult. Increased difficulty in directing the TEE probe also can be encountered in the presence of a nasogastric tube. Coagulopathy and thrombocytopenia, common problems in critically ill patients, can increase the risk of hemorrhage resulting from mucosal injury during blind insertion of the TEE probe. Daniel and colleagues reported significant complications related to TEE in 18 (0.18%) of 10,218 examinations. In 11 studies reporting on 943 patients undergoing TEE, the rate of complications was 1.7%. Serious complications occurred in only two patients (0.2%). Colreavy and colleagues studied the safety and utility of TEE performed by ICU physicians in 255 critically ill patients and reported that TEE was associated with a complication rate of only 1.6%. It is reasonable to conclude that bedside TEE is associated with few complications, given the high severity of illness. Close monitoring of hemodynamic and oxygenation parameters is essential. Box E2.4 lists specific contraindications to the insertion of a TEE probe.
Esophageal pathologies
Stricture
Mass or tumor
Diverticulum
Mallory-Weiss tear
Dysphagia or odynophagia not previously evaluated
Cervical spine instability
Esophageal varices
Recent esophageal or gastric surgery
Oropharyngeal carcinoma
Upper gastrointestinal bleeding
Severe cervical arthritis
Atlantoaxial disease
Echocardiography can provide diagnostic information noninvasively regarding cardiac structure and mechanical function. The supplementary information provided by this technique can help determine the cause of hypotension refractory to inotropic support or vasopressor infusions. It also can help in the diagnosis of a wide spectrum of other cardiovascular abnormalities (e.g., endocarditis) and guide therapeutic management. An adequate understanding of the proper use of echocardiography is a prerequisite for the intensivist. General indications for performance of an echocardiographic examination in the ICU are listed in Box E2.1 .
Accurate and prompt diagnosis is crucial in the ICU. The easiest and least invasive way to image cardiac structures is TTE. This noninvasive imaging modality is of great value in the critical care setting because of its portability, widespread availability, and rapid diagnostic capability. In the ICU, TTE may sometimes fail to provide adequate image quality because of factors that potentially can hinder the quality of the ultrasound signal, as described previously. The failure rate (partial or complete) of TTE in the ICU has been reported to be 30%–40%. , Nonetheless, improvements have been made in transthoracic imaging (e.g., harmonics and contrast and digital technologies), resulting in a progressively lower failure rate of TTE in the ICU (currently 10%–5% in our institution).
TEE is particularly useful for evaluation of suspected aortic dissection, prosthetic heart valves (especially in the mitral position), detecting cardiac emboli, valvular vegetations, possible intracardiac shunts, wall motion abnormalities, and unexplained hypotension. TEE allows better visualization of the heart than TTE, especially of the posterior structures, owing to the proximity of the probe and favorable acoustic transmission. Despite its limitations, TTE may provide complementary information. For example several areas of the heart and great vessels are difficult to visualize by TEE. The view of the left ventricular apex often is foreshortened with TEE, and an apical left ventricular clot can be missed. TTE usually is superior for visualization of the apex. Because of interposition of the left mainstem bronchus, the superior portion of the ascending aorta is another important area that may not be well visualized with TEE. The transducer position and angulation of TEE are constrained by the relative positions of the esophagus and heart. The relatively fixed relationship between the position of the probe and the heart often makes it impossible to align the Doppler beam parallel to the flow of interest (e.g., to evaluate the jet of blood resulting from aortic stenosis). In addition, the 2D imaging planes of TEE often make standard anatomic measurements more difficult to obtain.
As a result of the significantly improved technical quality of TTE, most ICU patients can be studied satisfactorily with this modality alone. Immediate TEE is still preferable, however, in certain specific clinical situations in which TTE is likely to fail or prove suboptimal. The major indications for primary TEE in the ICU , are listed in Box E2.2 . Even when TEE is necessary, data from the TTE examination are often essential for the final clinical interpretation.
Evaluation of left ventricular performance by echocardiography is often paramount in the ICU. Accurate and timely assessment of systolic function should be an integral part of the medical management of hemodynamically unstable critically ill patients. Global assessment of left ventricular contractility includes the determination of ejection fraction (EF), circumferential fiber shortening, and cardiac output.
The simplest quantitative approach is to measure the mid–left ventricular short-axis dimension at end diastole and end systole to determine the percentage of fractional shortening. Fractional shortening is related directly to EF; normal fractional shortening is 30%–42%.
In the setting of regional wall motion abnormalities, fractional shortening may underestimate or overestimate global ventricular function and must be interpreted in light of what is seen in all of the 2D imaging planes of the ventricle.
Global systolic ventricular function also can be assessed quantitatively by fractional area change (normal value is 36%–64%) and by EF (normal value is 55%–75%) ( Fig. E2.1 ):
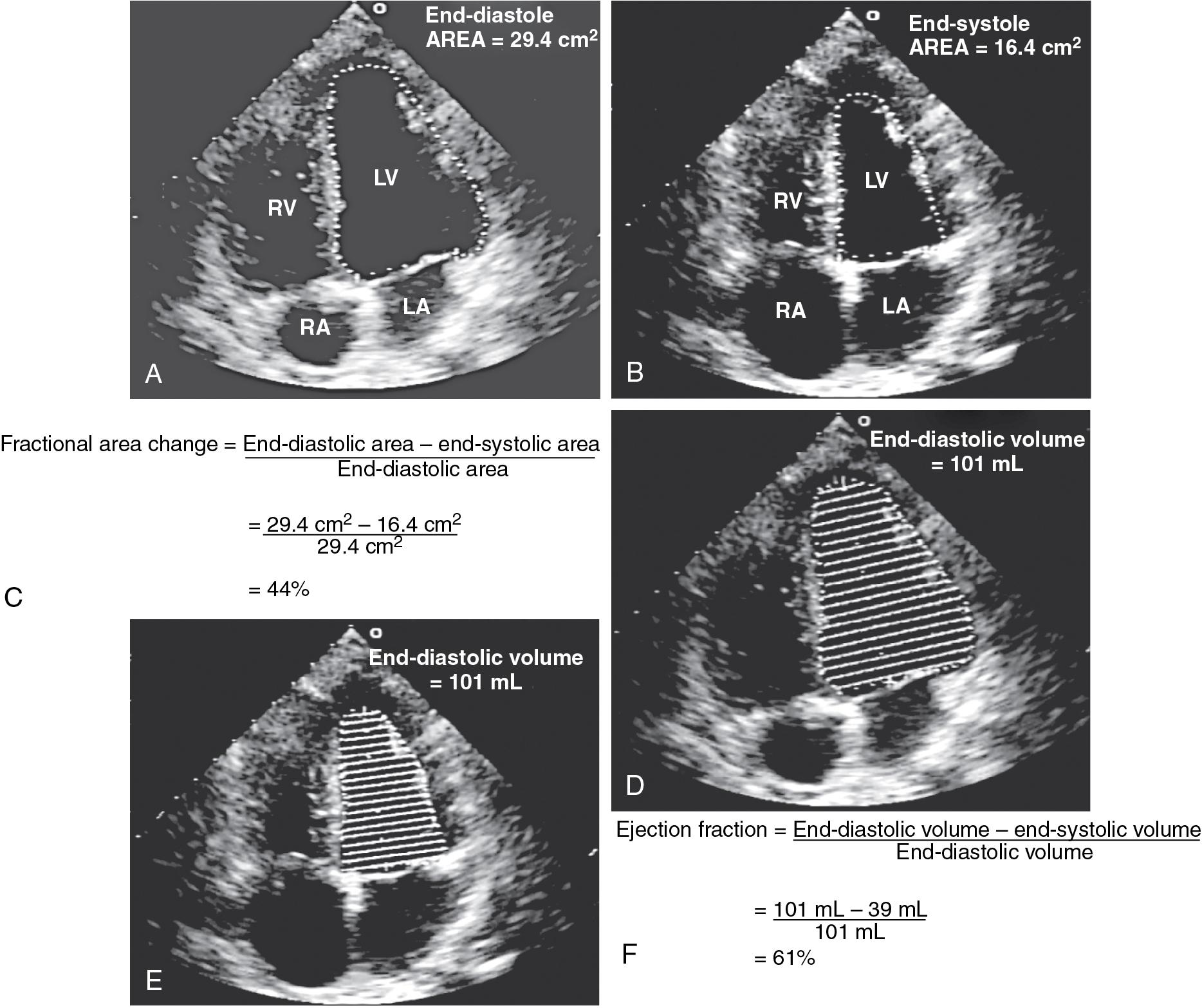
These measurements require good image quality, because endocardial border contours must be traced (see Fig. E2.1 ). Machine-integrated software uses the data to determine volumes, areas, and the resultant EF (see Fig. E2.1 ). In patients with regional wall motion abnormalities, more precise measures of stroke volume can be made by approximating ventricular volumes as a stack of elliptical disks on biplane imaging (modified Simpson method). ,
In the critical care setting, defining the endocardial border may be suboptimal because of poor image quality. , , In these cases, global ventricular function often is assessed qualitatively by visual inspection alone. This method has been found to be reliable when used by experienced clinicians. By simple visualization of the kinetics and size of the cardiac cavities in real time, an experienced intensivist with a sufficient echocardiographic background can establish a functional diagnosis immediately.
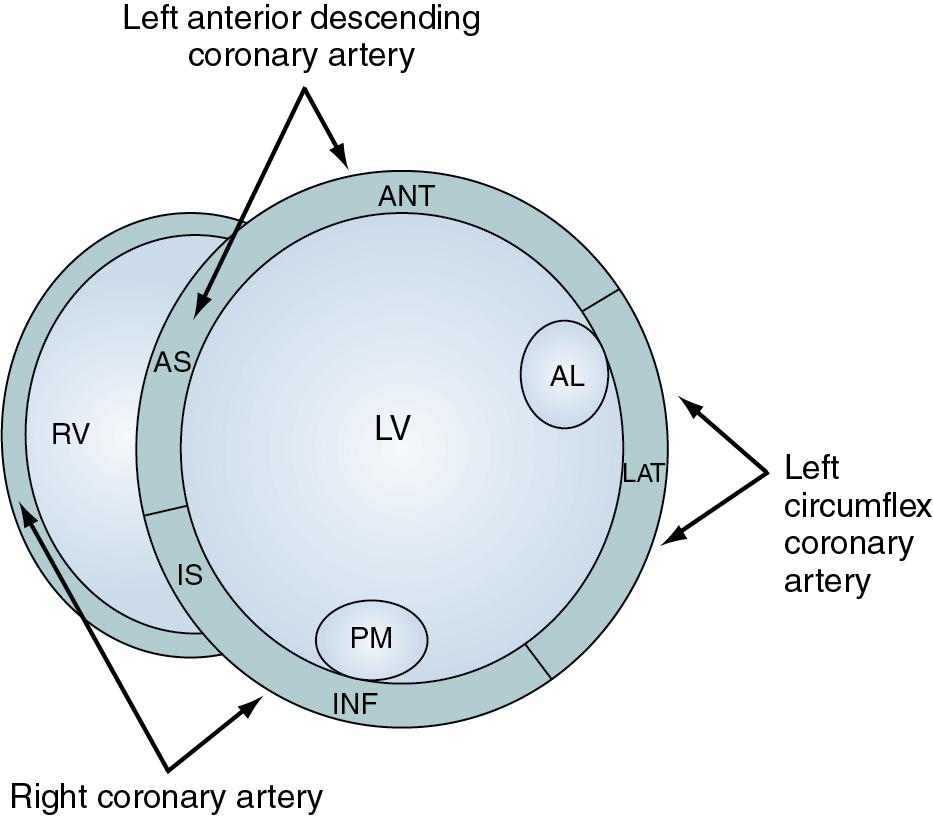
Analysis of regional wall motion includes a numeric scoring system to describe the movement of the different regions of the left and right ventricles (1 = normokinesia; 2 = hypokinesia; 3 = akinesia; 4 = dyskinesia; 5 = aneurysmal change). Visualized from the short-axis view of the left ventricle, a complete overview of myocardial areas perfused by the three major coronary arteries can be obtained ( Fig. E2.2 ). If the TTE examination is technically difficult and the endocardium is poorly visualized, harmonic imaging and possibly contrast, if needed, can dramatically improve endocardial border visualization and subsequent evaluation of global systolic function (as discussed further later in this chapter). For the remaining few technically challenging cases with suboptimal TTE, performance of TEE allows for more precise evaluation of ventricular function in most critically ill patients because of the higher image quality that can be obtained with this echographic modality.
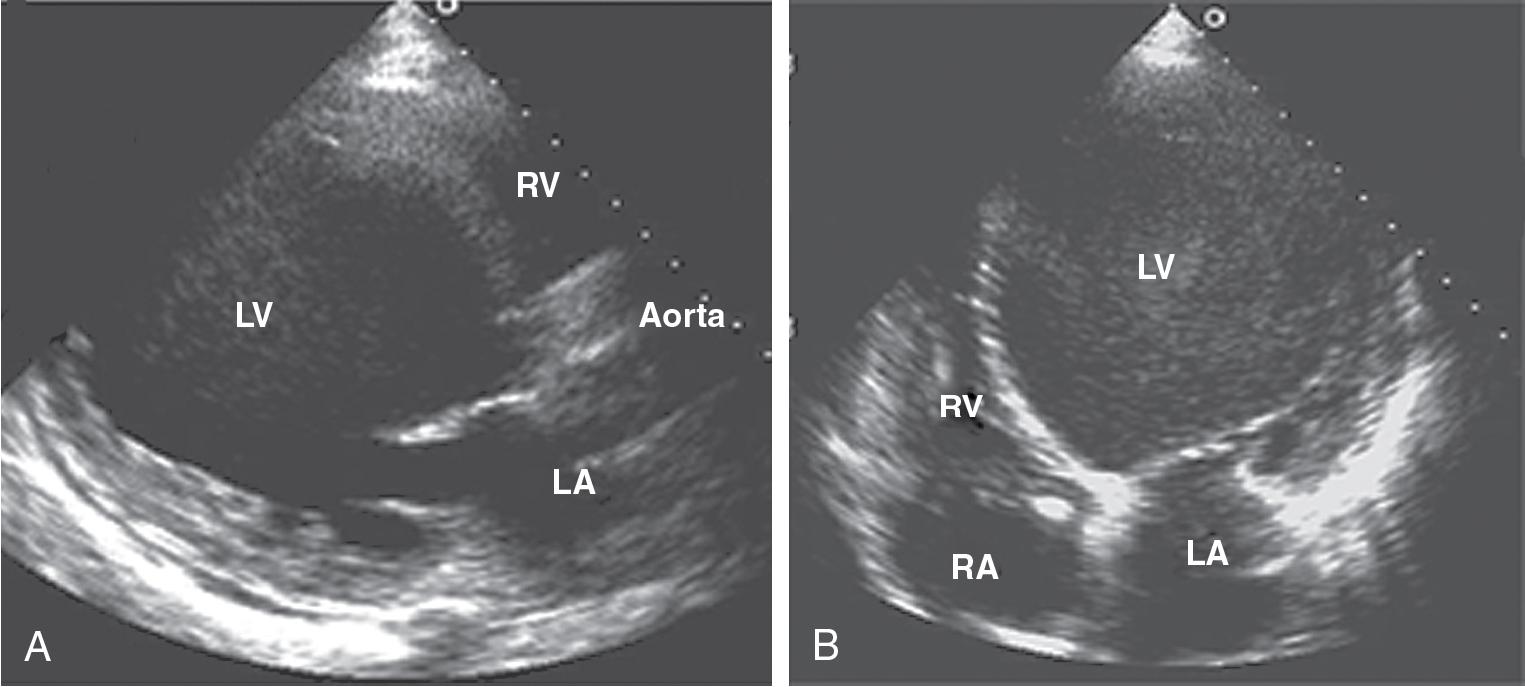
In a critically ill patient with unexplained hemodynamic instability, determination of cardiac function is an integral part of the medical management. Echocardiography is valuable in this setting because the clinical examination and invasive hemodynamic monitoring often fail to provide an adequate assessment of ventricular function. In a study by Fontes and colleagues that compared pulmonary artery (Swan-Ganz) catheterization with TEE, the overall predictive probability for conventional clinical and hemodynamic assessment of normal ventricular function was 98%, whereas for abnormal ventricular function (EF <40%), it was 0%. Several other studies have reported similar results. Assessment of biventricular function is one of the most important indications for echocardiography in the ICU. In a study by Bruch and colleagues, 115 critically ill patients were studied by TEE. The most common indication for TEE was hemodynamic instability (67% of patients). Of these hemodynamically unstable patients, 20 (26%) were found to have significant left ventricular dysfunction (EF <30%). In a study by McLean , the most common reason to request a TEE in the ICU was to assess left ventricular functioning. In most patients, left ventricular function was assessed adequately by TTE before TEE. In a study by Vignon and colleagues, TTE allowed adequate evaluation of global left ventricular function in 77% of mechanically ventilated ICU patients. Although TEE was needed for most other indications, TTE was shown to be an excellent diagnostic tool for assessment of left ventricular function in the ICU ( Fig. E2.3 ), even in the presence of positive end-expiratory pressure.
Several important points should be emphasized: (1) significant left ventricular dysfunction occurs commonly in critically ill patients; (2) ventricular function should be assessed in all patients with unexplained hemodynamic instability because this information is particularly important for guiding resuscitation and informing decisions regarding subsequent medical or surgical management; (3) it is now possible to obtain adequate information about ventricular function in most ICU patients using TTE, but TEE improves accuracy in patients with suboptimal imaging by TTE.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here