Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The primary cutaneous B-cell lymphomas share some histologic features with their nodal counterparts, but in many cases represent distinct clinicopathologic entities with significant clinical, immunophenotypic, molecular, and prognostic differences from their extracutaneous counterparts. In general, primary cutaneous B-cell lymphomas have a better prognosis than their nodal-based counterparts, and treatment strategies for them may be different. The classification system used in this chapter reflects the 2016 revision of the 2008 World Health Organization (WHO) classification of lymphoid neoplasms. Note that not all entities included here are necessarily of primary cutaneous origin (e.g., chronic lymphocytic leukemia/small lymphocytic lymphoma, mantle cell lymphoma, Burkitt lymphoma, intravascular large B-cell lymphoma, lymphomatoid granulomatosis) but may frequently involve the skin.
Germinal center >90% MIB-positive
Follicle center cells express BCL-6 and CD10
CD21 and CD23 demonstrate a well-defined dendritic network within the germinal center
Mantle zone of small lymphocytes that normally express BCL-2
Kappa:lambda ratio 2:1
Marginal zone is inconspicuous

Patchy, nodular, or diffuse infiltrate of lymphoid cells in the dermis and superficial panniculus
Characteristic “inverse” pattern of central darker, benign reactive lymphocytes with surrounding neoplastic cells with paler abundant cytoplasm (marginal zone cells)
Lack of epidermotropism
Small lymphocytes may surround or invade eccrine coils
Surrounding benign reactive follicles may be colonized by neoplastic cells
Neoplastic marginal zone cells often comprise only a minority of lymphoid cells in the lesions
CD20+, CD79+, CD5−, CD10−, CD43−, BCL-6−, and BCL-2+
Clonal rearrangement of immunoglobulin (Ig) H gene in >70% of cases
t(14;18)(q32;q21) present in a minority of cases
Intracytoplasmic monoclonal immunoglobulin (kappa or lambda) restriction
Primary cutaneous marginal zone B-cell lymphoma is an indolent lymphoma of small lymphocytes of B-cell origin, including centrocyte (marginal zone)-like cells with small- to medium-sized slightly irregular nuclei with inconspicuous nucleoli, admixed with plasmacytoid lymphocytes and occasional centroblast-like cells. Marginal zone lymphoma is one of the most common types of cutaneous B-cell lymphoma. The prognosis is excellent, with 5-year survival rates approaching 100%. The lesions usually present as violaceous nodules or plaques preferentially on the trunk and extremities, with upper extremities more commonly involved than lower extremities. The lesions have a nodular or diffuse architecture, often with a characteristic “inverse” pattern relative to benign reactive lymphoid follicles, i.e., they show a dense, darker-staining central nodular portion of benign reactive lymphocytes, which may contain germinal centers, surrounded by neoplastic lymphoid cells with slightly irregular nuclei and more abundant paler cytoplasm (monocytoid or marginal zone B cells). Often, the neoplastic lymphoid population only represents a minority of the cells in the lesion. The epidermis is spared, without epidermotropism of lymphocytes. Surrounding benign reactive germinal centers may be present, and are often colonized by tumor cells. In some cases, the neoplastic cells may surround and infiltrate eccrine coils, similar to the lymphoepithelial lesions seen in extranodal marginal zone lymphomas of the gastrointestinal tract (MALTomas). Primary cutaneous marginal zone B-cell lymphoma includes cases designated as primary cutaneous immunocytoma in earlier classification systems. Primary cutaneous immunocytomas are often associated with Borrelia and demonstrate high numbers of monotypic (i.e., they demonstrate monoclonal intracytoplasmic immunoglobulin) plasma cells and lymphoplasmacytoid lymphocytes, some of which may contain intranuclear immunoglobulin deposits (Dutcher bodies).

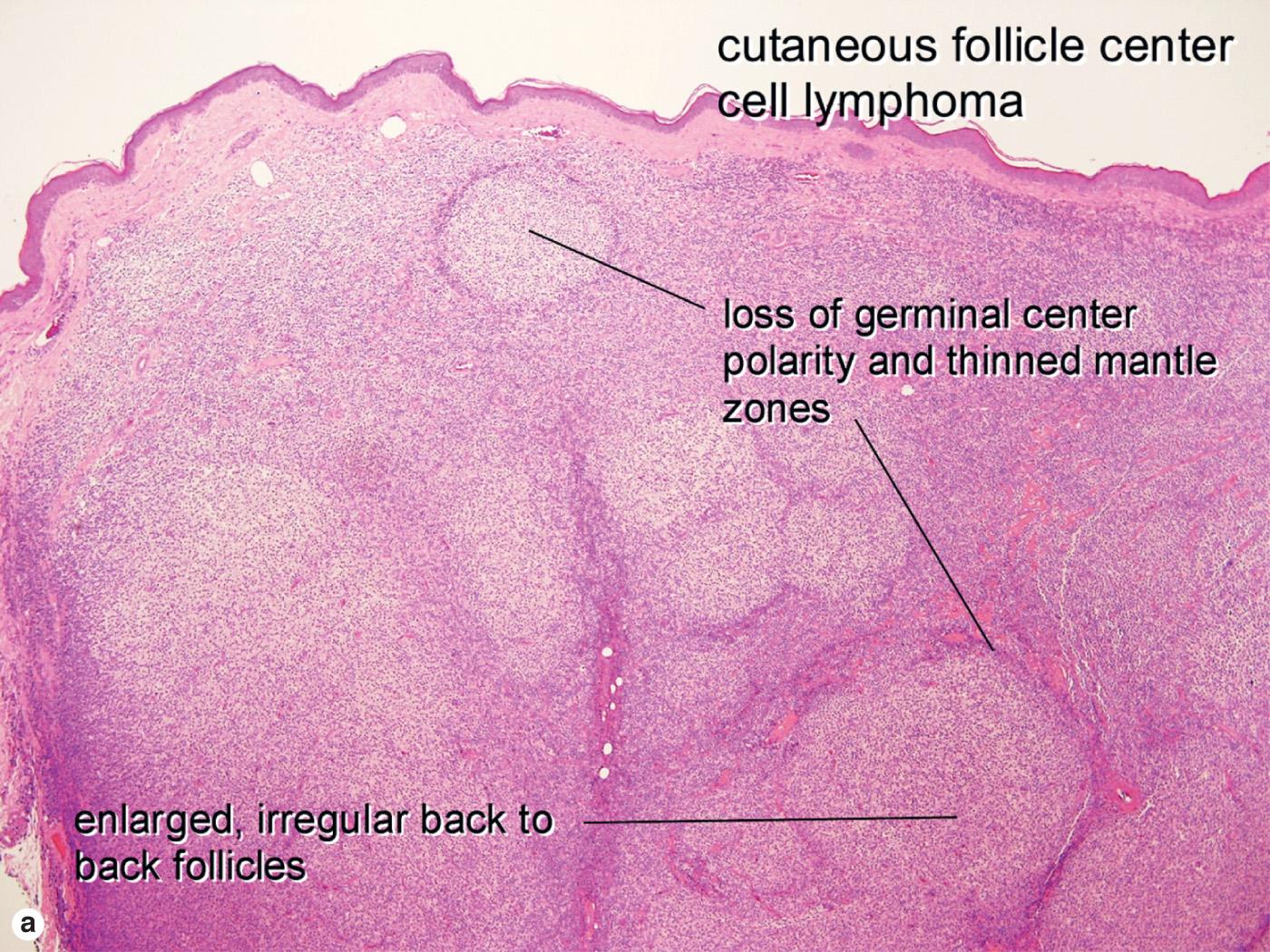
Diffuse, nodular and diffuse, or nodular lymphoid proliferation
If mixed architecture, lesions tend to have neoplastic follicles at the periphery of a central diffuse neoplastic infiltrate
Follicles have reduced or absent mantle zones
Follicles have decreased to absent tingible body macrophages
Lack of polarity of follicles (i.e., absent light and darker zones of polarity in follicle germinal centers)
CD20+ and CD79+
CD10+ (follicular pattern, most cases) or CD10− (diffuse pattern, most cases)
BCL-6+, BCL-2−, CD5−, CD43−, most cases are FOXP1− and IgM−
Reduced proliferative fraction by MIB-1 compared with benign reactive germinal centers
Monoclonal rearrangement of immunoglobulin heavy chain J gene
t(14;18) translocation is very uncommon in primary cutaneous follicle center cell lymphoma lesions
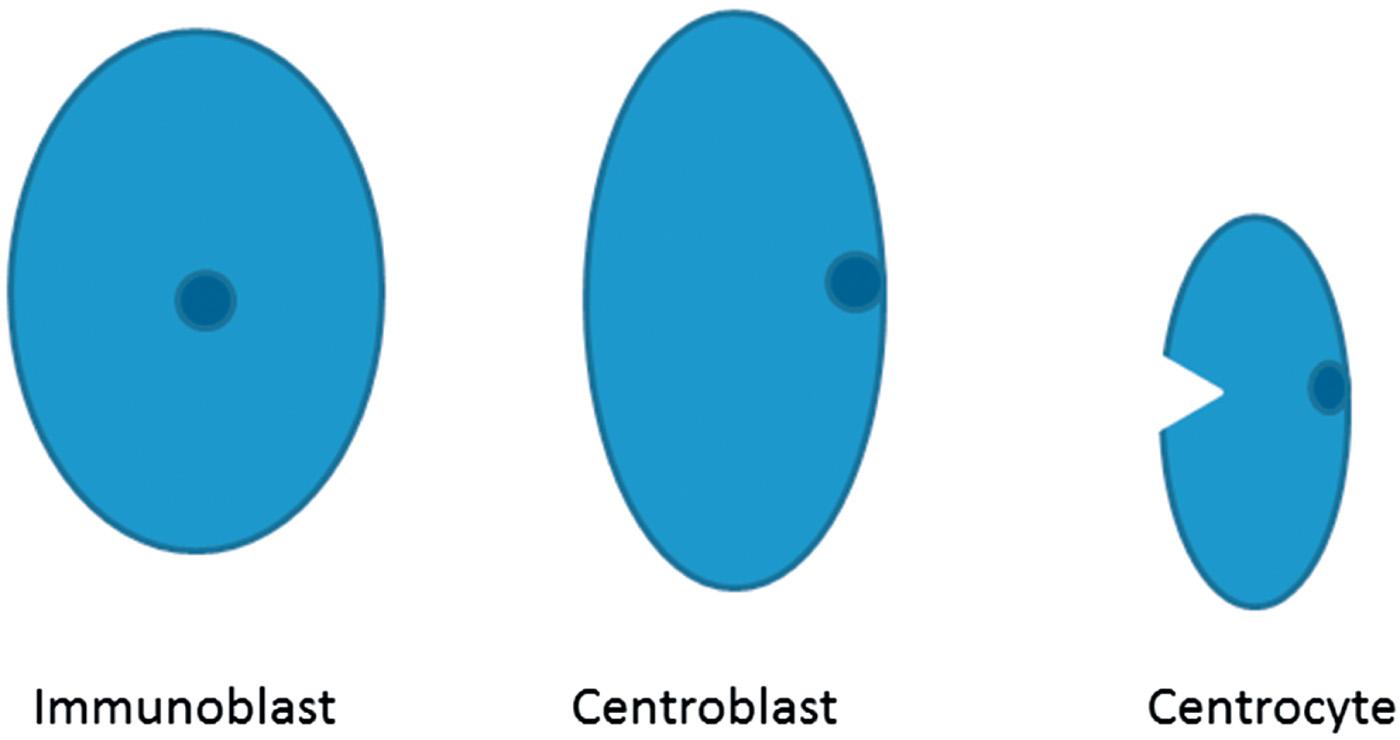
Primary cutaneous follicle center cell lymphoma is also an indolent mature B-cell lymphoma that exhibits a predilection for the head and trunk. In contrast to its nodal counterpart (primary nodal follicle center cell lymphoma), primary cutaneous follicle center cell lymphoma has a more favorable prognosis, with 5-year survival rates >90%. As with their nodal counterparts, these lesions may have a follicular, follicular and diffuse, or diffuse architecture, most commonly diffuse. However, it must be emphasized again that, despite similar appearances by hematoxylin and eosin, these lesions have different immunohistochemical, genetic, and prognostic features from primary nodal follicle center cell lymphomas. Histology shows a nodular or diffuse proliferation of centrocyte-like lymphocytes with small, slightly irregular nuclei and variable numbers of larger centroblast-like cells with larger, rounded vesicular nuclei and one or a few prominent nucleoli. In nodular lesions, the follicles appear monomorphous, with a loss of the normal polarity of light and dark zones of the germinal centers, an attenuated mantle zone around germinal centers, and lack of tingible body macrophages in the germinal centers. In larger lesions, the center may show a diffuse architecture, with residual monomorphous neoplastic follicles at the periphery. Unlike primary nodal follicle center cell lymphoma, primary cutaneous follicle center cell lymphoma is not graded at the current time.
In primary cutaneous follicle center cell lymphoma, the BCL-6–positive cells typically stray outside of the follicle. BCL-2 expression is characteristic of follicle center cell lymphoma in lymph nodes, but is rare in the primary cutaneous variety. At cutaneous sites, BCL-2 positivity in a follicle center cell lymphoma should raise suspicion for a nodal primary with secondary involvement of the skin.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here