Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
After assessment of insertional and spontaneous activity, the needle electromyography (EMG) examination moves on to the evaluation of motor unit action potentials (MUAPs). In a process similar to the analysis of spontaneous activity, MUAPs must be assessed for morphology (duration, amplitude, phases), stability, and firing characteristics. The pattern of MUAP abnormalities that emerges from this part of the examination usually will allow a determination of whether a disorder is primarily neuropathic or myopathic and often helps determine the time course (acute vs. chronic) and severity of the lesion. The assessment of MUAPs often is demanding and improves with the experience of the electromyographer over time. The task of evaluating MUAPs is made all the more difficult by the wide variation in what is considered a normal MUAP, depending on the muscle being studied and the age of the patient.
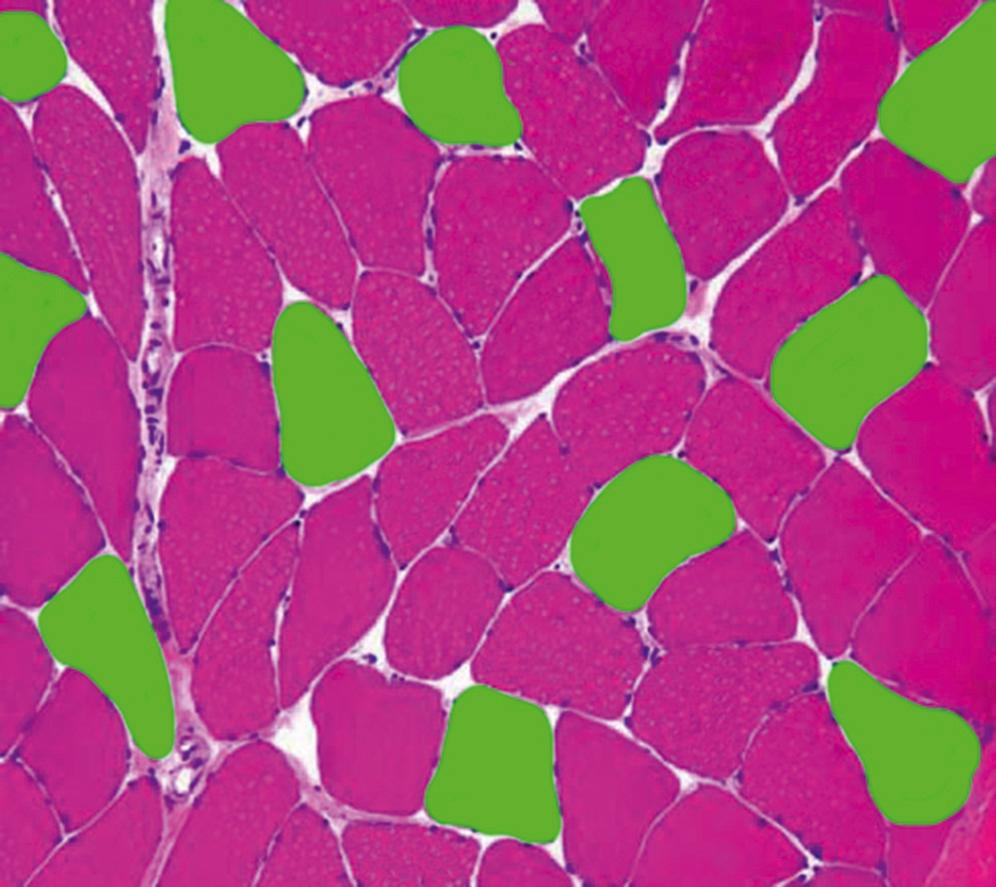
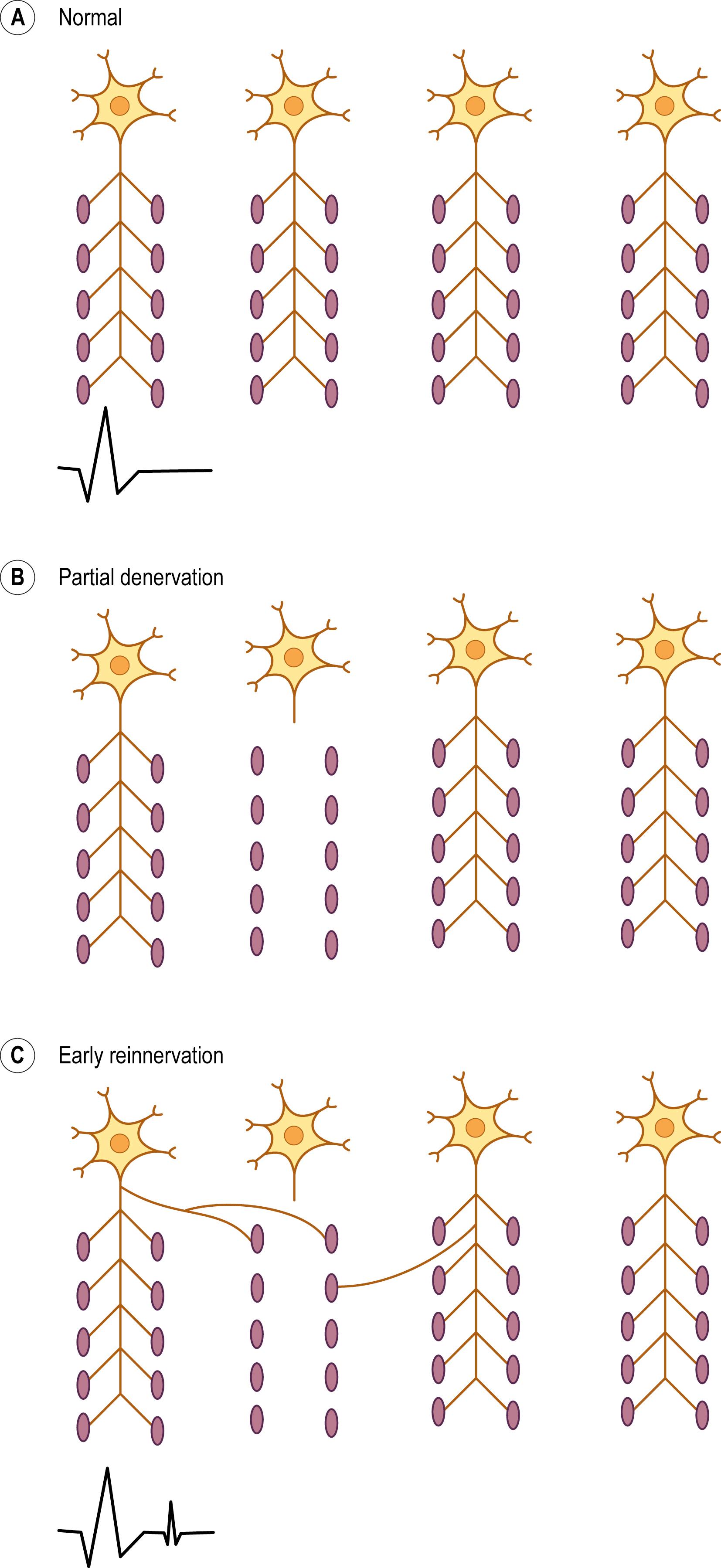
The basic component of the peripheral nervous system is the motor unit, defined as an individual motor neuron, its axon, and associated neuromuscular junctions (NMJs) and muscle fibers. The extracellular needle EMG recording of a motor unit is the MUAP ( Fig. 15.1 ). The number of muscle fibers per motor unit varies greatly, from 5 to 10 in laryngeal muscles to a couple of thousand in the soleus. Transverse motor unit territory increases greatly with age, doubling from birth to adulthood, mostly because of the increase in individual muscle fiber size. The transverse territory of a motor unit in adults usually ranges from 5 to 10 mm. Many motor unit territories overlap with one another. Because of this overlap, two muscle fibers from the same motor unit rarely lie adjacent to each other ( Fig. 15.2 ). Indeed, it is common that muscles fibers from five to six motor units intermix with each other, creating a so-called “mosaic pattern.” This innervation pattern results in more evenly distributed force during contraction.
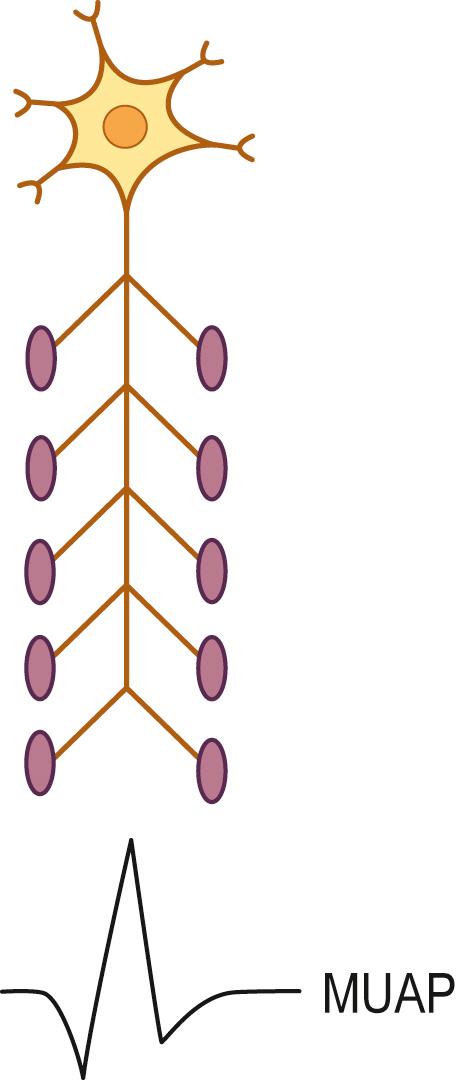
When a motor neuron depolarizes to threshold, a nerve action potential is generated and propagates down the axon. Under normal circumstances, this results in all muscle fibers of the motor unit being activated and depolarizing more or less simultaneously. Any variability between muscle fiber depolarization times is due to differences in the length of the terminal axons and in NMJ transmission times.
The “size principle” governs many of the properties of motor units ( Fig. 15.3 ). The size of the motor neuron is directly related to (1) the size of the axon, (2) the thickness of the myelin sheath, (3) the conduction velocity of the axon, (4) the threshold to depolarization, and (5) the metabolic type of muscle fibers that are innervated. The larger motor neurons have larger axons, with the thickest myelin sheath (hence, the fastest conduction velocity), highest threshold to depolarization, and connections to type II, fast twitch muscle fibers. Conversely, the smaller motor neurons have smaller axons, less myelin sheath, slower conduction velocity, lower threshold to depolarization, and, in general, connections to type I, slow twitch muscle fibers. Thus, with voluntary contraction, the smallest motor units with the lower thresholds fire first. As contraction increases, progressively larger motor units begin to fire. The largest type II motor units fire with maximum contraction. During routine needle EMG, most MUAPs analyzed are thus from the smaller motor units that innervate type I muscle fibers.

During the needle EMG examination, each MUAP recorded represents the extracellular compound potential of the muscle fibers of a motor unit, weighted heavily toward the fibers nearest to the needle. An MUAP recorded just outside a muscle membrane is 1/10–1/100 the amplitude of the actual transmembrane potential and the amplitude decreases rapidly as the distance between the needle and the membrane increases. The classification of an MUAP as normal, neuropathic, or myopathic rests on no single finding. As is true of spontaneous activity, recorded MUAPs must be assessed for morphology (duration, polyphasia, amplitude), stability, and firing characteristics before any conclusions can be reached.
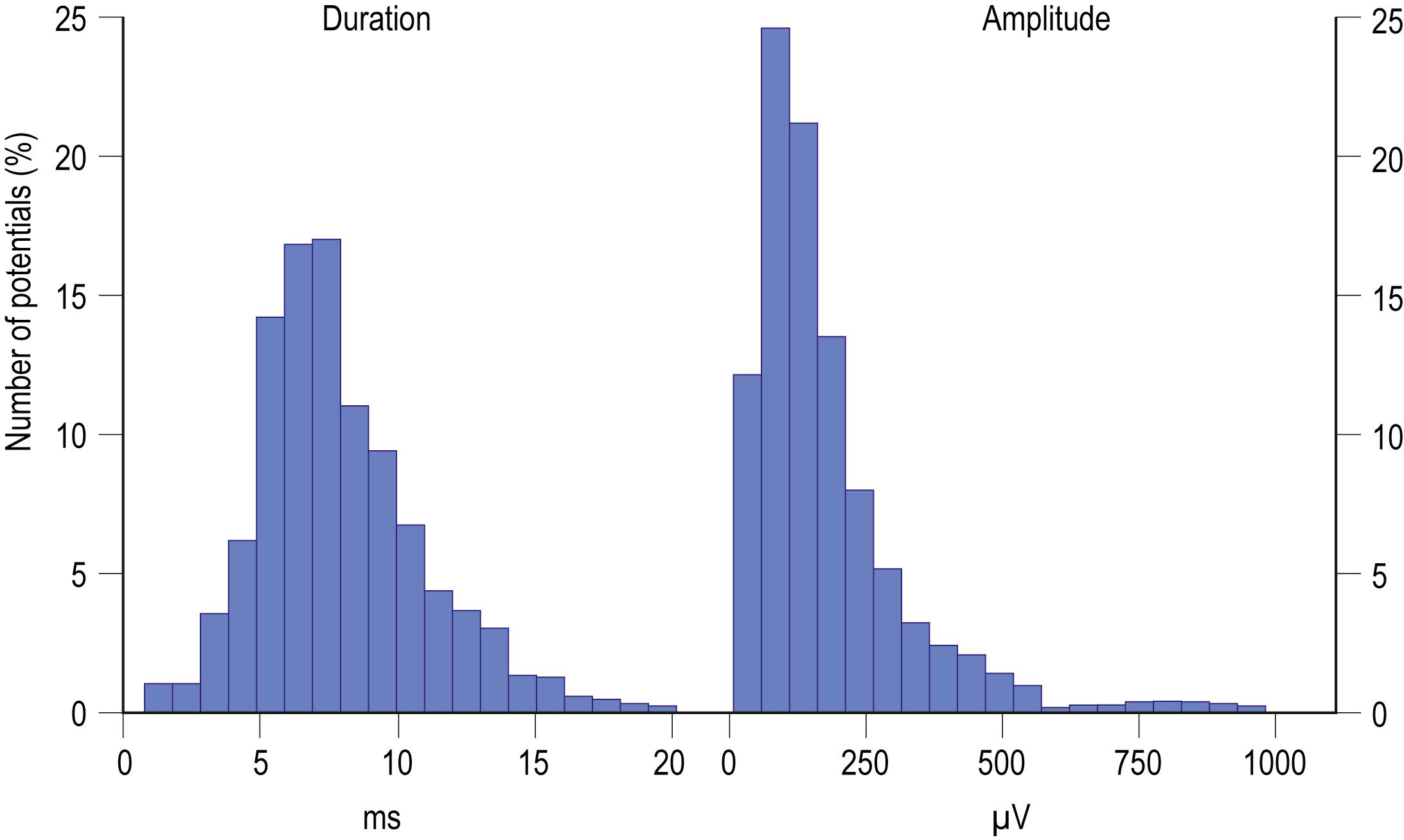
MUAP properties vary widely both within and between different muscles. Even within a muscle, there is a wide range of normal motor unit morphology, with MUAP size following a bell-shaped distribution curve ( Fig. 15.4 ). Due to this normal variability, normal values of MUAP morphology are based on the mean of many different MUAPs. The analysis of MUAP morphology can be performed on either a qualitative or a quantitative basis. To perform quantitative MUAP analysis, one must isolate 20 different MUAPs for each muscle being studied and measure their individual durations, amplitudes, and number of phases. From these values, the mean duration, amplitude, and number of phases are calculated and compared with a set of normal values for that particular muscle and age group. MUAP morphology varies depending on the muscle being studied and the patient’s age. This is particularly true of MUAP duration ( Table 15.1 ). In general, MUAPs in proximal muscles tend to be shorter in duration than those in more distal muscles. MUAP size in adults is larger than in children, primarily because of an increase in the size of muscle fibers during development. In addition, MUAP size is generally larger in older individuals, probably as the result of dropout of motor units from the normal effects of aging, leading to some compensatory “normal” reinnervation. The loss of motor units has been estimated to be approximately 1% per year, beginning in the third decade of life, which then increases rapidly after age 60.
| Age of Subjects | Arm Muscles | Leg Muscles | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Deltoid | Biceps | Triceps | Thenar | ADM | Quad, BF | Gastroc | Tib Ant | Per Long | EDB | Facial | |
| 0–4 | 7.9–10.1 | 6.4–8.2 | 7.2–9.3 | 7.1–9.1 | 8.3–10.6 | 7.2–9.2 | 6.4–8.2 | 8.0–10.2 | 6.8–7.4 | 6.3–8.1 | 3.7–4.7 |
| 5–9 | 8.0–10.8 | 6.5–8.8 | 7.3–9.9 | 7.2–9.8 | 8.4–11.4 | 7.3–9.9 | 6.5–8.8 | 8.1–11.0 | 5.9–7.9 | 6.4–8.7 | 3.8–5.1 |
| 10–14 | 8.1–11.2 | 6.6–9.1 | 7.5–10.3 | 7.3–10.1 | 8.5–11.7 | 7.4–10.2 | 6.6–9.1 | 8.2–11.3 | 5.9–8.2 | 6.5–9.0 | 3.9–5.3 |
| 15–19 | 8.6–12.2 | 7.0–9.9 | 7.9–11.2 | 7.8–11.0 | 9.0–12.8 | 7.8–11.1 | 7.0–9.9 | 8.7–12.3 | 6.3–8.9 | 6.9–9.8 | 4.1–5.7 |
| 20–29 | 9.5–13.2 | 7.7–10.7 | 8.7–12.1 | 8.5–11.9 | 9.9–13.8 | 8.6–12.0 | 7.7–10.7 | 9.6–13.3 | 6.9–9.6 | 7.6–10.6 | 4.4–6.2 |
| 30–39 | 11.1–14.9 | 9.0–12.1 | 10.2–13.7 | 10.0–13.4 | 11.6–15.6 | 10.1–13.5 | 9.0–12.1 | 11.2–15.1 | 8.1–10.9 | 8.9–12.0 | 5.2–7.1 |
| 40–49 | 11.8–15.7 | 9.6–12.8 | 10.9–14.5 | 10.7–14.2 | 12.4–16.5 | 10.7–14.3 | 9.6–12.8 | 11.9–15.9 | 8.6–11.5 | 9.5–12.7 | 5.6–7.4 |
| 50–59 | 12.8–16.7 | 10.4–13.6 | 11.8–15.4 | 11.5–15.1 | 13.4–17.5 | 11.6–15.2 | 10.4–13.6 | 12.9–16.9 | 9.4–12.2 | 10.3–13.5 | 6.0–7.9 |
| 60–69 | 13.3–17.3 | 10.8–14.1 | 12.2–15.9 | 12.0–15.7 | 13.9–18.2 | 12.1–15.8 | 10.8–14.1 | 13.4–17.5 | 9.7–12.7 | 10.7–14.0 | 6.3–8.2 |
| 70–79 | 13.7–17.7 | 11.1–14.4 | 12.5–16.3 | 12.3–16.0 | 14.3–18.6 | 12.4–16.1 | 11.1–14.4 | 13.8–17.9 | 10.0–13.0 | 11.0–14.3 | 6.5–8.3 |
Only by comparing mean MUAP morphology in each muscle studied to normal values for that particular muscle and age group can one determine whether the morphology is truly abnormal. Previously, quantitative MUAP analysis was tedious and time-consuming. However, many modern EMG machines now have programs that largely automate the process. With experience over time, however, the well-trained electromyographer usually can perform qualitative MUAP assessment with the same precision as can be achieved using quantitative methods. Essentially the same procedure is used. The needle is moved to several locations within the muscle until approximately 20 different MUAPs have been examined, qualitatively analyzed, and compared to the expected normal values for that particular muscle and age group.
MUAP duration is the parameter that best reflects the number of muscle fibers within a motor unit ( Fig. 15.5 ). Typical MUAP duration is between 5 and 15ms. Duration is defined as the time from the initial deflection from baseline to the final return of the MUAP to baseline. It depends primarily on the number of muscle fibers within the motor unit and the dispersion of their depolarizations over time. Dispersion in turn depends on the longitudinal and transverse scatter of endplates and on variations in terminal distances and conduction velocities. Duration lengthens as the number of fibers and the territory of a motor unit increase; it varies directly with age (increased age, increased duration) and inversely with temperature (decreased temperature, increased duration) and depends on the individual muscle being studied. Proximal and bulbofacial muscles in general have MUAPs of shorter duration. When performing EMG, it often is more rewarding to listen to the potential than to see it. This is especially true when evaluating MUAP duration, because duration correlates with pitch . Long-duration MUAPs (low frequencies) sound dull and thuddy, whereas short-duration MUAPs (higher frequencies) sound crisp and static-like [Video 15.1]. As the electromyographer gains experience, the sound of a long-duration versus a short-duration MUAP becomes unmistakable.
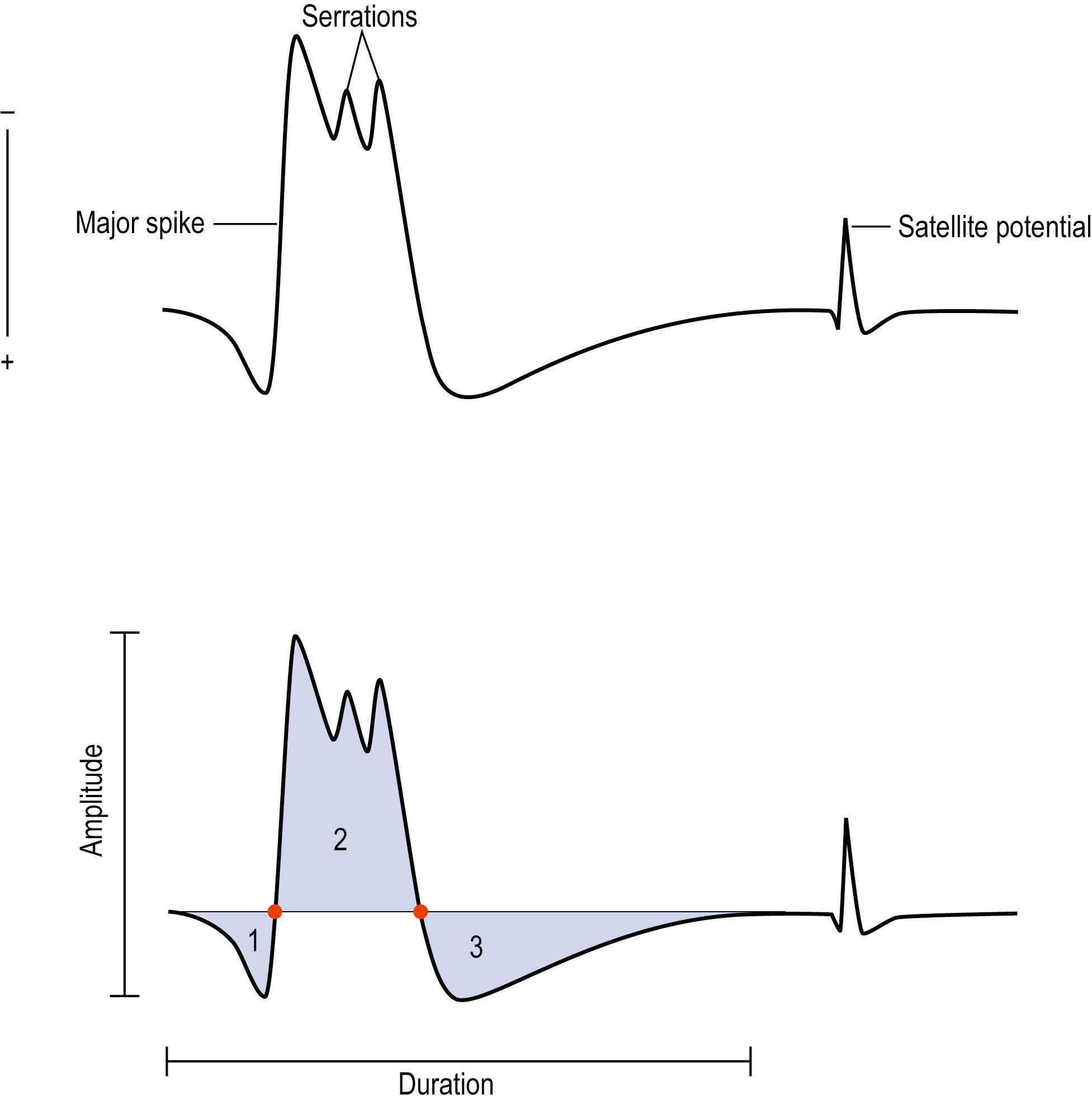
Polyphasia is a measure of synchrony, that is, the extent to which the muscle fibers within a motor unit fire more or less at the same time. This is a nonspecific measure and may be abnormal in both myopathic and neuropathic disorders. The number of phases can be easily calculated by counting the number of baseline crossings of the MUAP and adding one ( Fig. 15.5 ). Normally, MUAPs have two to four phases. However, increased polyphasia may be seen in up to 5%–10% of the MUAPs in any muscle and is considered normal. The one exception is the deltoid, where up to 25% polyphasia may be normal. Increased polyphasia beyond 10% in most muscles and 25% in the deltoid is always abnormal. Through the speaker, polyphasic MUAPs are recognized as a high-frequency “clicking” sound [Video 15.2].
Serrations (also called turns) are defined as changes in the direction of the potential that do not cross the baseline. Increased polyphasia and serrations have similar implications, indicating less synchronous firing of muscle fibers within a motor unit. Often, a serration can be changed into an additional phase with needle movement.
Satellite potentials (also known as linked potentials or parasite potentials ) are interesting phenomena seen in early reinnervation. After denervation, muscle fibers often are reinnervated by collateral sprouts from adjacent intact motor units. The newly formed sprout often is small, unmyelinated or thinly myelinated, and therefore very slowly conducting. Because of the slow conduction time and increased distance, reinnervated muscle fibers are time-locked potentials that trail the main MUAP ( Figs. 15.6 and 15.7 ) [Video 15.3]. These satellite potentials are extremely unstable (see section on Stability) and may vary slightly in their firing rate or may block and not fire at all ( Fig. 15.8 ) [Video 15.4] [Video 15.5] [Video 15.6]. Over time, the sprout matures, and the thickness of the myelin and consequently the conduction velocity increase. The satellite potential then fires more closely to the main potential and ultimately will become an additional phase or serration within the main complex. It is usually necessary to put the main MUAP on a delay line to appreciate a satellite potential and to demonstrate that it is time locked to the main potential.
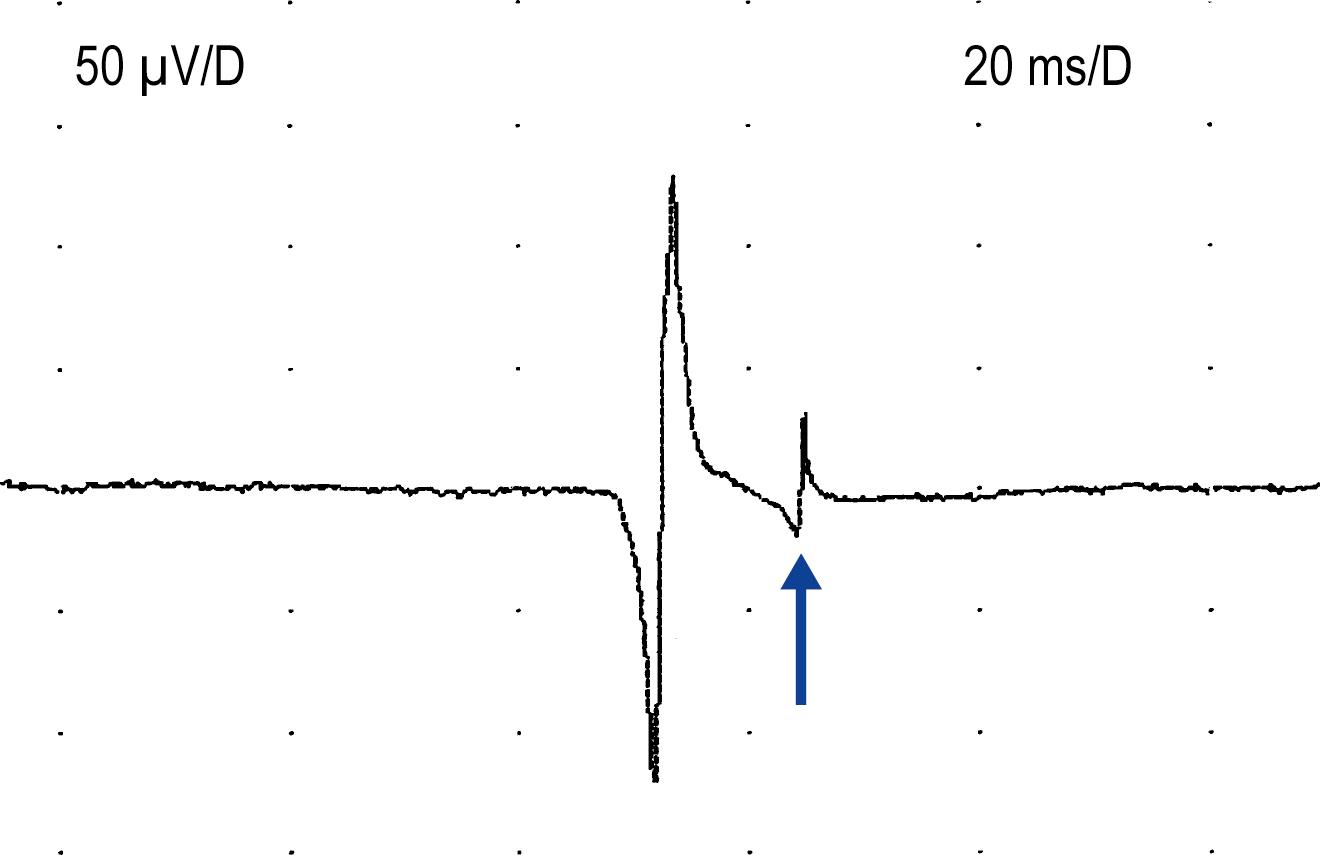

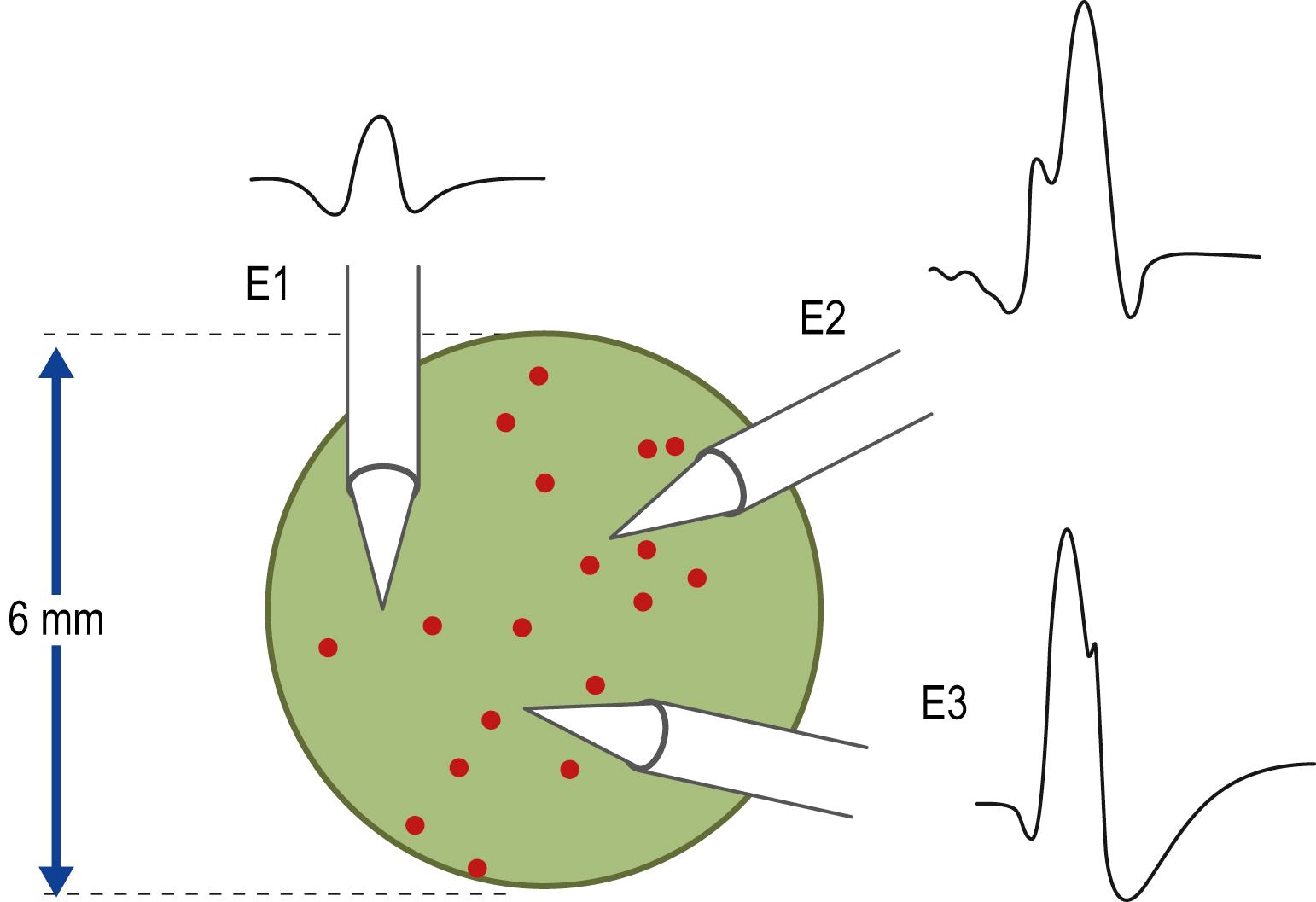
MUAP amplitude varies widely among normal subjects. Most MUAPs have an amplitude greater than 100μV and less than 2mV. Amplitude is generally measured from peak to peak of the MUAP ( Fig. 15.5 ). Amplitude is essentially a high-frequency response. Tissue between the needle and muscle fibers effectively acts as a high-frequency filter. Thus, unlike duration, most muscle fibers of a motor unit contribute little to the amplitude. MUAP amplitude reflects only those few fibers nearest to the needle (only 2–12 fibers) . Hence, amplitude is not as helpful as duration in judging motor unit size. Several factors are associated with increased amplitude, including (1) the proximity of the needle to the motor unit ( Fig. 15.9 ), (2) increased number of muscle fibers in the motor unit, (3) increased diameter of muscle fibers (i.e., muscle fiber hypertrophy), and (4) more synchronized firing of the muscle fibers. Listening to the EMG, the amplitude of MUAPs is correlated not with pitch but with volume.
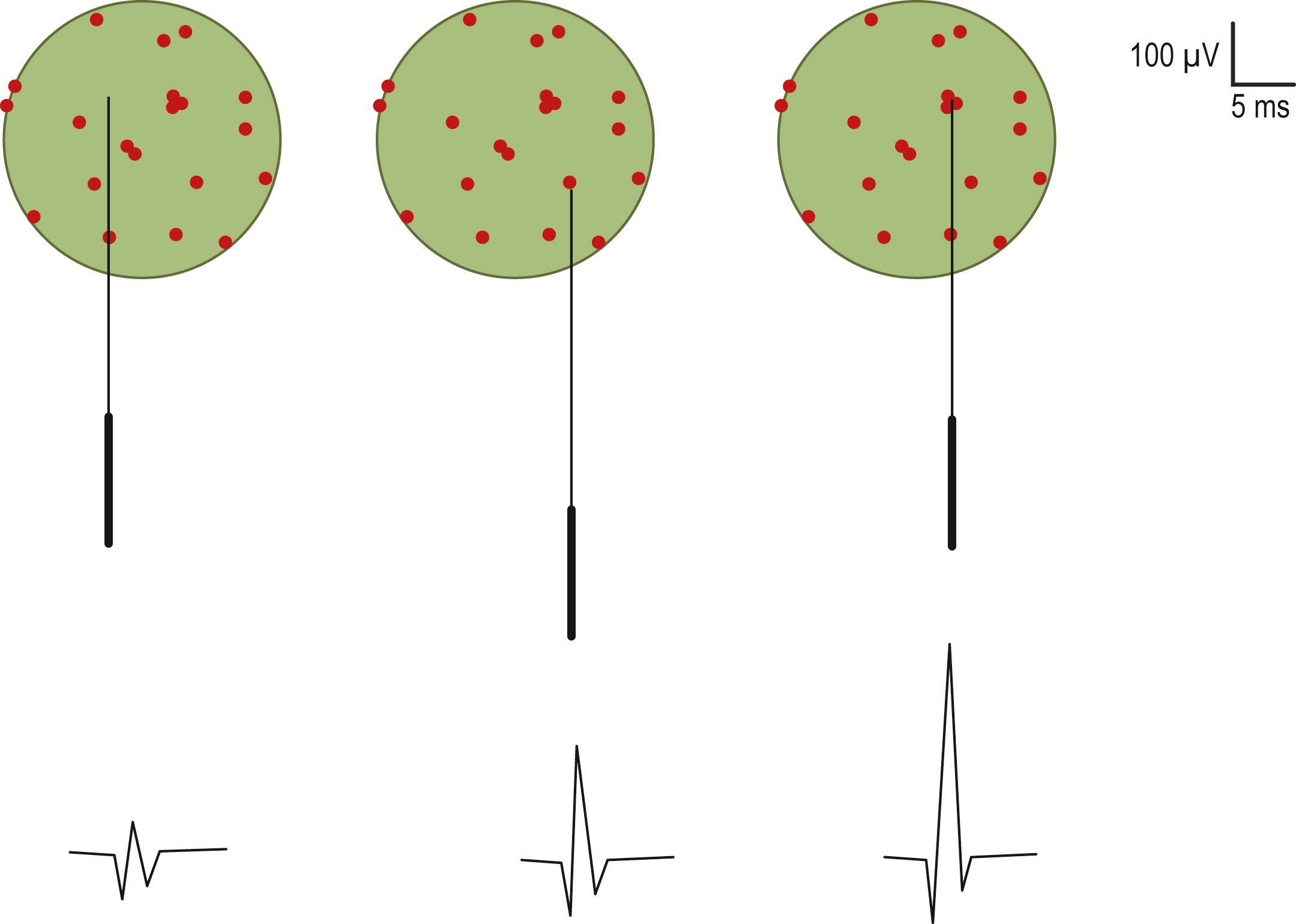
The major spike is the largest positive-to-negative component of the MUAP and usually occurs after the first positive peak ( Fig. 15.5 ). The major spike is the highest-frequency component of the MUAP. Because tissue acts as a high-frequency filter, as the needle is moved closer to the MUAP, the major spike increases in amplitude and its rise time shortens, indicating the proximity of the needle to the motor unit. MUAP parameters should be measured only when the needle is very close to the motor unit ( Fig. 15.10 ). When the needle is close to the motor unit, the MUAP becomes “sharp.” The sharp sound represents the high-frequency component of the major spike, occurring when the major spike rise time is less than 500 μs, indicating proper needle placement.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here