Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The first arthroscope was developed in 1920 with an optical cannula diameter of 7.3 mm by Dr. Kenji Takagi from Tokyo. His idea to look inside a closed knee with an instrument, a cystoscope, in 1918 came from his interest in the early diagnosis of tuberculous knees in Japan, which was a problematic disease at the time. Dr. Takagi is credited with being the first innovator and developer of arthroscopy. His successor, Dr. Masaki Watanabe, continued advancing Dr. Takagi's arthroscope design, which contributed largely to the popularization of arthroscopy. He also developed the concept of triangulation. Prior to Dr. Takagi, Dr. Nordentoft, a Danish surgeon, in 1912 published a manuscript at a meeting in Berlin, where he adapted the use of an endoscope to the knee joint and is credited as being the first to apply endoscopy to the knee, as well as the first to use the term “arthroscopy.”
Arthroscopy has revolutionized the treatment of intraarticular pathology. Arthroscopy has become the standard of care for many orthopedic problems and is currently the most common orthopedic procedure performed in the United States, with 1 million cases reported annually. Arthroscopy in experienced hands has low morbidity and high diagnostic yield. The benefits of arthroscopic surgery include reduced morbidity, less postoperative inflammation, smaller incisions, improved diagnostic accuracy, lower complication rates, reduced hospital stay, and reduced cost. The decision to use arthroscopy must involve consideration of the potential benefits of this method weighed against its limitations.
Advancements in arthroscopic technology have expanded its use in nearly every joint in the body, including those in the elbow, wrist, ankle, foot, and spine. Although results in some areas are superior to those of open surgery, such superiority has not been demonstrated for all arthroscopic procedures. The primary applications of arthroscopy are the diagnosis and treatment of intraarticular pathology. Arthroscopy is commonly used in the knee and shoulder for irrigation and débridement, synovectomy, removal of a foreign or loose body, débridement or repair of osteochondral lesions, and ligament reconstruction. Arthroscopy has also been applied to the hip for treatment of femoroacetabular impingement with repair or reconstruction of the labrum, cartilage, osseous deformity, and capsule. Absolute contraindications to arthroscopy are skin infection over the operative site or at a remote site, with risk of seeding. Relative contraindications are ankylosis of the joint and major capsular disruptions that risk excessive extravasation of fluid and make joint distension difficult.
Arthroscopy is performed in a standard surgical suite in a hospital or ambulatory surgical center. Arthroscopic equipment has become more streamlined, occupying less space in the operating room. Some operating rooms are now specifically made for use with arthroscopy and are fully equipped with mobile monitors and an arthroscopic tower attached to the ceiling along with the standard operating room lights ( Fig. 8.1 ). The operating room must be large enough to accommodate the required equipment and should be staffed by operating room personnel experienced with arthroscopy.

Arthroscopic cables and equipment are sterilized mostly by steam sterilizing autoclaves. The word autoclave comes from Greek roots auto (self) and clave (key), which together means self-locking. Autoclaves have an automatic locking ability that allow temperatures to exceed 270°F and pressures of 15 psi, which are the recommended settings for steam sterilization, creating an environment that no organism can survive in. The arthroscopic sterilization process begins with a standard wash of all the instruments, which then get wrapped with a blue sterilization wrap and sterilization indicator tape. Along with the sterilization indicator tape, a steam chemical indicator strip is attached to each individual tray and a Bowie-Dick Plus Test Pack is placed alongside the entire load to be autoclaved to ensure complete sterilization. These indicators turn black once fully autoclaved. A biologic indicator is also placed with the autoclave set, then inserted into a steam incubator and compared against a control biologic indicator for 1 hour to ensure all organisms have been eliminated. A plus sign for the control indicator and minus sign for the autoclaved indicator are digitally displayed to ensure complete sterilization. These sterilization tests are all documented and kept on record by the OR staff. For temperature-sensitive instruments such as smaller cameras and plastics, alternate methods of sterilization are used such as gas sterilization with ethylene oxide, low-temperature sterilization using peracetic acid (Steris, Mentor, OH), and cold disinfection using activated glutaraldehyde (Civco, Kalona, IA).
Advances in technology have resulted in improved arthroscope design and function. The arthroscopes currently used have improved optics and field of view with smaller diameter lenses, and they use fiberoptic and digital technology to improve visualization. Modern camera systems have the ability to use ultra HD 4K technology. Most arthroscopy systems allow video recording and the ability to take pictures. Newer technology integrating the camera system with tablet computers for arthroscopic video recordings, pictures, and editing will allow for higher-quality presentations and improved media for educational purposes.
The arthroscope is designed to fit inside a cannula, which is inserted into the joint first with use of a blunt trocar. Modern cannulas allow the flow of irrigation fluid into the joint. The camera is housed within the arthroscope and connected to the digital monitor for direct visualization of the joint. The light source, which comes from the light projector in the form of a fiberoptic cable, is attached to the arthroscope to allow visualization and minimizes the heat generated at the arthroscope.
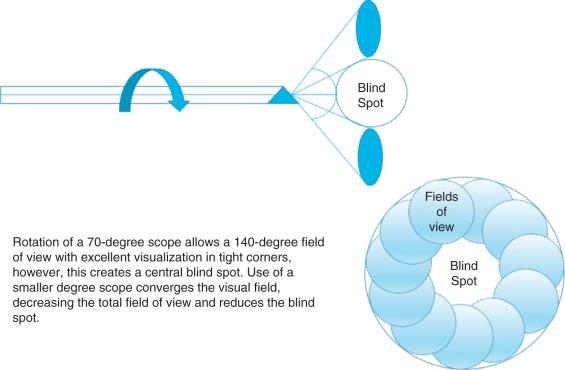
Arthroscopes have different optical characteristics, with several options in terms of lens diameter, field of view, and angle of inclination. The diameter of the lens determines the size of the arthroscope and the field of view and can vary from 1.7 to 7 mm. The field of view is represented by the total angle visualized by the lens of the arthroscope, with a larger lens diameter allowing a greater field of view. The angle of inclination is defined as the angle between the long axis of the arthroscope and a line perpendicular to the lens and can vary typically from 0 to 70 degrees. The advantage of using angled arthroscopes is that they provide better control and allow a wider field of view with rotation of the arthroscope, but a central blind spot directly in front of the arthroscope is created with arthroscopes that have a higher angle (70 to 90 degrees) ( Fig. 8.2 ). The degree of magnification of an object viewed with an arthroscope is determined by its distance from the lens. This characteristic makes judging arthroscopic distances and sizes difficult, but the use of an object of known size for comparison (such as a probe) can be of assistance.
The most commonly used arthroscope is 4 mm in diameter and has an angle of inclination of 25 to 30 degrees. Smaller joints can be accessed using arthroscopes with a smaller diameter (1.9 or 2.5 mm). Arthroscopes with increased angles of inclination (70 or 90 degrees) can be used to view difficult areas such as the posterior corners of the knee.
The fiberoptic light source and power console for shavers and drills are typically housed on an arthroscopic cart. Such a cart can be positioned easily in the operating room so it is close to the patient but does not obstruct personnel. Arthroscopy using modern equipment requires a light source capable of producing 300 to 350 watts, for which tungsten, halogen, LED, and xenon arc sources have been adapted. Fiberoptic cable uses bundled glass fibers to transmit light from the source to the arthroscope. The intensity and quality of light are diminished by the length of cable or damage to it, although modern fiberoptic cables are more durable.
Reduction of camera size, improved camera resolution, digitization of the video signal, and the integration of high-definition technology have all contributed to considerable improvement in the quality of visualization obtained using arthroscopy.
Irrigation fluid is vital for arthroscopy because it is responsible for joint distension, removal of debris, and improvement of visualization. Joint distension is supplied by the hydrostatic pressure of the irrigation fluid, which can be maintained using gravity, mechanical pumps, or manual control of outflow usually by the scrub tech. Every foot of elevation of the irrigation solution above the joint results in approximately 22 mm Hg of pressure. The use of a fluid pump allows more precise control of the rate of flow and hydrostatic pressure in the joint and can be used to minimize extravasation of fluids into the tissues.
Fluid management in arthroscopy consists of balancing the flow of fluids in and out of the joint. This balance is vital to maintain appropriate distension of the joint without causing excessive fluid extravasation into the tissues, and it plays a role in the management of bleeding, visualization, and debris clearance. Imbalances between inflow and outflow can cause turbulence of the irrigation fluid, reducing visualization and thus increasing operative time. This can occur when the shaver is used without compensatory changes in inflow/outflow or when the manual outflow of fluid is not controlled appropriately. Control of intraarticular pressure is critical, especially when working with the shaver in the posterior aspect of the knee. A situation where flow is decreased secondary to overzealous suction through the shaver can potentially deliver the posterior capsule into the shaver inadvertently. To prevent this problem, the inflow rate can be increased, the outflow through the suction or arthroscope can be decreased (or closed to prevent back flow), or outflow through the shaver can be decreased manually or by ensuring that the shaver window is occupied with tissue to be cut. Development of automated inflow and outflow mechanical irrigation pumps have shown promising results with consistent flow, greater degree of joint distension, and improved visualization, leading to reduced operative times. Modern irrigation systems also have functions that allow brief increases in pressure and flow to clear bleeding or debris, as well as functions to drain fluid such as at the end of the procedure.
A physiologic solution such as Ringer lactate or normal saline should be used for irrigation; the surgeon decides which solution to use. The addition of epinephrine to the irrigation fluid (1 mg/L) has been shown to shorten operating time and decrease bleeding, leading to improved visualization. Recently, it was shown that norepinephrine added to irrigation fluid reduces the incidence of hypotensive/bradycardic events significantly compared with epinephrine and is as efficacious in controlling intraoperative bleeding, thus maintaining clarity of the visual field when used in shoulder arthroscopy.
The temperature and osmolarity of the irrigation fluid used in shoulder arthroscopy has been a recent topic of discussion in the literature. Three randomized controlled studies evaluated the effect of warmed irrigation fluid versus room temperature irrigation fluid. One study did not demonstrate a significant difference in reducing perioperative hypothermia, whereas the other two showed that hypothermia occurred more often in the room temperature irrigation fluid group. Kim et al. showed that age and the amount of irrigation used correlated with core body temperature when using room temperature fluid and that warmed irrigation fluid decreased perioperative hypothermia, especially in elderly patients. The osmolarity of irrigation fluid may also be an important factor to consider when performing arthroscopy. An in vivo animal study was performed to evaluate the safety of using a hyperosmolar irrigation fluid (600 mOsm/L) compared with normal saline (300 mOsm/L) prior to designing a study on humans. They tested bilateral shoulders in dogs and found the mean percentage change in shoulder girth to be higher in the isotonic control group (13.3%) compared with the hyperosmolar group (10.4%). There were no detrimental effects on chondrocyte viability with either solution. Future clinical studies on this topic may provide more information on ways to decrease fluid extravasation during prolonged arthroscopic procedures.
A variety of hand-operated instruments are used in arthroscopy. Many are generalized, but some instruments have been developed for particular joints or procedure-specific tasks. These instruments include various arthroscopic probes, graspers, baskets, scissors, knives, suture passers, and radiofrequency instruments. The actual instruments required for arthroscopy depend on surgeon preference, the joint involved, and the procedure being performed.
The probe is the most important and used instrument in both diagnostic and therapeutic arthroscopy. Most probes are right angled at the working end, with a tip length of 4 mm that can be used to estimate intraarticular size, depth, and distance. Its primary purpose is palpation and identification of pathology, such as soft cartilage, loose bodies or cartilage flaps, meniscal tears, or insufficient tension of the anterior cruciate ligament. It is also a useful instrument for learning triangulation, planning surgical approaches, and positioning or retracting intraarticular structures or loose bodies. Care should be taken when palpating structures with the arthroscopic probe, because use of the tip may cause injury to tissues, and therefore use of the elbow for such activities is advisable.
Basket forceps are commonly used in procedures that involve the removal of intraarticular tissue, such as a meniscectomy. Basket forceps have a central opening and remove a portion of tissue that is then allowed to fall free into the joint, eliminating the need to remove the instrument from the joint to clear the basket each time ( Fig. 8.3 ). These forceps typically range in size from 3 to 5 mm and are available in straight, left- or right-curved, and up- and down-angled varieties to facilitate work in different areas. Left- and right-curved varieties enable the surgeon to access the anterior portion of the meniscus, whereas the up and down angled instruments permit trimming of the posterior meniscus around the femoral condyles. These instruments are also available in low-profile varieties for work in tight spaces, and some have hooked jaws that prevent tissue from slipping forward between the jaws when they are closed. Proper technique with these instruments is to use the jaws to remove small pieces of tissue because too large of a bite will strain the mechanical joints and may damage the instrument.

Grasping forceps are used to securely hold, apply tension to, or retrieve intraarticular materials. These forceps are available in jaw configurations that include numerous serrated interdigitating teeth or with one or two sharp hooks at the distal end of the jaws. Configuration of the grasping jaws can also differ, in that varieties exist with both or only one mobile jaw. The graspers with forceps that have both jaws mobile are more suited to grasping and gripping larger intraarticular objects.
Arthroscopic scissors are available in small and large sizes and with both straight and hooked blades to ensure an appropriate instrument for each situation. Hooked blades are easier to use compared with straight blades because they prevent the tissue from being pushed out from between the blades during the cutting motion. Curved and angled options, in which the shaft and blades are curved or the blades deviate from the shaft, respectively, are also available for difficult-to-reach resections.
Disposable arthroscopic knives are available in various shapes and sizes and should always be used with a cannula to protect the tissues during joint insertion and removal. Blade varieties include straight, curved, end cutting, and hooked, all of which allow the appropriate instrument for each situation. An important and useful characteristic of many arthroscopic knives is that the blades are magnetic to facilitate removal from the joint should it break.
Motorized shavers consist of a pair of cylinders, one inside the other, each with a matching window. The inner cylinder spins within the outer and has an edge to both sides of its window that cuts tissue drawn into the outer cylinder by the attached suction. The removed tissue is then drawn down the inner cylinder, out of the joint, and into a suction trap. Commonly used motorized shavers range in diameter from 3 to 5.5 mm, but a 2-mm option is available for access to smaller or tight joints. Shavers with a larger diameter have larger windows and can expedite removal of tissue. Shavers also are available in various shapes and angles with different blades or burrs, all designed for specific purposes. Control of the motorized shaver is possible either by a hand or foot pedal and allows clockwise, counterclockwise, and alternating rotation to improve the efficiency of tissue cutting and allow clearing of the blade. Practically, when the motorized shaver is in use, the blades should be in the field of view to prevent unwanted damage to normal tissues.
Cannulas and switching sticks of numerous sizes are available to assist with the insertion and use of instruments during arthroscopic procedures; they are all designed for use in specific joints. Cannulas are used to maintain the integrity of a portal into the joint so that the intervening soft tissues do not interfere with activities such as knot tying. They also allow easy insertion of instruments without trauma to the tissues through which the portal is made. Switching sticks are used to ease the passage of the arthroscope and cannulas into the joint in question by holding the path through the soft tissues into the joint so that a cannula or arthroscopic sheath can be inserted into the joint over it. When working in joints that are deep from the surface, switching sticks are particularly useful in maintaining these paths.
Electrocautery and radiofrequency instruments can be used for cutting and shrinking soft tissues and can play an important role in maintaining hemostasis. A variety of these instruments have been developed for use in specific joints or for specific purposes, including some with flexible tips. Electrocautery uses heat directly from the probe to effect tissue changes and has been adapted for intraarticular use with various irrigation solutions.
Radiofrequency instruments generate a high-frequency electromagnetic current at their tip, causing heat to be generated by the resistance to current passage through tissue. Monopolar and bipolar radiofrequency systems have been adapted for arthroscopic use. Monopolar systems allow current flow from the tip of the instrument to a grounding pad on the patient, using the path of least resistance, and generate heat at the tissue closest to the tip. Bipolar devices permit passage of current between two electrodes at the tip of the instrument, heating the tissue between them. The primary difference between the two radiofrequency systems is that monopolar instruments require a grounding pad to allow energy to pass from the body, whereas bipolar instruments pass energy between electrodes at the intraarticular site of interest.
The specific effect of radiofrequency instruments on tissues depends on the amount of heat transferred. Low levels of heat transfer cause collagen, which is the major constituent of most soft tissues, to denature and shrink by as much as 50% of its length. Higher levels of heat destroy collagen and are commonly used for tissue ablation and débridement. Use of these instruments intraarticularly may cause high fluid temperatures leading to cartilage damage or chondrolysis. Cadaveric studies have been performed measuring the effect of radiofrequency devices on intraarticular fluid temperature and cartilage. Increased duration of application, decreased distance between the probe and soft tissue, and decreased fluid rate showed temperatures deleterious to articular cartilage chondrocytes (>50°C). Irrigation-fluid flow is critical for maintaining low fluid temperatures rather than the continuous or intermittent use of the thermal device, because decreased flow rates significantly increase the temperature of the irrigation fluid. The penetration depth and area affected are proportional to the power and temperature used. A level I study evaluated a standard radiofrequency device compared with a new plasma radiofrequency device and found no significant difference between the two systems with respect to temperature generation or operative time.
“Arthroscopy is an art that requires three dimensional thought and vision.” –Dr. Ronald Krinick, MD, New York, 2010
There are several skills required before one can successfully perform arthroscopy. The top four general skills are anatomic knowledge, tissue manipulation, spatial perception, and triangulation. The top two skills specific to arthroscopy are portal placement and triangulating the tip of the probe with a 30-degree scope. Triangulation is the process by which your brain converts a two-dimensional arthroscopic image into a three-dimensional space, allowing your hands to manipulate an instrument entering from one portal in front of an arthroscopic camera with a specific degree of angulation from a separate portal. This is the most difficult aspect of arthroscopy initially and one that requires experience. Cadavers, arthroscopic computer simulators, and homemade arthroscopic simulators are great tools to have for acquiring these basic skills.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here