Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Bacterial sexually transmitted diseases (STDs) have become an important medical challenge worldwide, especially among the tropical countries. The ubiquitousness of STDs affects all nations and races, but is particularly evident in developing countries. Insufficient health-care centers, inadequate laboratory capabilities, and the unavailability of appropriate drug regimens of treatment perpetuate the prevalence of these STDs. However, it is important to appreciate that underservicing of areas and regions is not found exclusively in developing countries, but is evident in developed regions as well.
Syphilis is still a public health problem in many countries and some ethnic manifestations of the disease, especially among black populations, make it one of the most interesting dermatologic diseases nowadays. Pinta, bejel, and yaws are uncommon and non-venereal treponematoses that have been almost eradicated from most countries but are still observed in some areas of South America (Amazon rain forest), Middle East, and North Africa. These diseases were identified as human pathogens in early hominids, millions of years ago, because of the bone patterns associated with these infections.
Chlamydial and gonococcal infections are common worldwide, but the high endemicity in some tropical countries will allow the identification of some uncommon signs and symptoms associated with these diseases, such as the esthiomenic syndrome of lymphogranuloma venereum (LGV) and gonococcal ophthalmia in newborns.
The huge impact of human immunodeficiency virus (HIV) infection is especially clear among the STDs. It is well recognized that any previous STD is associated with an increased risk for HIV infection, particularly those characterized by genital ulcers such as syphilis, granuloma inguinale, and chancroid. Bacterial STDs are still a major threat to human health worldwide and should be considered as important infections.
Members of the order Chlamydiales are obligate intracellular Gram-negative bacteria. The order Chlamydiales has one family, the Chlamydiaceae, containing one genus, Chlamydia , and three species pathogenic to humans: C. trachomatis , C. psittaci , and C. pneumoniae .
C. trachomatis is a strictly human pathogen, with a tropism for the genital and conjunctival epithelia. C. trachomatis consists of 19 different serovars. Types A, B, Ba, and C infect mainly the conjunctiva and are associated with endemic trachoma; serovars D, Da, E, F, G, Ga, H, I, Ia, J, and K are predominantly isolated from the urogenital tract and are associated with STDs, Reiter's syndrome, inclusion conjunctivitis, or neonatal pneumonitis in infants born to infected mothers. Serovars L1, L2, L2a, and L3 can be found in the inguinal lymph nodes and are associated with LGV.
C. trachomatis is present in about 80% of patients with the venereal form of Reiter's syndrome – a disorder recognized by the clinical triad of arthritis, urethritis, and conjunctivitis. It is implicated as a possible agent of the disease and is considered to have a trigger function. Circinate balanitis is the most common cutaneous finding, being reported in about 36% of patients ( Fig. 26-1 ). Another common manifestation is keratoderma blennorrhagicum (15%), a scaling plaque-like process that resembles pustular psoriasis with a combination of crusting, exudation, and erosion associated with erythema ( Fig. 26-2 ).


C. trachomatis has the highest prevalence amongst young men and women. It is the most common STD in western countries. Worldwide, 89 million cases are estimated to occur each year. Infection with this agent can be asymptomatic in up to 80% of women. Left undetected and untreated, Chlamydia can ascend the upper genital tract, causing inflammation and scarring in both the female and male reproductive tract. In women it is responsible for urethritis, cervicitis, pelvic inflammatory disease, and sequelae such as infertility and ectopic pregnancy. In men it can cause arthritis and epididymitis, which can result in urethral obstructions and decreased fertility in some cases. Neonates may present with conjunctivitis and pneumonia.
Nicolas–Favre–Durand, tropical bubo, climatic bubo, d'emblé bubo, scrofulous bubo, subacute inguinal lymphogranulomatosis, inguinal lymphogranuloma
LGV is an uncommon STD with transient genital lesions followed by significant regional lymphadenopathy and systemic manifestations. LGV may progress to late fibrosis and tissue destruction in untreated cases.
The disease is almost always transmitted by sexual contact. Transmission has been attributed largely to asymptomatic female carriers. The main age of onset is 25 years, but the disease can be seen in any age group. The highest prevalence is found in young single male patients of low socioeconomic and educational status. Prostitutes and male homosexuals have a major role in the transmission of the disease.
The clinical course of LGV is classically divided into three stages.
The incubation period is extremely variable, but has been estimated to be between 1 and 2 weeks. This transient primary lesion usually appears as a vesicle, small erosion, or an ulcerated area that lasts for 2–3 days. The site of the primary lesion is usually around the genitals but may be anal, rectal, or oral, mainly in male homosexuals.
LGV is primarily a disease of the lymphatic system that progresses to lymphangitis. Adenopathy represents the most important objective element of the clinical exam and is unilateral in 60% of these cases. It usually occurs 2–4 weeks after onset of the primary lesion. In its earlier stages the adenopathy syndrome consists of painful inflammation and infection of the inguinal and / or femoral lymph nodes. In women, the deep pelvic nodes may also be involved. After several days they become matted, with a firm lobulated swelling not attached to the deep tissues. The overlying skin is often slightly reddened and edematous ( Fig. 26-3 ), but later it may become thickened and develop a purple hue. In a short time the lymph nodes become tender and fluctuant and are referred to as buboes. In the natural evolution of LGV, the nodes may undergo necrosis and spontaneous fistula tracts may develop ( Fig. 26-4 ). These nodes may also become fluctuant and rupture in 30% of patients. Although most buboes eventually heal without complications, some may progress to develop chronic sinus formation. The emergence of many fistulous orifices explains the comparison made with a “watering can.” There may be fever and chills during this stage of LGV, associated with other non-specific systemic symptoms such as headache, nausea, anorexia, and myalgia.


This stage does not necessarily follow the lymphadenopathy. It involves a series of conditions, resulting from progressive spread of the disease with destruction of tissue in the involved areas, including proctitis, acute proctocolitis mimicking Crohn's disease, fistulae, strictures, and a chronic granulomatous disfiguring condition of the vulva (esthiomene). The lymph nodes rupture, causing hemorrhage and friability of the anorectal mucosa, with rectitis, tenesmus, mucosanguineous rectal discharge, and constipation. Later, as healing occurs, there is formation of strictures, fistulas, and abscesses with destruction of anal and rectal structures ( Fig. 26-5 ).

The destruction of lymph nodes may result in elephantiasis of the vulva or penis and scrotum. It represents late manifestations, which are rare today. An association with rectal cancer has been reported. The esthiomenic syndrome, composed of vulvar ulceration followed by sclerosis and tegumentar hypertrophy, can occur in patients with LGV.
No studies have been performed on patients with concomitant HIV infection and LGV, and remarkably little anecdotal evidence regarding clinical features and treatment has been published. HIV appears to have no effect on the clinical presentation of the disease.
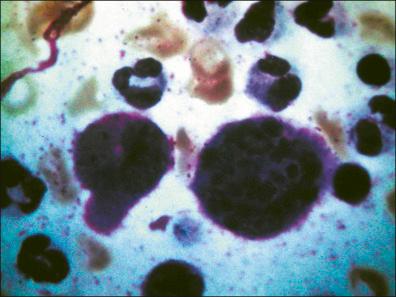
LGV can be suspected on positive Chlamydia serology and isolation of C. trachomatis from the infected site. Samples must contain cellular material that is obtained for direct bacteriological exam and culture from affected lymph nodes by aspiration from fluctuant lymph nodes / buboes, from the ulcer base exudates, or from rectal tissue. Staining of the smear (Giemsa or fuchsin) reveals the intracellular corpuscles of Gamna–Miyagawa, which occur in some chlamydial infections ( Fig. 26-6 ).
The culture on cycloheximide-treated McCoy cells of material from suspected LGV lesions is labor intensive, expensive, and of restricted availability. Its sensitivity is 75–85% at best, and often closer to 50% in the case of the bubo aspirate.
A complement fixation test, using group-specific antigens, is typically positive within 2 weeks of the onset of disease. A titer of ≥ 1 : 16, in the presence of a compatible clinical syndrome, is suggestive of LGV. Titers > 1 : 64 are considered diagnostic of LGV. Serial samples with a 15-day interval frequently show a fourfold increment in titer in the acute stage of the disease. Indirect immunofluorescence represents a sensitive method, but is not widely available. Antibody titers do not necessarily correspond with disease activity and may not decline after treatment. The microimmunofluorescence test is the only serologic means of distinguishing between different serotypes of C. trachomatis and is the diagnostic test of choice.
Enzyme-linked immunosorbent assay (ELISA) is considered a convenient and objective method, suitable for ulcer scrapes or bubo aspirates. Sensitivity is lower than other methods (75–80%) and should be confirmed by another method. Monoclonal antibodies are an extremely sensitive method and have high specification in the diagnosis of the LGV, capable of preventing serologic cross-reactivity among the causative and other serotypes of C. trachomatis .
Detection of nucleic acid is by DNA amplification techniques such as the ligase chain reaction (LCR) or polymerase chain reaction (PCR); these methods are becoming established for routine testing.
The differential diagnosis includes chancroid, syphilis, ganglionar tuberculosis, cat-scratch disease, and Hodgkin's disease. Late manifestations must be distinguished from neoplastic skin disease, filariasis, rectal cancer, inflammatory bowel disease, and hidradenitis suppurativa.
No controlled double-blind treatment trials have been published on LGV. However, because of its symptoms, which can often be difficult to perceive at first, and in view of the important consequences that may result from non-treatment of the disease, both rigorous evaluation of management and early treatment are of paramount importance. The sooner we begin treatment, the lower is the chance of chronic lesions.
Proper treatment cures infection and prevents ongoing tissue damage.
First choice is doxycycline:100 mg orally every 12 h, for 3 weeks.
Second choice is erythromycin base: 500 mg orally every 6 h, for 3 weeks.
Other treatments include:
Tetracyclines: 500 mg PO every 6 h, for 2–4 weeks
Thiamphenicol: 500 mg (2 capsules) PO every 8 h, for 2–3 weeks
Sulfadiazine: 500 mg PO every 6 h, for 2–3 weeks
Sulfisoxazole: starting dose of 4 g PO and then 2 g for 2–3 weeks.
The activity of azithromycin against C. trachomatis suggests that it may be effective with 1 g orally once weekly, for 3 consecutive weeks, but clinical data on its use are lacking. Alternative treatment with fluoroquinolone has also not been evaluated, but could be effective.
Clinical monitoring and evaluation of patients until cure are mandatory. After an initial course of treatment, patients should be seen at least every 3 months for 1 year. Retreatment should be given if there is clinical evidence of relapse. Sexual contacts should be treated similarly.
Pregnant and lactating women should be treated with the erythromycin regimen. Due to the risk of discoloration of teeth and bones, doxycycline should be avoided in the second and third trimester of pregnancy, although it is compatible with breast-feeding.
People who have had sexual contacts with a patient who has LGV within 60 days before onset of the patient's symptoms should be examined, tested for urethral or cervical chlamydial infection, and treated. The patient should be presumptively treated with doxycycline 100 mg orally twice a day for 7 days, or azithromycin 1 g orally single dose.
The Centers for Disease Control recommend the same treatments for LGV in HIV-negative and HIV-positive patients, with the note that these patients may not respond as well to therapy and so prolonged treatment may be required.
Tense and fluctuant nodules (buboes) require aspiration through intact skin to prevent major ulcerations. Dilation and partial amputation of the rectum are measures occasionally indicated to correct rectal stricture. Vulvectomy and colostomy are seldom necessary.
Patients should be followed clinically until signs and symptoms have resolved. This may occur within 3–6 weeks. However, there is also evidence of spontaneous remission in 8 weeks.
The prognosis is excellent for acute infections treated with appropriate antibiotics. The late disease becomes rarer each day, but severe lymphatic involvement is frequently irreversible. Malignant transformation of the genital lesions of elephantiasis and anorectal syndrome, which is more common in females, is considered exceptional. Therefore, we emphasize the importance of introduction of drugs in the early stages of infection.
Blennorrhagia, blennorrhea, “flow of seed”
Pandemic STD, only rarely spread by accidental contamination, mainly affects genital, rectal, oropharyngeal and conjunctival mucosa.
Gonorrhea is one of the most commonly reported diseases in the world. A few decades ago it was described as the second most common infectious disease, after flu. Today it is the second most common notifiable infectious disease in United States; the first is Chlamydia .
Gonorrhea in women, when not treated, can provoke infection of the upper genital tract, which can lead to ectopic pregnancy and infertility. In many developed countries, such as the USA, the rates of gonorrhea declined from 1970 to the mid 1990s. However, in 2008, the World Health Organization (WHO) estimated the global burden of gonorrhoea among adults to be 106 million cases, which represented a 21% increase since 2005.
Dissemination to other parts of the body varies from 0.5% to 3%, mainly affecting women, and manifests as gonococcal arthritis–dermatitis syndrome, suppurative arthritis, and rarely endocarditis, meningitis, or other localized infection.
Gonococcal drug resistance is increasingly common and the antimicrobial resistance profile of Neisseria gonorrhoeae is worsening, and as a consequence this disease still merits considerable attention.
The first reports of urethral secretions date from the time of the Chinese emperor Huang Ti, in 2637 bc . The disease was known to the Egyptians, and in 1500 bc Moses, father of the Hebrews, mentioned it in the Old Testament in Leviticus, indicating sanitary methods for its control.
In 1838, Ricord defined gonorrhea as inflammation of the urethra due to various causes. Neisser, in 1879, identified the etiologic agent, and called it gonococcus. In 1881, Credé demonstrated that silver nitrate could prevent ophthalmologic gonorrhea in newborns ( Fig. 26-7 ). Leistikow made the first culture of this microorganism in 1882. After long years of using potassium permanganate solution in intraurethral irrigations and instillations, sulfa drugs appeared in the 1930s. In the following decade penicillin was able to cure nearly all cases. In the early 1960s, the selective Thayer–Martin culture medium facilitated research and etiologic diagnosis.

The global map of the WHO, with estimates of the number of annual new cases of the four main STDs, shows their importance for public health. Few countries have a reliable system to notify transmitted infections, however. The total number of new cases of the four STIs in 2008 in adults between the ages of 15 and 49 was estimated to be 498.9 million. Gonorrhea alone accounts for 106 million new infections per year. Obviously, the developing countries are the most affected. Nevertheless, this is still a serious public health problem all over the world, including the developed countries. On a global scale, up to 4000 newborn babies annually may become blind because of gonococcal and chlamydial ophthalmia neonatorum.
Adolescents and young adults (15–25 years old) are the most affected. However, gonococcus has been increasingly found in individuals over 50 years old. New sexual stimulant medications for men (sildenafil, among others) and hormonal replacement therapy for women, along with greater acceptance of and increased sexual activity in older people could be among the reasons for increasing STDs in this age group. On the other hand, sexual abuse of children with transmission of STDs has become increasingly common. Under these circumstances, gonorrhea, as a purulent bacterium, has a high degree of infectiousness.
The risk of sexual transmission by men infected with urethral gonorrhea is more than 90%, while in infected women the risk of transmission to sexual partners is 50–60%.
As with all STDs there is an increased relative risk of HIV transmission, the average concentration of the virus in the seminal fluid is eight times greater in men with urethritis. HIV is present in cervicovaginal secretion in a concentration doubled among women with gonorrhea.
In adults, gonococcus species are mainly pathogens of the columnar and non-cornified squamous epithelia. After contagion, the gonococcus initially avoids the reaction of immunologic systems, thanks to fimbriae and external cytoplasmic membrane proteins. Through the protease, immunoglobulin A (IgA), mediated by the fimbriae and protein II, attaches to the host cell. The lipopolysaccharides impede ciliary activity and protein I promotes a closer contact between the gonococcus and the cell, followed by phagocytosis, and the gonococci are transported unharmed in phagosomes to the base of the cell, where they reproduce. From there, at some variable time afterwards, they are ejected to the subepithelial layers, initiating the local inflammatory process, exteriorization to the surface, and a possible invasion of the blood stream, provoking remote infections. The mononuclear lymphocytic infiltration and abnormal tissue may persist for weeks even after negative cultures.
It appears that the gonococcus prepares the way for subsequent infections by less aggressive microorganisms.
N. gonorrhoeae is a Gram-negative intracellular polymorphonuclear bacterium, about 0.6–1 mm in diameter, reniform, grouped two by two, and joined at the concave side. It grows only in enriched media (Thayer–Martin) with vitamin supplements, using inhibitors such as vancomycin, colistin, and nystatin, at an optimal temperature between 35 and 36.5°C in 5% CO 2 .
The incubation period varies from 2 to 10 days. However, it can range from 24 hours to 20 days.
The clinical manifestations differ between sexes. In men, the symptoms begin with a sensation of stinging or intraurethral itching, with dysuria. Soon after, a urethral mucosal flow starts that rapidly becomes mucopurulent, spontaneously flowing abundantly, or with very light pressure ( Figs. 26-8 and 26-9 ). The edges of the urethral meatus become edematous, with erythematosus ( Figs. 26-10 and 26-11 ).

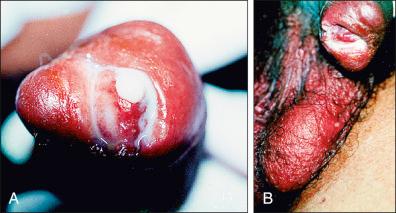

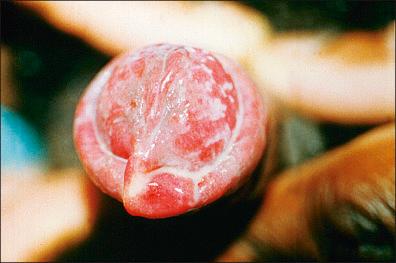
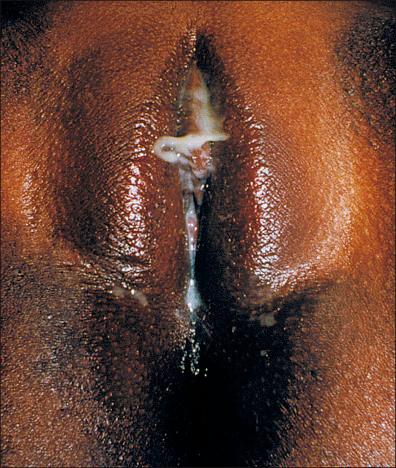
In women, gonococcal urethritis does not have such an exuberance of signs and symptoms as it does in men; the clinical manifestations are dysuria, a need to urinate, and, less frequently, a yellowish secretion ( Fig. 26-12 ). Generally, cases of gonorrhea in women are explained by endocervicitis, which, associated with clinical history data, make it possible to suspect gonococcal infection. However, over 90% of women remain asymptomatic.
The most frequent complications in men are: balanoposthitis, littritis, cowperitis, prostatitis, epididymitis ( Fig. 26-13 ), and urethral stenosis. In women the complications are: bartholinitis, infection of the upper genital tract (endometritis, salpingitis / inflammatory pelvic disease, pelviperitonitis), and peripatitis.

Other tegumentar manifestations include:
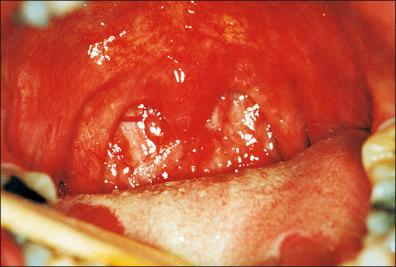
Buccopharyngeal gonorrhea – usually with massive oral edema and erythematous aspect of the uvula and tonsils, pustular areas in the pharynx, and irregular erosions on the upper surface of the tongue ( Fig. 26-14 )
Anorectal gonorrhea – presenting as acute proctitis with pain, pruritus, tenesmus, and rectal bleeding and purulent discharge
Conjunctivitis gonorrhea – with purulent exudate and ulceration of the cornea, an important clinical condition of the newborn babies of infected mothers (vaginal delivery or postpartum) potentially causing blindness, but can also be acquired by self-inoculation
Perihepatitis gonorrhea (Fitz–Hugh–Curtis syndrome) – resulting in abdominal pain, especially in the right upper quadrant, and signs of peritonitis. This occurs by direct spread of N. gonorrhoeae from the fallopian tube to the adjacent liver capsule and peritoneum, or by hematogenous or lymphatic spread.
In men, as well as in women, gonorrhea spreads to other parts of the body in 0.5–3% of affected patients and mainly affects the skin (dermatitis), articulations (arthritis), and, with less frequency, the bones (osteomyelits), the heart valves (endocarditis) and the brain (meningitis).
Approximately 50–75% of patients with disseminated gonococcal infection have cutaneous lesions, mainly in the nearby articular regions.
This clinical picture is composed of up to 10 small and painful lesions, which appear on the distal surfaces of the extremities ( Fig. 26-15 ). The lesion begins with a hemorrhagic macule with posterior pustulization, and a gray necrotic center, surrounded by a violet halo, which can evolve to form a crust ( Fig. 26-16 ).


The diagnosis can be made by demonstrating the microorganism in cutaneous lesions. Whenever one suspects gonococcemia, it would be prudent to obtain culture samples of all of the probably infected areas, and also from the blood, as the latter tests are positive in more than 50% of patients in the initial phase of the infection.
Differential diagnosis of gonococcemia lesions should be made, principally with meningococcemia lesions.
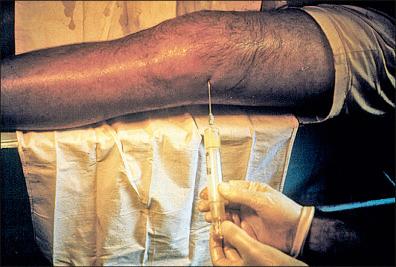
In young and sexually active people, gonococcal arthritis is the most frequent. It is present in more than 90% of cases of gonococcal septicemia, often being polyarticular. The symptomatology varies from arthralgia to acute arthritis, affecting mainly the wrist and knee. Synovial liquid can be removed by puncture; it will be serous or purulent, with high concentrations of proteins and low concentrations of glucose ( Fig. 26-17 ). If it is not immediately treated, the infection can evolve to erosion of the cartilage, atrophy of the adjacent bone structures, and incapacitating arthritis.
It is only possible to demonstrate the gonococcus, by bacterial culture or by direct exam, in 50% of the cases. The investigation includes centrifugation of the liquid and examination of the sediment.
The differential diagnosis should be made in comparison with other types of septic arthritis, including rheumatoid arthritis, rheumatic fever, and Reiter syndrome.
Normally, the signs only show up on radiologic examination 20 days after the initial appearance of arthritis, frequently revealing a decrease in the articular space with subchondral cysts and articular osteoporosis.
Recent revision of the Laboratory Diagnosis of Sexually Transmitted Infections manual by the WHO provides a basic understanding of the principles of laboratory tests in the context of screening and diagnostic approaches, and antimicrobial susceptibility testing for gonorrhea and other STDs. Indications and variations of sensitivity and specificity are observed between laboratory diagnostic methods ( Table 26-1 ).
| Exam | Sensitivity (%) | Specificity (%) |
|---|---|---|
| BACTERIOSCOPY BY GRAM | ||
|
90–95 | 95–99 |
|
45–65 | 90–99 |
|
Not recommended | |
| CULTURE | ||
|
94–98 | > 99 |
|
85–95 | > 99 |
| Molecular biology | 95–98 | > 99 |
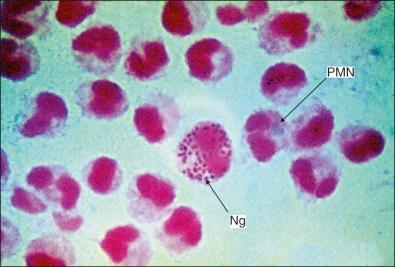
Bacterioscopy of the urethral secretion with Gram stain can show bacteria (intracellular Gram-negative diplococci) within polymorphonuclear leukocytes ( Fig. 26-18 ). Direct microscopic examination is not recommended for the diagnosis of rectal and pharyngeal infections because of the large number of other organisms present and the low sensitivity. Nevertheless, it is sensitive and specific in symptomatic men with urethral discharge.
Recommended selective media include: Thayer–Martin, modified Thayer–Martin, and New York City agar.
In cases of acute urethritis in men, bacterioscopy is a good method of culture. In women, culture of material from the cervical canal is the best option. It is sensitive and highly specific in optimized circumstances, inexpensive, and allows antimicrobial susceptibility testing.
In the case of disseminated infection, in addition to blood cultures, material must be collected from all the areas potentially infected (e.g., in dermatitis, swabs of the skin material and skin samples for biopsy; in arthritis, synovial fluid for punch biopsy; and in meningitis, lumbar puncture). In addition, one should always collect oropharyngeal material, and perianal and genital secretions.
Molecular detection of specific nucleic acid (DNA /RNA) sequences of N. gonorrhoeae is most commonly performed using commercially available kits that detect both N. gonorrhoeae and C. trachomatis , in the same kit and sometimes simultaneously, and often at little or no extra direct cost. Nucleic acid amplification tests (NAATs) generally have a greater sensitivity than culture, especially for pharyngeal and rectal samples. However, the specificity of several of the gonococcal NAATs is suboptimal in the diagnosis of urogenital samples and, in particular, extragenital samples, which results in low positive predictive value in low-prevalence populations. Despite these disadvantages, the use of appropriate NAATs in addition to culture (for antimicrobial susceptibility testing) should be encouraged even in resource-constrained settings.
The differential diagnosis in men is mainly non-gonococcal urethritis ( C. trachomatis , Mycoplasma hominis , Ureaplasma urealyticum , or Trichomonas vaginalis ), chemical urethritis (introduction of irritating substances into the urethra for prophylactic or curative purposes), and traumatic urethritis (due to the habit of expressing the gland to demonstrate secretion [milking]). Men with painful and / or swollen testicles may have a tumor or a twisted testicle.
In women the differential diagnosis is endocervicitis, bartholinitis, and salpingitis (infection of the upper genital tract in women) caused by Chlamydia .
Other differential diagnoses are necessary when the gonococcal infection settles in the skin, joint, eyes, etc. For example, gonococcal meningitis has clinical features similar to other types of bacterial infections, particularly the meningococcal type; differentiation is made by CSF culture.
The significant increase in the spread of infection by N. gonorrhoeae is due to the great ability of this bacterium to acquire antibiotic resistance. In recent decades numerous research papers have identified strains resistant to several antibiotics, such as penicillins, tetracyclines, fluoroquinolones, and, most recently, cephalosporins. Because of the great global concern over this, treatment of these infections requires constant monitoring of therapeutic failures and possible results. A thorough and didactic review of overall resistance was recently published by Lewis.
The treatment can be categorized by uncomplicated and complicated cases. Table 26-2 details the treatments recommended by some of the major organizations in cases of urethritis and endocervicitis. The Centers for Disease Control and Prevention (CDC) in 2012 and 2015, based on data from its Gonococcal Isolate Surveillance Project (GISP), reviewed the therapeutic regimen for gonorrhea.
| CDC (2015) | UK Guideline (2011) | EURO Guideline (2012) | |
|---|---|---|---|
| RECOMMENDED REGIMEN |
|
|
|
| ALTERNATIVE REGIMEN |
|
|
|
The CDC until recommends other drugs, if ceftriaxone is not available: ceftizoxime (500 mg IM), cefoxitin (2 g IM with probenecid 1 g orally), and cefotaxime (500 mg IM). Gonococcal infection of the pharynx is considered to be slower in healing and more difficult to eradicate than infections at urogenital and anorectal sites. The regimen recommended is: ceftriaxone 250 mg IM associated with azithromycin 1 g orally in a single dose, or doxycycline 100 mg orally each 12 h for 7 days in the case of azithromycin allergy.
In pregnancy and breast-feeding, ceftriaxone 500 mg IM is indicated, plus azithromycin 1 g orally in a single dose, or spectinomycin 2 g IM in a single dose.
Patients infected with HIV and gonococcal infection receive the same treatment regimen as those who are HIV negative.
The treatment indicated for complicated infections (disseminated gonococcal infection, endocarditis, orchiepididymitis, etc.) is ceftriaxone 1 g IM or IV every 12 or 24 hours plus azithromycin 1 g orally in a single dose for 10–14 days.
In chronic, extragenital, and / or complicated infections, treatment regimens should not comprise single doses; rather, classical doses and intervals should be implemented, for not less than 10 days.
Since infection with gonococci associated with C. trachomatis can exceed 30%, especially in young women, simultaneous treatment for this agent should also be started. In these situations the most commonly used treatment regimens are:
Uncomplicated disease or infection of the lower genital tract by Chlamydia (urethritis, endocervicitis):
Azithromycin 1 g orally in a single dose
Doxycycline 100 mg orally twice a day for 7 days
Doxycycline 200 mg orally once a day for 7 days
Erythromycin (stearate) 500 mg orally four times for 7 days
Complicated disease, or affecting the upper genital tract (endometritis, salpingitis / pelvic inflammatory disease), epididymitis, arthritis:
Doxycycline 100 mg orally twice a day, or 200 mg orally once a day for 14 days.
The successful method of Credé for preventing neonatal ophthalmia, in which aqueous solution of silver nitrate 1% is administered into the conjunctival sac soon after birth, effectively renders a diagnosis of this condition nowadays a blatant disregard for public health.
Treatment of a case of gonorrhea or other STD / genital infection requires immediate action. The syndrome approach permits immediate action, including a detailed investigation, whenever possible and indicated. Consequently the following steps should not be postponed:
Carry out a thorough clinical history.
Perform a satisfactory physical exam.
Advise counseling (health education).
Offer Venereal Disease Research Laboratory (VDRL, RPR, rapid test, etc), HIV, HTLV 1 and 2, and hepatitis testing.
Emphasize adherence to treatment (therapy supervised at the doctor's examination).
Emphasize the importance of consulting / treating sexual partners.
Emphasize the importance of family planning.
Emphasize the importance of periodic examinations (gynecologic, prostate).
Make condoms available (male / female).
Notify the official public health organizations of the case.
Schedule a return visit by the patient.
Patients with immunodeficiency (acquired immunodeficiency syndrome [AIDS], malignant neoplasms, use of immunosuppressors) can have atypical and / or exaggerated responses to many infections. In these people the treatment may require a higher dose, more time, and even changes in the route of administration of the drugs. It is not uncommon to have to repeat the treatment regimen or hospital stay with intravenous medication.
If there is recurrence or persistence of the urethritis, administration of 2 g metronidazole in an oral single dose may be a satisfactory solution for trichomoniasis.
According to the CDC, patients diagnosed with uncomplicated gonorrhea who are treated with any of the recommended or alternative regimens do not need a test of cure. Except patient with pharyngeal gonorrhea who is treated with an alternative regimen, in this case should return 14 days after treatment for a test-of-cure using either culture or NAAT. However, the authors recommend that, in women patients, a culture is made of endocervical material, 7–10 days after the end of the treatment period. The CDC guides that recent sex partners (i.e., persons having sexual contact with the infected patient within the 60 days preceding onset of symptoms or gonorrhea diagnosis) should be referred for evaluation, testing, and presumptive dual treatment.
Increased investment in research and development of new vaccines is key to halting the spread of genital herpes, gonorrhoea, chlamydia, syphilis, and trichomoniasis.
Condoms, when used consistently and correctly, can reduce the risk of transmission of gonorrhea and other STDs.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here