Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Autoimmune hemolytic anemia (AIHA) is a rare autoimmune disease caused by autoimmune-mediated destruction of red blood cells (RBCs) by autoantibodies with various properties and target specificities. Exact laboratory diagnosis may sometimes be difficult; therefore, experienced diagnostic reference centers play an important role. The disease can be primary (idiopathic) or caused by an underlying condition (secondary), including systemic autoimmune diseases, infections, primary immunodeficiencies, drugs, or neoplasms (mostly lymphomas). The clinical course of the disease as well as treatment decisions are influenced by the type of antibody involved. Currently, treatments for AIHA are still mainly based on experience and opinion as opposed to robust evidence and there is still no therapy licensed for AIHA. Several guidelines have been proposed. Recommendations for diagnosis and treatment by an international group of experts were recently published. Management of the disease still requires general hematologic skills as well as knowledge of diagnostic criteria and treatment options. In the last years, new promising treatment approaches have been developed.
The history of diagnostic and therapeutic progress in AIHA has been described by Dacie, one of the great pioneers in this field. Milestones were the discovery of the first RBC autoantibody (Donath–Landsteiner [DL] antibody) in 1904, the introduction of the Coombs test in 1945, the establishment of splenectomy as an effective treatment of AIHA in the 1950s, and the finding that rituximab was an effective treatment in the past decade. The diagnosis and treatment of patients with AIHA were reviewed by several authors.
Based on the characteristics and thermal amplitude of autoantibodies, AIHAs are usually classified as either warm (wAIHA) or cold (cAIHA). A low proportion of patients achieve spontaneous or treatment-induced, long-term remissions; overall mortality is relatively low and the prevalence of AIHA has been estimated as 17 in 100,000 in Denmark. The incidence of AIHA in children and teenagers is 0.2 to 1.0 per million per year. There is some evidence of a genetic predisposition and/or familial clustering of AIHA/Evans syndrome in children, but no clear genetic background has been identified for the majority of patients.
Primary AIHA and Evans syndrome are slightly more prevalent in adult females and in children. In secondary AIHA, the female-to-male ratio is very high in systemic lupus erythematosus (SLE), but close to 1 in chronic lymphocytic leukemia (CLL)-associated AIHA. The incidence of chronic cold agglutinin disease (CAD) is estimated to be approximately 1 to 2 per million per year with a female prevalence. Geographical differences have been suggested with a higher incidence of CAD in Northern climates, potentially explained by a higher number of symptomatic patients in these areas.
Hemolysis is initiated when an autoantibody binds to the one or several RBC membrane antigens and promotes antibody-dependent, cell-mediated cytotoxicity, and/or recruits and activates complement. Destruction of the RBC can occur directly in the circulation (intravascular hemolysis) and/or by removal of the cell by macrophages in the spleen, liver, or both (extravascular hemolysis) ( Fig. 47.1 ). Several immunoglobulin (Ig) subclasses can fix complement and activate the classical complement (Ct) pathway: IgG3 activates Ct more efficiently than does IgG1, whereas IgM, which is a potent Ct activator, is usually eluted ex vivo and therefore not found on RBC membrane by the direct antiglobulin test (DAT). Macrophages recognize opsonized erythrocytes via receptors specific for the Fc fragment of IgG, namely Fcγ receptors (FcγRs) and for C3d. RBCs coated with IgG or complement alone are destroyed in the spleen and liver, IgG-coated cells in the spleen, and IgM-coated cells in the liver. This has major implications for treatment, particularly for the effect of steroids and splenectomy.
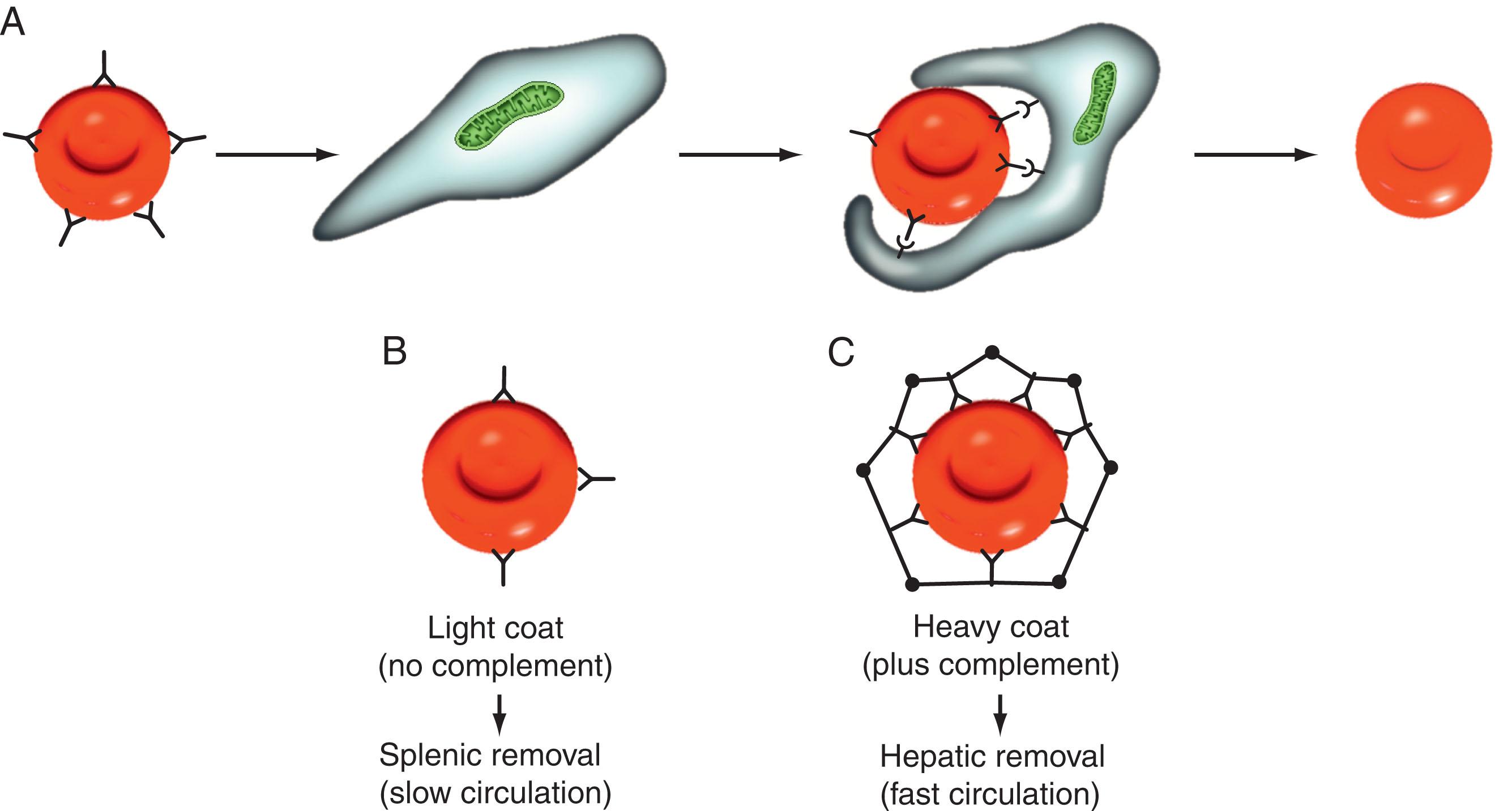
wAIHAs represent 60% to 80% of all AIHAs. The RBC antibodies in wAIHAs are mostly polyclonal IgG1 or IgG3, which are able to activate the complement system ( Table 47.1 ). The DAT in wAIHAs is positive either with IgG (37%) or IgG + C3d (43%). Rarely, the DAT is only positive with C3d (when the amount of IgG on the RBCs is very small or in case of “warm,” IgM autoantibody). Patients with IgG antibodies may have also IgA antibodies, but IgA antibodies without IgG antibodies are a very rare cause of wAIHAs. wAIHAs are often directed against Rh antigens, but also against other RBC’s membrane antigens (non-Rh–related autoantibodies) such as band 3 protein or glycophorin A. The antibodies fix complement and bind tightly to the RBCs at 37°C. Therefore, only a small amount of antibody is detectable in the serum. The antibody-coated RBCs are removed from the circulation by splenic (to a lesser degree also by hepatic) macrophages via FcγRIII receptors. IgG 3 and IgG 1 have the highest affinity for the Fc receptors of macrophages. Erythrocytes that are only partially phagocytosed by macrophages become spherocytes, which are removed in the splenic cords because of their rigid structure and can be easily detected on peripheral blood smear. Destruction of RBCs may also be caused by other mechanisms such as antibody-dependent cellular cytotoxicity as well as complement-dependent cytotoxicity when complement activation is involved.
| Immunoglobulin (Subclass) | Type of Antibody | Clonality | Specificity | Hemolysis | Predominant Site of Removal of Red Blood Cells | |
|---|---|---|---|---|---|---|
| wAIHAs | IgG (1–4) , IgA | Incomplete | Mostly polyclonal | Rh-antigens and non-Rh-antigens | Extravascular | Spleen (liver) |
| cAIHAs | IgM | Complete | Mostly clonal | Anti-i, -I T , -l, -Pr | Intravascular | Liver |
| Donath–Landsteiner antibody | IgG | — | Polyclonal | P antigen | Intravascular | — |
IgM wAIHAs are a very rare cause of AIHA. This type of AIHA can be suspected if RBC autoagglutination occurs at room temperature. The DAT result is positive with C3d alone (65%) or with IgG (24%), there are no detectable cold agglutinins (CA) in the serum. Using sensitive methods, IgM on the RBCs can be detected in 71%. Non-Hodgkin lymphoma (NHL) is the underlying disease in some of these cases. This AIHA is often life-threatening and refractory to steroids and splenectomy.
Cold antibodies in primary or secondary chronic forms of cAIHA (known as cold agglutinin disease or CAD) are usually monoclonal IgM. The IgM has two binding sites for C1q and fixes complement easily. The targets are polysaccharides (I, I T , I, or Pr antigens). The “i” antigen is a nonbranched polysaccharide in the cord blood and the “I” antigen is a similar but a branched molecule expressed in the RBCs of adults. Cold antibodies, more commonly known as “CAs,” bind to the RBCs at low temperatures and cause their lysis at temperatures above 22°C. The DAT is typically positive with C3d alone. When CAs are present at high titers, they may activate the complement system directly, produce a membrane attack complex, and produce intravascular hemolysis with hemoglobinuria. Usually complement-coated RBCs are sequestered by liver macrophages.
Some forms of transient cAIHA triggered by an infection may rarely occur, they can classically be associated with a Mycoplasma pneumoniae infection or yet with some viral infections (mostly EBV or CMV). The onset is usually abrupt and the degree of anemia may be severe with transfusion requirement, but the outcome is most often good within few weeks.
Lastly, paroxysmal cold hemoglobinuria (PCH) is a very rare form of AIHA caused by the DL antibody. This is a rare, usually polyclonal IgG cold antibody to P antigen (glycosphingolipid globoside), which binds to the RBCs at 4°C. The cells are lysed at higher temperatures. The DAT is positive with C3d, no CAs are present, and the diagnosis can only be ascertained by means of the DL test in a specialized lab. In this test, normal RBCs and patient and normal serum are incubated at 4°C. Agglutination occurs after warming to 37°C. The prominent clinical feature of PCH is a brisk, immediate but sometimes also delayed hemoglobinuria after cold exposure even in patients with low antibody titers. In the past, it has been associated with viral infections in children and secondary or tertiary syphilis in adults. Now, two types can be distinguished clinically : (1) an acute, severe form (often associated with hemoglobinuria) but self-limiting AIHA after (respiratory) infections in children, and (2) a rare, chronic AIHA in nonsyphilitic persons with various underlying conditions, including NHL. Patients with chronic PCH respond poorly to steroids and splenectomy.
A small number of patients have an AIHA mixed with a positive DAT for both IgG and C3d, indicating coexistence of warm IgG autoantibodies and high-titer CAs (titer >1/64). Mixed AIHAs have a severe course of disease and lower median hemoglobin (Hb) values (5.8 g/dL) that frequently require multiple therapy.
The term characterizes DAT-negative, IgA-driven, or warm-IgM forms. They represent a diagnostic challenge, resulting in delayed treatment.
Our knowledge about the etiology of AIHA is still limited. Factors that may play a role are antigen mimicry; immune deficiency; and, to a lesser extent, probably genetic factors. AIHA, similar to other autoimmune diseases, is a consequence of the loss of immunologic (self-) tolerance against antigens expressed on the erythrocyte surface. Production of RBC antibodies is a result of the interaction of T and B cells, as well as regulatory factors (e.g., T-regulatory cells, cytokines ). Disturbances of the Th1/2 T-cell subset balance with IL-10/IL-12 imbalance toward Th2 cells as well as the occurrence of clonal regulatory T cells specific for a RBC autoantigen have been described. Moreover, BAFF-dependent B-cell and plasma-cell activation plays a role with the possible emergence of long-lived autoreactive plasma cells.
This may be linked to the fact that AIHA does not only occur in immunocompetent individuals but frequently occurs in patients with acquired B or T-cell defects such as CLL, common variable immunodeficiency (CVID), HIV infection, or immunosuppressive therapy, particularly after stem-cell or solid-organ transplantation. Polymorphisms or altered expression of negative regulators of T-cell responses such as cytotoxic T lymphocyte antigen 4 (CTLA4) or interleukin-10 may also play a role. Mouse models (New Zealand black mice) have revealed an association of genetic loci with antierythrocyte antibody production or cold agglutinin escape tolerance after Mycoplasma infection.
Various target antigens have been described, with Rhesus polypeptides, glycophorin A, and erythrocyte band 3 being the most prominent in wAIHA. Cold reactive antibodies frequently target the I or i blood group-specific antigens. Events linked to the development of secondary AIHA by induction of cross-tolerance (molecular mimicry) are infections ( M. pneumoniae [I antigen target], parvovirus B19, herpes viruses), neoplastic diseases (paraneoplasia), and drugs by various mechanisms. Important differences exist in the pathogenesis of wAIHA and cAIHA. The pathogenesis of primary wAIHA is largely unknown. Secondary wAIHA is a complication of several congenital or acquired immune deficiencies. Both moderate (e.g., in CLL) and severe (HIV, post-transplant, congenital severe T-cell deficiencies) T-cell and humoral immune deficiency predispose to wAIHA, but no correlation has been established between the type and severity of immune deficiency and the risk of AIHA. One poorly understood phenomenon is the lack of a clear relationship between the presence of RBC antibodies and anemia. In many instances, no anemia is present despite a strongly positive DAT or high titers of cAIHAs. There is also only a poor correlation between antibody titers and severity of anemia. Another unexplained finding in secondary AIHA is the occurrence of both wAIHAs and cAIHAs in the same condition, for example, in lymphomas or infections.
Antibodies in primary AIHA are frequently polyreactive and polyclonal (no clonal B cells detected by polymerase chain reaction [PCR]). Antibodies in CAD are mostly produced by PCR-detectable, oligoclonal, or monoclonal B-cell populations. The nature of these antibodies has been extensively studied in CAD. However, in only a few cases has it been established that the RBC antibody is clonal. In most reports, clonality of RBC antibodies was assumed if the patient had a paraproteinemia.
B-cell neoplasms, expressing IgMκ antibodies, directed against RBC antigens have few somatic mutations, which seem to be fairly restricted to certain Igheavy and light-chain families (VH4–34, VκIV). Moreover, a VH4–34 CLL confounding subclone was shown to arise from a pre-existing CAD-producing, B-cell population. The restricted clonality of CAD-producing B cells is further corroborated by the detection of clonal Ig rearrangements and recurrent chromosomal aberrations (trisomy 3). CLL cells may also drive AIHA by presenting the autoantigen (e.g., erythrocyte protein band 3) to T cells.
The symptoms of AIHA depend on the type of antibody, the mode of onset, and the severity of anemia. In patients with wAIHA, the onset is mostly gradual or subacute and the symptoms (i.e., tiredness, reduction of physical activity, jaundice, and shortness of breath in elderly patients) are attributable only to anemia. However, patients with postinfectious, drug-induced AIHA or patients with DL or Pr antibodies often present with acute severe symptoms such as malaise, fever, jaundice, abdominal pain, shortness of breath, and hemoglobinuria. The course in such patients may be fulminant and even fatal. Patients with chronic cAIHA (CAD) often have a rather indolent course. Symptoms suggestive of cAIHA are cold sensitivity, cold-dependent acrocyanosis, acral numbness, and rarely livedo reticularis. Anemia worsens after cold exposure or after conditions associated with an acute phase reaction such as infections.
During clinical examination, a subicterus may be seen. Lymphadenopathy, important splenomegaly, or any organomegaly is rare in patients with primary AIHA. Its presence suggests secondary AIHA.
Patients with wAIHA are at an increased risk of venous thromboembolism, sometimes associated with a lupus anticoagulant (LA). Older patients with AIHA are at an increased risk of cardiovascular complications, which may also be partly caused by the treatment.
AIHA is essentially a laboratory diagnosis. The diagnostic pathway of AIHA should proceed in a stepwise fashion answering the following questions.
It is of utmost importance to differentiate between various types of autoimmune hemolytic anemia (AIHA). A step-wise approach helps in making the right decisions:
Question 1:Hemolytic anemia? The basic features of hemolytic anemia are low haptoglobin levels, elevated indirect bilirubin, and elevated lactate dehydrogenase. Reticulocytosis is a common feature (≈80% of the cases) of AIHA reflecting the increase of erythropoiesis in response to accelerated destruction of red blood cells (RBCs).
Question 2:Autoimmune hemolytic anemia? A direct antiglobulin test (DAT) is initially performed with a polyspecific antibody to detect IgG or complement C3d bound to RBCs. If the DAT result is positive, the diagnosis of AIHA is established in the absence of any other cause of hemolysis and/or any recent transfusion. In parallel, the peripheral blood smear is very helpful because it may show the presence of spherocytes (wAIHA) or agglutinates (cAIHA) and show the absence of schizocytes.
Question 3:Warm or cold autoimmune hemolytic anemia? The DAT is further elaborated with monospecific antibodies to IgG and complement (C3d). If the DAT result is positive with IgG alone or with IgG + C3d, the AIHA is most probably caused by a warm antibody (wAIHA). If the DAT is positive with C3d only, the AIHA is most probably caused by a cold antibody (cAIHA).
Question 4:Primary or secondary AIHA? More than half of wAIHAs are secondary to underlying diseases. Secondary AIHA should be suspected in patients with additional findings or who are refractory to initial steroid treatment. In this case, the underlying disease has to be diagnosed (e.g., by serologic tests, computed tomography (CT) scan, or bone marrow biopsy).
The first step is to establish the diagnosis of hemolytic anemia (see box on Four Important Questions for the Diagnosis and Management of Autoimmune Hemolytic Anemia ). This diagnosis is established by the presence of the following pentad of findings: normocytic or macrocytic anemia (male Hb <13.0 to 14.0 g/dL; female <12.0 g/dL), reticulocytosis (corrected reticulocyte count >2% or absolute reticulocyte count >100,000/μL to 120,000/μL), low haptoglobin, elevated lactate dehydrogenase (LDH), and elevated unconjugated (indirect) bilirubin. Haptoglobin is an α2-globulin that binds Hb. This Hb–haptoglobin complex is degraded in the liver. Hemopexin is another plasma protein with a very high binding affinity to Hb. It scavenges heme released from RBCs and protects the organisms from the adverse effects of circulating Hb. The determination of hemopexin is not essential for the diagnosis of AIHA. Indirect bilirubin is usually not more than 5 mg/dL except in associated liver disease (Epstein-Barr [EBV]-associated AIHA). Additional findings are increased urobilinogen in the urine and spherocytes in the blood smear ( Fig. 47.2 ). Leukoerythroblastosis occurs only in peracute AIHA, but microangiopathic hemolytic anemia should always be suspected in such cases. Bone marrow examination is usually not necessary except in patients in whom secondary AIHA, in particular lymphoma, is suspected. RBC survival is shortened, but its measurement with radioisotopes has no diagnostic value, not even for the prediction of the efficacy of splenectomy.
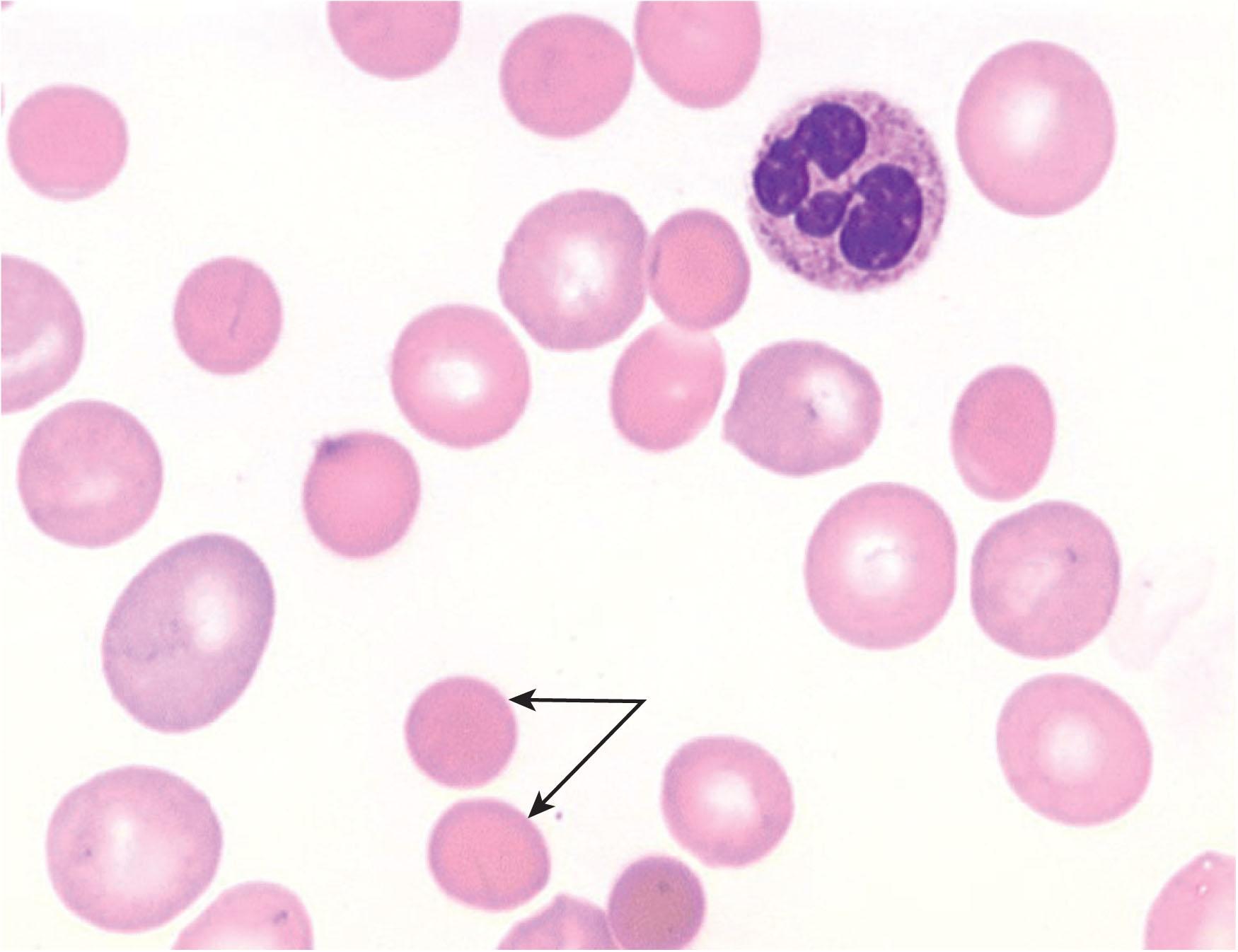
Among methodologic diagnostic problems, reticulocyte counting is the biggest because in many laboratories low-precision microscopic counts are still performed. Automatic-flow cytometric methods are more precise, reliable, and convenient. With flow cytometry, the number of highly fluorescent reticulocytes can also be measured. Falsely very high mean corpuscular volume (MCV) and mean corpuscular Hb concentration occur in some cases of cAIHA because RBC counts are falsely low because of agglutination of RBC at room temperature ( Fig. 47.3 ). If a cAIHA is suspected, blood samples should be sent as quickly as possible to the laboratory in warmed containers.
All of the findings of the pentad are not always present. Reticulocytosis is often (in ≈20%) not present at the onset of AIHA. This is mostly because of a delayed initial bone marrow response of erythropoiesis. After 1 week, most of these patients have reticulocytosis. In other patients (particularly in secondary cases), absence of reticulocytosis may be attributable to impairment of erythropoiesis caused by bone marrow infiltration, vitamin B 9 or B 12 deficiency or blunted erythropoiesis caused by an acute-phase reaction. If the reticulocyte count is very low, pure RBC aplasia (PRCA), either immune mediated or induced by a parvovirus (or HHV6) infection, should be suspected. Haptoglobin may be falsely normal or even slightly increased, particularly in patients with malignant or immune diseases, because haptoglobin is an acute-phase protein. Haptoglobin may be falsely low in patients with a haplotype H 0 H 0 and in patients with severe liver disease. Both increased bilirubin and elevated LDH have a limited specificity for AIHA.
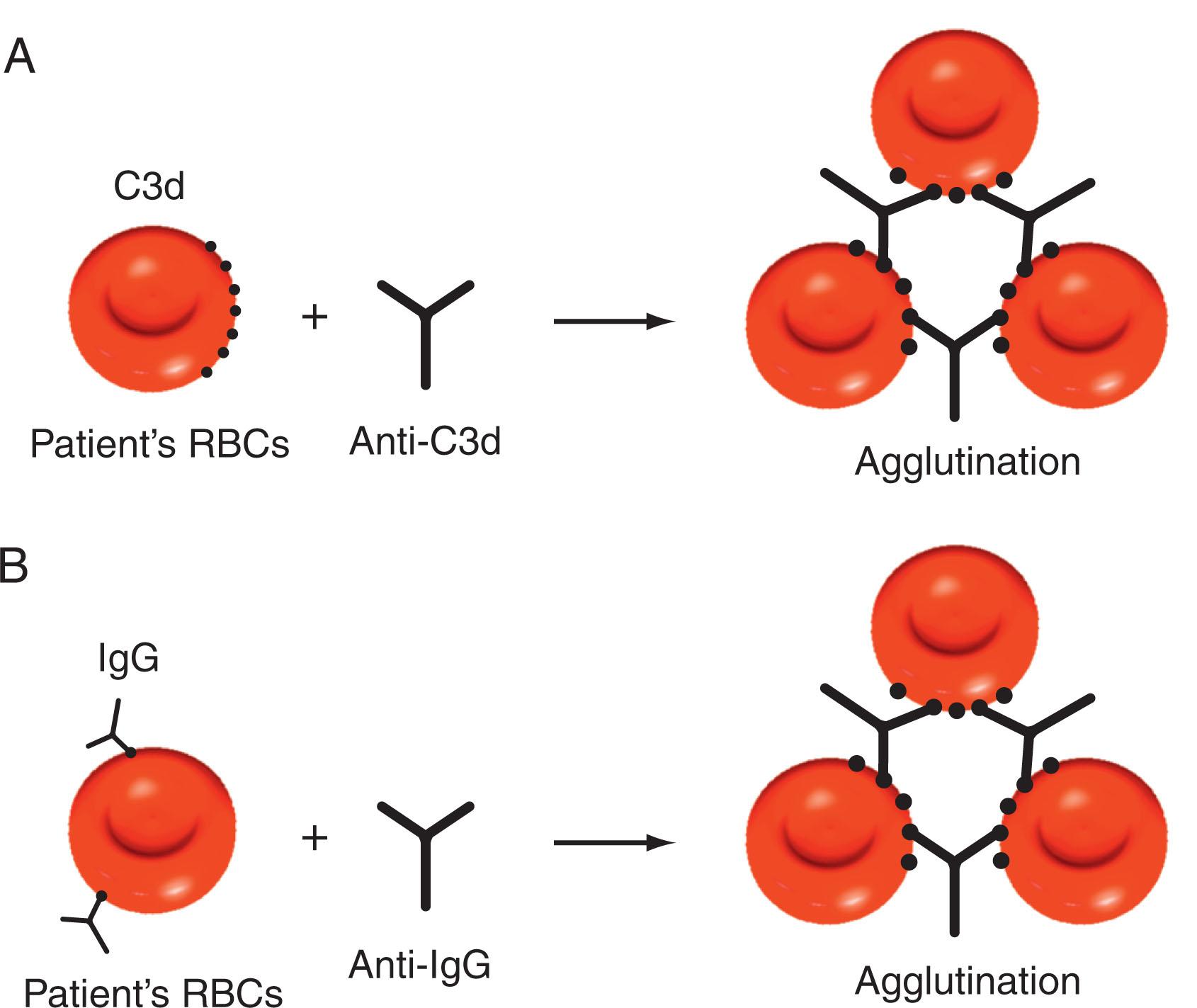
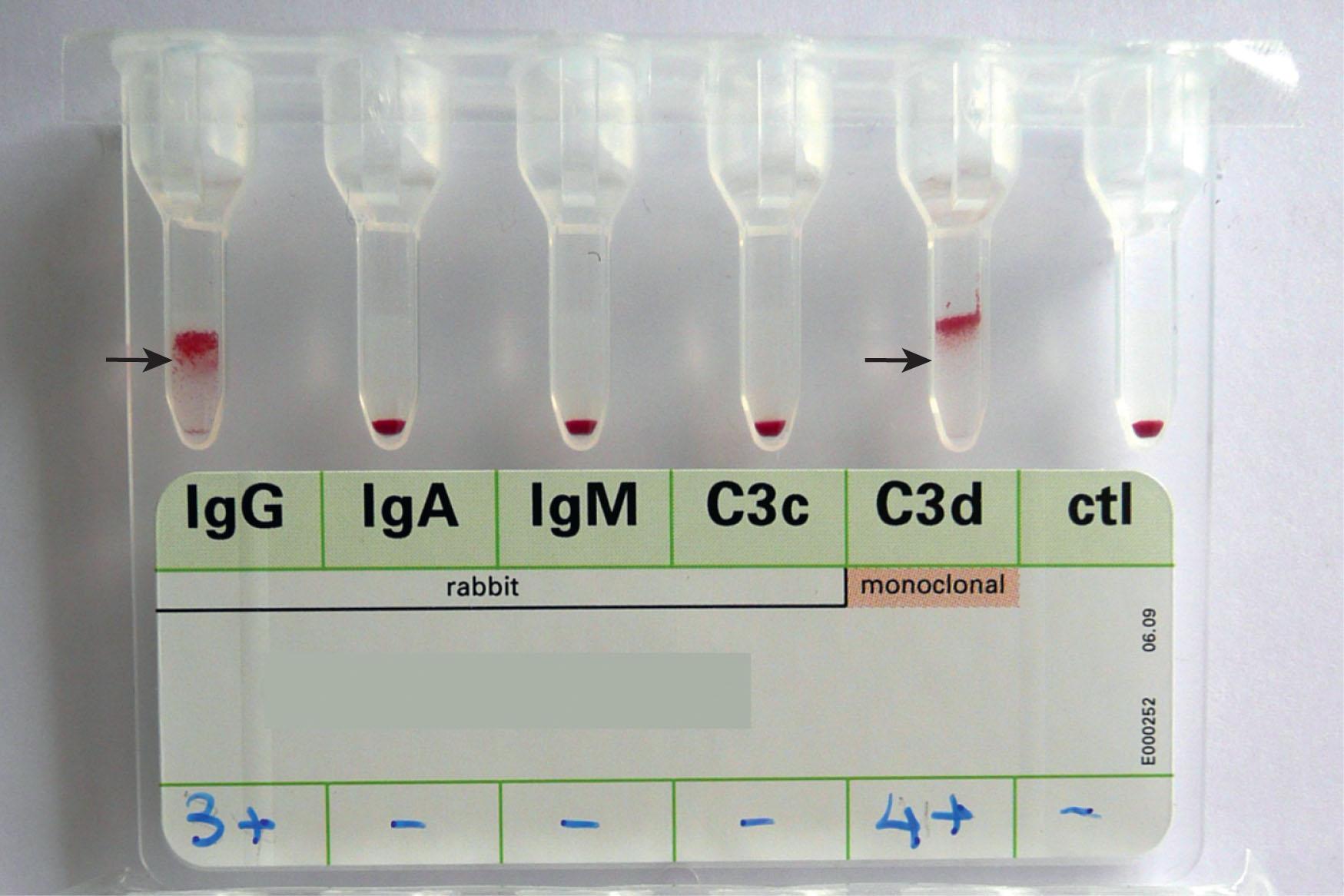
The next step is to find out whether the hemolytic anemia is an AIHA. This is best done by the DAT ( Fig. 47.4 ). In this test, washed RBCs of the patient (obtained from an ethylenediaminetetraacetic acid [EDTA] blood sample) are incubated in a tube with a polyspecific antibody to IgG and complement (C3d). If the RBCs agglutinate, the test result is positive. In many laboratories, the tube test has been replaced by the tube-gel test, which is easier to perform, more reliable, and probably more sensitive ( Fig. 47.5 ). In the indirect antiglobulin test (IAT), patient plasma or serum is incubated with test RBCs and (after washing) RBC-bound IgG is detected with the DAT. IAT is usually not required for the diagnosis of AIHA except when a drug-dependent antibody is suspected. For the differentiation of drug-dependent antibodies and autoantibodies, an acid eluate of the patient’s RBCs should be made and tested in the IAT. If the IAT result is positive, the patient has autoantibodies. The severity of AIHA does not correlate with the strength of the DAT, but rather with the Ig subclass of the antibody (IgG 1 or IgG 3 ). The result of the DAT is not a reliable marker of treatment success because patients with a complete hematologic remission may remain DAT positive, and DAT positivity or negativity has only limited value to predict the duration of hematologic remission.
If the conventional DAT test result is negative, hemolytic anemia is defined as DAT-negative. This implies that positive DAT with anti-IgA has been excluded as well as other causes or hereditary of acquired hemolytic anemia—in particular hereditary spherocytosis and paroxysmal nocturnal hemoglobinuria. However, AIHA cannot be definitely excluded because about 5% (2% to 11%) of AIHA patients are DAT negative. If AIHA is suspected for clinical grounds despite a negative DAT result, more sensitive quantitative tests are required to determine the amount of IgG on the RBCs. The threshold of positivity of the conventional DAT is 100 to 200 IgG molecules per RBC, but in some AIHA patients the RBC IgG is less than this amount. In about one-third of DAT-negative cases, one of the more sensitive test results (e.g., immunoradiometric tests) will be positive. However, the relationship between the amount of RBC IgG and hemolysis is not clear cut, and there is no “hemolysis threshold.” The reasons for these discrepancies between the in vitro and in vivo activity of RBC antibodies are largely unknown. Differences in macrophage activity may be one possible explanation. A search for antibodies in the RBC eluate in which antibodies are more concentrated is also useful. IgA antibodies are rare and sometimes not included in the analysis. Finally, there is the possibility of low-affinity antibodies. Such antibodies are washed out when the washes are made with 37°C saline. A high rate of DAT-negative AIHA has been observed in AIHA induced by nucleoside analogues, but also in other secondary AIHA.
The DAT result is positive in 1 in 10,000 to 3 in 10,000 normal persons and 10% of hospital patients without anemia or signs of hemolysis.
In a further step, the DAT is carried out with monospecific antibodies to IgG and complement (C3d) to find out whether a warm or cold antibody is the cause of hemolysis. If the DAT result is positive with IgG alone or with IgG plus C3d, the AIHA is most probably a wAIHA. If the DAT result is positive with only C3d, the AIHA is most probably a cAIHA. The differentiation between wAIHAs and cAIHAs is extremely important for the choice of treatment.
Some special diagnostic problems exist when it comes to cAIHAs. If cAIHA is suspected, it must be taken care that the blood sent to the laboratory is kept at 37°C to get reliable results. Patients with only RBC C3d may (rarely) have wAIHAs when the amount of RBC IgG is very small. In patients with C3d positivity, the cold agglutinin titer should be determined. If it is equal or greater than 1:64 the diagnosis of a CAD is established. There is no consensual threshold titer that separates normal from abnormal. If the titer is less than 1:64, the thermal amplitude of the antibody must be determined. If the thermal amplitude is above 22°C, the diagnosis is CAD. Mixed type AIHA is rare. Frequently used criteria are a positive IgG DAT result and a positive eluate result plus a C3d-positive DAT result and the presence of CAs with a thermal amplitude of greater than 30°C or high titer Cas (>1:40). Many published cases of mixed-type antibodies do not fulfill these criteria.
In the last diagnostic step, it must be determined whether the AIHA is primary or a complication of an underlying disease (secondary). About half of cases of AIHA (or probably even more) are secondary. The main causes are systemic immune diseases and malignancies and mostly B-cell lymphomas. Other underlying conditions are infections, primary immunodeficiencies, drugs, transplantation, and congenital defects. The decision regarding which diagnostic procedures should be used for this purpose depends mainly on the type of AIHA (wAIHAs or cAIHAs) and should include history, physical examination, laboratory tests, and imaging procedures if indicated. In children and younger patients with wAIHA, evidence for an infection should be sought. A list of all recent medication should be made. A history of weight loss, fever, or poor general condition, and arthritis points to a malignancy or systemic immune disease as the underlying condition. Palpable lymphadenopathy and important splenomegaly do not belong to the usual clinical picture of primary wAIHA. In this case, lymphoma (particularly splenic marginal zone lymphoma [SMZL]) should be suspected. Laboratory tests should include acute-phase proteins, LDH, quantitative determination of Igs, antinuclear antibodies, and other tests guided by the clinical history. A bone marrow examination is not obligatory except when lymphoma is suspected. Abdominal ultrasonography or a CT scan is reasonable in all cases to look for a disproportionate splenomegaly, the remote (but important) possibility of an ovarian teratoma (in women), another solid tumor, lymphadenopathy, or solitary extranodal lymphomas. An activated partial thromboplastin time with a lupus-sensitive reagent may reveal an LA. Fluorescence-activated cell sorting or PCR for the detection of monotypic/monoclonal lymphocytes may be done, but the clinical usefulness of such tests to guide treatment decisions is uncertain.
In cAIHA, a history of a febrile illness should prompt a thoracic radiography, and if results are positive, a serologic test for mycoplasma pneumoniae is required. The quantitative determination of serum Igs and a search for a clonal Ig by immune fixation are important. If immune fixation findings are positive, a search for lymphoma is necessary, which may include bone marrow biopsy even when there is no lymphadenopathy. In addition to classical CAD, CAs occurring in association with other cancers, aggressive lymphomas, or infection should be termed cold agglutinin syndrome .
Other tests, including blood glucose, Hba 1c , renal and hepatic function tests, HIV serology, hepatitis B antigen, and exclusion of latent tuberculosis are necessary to avoid complications of steroids (in wAIHAs) or rituximab (in cAIHAs and wAIHAs).
Evans syndrome is the simultaneous or sequential combination of wAIHAs with autoimmune thrombocytopenia (ITP) ± autoimmune neutropenia, a typical but rare association. Platelet antibodies are usually directed against glycoprotein IIB/IIIA. Autoimmune neutropenia occurs in 25% of patients. There is no sex predilection; about half of the cases are secondary. Evans syndrome is relatively more common in patients with SLE, antiphospholipid antibodies (APAs), CVID, and autoimmune lymphoproliferative syndrome (ALPS). A search for an ALPS is mandatory in younger patients with Evans syndrome. In roughly 50% of the cases, AIHA and ITP occur simultaneously; in the others disease starts with either ITP or AIHA. There may be an interval of several years between the onset of AIHA and ITP.
wAIHA, cAIHA, or a positive DAT result without anemia may be associated with PRCA. PRCA may be either immune mediated such as in T-cell neoplasms (particularly T-cell large granulocytic leukemia or thymoma) or may be caused by an infection with parvovirus B19. Patients with parvovirus-associated AIHA often present with PRCA.
AIHA is definitely associated with APAs and LA. In one single-center, prospective study, LA was found in 30% predominantly idiopathic AIHA. AIHA (4%) and Evans syndrome (10%) are frequent in patients with APAs. It is well established that patients with AIHA have a significantly (2.8-fold to 3.8-fold) elevated risk of venous thromboembolism, especially during the active phases of the disease. It is likely, but not proven, that patients with AIHA associated with LA are at a higher risk.
In lymphomas, some cases of AIHA are associated with C1-esterase inhibitor deficiency and mixed cryoglobulinemia.
The temporal relationship of AIHA to an underlying condition is complex. AIHA antedates the diagnosis of malignancy in many cases—including NHL—sometimes for years. In population-based studies, clonal B cells have been detected in some patients with seemingly “idiopathic,” AIHA. In most instances, AIHA occurs concurrently with the malignancy. In some other cases, AIHA occurred only at the recurrence and rarely in complete remission (CR) after successful treatment. In CLL, AIHA occurs preferentially in a late and active phase of the disease. The patients have poor prognostic factors and often have been treated with various agents.
In immune diseases, particularly SLE, AIHA is a complication of the early phase of the disease. Infection-related AIHA occurs shortly after the onset of symptoms, except in HIV infection in which AIHA is a complication in the late advanced stage of the disease.
In CIVD, AIHA or Evans syndrome preceded or revealed CVID in more than half of the cases.
It is an interesting phenomenon that in underlying diseases associated with AIHA, all serologic types of AIHA may occur, but usually one serologic type (wAIHA, cAIHA, or DL antibody) prevails. The only exception is ovarian teratoma, which is only associated with wAIHA.
The prevalence of AIHA in patients with SLE is 7.5% (average of seven studies; range: 5.2% to 12.5%). AIHA may occur at any time during the course of SLE, but two-thirds of cases of AIHA occur at diagnosis or soon thereafter. Almost half of the patients are already taking steroids. Most patients are women and have wAIHA. Evans syndrome is common. Compared with SLE patients without AIHA, those with AIHA are younger; have a higher prevalence of thrombocytopenia, APAs, renal disease, serositis, and central nervous system involvement; and have a higher risk of venous thrombosis.
The prevalence of AIHA in primary antiphospholipid syndrome (PAPS) is about 10%. AIHA precedes PAPS in 25% of cases, but in others occurred after a median time of 4.4 years after the diagnosis of PAPS. Patients with PAPS and AIHA have an increased risk for the development of SLE.
In the only larger study, the prevalence of AIHA in ulcerative colitis was 1.7%. The mean time from diagnosis of colitis to AIHA was 17 months. Three-quarters of these patients had total colitis. AIHA may also be associated with Crohn disease, but the prevalence is lower than in ulcerative colitis.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here