Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Since the early 1990s, percutaneous peripheral atherectomy has provided an ancillary approach to the treatment of atherosclerotic occlusive disease beyond angioplasty and stenting. A variety of technologies have been developed to debulk atherosclerotic lesions, including directional excisional, excimer laser, orbital ablation, and rotational atherectomy. These technologies are designed to treat a variety of lesions from heavily calcified stenoses to soft thrombus-containing occlusions. By removing atherosclerotic plaque, atherectomy provides luminal gain to diseased vessels rather than simply dilating the existing lumen and leaving disease in situ. This can be achieved with a technique that leaves no intraluminal foreign body and facilitates reinterventions if necessary. Furthermore, atherectomy may be used to treat lesions involving joint spaces that are under continuous dynamic stress forces, where stents may be at increased risk of fracture and subsequent failure. The theoretical advantages of atherectomy are apparent, but the data to support its use have been mixed and of poor quality to date. There are a number of commercially available atherectomy devices approved by the US Food and Drug Administration (FDA). Atherectomy devices vary in their mechanism of action and include laser, orbital, rotational, and directional means of removing atherosclerotic plaque. This chapter describes an overview of the clinical data for atherectomy and the indications, ideal lesions, outcomes, and complications are presented.
Percutaneous atherectomy as an endovascular modality was initially applied in the coronary bed. However, despite the theoretical advantages, several studies showed unfavorable long-term results compared to angioplasty. This same technology was subsequently applied to the first generation of peripheral atherectomy devices, including the Simpson AeroCath (Guidant, Santa Clara, California) and the Auth Rotablator (Boston Scientific, Quincy, Massachusetts). Despite high initial technical success rates of 90%, the first-generation atherectomy devices were associated with poor intermediate and long-term patency rates. Subsequent advances have led to the current generation of atherectomy devices, which are now being applied to treat lesions in both the femoropopliteal and infrapopliteal segments.
The data supporting atherectomy as an adjunct to angioplasty and stenting have been mixed. A 2014 Cochrane Review of atherectomy compared to angioplasty alone was only able to incorporate four studies, including one study performed in 1995 with a first-generation extraction catheter and another performed in 1996 with a cohort of 36 patients. Also included was a more recent study of 58 patients undergoing directional atherectomy versus angioplasty alone that concluded no difference at one year, but fewer bailout stents placed in the atherectomy group, at the cost of higher rates of macroembolization. Orbital atherectomy, by the same author, faired only slightly better in calcified lesions. They concluded that there was no benefit to atherectomy over angioplasty alone. There are a number of retrospective studies that show significant benefit in patients treated with atherectomy, with 1-year primary patency ranging from 60% to 83%, limb salvage of 79% to 95% at 2 years in critical limb ischemia (CLI), complications requiring intervention in 0% to 7% of cases, and target lesion revascularization in up to 28% at 2 years. Data for infrapopliteal intervention using atherectomy are also mixed. One retrospective study comparing 333 percutaneous tibial angioplasty (PTA) to 79 atherectomy interventions (33 laser, 13 directional, and 33 orbital) showed no benefit to PTA with atherectomy compared to PTA alone, but with no difference in complication rates. Another prospective multicenter trial of directional atherectomy demonstrated 90% primary patency of infrapopliteal interventions in claudicants, and 78% in CLI, limb salvage of 95%, and a 3.8% rate of distal embolization. This core-lab adjudicated data compare favorably to primary stent trials. Peripheral interventions in claudicants and nondiabetic patients compare favorably to those who have CLI and diabetes, and the same is true for atherectomy.
The Hawk family of atherectomy catheters was initially approved for peripheral arterial use in 2003 by the FDA ( Fig. 18.1 ). The SilverHawk catheter debulks lesions without the use of a balloon and instead relies on self-apposition against plaque through a hinged system at the distal end of the catheter. The device consists of a detachable, battery-powered motor that attaches to a 0.014-inch monorail atherectomy catheter. The tip of the catheter contains a rotating blade and a plaque collection chamber. The carbide cutting blade rotates at 8000 rpm when activated. This blade has a concave design that shaves the plaque and then packs it into the nosecone storage compartment. The operator places the tip of the catheter just proximal to the target lesion, activates the blade, and then slowly advances the tip of the catheter through the entire length of the lesion, periodically emptying the nosecone ( Fig. 18.2 ). This process is repeated until an adequate flow channel is achieved. The tip of the catheter may be rotated 360 degrees and thus, plaque excision may be carried out in all four quadrants of the lumen. There is a single (SilverHawk) and double (HawkOne, TurboHawk) jog in the catheter design, which aids in arterial wall apposition. Once the nosecone collection unit is full, the entire catheter must be removed prior to reinsertion and additional passages.
| TurboHawk Plaque Excision System | CVX-300 Excimer Laser | Diamondback 360 Orbital Atherectomy System | Jetstream Atherectomy System | |
|---|---|---|---|---|
| Manufacturer | Medtronic (Minneapolis, Minnesota) | Spectranetics (Colorado Springs, Colorado) | Cardiovascular Systems Inc. (St. Paul, Minnesota) | Boston Scientific (Marlborough, Massachusetts) |
| FDA approved | Yes | Yes | Yes | Yes |
| Mechanism | Directional blade plaque excision | Ultraviolet light plaque dissolution | Centrifugal force plaque sanding | Rotational blade plaque excision and suction |
| Catheter tip size | 1.9–2.7 mm | 0.9–2.5 mm | 1.25–2.25 mm | 1.6–2.4 mm |
| Sheath size | 5–8 French | 4–8 French | 4–6 French | 7 French |
| Guidewire | 0.014 inch | 0.014, 0.018, and 0.035 inch | 0.014 inch | 0.014 inch |
| Lumen treatment range | 3–7 mm | 1.4 to >3.8 mm | 2 to >5 mm | 2.5 to >5 mm |

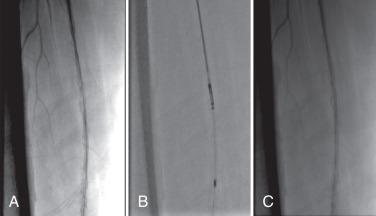
There are several different catheter sizes available to treat target vessel sizes ranging from 2 to 7 mm. All of these require a sheath ranging in size from 5 to 8 French, are introduced over a 0.014-inch guidewire, and have a crossing profile of 1.9 to 2.7 mm. Access may be achieved via a contralateral common femoral arterial puncture or an antegrade approach. The use of a filter to protect against distal embolization is recommended in calcified lesions. The catheter may be used in the flow channel or in a subintimal plane ( Fig. 18.3 ). The TurboHawk device improves on the SilverHawk with a more efficient cutter, more robust driveshaft, and dual jog catheter for wall apposition. The HawkOne device improves the crossing profile, simplifies cleaning, and is more effective in calcium. It is approved for vessels 3.5 to 7.0 mm and is 7 French sheath compatible.

There has been one small randomized trial of SilverHawk atherectomy versus angioplasty alone. A two-center prospective randomized trial enrolled 29 patients for atherectomy and adjunctive PTA versus 29 patients with PTA alone. The study found no significant differences in freedom from target lesion revascularization (TLR) between the two groups (89% vs. 83%). There was one clinically significant embolization in the atherectomy arm, requiring intervention at the time of the procedure with no sequelae. Of note, bailout stent rates in the plain old balloon angioplasty (POBA) were 62.1% per patient versus 27.6% in the atherectomy arm. Importantly, this small study excluded lesions greater than 10 cm or heavily calcified lesions, which POBA has traditionally failed.
There have been several reports demonstrating the effectiveness of directional atherectomy for the treatment of atherosclerotic lesions in the femoropopliteal and the infrapopliteal segments. The recent DEFINITIVE LE is a multicenter prospective industry-sponsored database that enrolled 800 patients looking at primary endpoints of 12-month patency and freedom from amputation. The primary patency, defined as peak systolic velocity ratio (PSVR) less than 2.4 by core lab adjudication, was 78% in claudicants and 71% in CLI patients, with 95% rate of limb salvage. The rate of clinically significant embolization was 1.2% to 3.0%, dissection 1.3% to 2.0%, and perforation 1.5% to 5.0%. The bailout stent rate was 3%. Zeller et al. reported 71 lesions treated in 52 patients, with an average lesion length of 48 ± 64 mm. Forty-two percent of these were primary stenoses, 38% were native vessel restenosis, and 20% were in-stent restenosis. The latter was performed outside of the manufacturer's instructions for use. Adjunctive angioplasty was used in 58% of these procedures, whereas stenting was used in 6%. Primary patency rates at 6 months were 80% for primary lesions, 63% for postangioplasty lesions, and 71% for in-stent restenoses. Zeller et al. subsequently reported longer-term data of 131 lesions in 84 patients with 12-month primary patency rates (defined as < 50% restenoses on ultrasound) of 84% for de novo lesions, 54% for native vessel restenoses, and 54% for in-stent restenoses. At 18 months, these fell to 73%, 42%, and 49%, respectively; however, secondary patency rates were 89%, 67%, and 79%.
The largest outcome data of the SilverHawk atherectomy catheter is the nonrandomized, manufacturer-sponsored TALON registry (Treating Peripherals With SilverHawk: Outcomes Collection), which involved 19 centers in the United States and collected data on 1258 lesions treated in 601 patients. Mean lesion length was 62.5 ± 68.5 mm above the knee and 33.4 ± 42.7 mm below the knee. Procedural success was 97.6% with less than 50% residual stenosis achieved in 94.7% of lesions. Adjunctive angioplasty was used in 21.7% of cases and stenting in 6.3% of cases. Six-month and 12-month freedoms from target lesion revascularization were 90% and 80%, respectively. Predictors of target lesion revascularization included a history of myocardial infarction or coronary revascularization and increasing Rutherford classification.
Recent data from a prospectively maintained database of 559 lesions treated in 255 patients included 228 in the superficial femoral artery (SFA; 106 occlusions), 176 in the popliteal artery (84 occlusions), and 229 in the infrapopliteal arteries (130 occlusions). Eighteen-month primary and secondary patency rates for all lesions were 45.9% ± 3.4 and 80.3% ± 2.5, respectively, with reported 18-month primary and secondary patency rates for claudicants of 59.2% ± 4.9 and 88.1% ± 3.3 and for patients with CLI of 34.3% ± 4.5 and 73.6% ± 3.6. Overall limb salvage was 93.1%.
The use of the SilverHawk atherectomy catheter specifically for the treatment of CLI has also been reported. Kandzari et al. reported the results of 160 lesions in 74 limbs ranging from the external iliac to the dorsalis pedis in patients with Rutherford class 5 and 6 disease. Mean above-knee lesion length was 74 ± 88 mm. Technical success was achieved in 99% of patients, with 17% requiring adjunctive angioplasty and/or stenting. The primary endpoint evaluated was a composite of major adverse events, including death, myocardial infarction, unplanned amputation, or repeat target vessel revascularization. At 6 months, 23% of patients met this endpoint. Amputations that were less extensive than initially planned or avoided completely occurred in 93% of patients at 30 days and 82% at 6 months. Keeling et al. also reported on the use of the SilverHawk atherectomy catheter for the treatment of both claudicants and patients with CLI. The technical success was 87.1% with a 1-year primary patency rate of 61.7%. Restenosis was higher in patients with TASC C or D lesions compared to those with TASC A or B lesions.
Zeller et al. reported additional data on the use of the SilverHawk atherectomy catheter for infrapopliteal lesions alone on 52 lesions in 33 patients. Atherectomy was used alone in 71%. Restenosis (>70% on ultrasound) was observed in 14% of lesions at 3 months and 22% at 6 months, however the cumulative patency rate was 94.1% at 6 months.
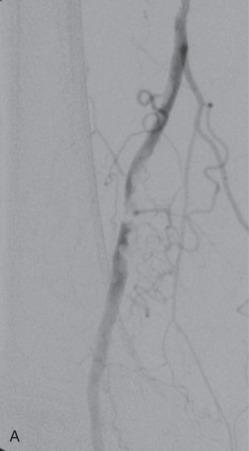
The primary complications associated with this device include perforation and distal embolization. Using the first-generation device, Suri et al. reported a 100% rate of embolic debris in 13 lesions treated with the SilverHawk atherectomy catheter with the concomitant use of a FilterWire (Boston Scientific, Natick, Massachusetts). This embolic debris ranged in size from 0.5 to 10 mm, and, in one patient, led to vessel occlusion that resolved with removal of the filter. Lam et al. also detected emboli during use of the SilverHawk atherectomy catheter using simultaneous Doppler monitoring. Of note, in this study, emboli were detected during the period between passes of the catheter, indicating that debris may shower from the disrupted intimal surface. However, no patient developed any clinically significant sequelae from these emboli.
In more recent studies, the clinically significant embolization rates were significantly lower, particularly in conjunction with an embolic protection device.
The Hawk family of atherectomy catheters is indicated for peripheral arterial atherectomy. It is not intended for coronary, carotid, or aortoiliac use. Each catheter has indicated vessel diameters (L 3.5-7, S 2.0-4.0) and cutter blades designed for calcium or soft lesions. In addition, there are nosecones and packing devices designed to more effectively capture debris and shorten treatment time. For example, a long calcified SFA lesion would call for a large device and a cutting blade with a long packer (LX-C). A tibial artery with a soft lesion would be better suited to a small device with a standard tip (SS+). This provides flexibility in treating a variety of lower extremity lesions. The Hawk devices are best suited to long segment, moderately calcified lesions, and are most safely used in conjunction with distal embolic protection devices. These devices can effectively treat dissection, soft or calcified lesions, and in-stent restenosis. It is not indicated in thrombus. They can be used in chronic total occlusion (CTO) lesions and subintimal planes, due to their directional cutting capability.
The Diamondback 360 Orbital Atherectomy System uses orbiting action to remove plaque and increases lumen diameter by increasing the orbital speed (80,000 to 200,000 rpm). An eccentrically mounted diamond-coated crown rotates at high speed at the end of the catheter to sand away plaque as the crown is slowly advanced through the target lesion. As crown rotation increases, centrifugal force presses the crown against the lesion to effect plaque removal, while the less diseased, more elastic arterial wall flexes away from the crown, minimizing the risk of vessel trauma ( Fig. 18.4 ). It is thought that the “sanding” of lesions creates particles that are too small to cause clinically significant embolization and can be reabsorbed through the reticuloendothelial system and thus the use of embolization protection filters is not needed. This technique emphasizes “plaque modification,” that is, emphasizing more effective balloon angioplasty by disrupting the calcium bed over luminal gain. The crown is positioned at the proximal portion of the target lesion and slowly advanced. This crown is manufactured in sizes of 1.25, 1.50, and 2.00 mm in solid micro, classic and solid configurations, to allow for final lumen diameters ranging from 1.25 to 3.50 mm based on the rotational speed. Micro crowns are used in the tibial vessels, and solid or classic crown is used in SFA/popliteal disease. This device is placed over a 0.014-inch guidewire and requires a 6 or 7 French sheath for access depending on the device size. It is used in conjunction with a lubricant ViperSlide, an emulsion composed of soybean oil, egg yolk phospholipids, glycerin, and water. Allergy to egg is a contraindication for use.
The data regarding orbital atherectomy in the peripheral system are scant and of poor quality. A number of recent trials have evaluated the Diamondback orbital atherectomy system. A small randomized multicenter study evaluated 1-year outcomes in 50 patients with calcified lesions and CLI comparing Diamondback orbital atherectomy with angioplasty to POBA. Bailout stenting occurred in 6% of atherectomy and 14% of POBA patients (not significant). Freedom from TLR in the atherectomy group was 93% versus 80% in POBA (not significant) at 1 year. In the industry sponsored OASIS (Orbital Atherectomy System Investigational Study) trial, a prospective, multicenter database enrolled 124 patients with 201 lesions. Fifty-one percent of these lesions were reported to be noncalcified and 85% were infrapopliteal. This study demonstrated an acute debulking rate, as measured angiographically, of 62%. Device success, as defined by less than 30% residual stenosis on angiography following orbital atherectomy alone, was 78%. The use of adjunctive angioplasty and/or stenting for 84 lesions (42%) increased this to 93%. Ankle-brachial indices were 0.68 at baseline, 0.90 at 30 days, and 0.82 at 6 months. Additionally, the 6-month target lesion revascularization rate was 0.9%. Of note, the mean lesion length in this study was 3.0 cm ± 2.9 cm. The large industry sponsored CONFIRM registry collected data on 3135 interventions with 81% moderate/severe calcium, 36% below the knee (BTK) with mean lesion length 7.2 cm. It revealed high rates of procedural success (defined by target lesion stenosis <30%) but does not report long-term clinical outcomes.
In the OASIS trial, there was a serious adverse event rate of 8%, although only 3.2% of these were directly device related. These device-related complications consisted of thrombus formation at the site of the treated lesion, perforations (at the site of the target lesion and distal to the lesion), and embolization. In the CONFIRM registry, flow limiting dissection occurred in 1.6% of cases, embolism in 1.8%, and vessel rupture in 0.5%. Interestingly, “slow flow” was listed as a complication in 2.9% of cases, perhaps representing microembolization of small particles causing diffuse small vessel outflow occlusions. In addition, vessel closure and spasm occurred in 1.5% and 4.2% respectively. Hemolysis is a unique complication of orbital atherectomy that occurs in 33% of patients. The clinical significance of hemolysis is unclear, but appears to be minimal including hemoglobinuria (9%) and hypertensive crisis (3%).
Instructions for use of the Diamondback 360 device include iliac and infrainguinal calcified atherosclerotic peripheral arterial disease (PAD). Vessel diameter from 2.0 to 10 mm can be treated. The system is designed to modify the plaque, allowing for more effective angioplasty and deemphasizes luminal gain. It is contraindicated in the presence of dissections because the spinning crown can catch and wrap on dissection flaps. It is ineffective in soft lesions or thrombus, and it will cause increased distal embolization. The device is best suited to short heavily calcified lesions with robust tibial runoff. It can also be effective in treating calcified tibial lesions where alternative interventions are limited. Safety can be increased by using short run times and small crown selection.
The Jetstream atherectomy device works by plaque extraction through a rotational cutting blade loaded on a delivery shaft along with active aspiration ( Fig. 18.5 ). The aspiration port is designed to remove debris to minimize the risk of embolization. This is a modification of the Pathway device, which was plagued by high rates of distal embolization. The latest iteration moved the location and increased the suction capacity of the aspiration port. The device is not directed, and thus must be used in true-luminal wire position. It cannot be used in CTO if crossing in subintimal planes. Multiple cutter blade options are available depending on luminal diameter of the treated vessel. There are two cutter designs with the Jetstream device. The Jetstream XC (or eXpandable Cutter Catheters) comes with 2.1- or 2.4-mm tips and is suitable for vessels 3 to 5 mm or larger. The Jetstream SC (or Single Cutter Catheters) comes with 1.6- or 1.85-mm tips (145-cm in length) and are best suited for vessel size 2 to 3 mm. The single cutters have only a front end cutter with no “blades up” feature and are typically used for tibial vessels. It is recommended by some authors to use a saline flush bag with nitroglycerin to prevent vessel spasm around the catheter tip.

Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here