Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
About 1 in 89 spontaneous conceptions results in the birth of twins. However, with the widespread use of artificial reproductive technologies, the incidence of twinning has increased dramatically worldwide, so that in some countries twins now occur once in every 30 pregnancies. Of spontaneously conceived twins, 55% are dizygotic, whereas 45% are monozygotic. Monozygotic cleavage therefore occurs in about 1 of 200 spontaneous conceptions. Dizygotic twins always have separate placentas and are therefore by definition dichorionic. In spontaneous monozygotic twins depending on the timing of cleavage of the early embryo, 35% are dichorionic whereas 65% share a single placenta (monochorionic). Artificial reproductive technologies increase the chance of multiple pregnancies, mainly due to polyovulation. Depending on the method and number of embryos transferred, 1 in 3 to 1 in 10 assisted pregnancies involves a twin pregnancy. Of these, 95% are dizygotic and the result of polyovulation. Nevertheless, 5% are monozygotic of which 20% are dichorionic and 80% monochorionic. What is often neglected is the fact that artificial reproductive technologies (ART) increase the risk of monozygotic splitting which is increased to a risk of 1 in 50 after in vitro fertilization and even to 1 in 25 after ovulation induction. Assisted monozygotic twins are also more likely to have a monochorionic placenta than spontaneously conceived monozygotic twins. In summary, because of ART, the incidence of twin pregnancies has risen significantly. Most of the assisted twin pregnancies are dizygotic and thus dichorionic. Nevertheless the risk of monozygotic cleavage is also increased and these assisted monozygotic twins are also more likely to have a monochorionic placenta.
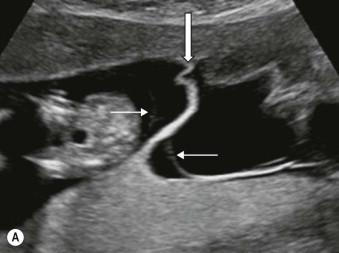
It is neither zygosity nor mode of conception, but chorionicity that is the main determinant for pregnancy outcome. The risk of death between the first trimester and 24 weeks is about 12% for a monochorionic pair which is six times higher than the 2% risk of a dichorionic twin pregnancy. Although most deaths occur prior to 24 weeks, even after viability monochorionic twins remain at significantly increased risk. Complications of the shared circulation account for this excess mortality. During intrauterine life about 95% of monochorionic twins have vascular anastomoses on the placental surface that connect the two circulations ( Figure 9-1 ).

The nearly ever-present blood exchange in monochorionic twin pregnancies is responsible for some unique complications, such as the twin-to-twin transfusion syndrome (TTTS), the twin anaemia polycythemia sequence (TAPS), the twin reversed arterial perfusion (TRAP) sequence and monoamniotic and conjoined twinning. Another consequence of the shared circulation is that the well-being of one twin critically depends on that of the other. After the diagnosis of spontaneous demise of one of a monochorionic pair, the survivor has a 15% risk of death and a 25% risk of neurodevelopmental impairment because of acute exsanguination along the anastomoses into its demised co-twin. The fact that their well-being is interrelated also poses some specific problems in the management of poor growth and imminent demise of the growth-restricted twin, or if one twin has a severe anomaly and selective reduction is considered.
Compared to singletons, twins have a more complicated intrauterine journey with higher risks of intrauterine demise, poor growth, congenital anomalies, miscarriage and preterm birth. In monochorionic pairs, there is the added risk of the shared circulation that makes their well-being interrelated. Most importantly, the management of twin pregnancies is complicated because the interests of both twins have to be taken into account. Ultrasound plays a key role in the surveillance of these pregnancies. The advantage of scanning a twin pregnancy is that growth and amniotic fluid can be compared as the co-twin can serve as a control. The downside is that visualization may be hampered and it is important to accurately label the twins to avoid scanning the same twin twice.
In this chapter, we will discuss the importance of the first trimester scan for an accurate determination of chorionicity. We will describe the complications unique to monochorionic twin pregnancies and the role of ultrasound in their management. We will also address the demise of one of the twins, poor growth and the presence of an anomaly, which are complications that occur in dichorionic as well as monochorionic twins but require a different management depending on chorionicity. Finally, cervical length measurement in the prediction of preterm birth will be addressed. As a summary, we will provide a scheme that can be used for the assessment of twin gestations.
The first trimester ultrasound scan is of paramount importance in the evaluation of twin gestations for the determination of chorionicity, accurate dating, labelling of each twin, risk assessment for chromosomal anomalies and finally for the detection of major structural anomalies.
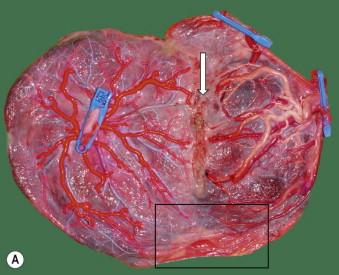
The management of twin pregnancies starts in the first trimester with an accurate determination of the chorionicity. It is of paramount importance to identify monochorionic twin pregnancies, for which increased monitoring will improve outcome. It is essential for genetic counselling and for the management of in utero demise, poor growth or an anomaly in one of the twins. The distinction between a high-risk monochorionic and a lower risk dichorionic twin pair is most accurate at the 11 to 14 weeks' scan because amnion and chorion have not yet fused. The sonographer simply has to count and assess the different layers that separate the twins. In a dichorionic twin pair, the twins are separated by three layers: one thick layer in the middle consisting of the two adjacent chorionic membranes with two thin layers of amniotic membrane on each side. Also, the yolk sacs are in separate exocoelomic cavities. In monochorionic diamniotic twin pairs, separation is only by two thin amniotic membranes and in the rare monoamniotic twins, there is no separation and the common amniotic membrane encircles both twins ( Figure 9-2 ). In monochorionic twins, the yolk sacs are in a common exocoelomic cavity. In contrast to common belief, the number of placental masses does not predict the chorionicity. Dichorionic placentas are commonly fused to a supposedly single mass and monochorionic placentas can be bilobar and thus present as two apparently separate placental masses, which does not preclude the presence of vascular anastomoses ( Figure 9-3 ). Similarly, the amnionicity is not predicted by the number of yolk sacs. A minority of monoamniotic twins have two yolk sacs, whereas a minority of diamniotic twins have a single yolk sac. The literature often describes the dichorionic septum as a lambda sign, whereas the monochorionic septum is said to form a T sign on its uterine insertion. In our opinion, these terms are best avoided in the first trimester, as this is clearly a second trimester feature and may lead to misclassifications. In the first trimester, the close apposition of the two amniotic sacs forms a true lambda sign in monochorionic pairs, whereas the fusion of the two chorionic layers forms a twin peak sign ( Figure 9-4 ).


After 14 weeks, when amnion and chorion have fused, it becomes impossible in a same sex twin pair to determine with certainty if the placenta is monochorionic or dichorionic. Therefore, each first-trimester scan should specify chorionicity and failure to determine this is truly a missed opportunity and considered substandard care. This is because of the potential major implications for management and follow-up. An image of the intertwin septum should be kept in the patient's notes should any doubt arise later in the pregnancy.
In contrast to chorionicity, zygosity cannot always be determined on prenatal ultrasound scan. If the pregnancy is monochorionic, parents can be told that their twins are monozygotic. However, if the pregnancy is dichorionic and later scans confirm a similar sex, then only DNA fingerprinting can determine if the twins are mono- or dizygotic.
As in singleton pregnancies, knowledge of the exact gestational age in twin pregnancies is important, though induction of labour for post-term twin pregnancies is less of an issue. The problem of accurate dating only applies to spontaneous twin pregnancies; the date of ovum pick-up or insemination correctly determines the conception date in assisted twins. As in spontaneously conceived singletons, an accurate measurement of the crown–rump length reflects gestational age in twin pregnancies more precisely than the last menstrual period. The problem arises when there is a significant difference in crown–rump length, and if the smaller, larger or an average crown–rump length should be used for pregnancy dating. Although the literature gives no firm answers on the best option, taking the crown rump length of the larger twin seems most prudent because it will give the worst possible scenario in the assessment of discordant growth. Dating by the smaller crown–rump length may falsely reassure the sonographer that the larger twin is too large and the smaller is still growing appropriately.
For the purpose of serial follow-up in diamniotic pregnancies, we label each twin individually in the first trimester. As such, the twin that is most right-sided (from a maternal perspective) is called twin 1 and the most left-sided twin 2 ( Figure 9-5 ). This works well in more than 90% of cases in the sense that each twin maintains its side of the uterus during the course of pregnancy. However, in the minority that are in a transverse position with one below and one above, then the most right sided cord insertion is chosen to be twin 1. Of course, the placental location and site of cord insertion are described for each twin for additional verification. In the third trimester, the presenting twin is also noted. In monoamniotic twins with concordant growth and no distinguishing ultrasound findings, labelling is not possible.

As in singleton pregnancies, parents can choose between three options: no screening (if a termination is not desired for aneuploidy), to screen (if parents would consider termination) or have a diagnostic test (if parents consider termination and want 100% certainty about the absence of aneuploidy). For patient counselling, diagnosis and management, knowledge of chorionicity is mandatory. As such, in dichorionic and thus most likely (90%) dizygotic twins, a selective reduction can be done if a chromosomal abnormality is diagnosed in one twin. If the diagnosis is made in the first trimester, selective reduction by intracardiac potassium injection by an experienced operator is associated with a 7% risk of loss of the entire pregnancy, and a 14% risk of birth before 32 weeks, and is probably somewhat safer when performed in the first trimester. On the other hand, in monochorionic twin pregnancies and thus by definition monozygotic twin pregnancies, one would expect both fetuses to be affected and a termination of pregnancy may be performed. Nevertheless, discordance for all common human aneuploidies (trisomy 13, 18, 21, Turner syndrome and triploidy) has been reported in monochorionic twin pairs. This discordance known as heterokaryotypia is only diagnosed by amniocentesis of both sacs. In the event of heterokaryotypic monochorionic twin pregnancies, selective reduction by umbilical cord occlusion can be offered from 16 weeks onwards, but at a procedure-related loss rate of about 20% for the healthy twin. Parents must be thoroughly counselled about the different possible scenarios before they can give their informed consent for screening.
The best screening test for aneuploidy in twin pregnancies is by a combination of maternal age and measurement of the nuchal translucency in the first trimester. Its performance can be improved by adding maternal serum biochemistry, but adjustments are necessary to correct for chorionicity. In dichorionic twin pregnancies, levels of free β-human chorionic gonadotropin and pregnancy-associated plasma protein-A are twice as high as in singletons, whereas in monochorionic twins levels are lower than in dichorionic twins. No specific studies are available on how the addition of other markers such as nasal bone, tricuspid regurgitation and ductus venosus flow affect screening in twins, but they are likely to improve screening, at least in dichorionic twins. Nuchal translucency measurements in euploid dichorionic twins are correlated and this correlation is more than simply a sonographer effect, so for risk calculation this should be taken into account as well. For dichorionic twins (dizygotic in 90%) it makes sense to quote the specific risks for each twin separately. As such, combined first-trimester screening (ultrasound and biochemistry) will detect about 90% of affected fetuses, with a false-positive rate of 3% per fetus but 6% per pregnancy. As two fetuses are evaluated separately, the chance that the test will classify one of them at increased risk is 6%, i.e. the false-positive rate is thus twice as high as in singleton pregnancies and patients need to be informed of this. The main advantage of first-trimester screening in dichorionic twin pregnancies is that an early first trimester selective reduction can be done if the chorionic villus sampling confirms aneuploidy in one of the twins. Also, the increased nuchal translucency helps to identify the affected fetus.
The standard of care is to perform a chorionic villus sampling for the diagnosis of chromosomal anomalies in dichorionic twins: ideally both twins should be sampled as only 10% of dichorionic twins are monozygotic. Sampling can be done transabdominally, transvaginally or by a combination of both. To avoid a reduction of the wrong twin, it is important to map the placentas and cord insertions accurately and preferably both the diagnostic test and later selective reduction is done by the same operator. Although no good data are available, it seems fair to counsel the patient that the risk of miscarriage is somewhat higher than the 1 in 100 that is usually quoted in singletons, especially if two punctures are necessary. The risk of contamination is probably also higher and the need for later re-sampling is increased as well.
In monochorionic twin pregnancies, an increased nuchal translucency of one or both twins is present in 13% and may be a manifestation of an early twin transfusion imbalance rather than indicating the presence of a chromosomal anomaly. Quoting the risk of the fetus with the largest nuchal measurement may overestimate the true risk and increase false-positive rates. Therefore, in a monochorionic pair, the risk assessment should be done by taking the average of the two nuchal measurements. For monochorionic twin pairs, a pregnancy-specific risk is calculated, in the assumption that both are expected to be affected in a monozygotic pair. Detection rates are similar to those in dichorionic twin pregnancies, but with a higher false-positive rate of 13%.
Because chorionic villus sampling may miss the presence of the aneuploid or euploid fetus in the setting of heterokaryotypic twins, we always perform an amniocentesis of both amniotic sacs at 16 weeks. If at 16 weeks, there are signs of developing TTTS, we defer the karyotyping to 18–20 weeks to avoid bloodstained amniotic fluid should a laser procedure be necessary later on. An exception to a dual sampling may be that the invasive test is done for maternal anxiety when both twins have normal appearance, in which case it may be acceptable to sample only one twin. In order to avoid an iatrogenic monoamniotic twin, we always perform a double transabdominal puncture instead of a single puncture with septostomy.
Structural anomalies are more common in twins than in singletons. Unfortunately, most studies do not subgroup incidence by either zygosity or placentation. The rate per fetus in dizygotic twins is probably the same as in singletons, whereas it is two to three times higher in monozygotic twins. Abnormalities associated with twins include neural tube defects, brain lesions, facial clefts, gastrointestinal defects, anterior abdominal wall defects and cardiac anomalies. Even in monozygotic twins, concordance for a structural anomaly is rare (<20%). Vascular events in early embryogenesis and later fetal life contribute to discordant brain and heart anomalies encountered in monochorionic twins. In our series of 202 monochorionic twin pairs, major discordant congenital anomalies occurred in 1 in 15 pregnancies and always affected only one twin.
The first-trimester scan is an ideal opportunity to check the fetal anatomy of both twins and exclude any major anomalies. A recent large series showed that nearly half of all major anomalies can be identified on the first-trimester ultrasound scan. Abnormalities that are always detectable are anencephaly, alobar holoprosencephaly, omphalocoele, limb body wall defect, megacystis and gastroschisis and, in a monochorionic twin pregnancy, the twin reversed arterial perfusion sequence. Other anomalies, such as absence of limbs, facial clefts, structural heart defects, renal agenesis, and diaphragmatic hernia may also be detectable, but these require more experience and time, better equipment and often a combination of vaginal and abdominal scanning ( Figure 9-6 ).

TTTS complicates 1 in 10 monochorionic diamniotic twin pregnancies and usually occurs between 16 and 26 weeks. TTTS is strictly a sonographic diagnosis, characterized by amniotic fluid discordance with polyhydramnios and a distended bladder in the volume-overloaded polyuric recipient, and oligohydramnios and a small or empty bladder in the volume-depleted oligouric donor. Because amniotic fluid varies with gestation, most European centres use a gestational age-dependent cut-off to define polyhydramnios in the recipient: a deepest vertical pocket of >8 cm is used prior to 20 weeks, whereas >10 cm is used after 20 weeks. In the United States, >8 cm is used as a cut-off throughout gestation. The definition of oligohydramnios in the donor sac is similar in Europe and the USA, and is set at <2 cm. The sonographic diagnosis of TTTS is thus straightforward and simple. It does not require any advanced skills besides being able to measure the deepest vertical amniotic fluid pocket in each sac ( Figure 9-7 ). Alternatively the documentation of a free-floating intertwin membrane rules out the presence of TTTS.

The exact pathophysiology of TTTS is not fully understood. Certainly, vascular anastomoses are necessary for its development, but there is no unique pattern of anastomoses that causes TTTS, although the presence of a bidirectional artery-to-artery anastomosis seems to be protective. Cordocentesis studies have shown that as a rule the recipient is not polycythemic and the donor is not anaemic. An elevated middle cerebral artery-peak systolic velocity (>1.5 MoM) is present in only 4% of donors and in 3% of recipients. Therefore, TTTS is not caused by a simple transfer of red blood cells. Instead TTTS is a problem of amniotic fluid imbalance. Therefore endocrine factors related to fluid and pressure homeostasis are likely to be involved as well. The intertwin blood exchange exposes one twin to the endocrine environment of the other. As such, transfer of renin-angiotensin-aldosterone effectors from the donor may partly explain the recipient's hypertensive cardiomyopathy and volume overload.
Discordant growth with a larger recipient and smaller donor is usually present, but is not essential for the diagnosis. Also, signs of mostly right ventricular dysfunction are commonly present in the recipient with cardiomegaly due to increased myocardial thickness, tricuspid regurgitation and right ventricular outflow tract obstruction. These signs of cardiac dysfunction are neither essential for the diagnosis nor specific for TTTS as they also commonly occur in the larger twin in discordant growth without TTTS. Nevertheless, detailed echocardiography with documentation of cardiac function forms an integral part of each pre- and postoperative assessment, but as cardiac dysfunction predicts neither the development of TTTS nor the survival after treatment, so treatment decisions will not usually depend on the degree of cardiac dysfunction. Treatment will be offered as soon as the amniotic fluid criteria are fulfilled.
The severity of TTTS is usually assessed according to the Quintero staging system, based on the presence (stage 1) or absence (stage 2) of bladder filling, abnormal Doppler patterns (stage 3), hydrops (stage 4) or intrauterine demise (stage 5). The usefulness of this staging system has been questioned, because firstly it does not represent a timescale of progressive deterioration. As such, pregnancies can progress directly from stage 1 to stage 5, without passing through stage 2, 3 and 4. Secondly, it only correlates weakly with outcome, and treatment is the same for stage 1 to 4. Nevertheless, because it describes different manifestations of the same disease, its ease of use and the lack of a better alternative, the Quintero staging system is still universally used.
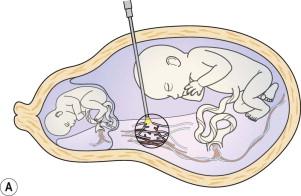
TTTS is the most important cause of death and disability in a monochorionic diamniotic twin pregnancy, even with the best care. Because TTTS occurs in the pre-viable period, its prognosis is dismal without treatment. Polyhydramnios-related miscarriage or the preterm birth of two sick neonates is common as well as intrauterine demise of one or both twins. Fetoscopic laser coagulation of all vascular anastomoses is currently the best treatment, regardless of disease stage ( Figure 9-8 ). There is still debate on whether stage 1 disease (normal Doppler assessment and bladder filling in the donor) should be treated with laser, and a current randomized control trial is comparing immediate laser treatment with initial expectant management for stage 1 disease. Laser aims to cure the disease by disconnecting the two fetal circulations ( Figure 9-9 ). Successful interruption leads to a normalization of urine output, amniotic fluid volumes and cardiac function in the recipient twin. Although survival doubles from approximately 30% in untreated cases to 60% after laser therapy, outcome is still far from perfect. In experienced hands, in about 50% to 60% of cases, both twins survive in 30% one baby survives and in 10% to 20%, both are lost. Most double losses are miscarriages or severe preterm births and less commonly related to residual anastomoses. Most single deaths are an intrauterine demise typically within the first postoperative weeks and probably related to unequal placental sharing, cardiac failure, perioperative exsanguination or missed anastomoses. Of surviving infants, 11% have some form of developmental impairment, of which cerebral palsy is the most common (present in 5%). An early gestational age at birth is the single most important predictor of impairment.
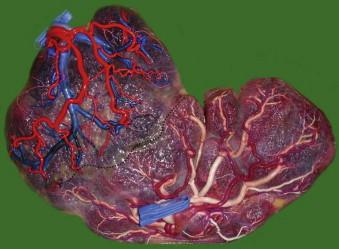
After laser treatment with dual survival, close ultrasound surveillance remains necessary. About 1 in 10 pairs will develop twin-anaemia polycythemia sequence (iatrogenic TAPS) or recurrent TTTS due to missed anastomoses. TAPS usually only occurs several weeks after the procedure with a recipient that becomes anaemic and the former donor becoming polycythemic. Iatrogenic TAPS is associated with missed small-calibre anastomoses (<1 mm) ( Figure 9-10 ), which owing to the polyhydramnios and increased intrauterine pressure, may be invisible at the time of surgery. A chronic net transfusion via these hairlike anastomoses may lead to severe haemoglobin discordances several weeks later. TAPS is usually not associated with severe amniotic fluid discordance and is only picked up by serial measurement of the middle cerebral artery-peak systolic velocity (MCA PSV). Typically MCA PSV will progressively rise above 1.5 multiples of the median (MoM) in the anaemic twin and decrease below 1 MoM in the polycythemic co-twin. Once TAPS is suspected, a cordocentesis will confirm the diagnosis and an intrauterine transfusion may gain some extra time. However, if the anaemia recurs within a week, an elective birth, a repeat laser procedure or selective reduction by cord coagulation can be offered depending on gestational age, the accessibility of the anastomoses and the condition of the twins.
Recurrent TTTS is typically associated with large residual anastomoses and usually the polyhydramnios recurs within the first 3 weeks after the initial laser procedure. The demonstration of bladder filling and increasing amniotic fluid of the donor is a sign of resolution of TTTS. However, fluid only normalizes in the donor twin after one week. If there was an accidental septostomy during the procedure, then both twins will have an equal amount of amniotic fluid immediately after the procedure and it is important to look for possible cord entanglement. Similar to TAPS, the management of recurrent TTTS also depends on gestational age, the accessibility of the anastomoses and fetal condition. Possible options are an elective birth, amnioreduction, a repeat laser procedure or selective reduction. For the detection of these late complications, it is generally recommended that surviving pairs are scanned weekly for the first 4 postoperative weeks and 2-weekly thereafter. MCA PSV measurement should be part of the surveillance to allow timely detection of TAPS.
After successful laser treatment, cardiac dysfunction generally normalizes in the recipient within 1 month while the donor suffers from a temporary impairment of cardiac function. Rarely, the donor may show one or more hydropic signs which are usually mild and transient. Nevertheless, 8% of recipient twins will have pulmonary artery stenosis at birth and 4% of survivors will suffer antenatal brain damage. Functional heart problems and antenatal cerebral lesions may only become obvious in the third trimester and careful assessment of the heart and brain are required throughout pregnancy. To detect brain anomalies, such as migration and proliferation disorders, we offer a fetal brain MRI at 30 weeks to all survivors after laser treatment. Special attention is paid to limb development as the recipient twin is at risk for amputation, mostly of the lower limbs due to thrombi or more rarely amniotic bands ( Figure 9-11 ).

Several first-trimester markers such as discordance in nuchal translucency or in crown-rump length measurement or reversed a-wave in the ductus venosus have been proposed to predict TTTS. Of these, a reversed a-wave in the ductus venosus in one or both twins seems the best predictor. Yet, an abnormal ductus venosus will pick up only 38% of all pregnancies that develop TTTS, and of those predicted to be at high risk only 30% will ultimately develop TTTS. TTTS is therefore mostly unpredictable, but a timely diagnosis is necessary to offer laser treatment before intrauterine demise, ruptured membranes or cervical changes occur. Therefore, it is recommended that all monochorionic twin pregnancies require an ultrasound scan every fortnight to exclude TTTS. All patients expecting monochorionic twins should receive information about the symptoms of TTTS and be instructed to seek medical advice should they experience sudden abdominal distension, difficulty breathing or menstruation-like abdominal pain.
Spontaneous TAPS complicates about 1 in 20 monochorionic diamniotic twin pregnancies and is a complication of the third trimester which usually occurs after 26 weeks. TAPS is characterized by a haemoglobin discordance with a polycythemic recipient and anaemic donor. Iatrogenic TAPS may occur after laser treatment for TTTS in up to 1 in 10 pregnancies with 2 surviving twins. The antenatal diagnosis is based on the presence of an elevated MCA PSV (>1.5 MoM) in the donor and a decreased middle cerebral artery-peak systolic velocity MCA PSV (<1 MoM) in the recipient and anaemia is best confirmed by cordocentesis. The postnatal diagnosis requires the presence of an intertwin haemoglobin difference of more than 8 g/dL in combination with proof of a chronic transfusion imbalance: either a placenta with only small anastomoses (<1 mm) or a donor/recipient reticulocyte count ratio of more than 1.7. Discordant amniotic fluid is commonly present. Rarely, the fluid discordance is severe and fulfills the criteria for TTTS. In that case, the condition will be diagnosed and treated as TTTS. Discordant growth is present in about half the TAPS cases with a small anaemic donor and large plethoric recipient, but it is not essential for the diagnosis. Typically in TAPS, the growth discordance only develops after 20 weeks, so a progressive increase in estimated fetal weight difference in the latter half of pregnancy should prompt assessment for TAPS. Additional ultrasound findings in TAPS include differences in placental echogenicity and thickness with a bright, thickened section for the donor twin and an echolucent thin recipient section. The placentas of spontaneous and iatrogenic TAPS are strikingly similar. The liver of the polycythemic twin may have a starry sky pattern due to diminished echogenicity of the liver parenchyma and an increased brightness of the portal venule walls. Finally, if the anaemia is severe, signs of hydrops may be detected in the donor ( Figure 9-12 ).

The pathophysiology of TAPS is thought to be different from that of TTTS. The anastomoses in TAPS are minuscule and few, which suggests that TAPS is a true intertwin transfusion imbalance due to a chronic net transfer of red blood cells.
Because spontaneous TAPS typically occurs in the viable period when elective birth is an option, it does not usually lead to death and disability. Nevertheless, if undiagnosed, severe anaemia can cause intrauterine demise, and cerebral damage such as cerebellar haemorrhage and polycythemia may cause cerebral or limb infarctions. If a severely preterm birth is necessary this may obviously complicate the outcome too. The best treatment is not well established but will primarily depend on the gestational age at diagnosis. Once TAPS is suspected antenatally based on discordant MCA PSV, then we repeat the assessment in 2–3 days, unless there are signs of hydrops in the anaemic donor. If discordance persists in a pregnancy below 34 weeks, we perform a cordocentesis and transfusion and monitor middle cerebral artery-peak systolic velocities every 2–3 days. If discordance recurs, a second transfusion may be considered. If there is rapid recurrence of the anaemia after two transfusions, the options are elective birth, selective reduction or (re)laser of the vascular anastomoses, depending on gestation, fetal condition and accessibility of the equator. In rapidly recurring anaemia, the risk of hyperviscosity-related complications in the receiving twin is increased, so usually only two transfusions are given. A fetoscopic laser procedure for TAPS is more difficult than for TTTS, because of the lack of polyhydramnios, the minuscule anastomoses and more advanced gestational age. After 30 weeks and administration of steroids, an elective birth seems the most rational approach.
Because TAPS may cause late intrauterine demise in previously uncomplicated pregnancies, and will not necessarily present with discordance in growth or amniotic fluid, we measure the MCA PSV routinely every fortnight from 20 weeks until birth. Although TAPS rarely occurs before 26 weeks, with serial measurements a gradual and progressive discordance is picked up more easily when the measurements are plotted. In pairs with worsening growth discordance after 24 weeks, one should be suspicious of TAPS.
TRAP is a rare condition, affecting 1 in 100 monochorionic twin pregnancies. In TRAP, blood flows from an umbilical artery of the healthy pump twin in a reversed direction into the umbilical artery of its co-twin, via an arterioarterial anastomosis and usually returns via a venovenous anastomosis back to the pump twin. The perfused twin is thus a true parasite and usually does not have any cardiac activity of its own, hence the name acardiac twin. The acardiac twin's blood supply is by definition deoxygenated and this results in variable degrees of deficient development of the head and upper limbs. Oxygen-depleted blood usually returns via a venovenous anastomosis to the pump twin, causing some degree of hypoxaemia.
TRAP is a first-trimester diagnosis and is characterized by a grossly abnormal twin that grows and may move but has no functional cardiac activity of its own. Rarely a rudimentary heart may show pulsatility. Marked hydrops and cystic hygroma are frequently present, especially towards the end of pregnancy. Doppler studies reveal the pathognomonic features of reversed arterial perfusion through an arterioarterial anastomosis ( Figure 9-13 ). Sometimes the cord of the acardiac twin arises directly from the pump twin's cord. TRAP can easily be distinguished from single demise by the presence of fetal movements and the typical retrograde perfusion.

Two criteria are necessary for the development of TRAP sequence. The first prerequisite is a large arterio-arterial and venovenous anastomosis and the second is a discordant development or an intrauterine demise of one of the monochorionic twins, allowing for the reversal of blood flow. In dichorionic twin pregnancies, intrauterine demise of one twin in the first trimester invariably leads to a ‘vanishing twin’, whereas in monochorionic twins, existing anastomoses may actually prevent ‘vanishing’. Each time a single demise is diagnosed in a monochorionic twin pregnancy in the first trimester, the possibility of TRAP sequence should be considered and the umbilical artery examined for reversal of flow.
TRAP is associated with a high risk of perinatal death caused by a combination of high-output cardiac failure and polyhydramnios-related preterm birth. There is also concern about long-term neurologic consequences for the pump twin because of chronic hypoxaemia, cardiac failure and preterm birth. The outcome may be improved by arresting the circulation of the acardiac twin. The type of procedure is best adapted to the clinical presentation and may consist of coagulation of the umbilical cord and/or placental anastomoses or of intrafetal laser or radiofrequency ablation. After such an intervention, 80% to 90% of pump twins survive with an average gestational age at birth between 35–36 weeks.
TRAP is now mostly diagnosed in the first trimester. However, intrauterine intervention to arrest the flow is usually performed only after 16 weeks, after fusion of amnion and chorion. As such, all our patients are offered a prophylactic intervention at 16 weeks, because pump twin demise is difficult to predict in the early second trimester and it precludes the difficulty of achieving arrest of flow in the larger and often hydropic mass later on in pregnancy. Nevertheless, parents need to be aware that there is a 1 in 3 risk of intrauterine demise of the pump twin before the time of the planned intervention. To address the high mortality of TRAP in the first trimester, small case series have examined the outcome of intrafetal coagulation in the first trimester. Although these show promising results, larger series are necessary to confirm the safety of this procedure.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here