Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Reconstruction of the hepatic artery is one of the principal technical challenges in orthotopic liver transplantation, and successful patient and allograft outcomes depend on robust, uninterrupted arterial flow into the newly implanted liver. Because oxygen is delivered to the allograft's biliary ductal system almost solely through the hepatic artery, and because recipient collaterals to the liver are divided during the hepatectomy, the technical aspects of arterial reconstruction (inflow, anastomosis, and outflow) are of paramount importance. Complications related to the hepatic artery are a major source of recipient morbidity and graft loss and can lead to recipient mortality. Liver allograft recovery and viability therefore depend heavily on expert and efficient restoration of arterial flow into the liver ( Fig. 61-1 ).
The most common complication related to hepatic artery reconstruction is hepatic arterial thrombosis (HAT) ( Fig. 61-2 ), which occurs in about 5% of adult and 7% of pediatric liver transplants. HAT has been associated with biliary complications ( Figs. 61-3 and 61-4 ) and decreased patient and allograft survival, and retransplantation is required in most cases. Additional complications include stenoses or kinks of the hepatic artery related to anastomotic construction as well as to the lack of supportive periarterial tissue after liver transplantation. Hepatic artery pseudoaneurysm or rupture can also occur, is frequently associated with infection, can be extremely difficult to treat with surgical or endovascular means, and is often fatal.
Prevention of these complications can be achieved by (1) understanding the factors that predispose to arterial complications, (2) identifying specific risk factors for arterial problems in the recipient and in the donor liver, (3) optimizing recipient arterial inflow, (4) reconstructing the arterial supply in a manner to eliminate arterial dissection, twist, kink, and redundancy, and (5) restoring arterial flow as expeditiously as possible to promote effective allograft recovery. This chapter will detail how the transplanting surgeon can effectively plan arterial reconstruction and anticipate potential pitfalls to maximize the technical precision and the efficiency of transplant arterialization.
Although some have emphasized medical factors in arterial complications, most surgeons continue to view this problem as technical in origin unless proven otherwise. Maintenance of hepatic artery patency and optimal flow requires (1) satisfactory arterial inflow in the recipient, (2) a properly oriented anastomosis with perfect intima-to-intima opposition, and (3) relatively low-resistance outflow through a healthy allograft. Achieving these goals requires thorough pretransplantation preparation by imaging review (ultrasonography, computerized tomography [CT], magnetic resonance imaging [MRI]), effective donor-recipient matching, meticulous surgical technique, and minimization of cold-ischemia time to limit ischemia-reperfusion injury. During any liver transplantation the surgeon has to be ready for surprises such as arterial variants or poor flow in the recipient hepatic artery; however, proper preparation with imaging review before starting the recipient hepatectomy will minimize unexpected findings, expedite arterial reconstruction, and improve arterial and graft outcomes.
In truth, the hepatic arterial reconstruction begins during the pretransplantation surgical evaluation. This initial encounter with the liver recipient can help identify several factors that can affect arterial reconstruction, such as (1) history of arterial occlusive disease at other sites, (2) history of hepatic arterial manipulations such as transarterial chemoembolization, (3) history of prior thromboembolic events suggestive of heritable thrombophilia, (4) prior liver transplantation, and (5) prior major aortic interventions (open or endovascular). Of critical importance during the pretransplantation evaluation is the review of the candidate's contrast-enhanced hepatic imaging. When done thoroughly, this process allows the surgeon to identify potential intraoperative problems ahead of time, creating the opportunity for operative planning and avoidance of complications. In the evaluation of the potential liver transplant candidate, a contrast-enhanced CT or MRI scan is a nonnegotiable step, and its results can influence or even determine the appropriateness of listing the patient. Although some candidates have significant renal insufficiency as part of their liver disease, almost all candidates can get contrast-enhanced imaging without suffering irreversible renal injury or dermatosclerosis. The objectives of the pretransplant imaging are as follows: (1) to identify the arterial anatomy, (2) to assess adequacy of the inflow vessel(s), (3) to identify the relationship of the optimal inflow vessel to other structures (varices, portal vein, and its tributaries), and (4) to assess the quality of the infrarenal aorta for aortohepatic grafting, if necessary.
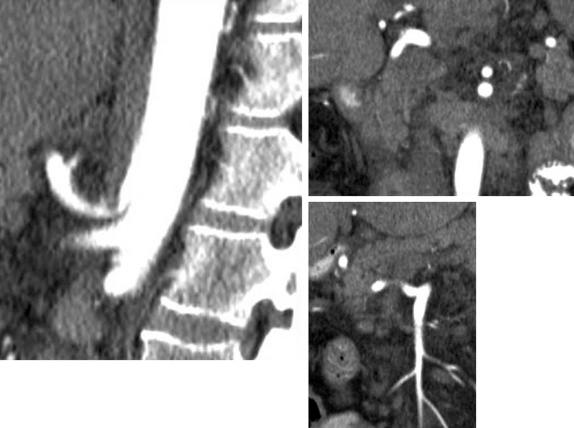
An abundance of information can be obtained through review of the patient's images before transplantation. Native liver size, recipient body habitus, and presence of ascites are all easily assessed by reviewing cross-sectional imaging such as CT or MRI. These factors can influence donor-recipient matching as well as maneuvers required for adequate arterial exposure during transplantation. In addition, these images detail arterial anatomy and allow the surgeon to identify the best arterial candidate vessel(s) for inflow. This process can expedite hepatectomy, because preoperative definition of hepatic arterial anatomy will direct the conduct of arterial exposure during the operation. For example, identification of a retroportal common hepatic artery arising from the superior mesenteric artery will eliminate unnecessary dissection on the patient's left side of the portal vein during hepatectomy. This leads to expeditious arterial definition and less bleeding during hepatectomy. Preoperative imaging can also demonstrate median arcuate ligament compression of the celiac axis ( Fig. 61-5 ). This median arcuate ligament syndrome (MALS) can compromise arterial inflow and predispose to HAT. On CT or MRI, MALS is best identified in the sagittal view, where celiac compression is readily and often dramatically apparent. Intraoperatively, MALS is heralded by respiratory variation in the intensity of the pulse and thrill of the hepatic artery: during deep ventilations, the pulse and thrill are stronger than during exhalations. Identifying these pitfalls will enable the surgeon to anticipate surgical division of the median arcuate ligament at the time of arterial reconstruction, to identify potential alternative inflows, or to expedite moving to aortohepatic grafting (see Fig. 61-5 ). After preoperative image review the surgeon should have in mind (1) the recipient's arterial anatomy, (2) the optimal inflow vessel for the donor hepatic artery (common hepatic versus replaced right versus aorta), (3) presence or absence of median arcuate compression or celiac atherosclerosis, and (4) the threshold for aortohepatic grafting and overall quality of infrarenal aorta. Some patients have densely calcified abdominal aortas, prior aortic aneurysm repair, or even aortic endograft and are dangerous candidates for aortohepatic grafting. If this is the case, then use of the supraceliac aorta for inflow is possible, or the patient may not be an acceptable candidate for orthotopic liver transplantation given high vascular risk. Ideally, the artery and aorta are first assessed during transplant evaluation and again reviewed just before transplantation.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here