Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Cardiac arrhythmias require urgent attention, as some are life-threatening and can lead to sudden death.
The most important initial evaluation is for haemodynamic stability. Patients who are hemodynamically stable should have a 12-lead electrocardiogram (ECG), whereas unstable patients require immediate intervention.
Bradyarrhythmias should always be evaluated in the light of the patient’s presenting symptoms as well as the ECG abnormality.
Patients with wide complex tachycardia should be considered to have ventricular tachycardia unless proved otherwise.
Arrhythmia is the term used to describe an abnormal heart rhythm. The most common arrhythmias are atrial or ventricular ectopic beats. Tachycardia occurs when the heart rate is greater than 100 beats per minute (bpm), and bradycardia is defined as a rate below 60 bpm. The management of cardiac arrhythmias depends on the presentation of the patient, his or her haemodynamic stability, underlying heart disease (if any) and the exact type of arrhythmia. Patients with asymptomatic stable arrhythmias in the absence of underlying heart disease usually do not require emergency treatment. However, patients with symptomatic arrhythmias, especially when associated with underlying heart disease, require more urgent therapy. The key objective is restoration of adequate cardiac output to maintain cerebral perfusion as well as a stable rhythm using interventions least likely to cause harm.
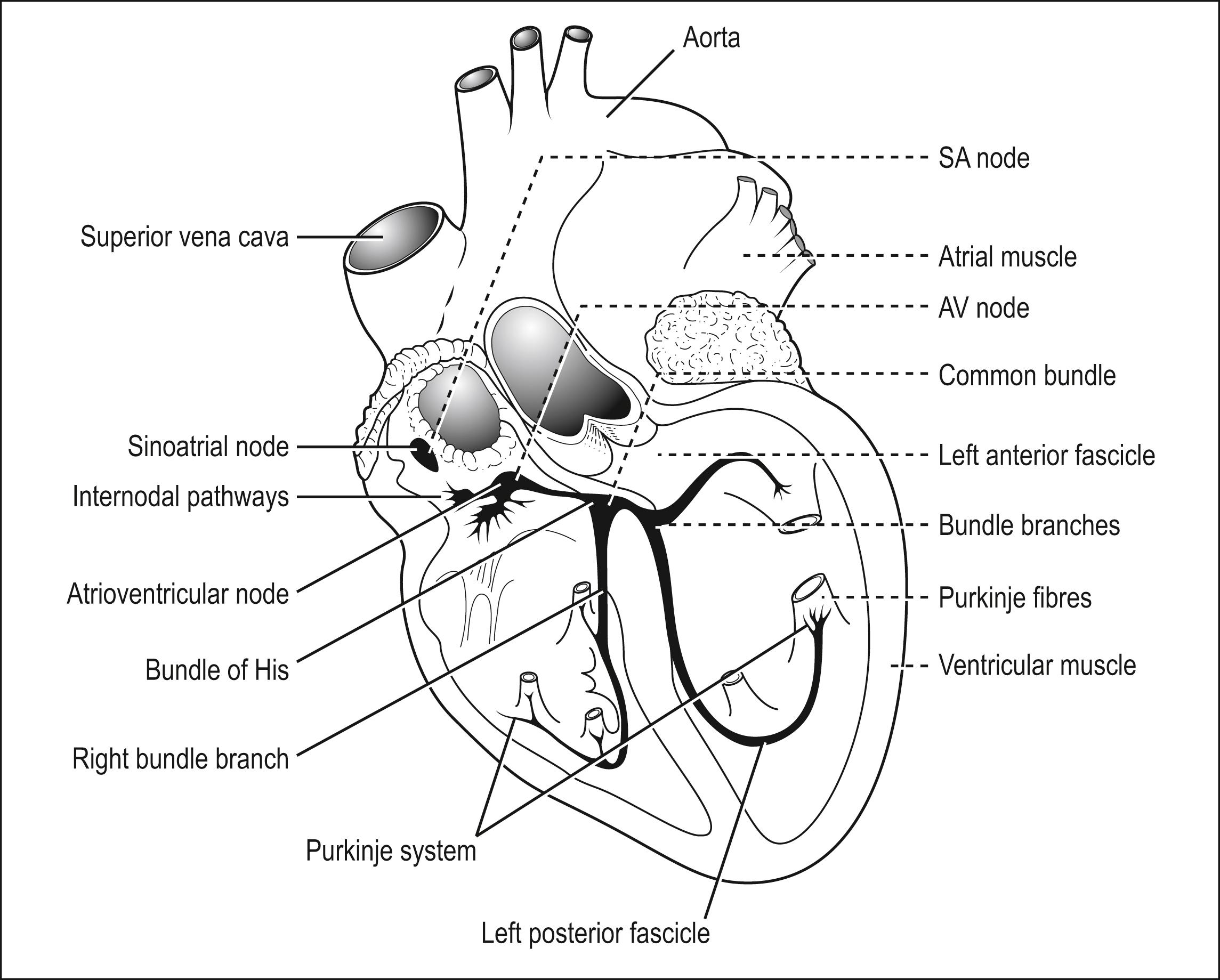
An understanding of cardiac arrhythmia requires knowledge of the normal conduction system ( Fig. 5.4.1 ). In the normal heart, electrical impulses start from the sinoatrial (SA) node and conduct via the atria to the atrioventricular (AV) node. The electrical impulses then conduct down the bundle of His to the right and left bundle branches and subsequently via the Purkinje fibres to the ventricular myocardium.
Different mechanisms—such as re-entry, enhanced automaticity and triggered activity—can result in arrhythmias. Generally arrhythmias are thought of as abnormal impulse generation or abnormal impulse conduction. Abnormal impulse generation in the SA node, as in sick sinus syndrome, can result in failure of impulse formation. Abnormal impulse conduction in the AV node can result in failure of electrical conduction from the atrium to the ventricles, resulting in various degrees of AV block. Ectopic impulses in the atria result in atrial ectopics or atrial tachycardia. Accessory pathways between the atrium and ventricle can result in supraventricular tachycardia (SVT). Abnormalities in ventricular conduction can result in bundle branch blocks or a variety of intraventricular conduction abnormalities. The most dangerous arrhythmias arise from the ventricles, as these, especially in the presence of underlying structural heart disease, may be associated with sudden death.
Re-entry occurs when a closed loop of conducting tissue transmits an electrical impulse around the loop and stimulates atrial or ventricular electrical activity with each pass around the circuit. This pathway can either be an anatomical abnormality such as an accessory pathway or functional abnormality, as in a diseased myocardium caused by ischemia.
Automaticity refers to the generation of an action potential by either the SA node or by abnormal tissue within the myocardium. Automaticity can be enhanced, as during exercise or by drugs. Automaticity can also be abnormal, for example, when action potentials are initiated by tissue other than the SA node, as in ventricular arrhythmias.
Triggered activity is due to after-depolarizations, which are depolarizations of the myocardium before full repolarization occurs. After-depolarizations can be early, as in the case of torsades de pointes VT associated with a prolonged QT, or they can be late, as in the case of catecholaminergic polymorphic VT and idiopathic outflow tract VT.
Patients with arrhythmias may present with symptoms due to the arrhythmia, such as palpitations or syncope, or they may be asymptomatic and have the arrhythmia noticed during routine examination or investigations. All patients should initially be managed in an area where cardiac and other physiological monitoring is available.
The management of arrhythmias should begin with attention to the airway, breathing and circulation. Management of cardiac arrest is discussed in Section 1 . For stable patients, the usual process of history, physical examination and investigations (particularly ECG), is appropriate. Family history of sudden cardiac death should raise the suspicion of ventricular arrhythmia. For unstable patients, urgent intervention is required, with restoration of a stable cardiac rhythm and cerebral perfusion being the priorities. Unstable patients are those with hypotension, dyspnea, chest pain or a decreased level of consciousness. Clinical information—for example, that from a patient with a history of renal failure or heart failure taking spironolactone—should raise the suspicion that a wide complex tachycardia is due to hyperkalemia.
Intravenous access should be obtained and blood drawn for investigations such as full blood counts, electrolytes and cardiac markers (if indicated). A 12-lead ECG is essential, and a chest x-ray may be helpful. Other specific investigations—such as serum digoxin level, thyroid function tests and theophylline levels—may sometimes be indicated, depending on the arrhythmia and the clinical context.
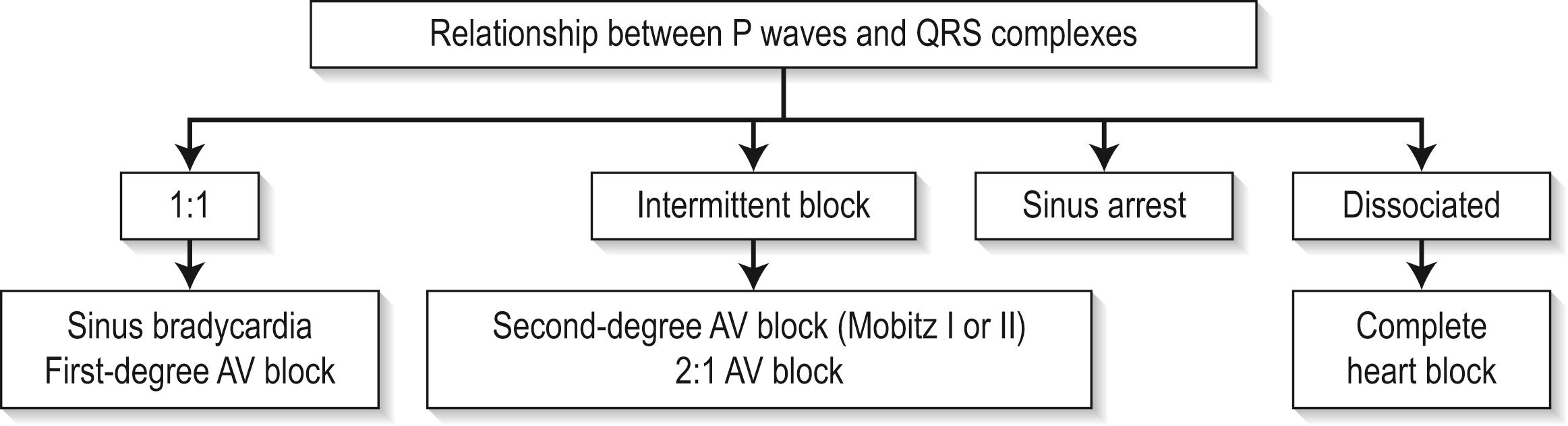
Bradycardia is defined as a heart rate of less than 60 bpm. It is important to take into account the patient’s underlying clinical state when bradyarrhythmias are being treated. ECG diagnosis of bradyarrhythmias can be simplified by the algorithm in Fig. 5.4.2 . Note that denervated transplanted hearts will not respond to atropine; thus, if treatment is required, pacing, catecholamine infusion or both should be used.
Physiological sinus bradycardia may be associated with good physical conditioning (e.g. marathon runners), drug effects (e.g. β-blockers, calcium antagonists) and vagal stimulation (e.g. vomiting). More serious causes include acute inferior myocardial infarction, raised intracranial pressure, hypothermia and hypothyroidism.
There are often no signs or symptoms. Symptoms may be related to the underlying cause.
ECG features are
Atrial rate equal to ventricular rate
Normal PR interval
Normal P-wave morphology
Treat the underlying cause. If there is evidence of hypoperfusion, intravenous atropine 0.5 mg may be used while the cause is being investigated. Physiological bradycardia does not require treatment. Disposition will depend on the cause.
This is most commonly found in elderly patients and results from fibrosis around the sinus node. It can also occur with congenital heart disease, rheumatic disorders, myocarditis, pericarditis, rheumatological disease, metastatic tumours, surgical damage, cardiomyopathies and ischaemic heart disease. It is a heterogeneous disorder that includes a wide variety of intermittent SVTs and bradyarrhythmias. Pathophysiologically, there is sinus bradycardia with intermittent failure of sinus node function, with the prolonged pause interrupted by a temporary escape rhythm. Drugs such as β-blockers, digoxin and antiarrhythmics—as well as conditions such as abdominal pain, thyrotoxicosis and hyperkalemia–can exacerbate the condition.
Typical features are syncope, light-headedness, palpitations, dyspnoea, chest pain, collapse and cerebrovascular accidents.
ECG features are
Sinus bradycardia
Intermittent cessation of P-wave activity
Long pauses interrupted by escape rhythms
Resumption of sinus node activity
Unstable patients should be managed with intravenous atropine 0.5 mg IV as a bridge to pacing. If not effective, then consider adrenaline infusion (epinephrine) (2 to 10 μg/min) or dopamine (2 to 10 μg/kg/min) infusion if pacing is delayed. Transcutaneous pacing should be required if drugs are ineffective. Drug treatment for tachyarrhythmia risks aggravating pre-existing AV block or sinus arrest and should be avoided until pacemaker insertion. These patients eventually require a permanent pacemaker.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here