Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The understanding of low-grade gliomas has significantly changed over the past 10 years. Genomic and epigenetic discoveries have revolutionized our understanding of these cancers. For the first time, the 2016 WHO classification of central nervous system tumors integrated molecular information with histologic classification to more precisely differentiate types of brain and spinal cord tumors. Previous histologic systems classified low-grade gliomas as astrocytomas, oligodendrogliomas, or mixed oligoastrocytomas based on their histologic appearance. Now, molecular classification has allowed for a more precise characterization of tumor biology (see Chapter 1 for further discussion of molecularly defined classification of gliomas).
Most diffuse low-grade gliomas can be separated into three molecularly, prognostically, and clinically distinct groups: (1) Isocitrate dehydrogenase (IDH)- gene mutated tumors with co-deletion of chromosomes 1p and 19q (e.g., IDH -mutated, co-deleted low-grade gliomas), (2) IDH -mutant non–co-deleted diffuse gliomas, and (3) IDH wild-type diffuse gliomas. This first group of IDH -mutant, co-deleted tumors are molecularly the pure oligodendrogliomas that are associated with a prolonged survival and an excellent response to chemotherapy. IDH -mutant, non–co-deleted tumors do not possess loss of chromosomes 1p and 19q (e.g., non–co-deleted) and are molecularly astrocytomas. They have an intermediate prognosis; compared to the IDH -wild-type gliomas, they have better survival rates and response to chemotherapy. IDH wild-type gliomas have the worst prognosis of the three groups and behave similarly to glioblastoma despite their lower grade.
Molecular characterization now not only influences our classification of gliomas but also guides molecularly driven clinical management decisions. Compared to treatment of high-grade gliomas, the decision for treatment of low-grade gliomas is more complex. Available data do not address all clinical questions that confront treating clinicians. One of the common challenges in clinical management of patients with low-grade gliomas is whether to initiate treatment at the time of first diagnosis or to wait until tumor growth is evident (e.g., timing of therapy). Another challenge is choosing which chemotherapeutic regimen is most optimal. Common regimens include temozolomide or lomustine, procarbazine, and vincristine (PCV) (see Chapter 4 for an evidence-based review of chemotherapy for glioma).
In this chapter, we present a single clinical case of a patient presenting with a low-grade glioma and walk through key data that guides the increasingly complex algorithms for managing patients with low-grade gliomas.
Case . A 51-year-old woman without contributory medical history acutely developed word-finding difficulties. A few minutes later she lost consciousness, collapsed to the ground, and had generalized involuntary jerking movements consistent with a generalized tonic-clonic seizure. The episode lasted for approximately 2 minutes before she regained consciousness. She was evaluated in the emergency room where her physical examination was significant for lethargy and disorientation to place and situation. Her Karnofsky performance status (KPS) was 90%. A CT scan of the head revealed an area of hypodensity in the right parietal lobe; there were no signs concerning for intracranial hemorrhage.
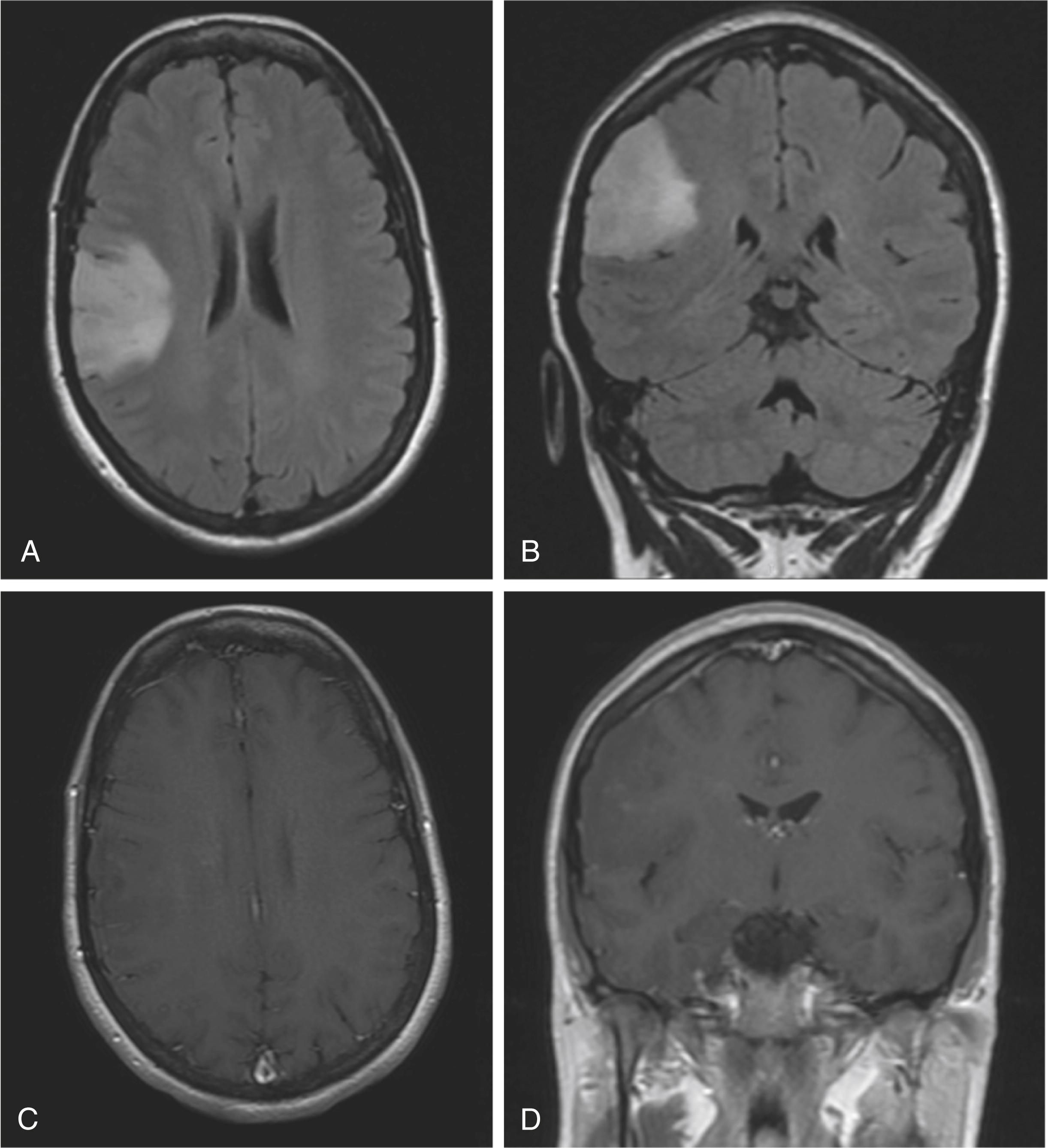
Brain magnetic resonance imaging (MRI) with and without contrast was requested to better characterize the lesion ( Fig. 11.1 ). The images showed an infiltrative lesion that involved the cortex and the subcortical white matter. The mass had a significant amount of perilesional T2/fluid attenuated inversion recovery (FLAIR) hyperintensity with minimal punctate contrast enhancement. The patient gradually recovered over the next 4 hours and was back to her baseline status without residual deficits on examination. She was started on levetiracetam 500 mg orally twice daily and dexamethasone 4 mg every 6 hours.
The patient was evaluated by a neurosurgeon who recommended performing an open biopsy through an awake craniotomy. The surgeon achieved a subtotal resection a few days after her initial presentation, while preserving eloquent brain regions. Histologic appearance was consistent with a low-grade oligodendroglioma, WHO grade II. The Ki-67 proliferation index was low and molecular studies revealed deletions of the entire short arm of chromosome 1 and the entire long arm of chromosome 19 (e.g., 1p/19q co-deletion), as well as an IDH1 R132H gene mutation. Her seizures were controlled medically and she was tapered off corticosteroids quickly after surgery. Once the pathology results were available, neuro-oncology and radiation oncology consults were requested.
What final diagnosis integrates the histopathologic analysis with molecular characterization?
Is this patient at high or low risk of early tumor progression?
Should active therapy be recommended now or is initial observation an option?
If treatment is recommended, which treatment should the patient receive?
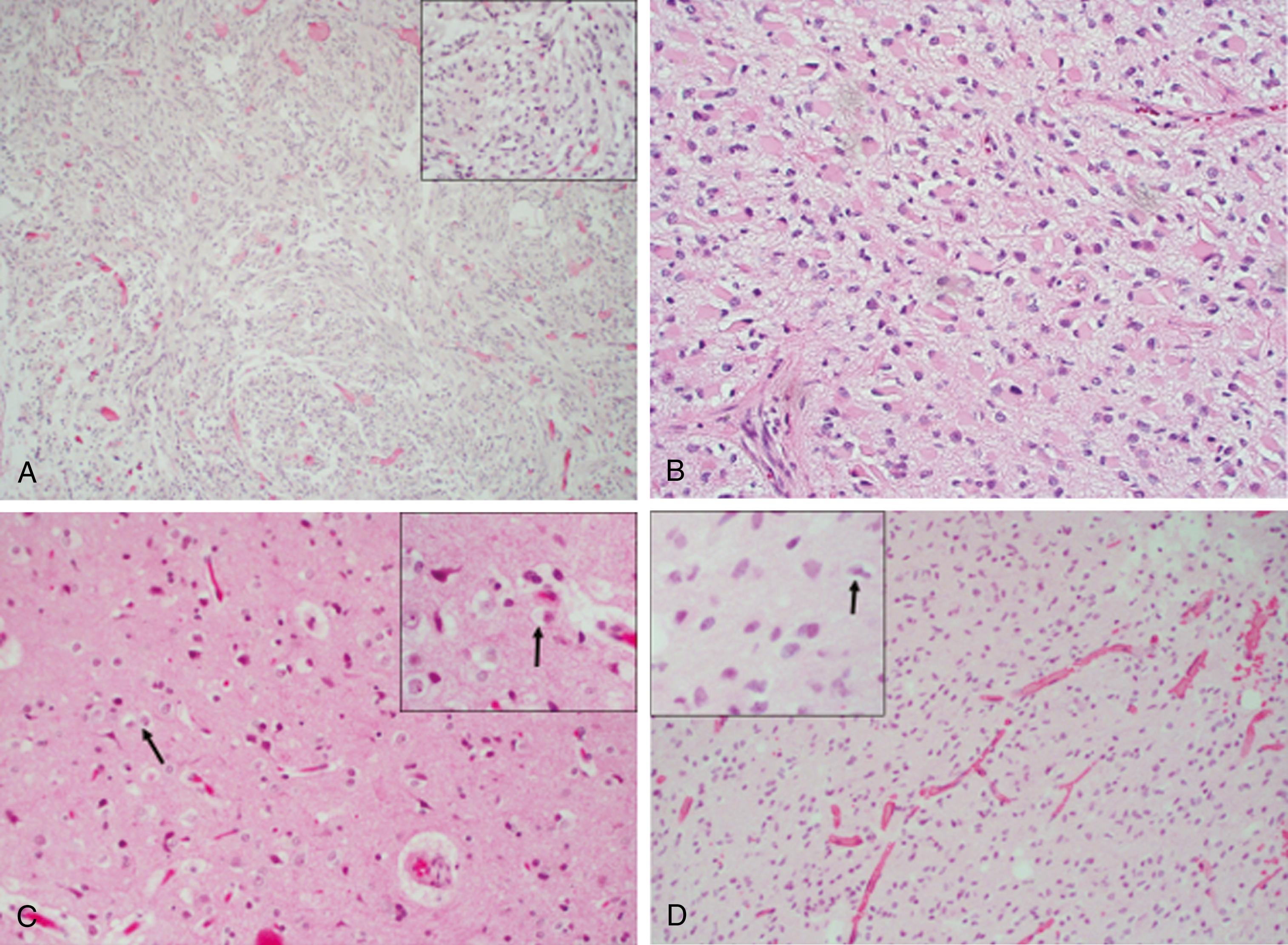
The tumor in this case was found to be a WHO grade II diffuse glioma with an IDH1 gene mutation and whole arm loss of chromosomes 1p and 19q, which is consistent with a diagnosis of IDH -mutated, co-deleted low-grade glioma. Historically, the diagnosis of low-grade gliomas was based on histopathologic analysis showing a glial-based tumor that infiltrated brain tissue and was low-grade with no or low mitotic activity, no endothelial proliferation, and no pseudopallisading necrosis (representative examples shown in Fig. 11.2 ). Over the past decade, landmark discoveries, including genome-wide studies, have shown that profiling molecular characteristics of cancer provides a more accurate way to predict treatment response and risk of recurrence. Molecular features are now a major component in the diagnosis and subgrouping of tumors and trump histopathologic interpretation and provide a more precise description of the tumor’s biology, as well as prognostic and treatment implications ( Fig. 11.3 ). Occasionally, histopathologic findings in low-grade gliomas can be difficult to distinguish from a reactive process or other brain tumors. Pilocytic astrocytomas can have a morphology that resembles oligodendrogliomas. Some tumors have features of both oligodendrogliomas and astrocytomas, historically described as oligoastrocytomas or “mixed” gliomas. In these instances, molecular characterization can guide the diagnosis. In fact, in the most recent WHO classification of gliomas, this entity of “mixed” gliomas virtually ceases to exist and these tumors are classified as oligodendrogliomas (e.g., IDH -mutant, 1p19q co-deleted) or astrocytomas (e.g., IDH -mutant, non–co-deleted) based on molecular characteristics.
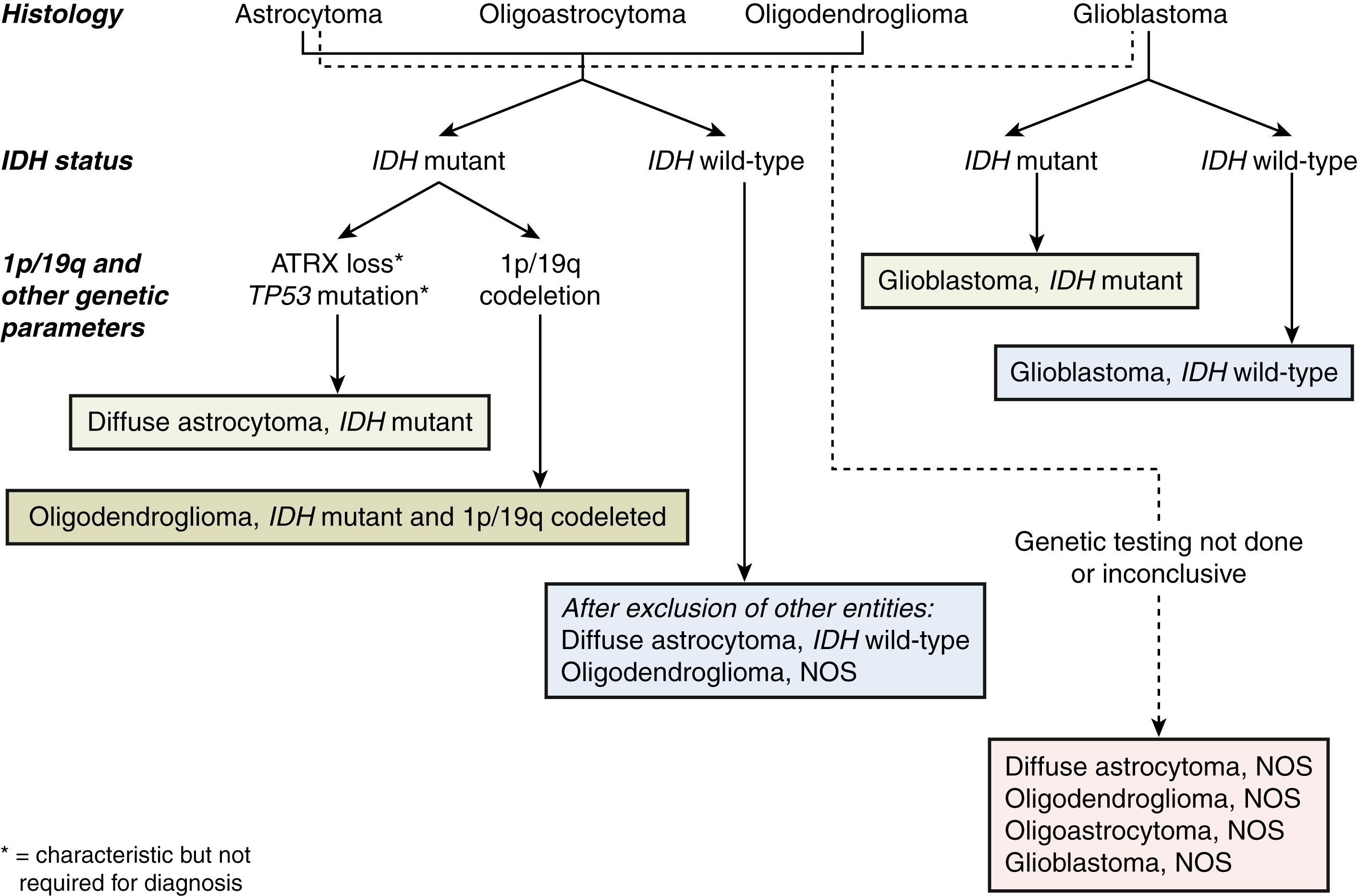
Oligodendrogliomas are characterized by the presence of an IDH1 or IDH2 mutation and synchronous whole arm deletions of chromosomes 1p and 19q. Partial deletions of 1p and 19q do occur and are not associated with the oligodendroglial phenotype; they are frequently associated with tumors of astrocytic lineage, which carry a worse prognosis. , Oligodendrogliomas frequently have an activating mutation of the TERT promoter region and mutations of the CIC and FUBP1 genes. , Astrocytic tumors may also demonstrate IDH1 or IDH2 mutation but lack co-deletion of 1p/19q and TERT promoter mutations, and instead are characterized by a loss of ATRX and mutations in the TP53 gene.
Gliomas have a similar histologic appearance in adult and pediatric populations; however, the molecular signatures of low-grade gliomas differ by age. Approximately 80–90% of low-grade tumors in adult patients harbor a mutation in the IDH1 or IDH2 genes. By contrast, low-grade gliomas in children rarely have these mutations. Adult patients with IDH wild-type diffuse astrocytomas carry a worse prognosis, especially those with a TERT promoter mutation, EGFR amplification, or a concurrent whole chromosome 10 loss and whole chromosome 7 gain. Due to the more aggressive nature of these tumors, it has been suggested that they be classified as grade IV neoplasms, irrespective of their histologic appearance.
In addition to low-grade diffuse oligodendrogliomas and diffuse astrocytomas, both of which are classified as WHO grade II tumors, there are a myriad of other low-grade gliomas. These include several histologic subtypes of tumors with an astrocytic lineage such as pilocytic astrocytoma (WHO grade I), pilomyxoid astrocytoma, gemistocytic astrocytoma, subependymal giant cell astrocytoma (SEGA), pleomorphic xanthoastrocytoma, and astroblastoma among others. Some of these tumors are exclusively seen in young adults and in the pediatric population. Other low-grade tumors arise from ependymal surfaces; these include subependymomas and ependymomas of different subtypes (myxopapillary, clear cell, tanacytic, and papillary).
The patient in this case had both favorable and concerning clinical prognostic features at presentation. On the one hand, the patient was considered to be at high risk for early disease progression due to her age (i.e., >40 years), subtotal resection (instead of complete resection of the tumor), and the proximity of the tumor to eloquent brain areas. On the other hand, several favorable prognostic factors were also identified, including her good performance status, and favorable molecular features including the presence of 1p/19q co-deletion and IDH –gene mutation.
The clinical presentation of a low-grade glioma varies depending on the tumor location. Signs and symptoms may include seizures, headaches, changes in mental status, and other symptoms associated with intracranial hypertension. Imaging findings can suggest the etiology, but in most cases, pathologic examination of a tissue sample from a biopsy or resection is needed to confirm the diagnosis. A lumbar puncture for analysis of cerebrospinal fluid has low diagnostic yield and could lead to severe complications in cases where there is risk of herniation. Patients who present with seizures are managed with antiepileptics and, when focal neurologic deficits or symptoms of increased intracranial pressure are evidenced, corticosteroids are initiated.
The natural history and prognosis of low-grade gliomas is highly variable, and assessment of risk in newly diagnosed patients is complex. There are currently no uniformly agreed-upon validated criteria to assess risk factors for early progression and poor prognosis. However, several clinical risk factors have been identified that can be used in clinical decision-making. These include tumor-related symptoms, poor performance status, preoperative tumor size (worse if ≥5 cm), incomplete resection, age (high-risk is >40 years of age), astrocytic histology, and high proliferative index (poor if MIB-1 is >3%). In addition, the absence of IDH mutation and co-deletion of 1p/19q are adverse risk factors. Many of these factors represent a continuum (for example, age), and the interplay of the different factors needs to be carefully considered on an individual basis. The best possible risk assessment relies on a personalized evaluation of clinical, molecular, and treatment factors to determine those patients who may benefit from early postoperative treatment and those for whom initial observation may be appropriate.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here